Abstract
Background and Aim
Timely diagnosis of dysphagia is important for people with an intellectual disability. Periodic screening of each individual by speech-language therapists is barely feasible with respect to limited resources. Therefore, preselection of individuals with an increased dysphagia risk through screening by caregivers is crucial.
Objective
This study aimed to develop the novel Screening instrument for Dysphagia for people with an Intellectual Disability (SD-ID).
Methods
The SD-ID was developed, validated and optimised in two rounds. Version 3, consisting of nine risk factors and 20 items concerning eating/drinking behaviour, was thoroughly studied for feasibility, concurrent validity and reliability, and then optimised.
Outcomes and Results
The SD-ID (version 3) was filled out in an average of four minutes (feasibility). A strong positive association was found between scores on SD-ID and Dysphagia Disorder Survey (concurrent validity). Test-retest and interrater reliability were very good. Two additional risk factors were added and two items removed to yield the final version 4. The most optimal cut-off score appeared to be either 4 or 5.
Conclusions and Implications
The SD-ID is a reliable instrument to screen for an increased risk of dysphagia in people with an intellectual disability. Ideally it is part of a cyclic work process: Screening with SD-ID (step 1), diagnostic work-up if necessary (step 2), recommendations (step 3), and evaluation (step 4).
Similar content being viewed by others
Avoid common mistakes on your manuscript.
People with an intellectual disability face an increased risk of dysphagia. In the Netherlands, dysphagia is present among approximately 6% of the general population without an intellectual disability (Nederlandse Vereniging voor Keel- Neus- Oorheelkunde en Heelkunde van het Hoofd-Halsgebied (NVKNO), 2017). With age, prevalence increases to 23% (Chen et al., 2009). Dysphagia is more prevalent among people with an intellectual disability: two representative studies suggest a prevalence of 8.1–11.5% (Ball et al., 2012; Chadwick & Jolliffe, 2009). With age this increases to 52% among those aged over 50 years (Hermans & Evenhuis, 2014). In intellectual disability care, the terms dysphagia and feeding and swallowing disorders are used intermingled (Manduchi et al., 2020; Sheppard et al., 2014). Here we use the term dysphagia for feeding and swallowing disorders.
Among people with an intellectual disability, dysphagia presents very differently. It often involves a combination of developmental, physiological and behavioural problems (Sheppard et al., 2014). A relation has been found between the level of intellectual disability and the presence of dysphagia: people with profound intellectual disability face the highest risk of dysphagia (Robertson et al., 2018). Since people with severe/profound and multiple disabilities often show no signs of distress when choking and therefore aspire silently, signs of mild and moderate dysphagia are frequently missed (van Timmeren et al., 2019).
Consequences of dysphagia may be severe. Aspiration pneumonia is regarded one of the most severe consequences due to the high risk of severe disease course and mortality. Other consequences include airway obstruction leading to suffocation, a poor nutritional status, dehydration or constipation. Next to health complications, psychosocial consequences comprise, among others, the inability to engage in a conversation during meals, increased stigma when eating with others and loss of dignity relating to necessary support with eating/drinking from others (Robertson et al., 2018).
Therefore, timely diagnosis of dysphagia is of the essence. Prompt examination allows identification of potential risks, which would enable speech-language therapists (SLTs) to provide dysphagia management recommendations, such as modifying oral intake (e.g., adjusting food and fluids consistencies) and initiating appropriate therapy. Currently, a diagnosis is established through clinical observation/judgement by SLTs aided by additional tests/instruments (Fig. 1a). The Dysphagia Disorder Survey (DDS) (Sheppard et al., 2014) is used in Dutch intellectual disability care to diagnose and to track changes in feeding and swallowing disorders. The DDS, consisting of a part about dysphagia related factors and a part about feeding and swallowing competencies, is considered the gold standard for systematic and comprehensive screening and objective clinical observation of dysphagia. The DDS is standardized and validated for people with an intellectual disability from a biological age of 2 years and older (Sheppard et al., 2014). Additionally, cervical auscultation, a videofluoroscopy or a fibreoptic endoscopic evaluation of swallowing (FEES) could be used. Videofluoroscopy and FEES are seldomly performed because these are often considered burdensome for people with an intellectual disability (Helmhout & Dorland, 2017).
Based on information from the diagnostic process, SLTs provide recommendations, which are ideally evaluated after a period of time (Fig. 1a; Schüller-Korevaar et al., 2022).
A major drawback of this diagnostic process (Fig. 1a) concerns the fact that periodic screening of all people with an intellectual disability by SLTs is barely feasible with respect to limited (human) resources (Chadwick & Jolliffe, 2009). Therefore, caregivers have a crucial role in the screening process. However, caregivers are insufficiently capable to recognise dysphagia (Chadwick & Jolliffe, 2009). Consequently, dysphagia is not (timely) recognised, resulting in underdiagnosis.
To address this, we are in need of a valid, reliable and quick screening instrument completed by caregivers to detect an increased risk of dysphagia. This is endorsed by O’Leary et al. (2023) in a recent sco** review. The purpose of such a screening is to determine the likelihood that dysphagia exists and the need for further assessment. Based on a specific cut-off score on such a screening instrument, SLTs may subsequently start a more comprehensive diagnostic process (Fig. 1b). Such a stepped approach enables SLTs to select individuals at risk who should be prioritised over others with respect to the available resources. Currently, such a valid, reliable and quick instrument for caregivers is not available worldwide (O’Leary et al., 2023).
Therefore, this study aims to develop and optimise a screening instrument and study it in daily practice with respect to feasibility, validity, reliability.
Methods
Study Design
This study is composed of four parts:
-
Part 1: Development of the Screening instrument for Dysphagia in people with an Intellectual Disability (SD-ID, version 1) and first pilot test.
-
Part 2: Validation of SD-ID (version 2).
-
Part 3: Validation and reliability testing of SD-ID (version 3).
-
Part 4: Final optimisation (version 4).
The results obtained in part 1 and 2 have been previously published in a peer reviewed Dutch scientific journal (van der Woude et al., 2021). Although the focus of this article concerns part 3 and 4, we also provide a brief summary of parts 1 and 2 in order to comprehensively understand the process of development and (first) validation as step**stones for part 3.
Study Setting
The three study parts have been conducted at Alliade, a care organisation in the Dutch province of Friesland providing care, diagnostic work-up and treatment for several thousands of people with an intellectual disability. With respect to provided services (various residential facilities, day-care centres, ambulatory care and outpatient clinic) and characteristics of individuals with an intellectual disability (age, sex, level of intellectual disability, living situation), Alliade and the Frisian situation is considered representative for the Dutch intellectual disability care sector.
Ethics and Consent
The Medical Ethics Review Board of the University Medical Center Groningen (UMCG) concluded that the Dutch Medical Research Human Subjects Act did not apply to this study (part 1 + 2: METc 2020/35; part 3 + 4: METc 2020/252). The project has been registered in the UMCG Research Register (part 1 + 2: nr. 202000391; part 3 + 4: nr. 202100261) and has been approved by the Review and Advisory Committee Practice-oriented Scientific Research of Alliade (nr. PWO-TAC-2021-07). The study is conducted in accordance with the EU General Data Protection Regulation and the Declaration of Helsinki.
SLTs selected participants according to the following inclusion criteria: diagnosed intellectual disability (mild, moderate, severe or profound) based on (medical) records and eligible for long-term residential care at Alliade. Exclusion criteria were: no intellectual disability, acquired brain injury, tube feeding without oral supplementary feeding and < 18 years. Legal representatives were informed about the study with an information folder. After given consent, concordance with inclusion and exclusion criteria were double checked. To ensure sufficient diversity within the study group, differences in age, sex and level of intellectual disability were taken into account. SLTs collected data on basis of privacy by design and data minimization. Data were pseudonymized.
Part 1: Development of SD-ID (version 1) and First Pilot Test
Development
The SD-ID is developed on the basis of symptoms obtained from (1) scientific literature, (2) existing, suboptimal screening instruments for dysphagia and (3) experiences from SLTs and physicians for people with an intellectual disability in the Netherlands.
Firstly, risk factors for dysphagia and symptoms indicative of dysphagia (eating/drinking behaviour) were obtained from English literature using databases PubMed and Scopus. Search terms concerned: ‘dysphagia AND intellectual disabilities’, ‘dysphagia AND mental retardation’, ‘risk factors AND dysphagia’, ‘screening AND dysphagia AND intellectual disabilities’, ‘asphyxiation AND risk factors’ and ‘choking AND risk factors’. With respect to ambiguous results, specific additional database searches were performed to clarify this. Relevant publications found in reference lists of obtained articles were included as well.
Secondly, symptoms included in items in two freely available Dutch screening instruments – Signaleringslijst Verslikken (SV) (Helder, 2010) and Verslik Alarm Lijst (VAL) (Helder, 2010)– and one English instrument – Nutrition and Swallowing Checklist (NSC) (Stewart, 2003) – were studied as well.
Thirdly, two SLTs (SvdW/MSK) with vast experience in intellectual disability care, evaluated the relevance of found risk factors, symptoms indicative of dysphagia from literature and symptoms found in existing instruments. This finally resulted in an integrated list of symptoms to be included in the SD-ID. Symptoms were deduplicated, merged and clarified. The SD-ID has two sections: section A consists of items addressing risk factors and section B consists of items addressing symptoms concerning eating/drinking behaviour that are indicative of dysphagia. The fifth column in Table 1 shows the source(s) on which the included items were based.
The scoring system considered characteristics and working circumstances of caregivers in daily practice, that is (1) limited time (completion of the SD-ID should maximally take 10 min) and (2) limited background and education in dysphagia. Consequently, we decided to implement an easy, self-explanatory and time efficient dichotomous scoring system, largely in accordance with Helder (2010). Items are to be scored by caregivers as ‘yes’ (score = 1) or ‘no’ (score = 0) based on observations. Three prerequisites have been defined: 1) caregivers need to work at least two months with the person with an intellectual disability, 2) caregivers should have been present at least at one meal of the person in the week before completing the SD-ID and (3) the person is not completely tube feeded.
Pilot Test: Validity and Optimisation
Face validity of SD-ID version 1 was ensured by presenting it to two panels of experts in intellectual disability care: a panel of 7 SLTs and a panel of 10 physicians specialised in people with an intellectual disability. Both panels deemed the content of the SD-ID appropriate and did not provide additional items. Concurrent validity was studied in a cross-sectional pilot study with 42 individuals. For each person, the SD-ID was completed by one caregiver, followed by a meal observation (almost without exception at breakfast) by a SLT within two weeks using the DDS. In this study, a DDS score of ≥ 3 points is considered indicative of the presence of dysphagia. Experiences obtained in the pilot study provided input for slight optimisation for SD-ID version 2 (see flow chart, Fig. 2).
Part 2: Validation of SD-ID (version 2)
The slightly optimised SD-ID version 2 was subsequently used in daily practice for a large population of 1064 eligible people with an intellectual disability (cross-sectional sample). Resembling the pilot study (part 1), the SD-ID was completed by one caregiver for each person. In contrast to part 1, SLTs only observed a meal with the DDS for this person if SD-ID score was ≥ 1 points due to restrains in resources (n = 759).
In the context of optimisation (Fig. 2), we evaluated three aspects: (1) additional risk factors, (2) item relevance (items which are hardly scored have limited clinical relevance) and (3) association between items (using the symmetrical association measure Phi).
Part 3: Validation and Reliability Testing of SD-ID (version 3)
The optimised SD-ID (version 3) was studied in further depth for 220 individuals (cross-sectional sample). A total of 387 individuals were invited (according to inclusion and exclusion criteria mentioned in Methods section Ethics and Consent), living at 31 residential facilities of Alliade. With respect to a representative sample, a purposeful sample was obtained selecting individuals with different ages, sex and levels of intellectual disability. In part 3 we determined (1) feasibility, (2) concurrent validity, (3) reliability and (4) required optimisation. Study data were collected and managed using Research Electronic Data Capture (REDCap) system hosted at Alliade (Harris et al., 2009, 2019).
Feasibility
An important goal of the SD-ID was a short administration time (maximum 10 min). Caregivers completed the instrument digitally and the time it took to complete was measured. The automatic count in REDCap started when the form was opened by the caregiver and stopped after sending the form.
Concurrent Validity
The validity of the SD-ID version 3 was tested against the DDS (≥ 3 points), similar to parts 1 and 2.
Reliability
Test-retest reliability was calculated by asking the same caregiver to complete the SD-ID again for the same participant after 2–5 weeks. If a participant faced changes that may affect eating/drinking between the first and the second date of completion, this person was excluded from retest analyses. Participants who did not face changes or faced changes without effect on eating/drinking were included. Interrater reliability was calculated by asking two caregivers to complete the SD-ID for the same participant in the same period of time. For both test-retest reliability and interrater reliability, SD-ID scores were only analysed if they had been completed prior to the SLTs’ dysphagia diagnosis to prevent bias.
Required Optimisation
In the context of optimisation (Fig. 2), three aspects were evaluated: (1) additional risk factors, (2) item relevance (items which are hardly scored have limited clinical relevance) and (3) removal of items with minimal reliability.
Specifically, some risk factors were found in literature, which may be of additional importance for the SD-ID, namely (a) medication, (b) dependent eater and (c) using wheelchair for all mobility and/or physical disability (Chadwick & Jolliffe, 2009; Perez et al., 2017; van der Woude et al., 2021).
-
a)
Medication that often to very often has side effects of dysphagia and/or dry mouth was tested as a possible risk factor. The first rater filled out which drugs the participant was taking. The completion time of the form was automatically tracked in order to estimate the time investment. Medication was categorized based on ATC-codes. Only ATC-groups with 10 or more registrations were considered in this study, that is, the antiepileptics (N03A), antipsychotics (N05A), anxiolytics (N05B), and antidepressants (N06A).
-
b)
Dependent eater: It was tested whether not being able to eat independently is a risk factor for dysphagia. In the DDS this item is scored in four variables: (1) eating completely independent, (2) eating independent with little assistance, (3) eating completely dependent, and (4) being completely tube feeded. Here, we compared participants with score 3 versus scores 1 + 2 (tube feeded was an exclusion criterion).
-
c)
Using a wheelchair was recorded as absent or only for long distances outdoors versus always. The absence/presence of a physical disability was also recorded. The two variables wheelchair-user for all mobility and physical disability were merged into a common ‘and/or’ variable.
Part 4: Final Optimisation of SD-ID (version 4) and Optimal Cut-Off Score
Based on the outcome of the previous step, a final SD-ID version 4 was created. Sensitivity, specificity, positive and negative predictive values, and area under the receiver operating characteristic curve (ROC) were calculated for each SD-ID score as compared to the absence (DDS < 3 points) and presence (DDS ≥ 3 points) of dysphagia based on the DDS score. Optimal cut-off scores were determined by maximizing Youden’s index (Šimundić, 2009; Trevethan, 2017). In addition, percent agreement was determined between DDS-dysphagia diagnosis (DDS ≥ 3 points) and SD-ID score, based on calculated cut-off scores.
Statistics
Categorical variables were compared using Pearson’s Chi-squared tests, ordinal data using Fisher-Freeman-Halton Exact Test and continuous data using independent t-test.
Internal consistency was determined using the Kuder-Richardson Formula 20 (KR-20) and concurrent validity was determined associating the total SD-ID score with the total DDS score using Spearman’s rank correlation. Since in part 2 the SD-ID = 0 scores could not be compared to DDS scores given the absence of observations by SLTs, these results provide a mere indication.
Considering the optimisation in part 2 (see Methods section Part 2: Validation of SD-ID (version 2)), the effect of Down syndrome (present/absent) and level of intellectual disability (mild, moderate, severe/profound) on the mean SD-ID scores were determined using independent t-test and one-way ANOVA, respectively. Associations (symmetrical) between individual items were determined using Phi. Interpretation of Phi: strong (0,51 − 0,80), very strong (0,81 − 0,99) and perfect (1) association (van Groningen & de Boer, 2016). For more detailed descriptions of the methods of part 1 and 2 (not further elaborated on here) we refer to (van der Woude et al., 2021).
Test-retest and interrater reliability: Total scores were compared using intraclass correlation coefficients (ICC) and item scores (dichotomous variable) were compared using both Cohen’s kappa and percent agreement.
The associations between DDS-dysphagia diagnosis and the additional risk factors medication groups, dependent eater, and wheelchair-user for all mobility and/or physical disability were determined by means of Chi-square tests and logistic regression (DDS diagnosis as dependent variable).
Analyses have been performed in IBM SPSS Statistics version 28 and JASP version 16.2.
Results
A four-part development process led to the final version of the SD-ID (version 4). The developmental process is shown in Fig. 2. Each part of the process is described separately below.
Part 1: Development of SD-ID (version 1) and First Pilot Test
The first SD-ID version consisted of section A with 8 risk factors for dysphagia and section B with 20 items about eating/drinking behaviour (van der Woude et al., 2021). A pilot with 42 persons (69% male, mean age 43.1 ± 14.7 years, age range from 18.1 to 72.7 years) with different levels of intellectual disability (14.3% mild; 31.0% moderate; 54.8% severe/profound) yielded first insights in validity and use in daily practice.
Concerning concurrent validity, Spearman’s rank correlations indicated strong positive association between scores on SD-ID and DDS (rho = 0.753; p < 0.001, n = 42). A higher SD-ID score thus generally associates with a higher DDS score. KR-20 demonstrated that the 28 items together constituted a reliable scale for measuring the latent variable ‘risk of dysphagia’ (alpha = 0.907). Removing individual items did barely improve the internal consistence. Experiences in daily practice lead to one item being changed to two separate items (van der Woude et al., 2021).
Part 2: Validation of SD-ID (version 2)
The optimised SD-ID version 2 consisted of section A with again 8 risk factors and section B with 21 items about eating/drinking behaviour. It was subsequently tested among 1064 individuals (57.0% male, mean age 48.9 ± 15.3 years, age range from 18.0 to 91.3 years) with different levels of intellectual disability (27.4% mild; 37.5% moderate; 35.1% severe/profound).
Concerning concurrent validity, Spearman’s rank correlations indicated a moderate-strong positive association between scores on SD-ID and DDS (rho = 0.665; p < 0.001, n = 759). A higher SD-ID score thus generally associates also in this second version, with a higher DDS score, although these results might be slightly biased by the lack of a DDS score for those with SD-ID = 0 (n = 305). KR-20 demonstrated that the 29 items together constituted a reliable scale (alpha = 0.879). Removing individual items did barely improve the internal consistence.
Concerning optimisation, the presence of Down syndrome and severe/profound intellectual disability were found to be relevant to add as additional items to section A. Two other items were removed and experiences in daily practice guided rephrasing of items and addition of notes/examples (van der Woude et al., 2021).
Part 3: Validation and Reliability Testing of SD-ID (version 3)
SD-ID
The new SD-ID version 3 (Table 1) included 9 risk factors (section A) and 20 items (section B). The fifth column in Table 1 indicates the basis for a specific risk factor or symptom, i.e., literature, existing screening instruments, experiences in daily practice or results from study parts 1 and 2.
Study Population and Characteristics
Figure 3 shows the flow chart of inclusion/exclusion of participants. In summary, caregivers completed 229 unique assessments. For 224 individuals SLTs were able to complete a subsequent valid observation with the DDS. Four of those had to be excluded as the person faced changes between the moment of SD-ID completion and DDS completion that may impact his/her eating/drinking behaviour. Characteristics of the 220 included participants and their caregivers are provided in Table 2. Comparing those with a dysphagia diagnosis (DDS ≥ 3 points) and without (DDS < 3 points), demonstrated that dysphagia is more prevalent with increasing severity of intellectual disability. Moreover, dysphagia is less prevalent in those with autism spectrum disorder.
Flow chart of participants’ recruitment, including reasons for exclusion and final numbers of inclusions
Legend: *The three prerequistes are described in Methods section Development (Part 1).
Feasibility
After removing three outliers (> 5000 s) who appeared to have been disturbed in their daily work, the mean completion time for the entire SD-ID (n = 217) was found to be 4.0 min (SD = 4.5; range = 0.8–43.3). The additional medication form was completed on average in 2.9 min (SD = 2.5; range = 0.1–17.9).
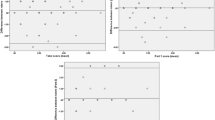
Validity
Concurrent validity was assessed with Spearman’s rho, indicating a strong positive association between scores on SD-ID and DDS (rho = 0.772, p < 0.001, n = 220). Additionally, logistic regression was calculated with the total SD-ID score as independent variable and the presence/absence of dysphagia based on the DDS score (DDS ≥ 3 points) as dependent variable. SD-ID score was positively associated with the presence/absence of dysphagia: a higher SD-ID score yielded a higher risk of the presence of dysphagia (B = 0.481; OR = 1.611; 95% CI: 0.346–0.608; p < 0.001).
Reliability
KR-20 indicated that the 29 items of the SD-ID constitute a reliable scale (alpha = 0.868). Test-retest reliability was established for 171 individuals. For the entire SD-ID score (continuous), an ICC was found of k = 0.961 with 95% CI: 0.947–0.971. Interrater reliability was calculated for n = 174 individuals with ICC of k = 0.942 with 95% CI: 0.922–0.957. Table 3 presents reliability results for individual item scores (dichotomous) using Cohen’s kappa and % agreement. Overall, results demonstrate adequate to excellent reliability, with the exception of moderate interrater reliability for items 13, 14, 21, and 26 (based on more stringent Cohen’s kappa).
Optimisation
Three potential risk factors were studied: (a) medication, (b) dependent eater and (c) wheelchair-user for all mobility and/or physical disability. The use of N03A (antiepileptics), N05A (antipsychotics), N05B (anxiolytics) and N06A (antidepressants) were compared between the groups with and without a DDS dysphagia diagnosis: antipsychotics were used significantly less in the group with dysphagia (χ² (1) = 5.765; p = 0.016), while anxiolytics seemed to be used more in the group with dysphagia (χ² (1) = 4.051; p = 0.044). However, the power of the anxiolytics test is low, due to the low numbers in each group (n = 9 with dysphagia, n = 2 without dysphagia), which makes interpretation difficult. The use of antiepileptics and antidepressants did not differ significantly between groups. Binary logistic regression analysis showed that the use of antipsychotics negatively predicts dysphagia (p = 0.021; OD’s ratio = 0.336 with 95% CI = 0.133–0.845), while the use of antiepileptics (p = 0.165), anxiolytics (p = 0.063) or antidepressants (p = 0.249) were not predictive.
Next, comparing groups with/without a dysphagia diagnosis (Table 2) showed that all 25 participants who are dependent eaters, also have a DDS dysphagia diagnosis (χ2(1) = 25.753; p < 0.001). No logistic regression analysis was performed, as there were no cases with eater dependency and absence of dysphagia diagnosis. Among the 82 participants who had a physical disability and/or used a wheelchair for all mobility, 68 (82.9%) had a DDS dysphagia diagnosis (χ2(1) = 49.237; p < 0.001). Logistic regression analysis suggests that physical disability and/or using a wheelchair is predictive of dysphagia (p < 0.001; OD’s ratio = 9.404 with 95% CI = 4.791–18.459). Taken together, two risk factors (dependent eater and physical disability and/or wheelchair use for all mobility) were deemed appropriate to add to SD-ID version 4. The use of antipsychotics was not added with respect to the questionable clinical relevance. After all, the use of antipsychotics was even significantly less in the group with dysphagia as compared to those without.
Furthermore, data suggested that 5 items were potential candidates for removal. First of all, item 28 was found to be scored the least frequent (Table 1) in the group with a dysphagia diagnosis, indicating limited clinical relevance. Moreover, items 13, 14, 21 and 26 had minimal interrater reliability (underlined in Table 3; (McHugh, 2012). Together with item 28, these items were further evaluated by comparing them between the groups with and without a DDS dysphagia diagnosis (p-values: item 13, p = 0.016; item 14, p = 0.006; item 21, p < 0.001; item 26, p = 0.692; item 28, p = 0.910). Based on these results, items 26 and 28 were deemed appropriate for removal as they did neither clinically nor statistically contribute to differentiating between those with and without a dysphagia diagnosis.
Part 4: Optimised SD-ID (version 4) and Cut-Off Score
Adding and removing items finally yielded the definitive SD-ID version 4 (Table 1, V4). Recalculating scores enabled us to determine sensitivity, specificity, PPV and NPV for each score (Table 4). The most optimal SD-ID (version 4) cut-off score appeared to be either score 4 or 5. Moreover, for each SD-ID score, the sum of the number of true positives and true negatives was compared to the dysphagia diagnosis (present/absent) according to the DDS using percent agreement. SD-ID = 4 and SD-ID = 5 yielded the same percent agreement, that is 82.3%. KR-20 indicated that the 29 items of the SD-ID version 4 constitute a reliable scale (alpha = 0.883).
Discussion
The aim of this study was to develop a screening instrument to assess the risk of dysphagia in people with an intellectual disability, which can be easily used by caregivers in daily practice. To the best of our knowledge, such an instrument does not exist to date, as was also indicated by O’Leary et al. (O’Leary et al., 2023). In a process of four study parts such an instrument has been developed, resulting in the final SD-ID version 4. In the first part, the instrument was developed based on literature, suboptimal existing instruments and experiences in daily practice. Data from a small pilot (n = 42) led to optimisation. In the second part, the optimised version was studied (n = 1064), again yielding aspects for optimisation, resulting in the third version. In the third part, version 3 was studied in more depth among n = 220 individuals for feasibility, as well as reliability. SD-ID version 3 was found to be feasible as it could be completed on average in 4.0 min (SD = 4.5) by caregivers. In all three study parts, internal consistency (alpha = 0.907, 0.879 and 0.868, resp.) and convergent validity (rho = 0.753, 0.665 and 0.772, resp.) were promising. Similarly, a higher SD-ID version 3 score yielded a higher risk of the presence of dysphagia (B = 0.481; OR = 1.611; p < 0.001). Excellent test-retest reliability (ICC = 0.961) and interrater reliability (ICC = 0.942) were found for the entire SD-ID as well as for most individual items. In part four, additional risk factors were evaluated, as well as items with low scoring frequencies and items with minimal interrater reliability. The evaluation resulted in removal of two items and addition of two risk factors, finally resulting in the definite SD-ID version 4 This version appeared to have optimal cut-off scores of 4 or 5.
The final SD-ID (version 4) has proven to be a useful instrument to assess the risk of dysphagia in people with an intellectual disability and it fits perfectly well in a cyclic work process, visualised in Fig. 1b. The large benefit of the SD-ID, compared to the DDS, is that it can be used by daily caregivers and it takes not more than a few minutes to complete. It does not pretend to make a dysphagia diagnosis, but aims to map out the risk of dysphagia, which SLTs can subsequently act upon.
Study Strengths
An important strength of this study is that it addresses a highly frequent question from daily practice regarding the need for a valid, reliable and quick screening instrument for caregivers to detect an increased risk of dysphagia.
The second strength is the large diverse sample of participants. Alliade is a care organisation that provides care for a varied group of people with intellectual disability and therefore the sample of participants is a representative reflection of Dutch intellectual disability care.
The third strength is that this study consisted of several rounds, which enabled us to reflect on the obtained results and to constantly optimise the instrument. The fourth strength is that the SD-ID is developed by triangulation, because it is based on scientific literature, existing suboptimal screening instruments for dysphagia and experiences from SLTs and physicians for people with intellectual disability in the Netherlands.
Study Limitations
A first limitation is that the SLTs who developed the SD-ID also conducted the data collection of this study, which could have introduced a slight bias. However, caregivers completed the SD-ID (not the SLTs), which may reduce this risk again. In addition, in part 3 these two SLTs were assisted by a third SLT, who did not participate in development of the SD-ID and in part 2 the data collection was performed by eleven SLTs working at Alliade. As bias is less likely to occur in a bigger group of SLTs that are not the main developers of the SD-ID, this issue was partly addressed.
A second limitation is that scoring frequency of some items was too low to yield solid conclusions. In particular the additional tests of some of the risk factors of part A are underpowered due to the low scoring frequency.
A third limitation is that the search strategies in scientific databases for literature were not fully systematic according to the PRISMA criteria (Moher et al., 2009). Furthermore, the assessment of relevance of findings in literature and items in existing instruments were not based on a strict predetermined protocol, but this assessment was strongly based upon practical experiences of SLTs with vast experience in intellectual disability care. This can be seen as a limitation, but also as a strength.
Implications for Daily Practice
This study indicates that SD-ID is a feasible, valid and reliable screening instrument to be implemented in daily practice. It is recommendable to incorporate the SD-ID in the first step of a cyclic work process (visualised in Fig. 1b, more details in (Schüller-Korevaar et al., 2022). Based on the SD-ID score, individuals at risk can be identified to prioritise for further diagnostic work-up by SLTs. The use of such a two-step process strongly contributes to reducing underdiagnosis and enhancing efficient care, because limitations in resources (financial, human) are common nowadays. Depending on available resources, care organisations can choose for SD-ID cut-off score 4 (higher sensitivity, lower specificity) or 5 (higher specificity, lower sensitivity). This has to be considered, balancing pros and cons as well as practical limitations. Although Alliade is considered representative for the Dutch intellectual disability care sector, further study of the SD-ID would preferably include other care organisations as well.
Conclusions
In a series of rounds, we developed and optimised the SD-ID. Version 3 was thoroughly studied and found to be feasible (average time 4 min), valid (strong concurrent correlation with the DDS) and reliable (high internal consistency, adequate to excellent interrater and test-retest reliability). The SD-ID was optimised again by adding two risk factors to part A and removing two items from part B. This final version 4, with a total number of 29 items, was found to have the best sensitivity, specificity, positive and negative predictive values with cut-off score 4, closely followed by cut-off score 5.
The SD-ID proved to be a valid and reliable instrument to screen for an increased risk of dysphagia. Ideally, the SD-ID is an integral part of a cyclic work process, in which screening with the SD-ID is the first step. By using the SD-ID, the risk of dysphagia can be detected earlier and SLTs can prioritise which individuals need diagnostic work-up. This allows the further treatment process to be initiated with the ultimate goal of reducing the potential risk of dysphagia consequences and increasing quality of life.
References
AlMutairi, H., O’Dwyer, M., Burke, E., McCarron, M., McCallion, P., & Henman, M. C. (2020). Laxative use among older adults with intellectual disability: A cross-sectional observational study. International Journal of Clinical Pharmacy, 42(1), 89–99. https://doi.org/10.1007/s11096-019-00942-z.
Aziz, S. J., & Campbell-Taylor, I. (1999). Neglect and abuse Associated with Undernutrition in Long-Term Care in North America: Causes and solutions. Journal of Elder Abuse and Neglect, 10(1–2), 91–117. https://doi.org/10.1300/J084v10n01_07.
Ball, S. L., Panter, S. G., Redley, M., Proctor, C. A., Byrne, K., Clare, I. C. H., & Holland, A. J. (2012). The extent and nature of need for mealtime support among adults with intellectual disabilities. Journal of Intellectual Disability Research, 56(4), 382–401. https://doi.org/10.1111/j.1365-2788.2011.01488.x.
Böhmer, C. J. M., Taminiau, J. A. J. M., Klinkenberg-Knol, E. C., & Meuwissen, S. G. M. (2001). The prevalence of constipation in institutionalized people with intellectual disability. Journal of Intellectual Disability Research, 45(3), 212–218. https://doi.org/10.1046/j.1365-2788.2001.00300.x.
Chadwick, D. D., & Jolliffe, J. (2009). A descriptive investigation of dysphagia in adults with intellectual disabilities. Journal of Intellectual Disability Research, 53(1), 29–43. https://doi.org/10.1111/j.1365-2788.2008.01115.x.
Chen, P. H., Golub, J. S., Hapner, E. R., & Johns, M. M. (2009). Prevalence of perceived dysphagia and quality-of-life impairment in a geriatric population. Dysphagia, 24(1), 1–6. https://doi.org/10.1007/s00455-008-9156-1.
Faulks, D., Collado, V., Mazille, M. N., Veyrune, J. L., & Hennequin, M. (2008). Masticatory dysfunction in persons with Down’s syndrome. Part 1: Aetiology and incidence. Journal of Oral Rehabilitation, 35(11), 854–862. https://doi.org/10.1111/j.1365-2842.2008.01877.x.
Harris, P. A., Taylor, R., Thielke, R., Payne, J., Gonzalez, N., & Conde, J. G. (2009). Research electronic data capture (REDCap) - a metadata-driven methodology and workflow process for providing translational research informatics support. Journal of Biomedical Informatics, 42(2), 377–381, https://doi.org/10.1016/j.jbi.2008.08.010.
Harris, P. A., Taylor, R., Minor, B. L., Elliott, V., Fernandez, M., O’Neal, L., McLeod, L., Delacqua, G., Delacqua, F., Kirby, J., & Duda, S. N. (2019). The REDCap consortium: Building an international community of software platform partners. Journal of Biomedical Informatics, 95, 103208, https://doi.org/10.1016/j.jbi.2019.103208.
Helder, A. M. (2010). De Signaleringslijst Verslikken: eindrapport van het onderzoeksproject “signaleren van verslikken.”
Helmhout, S., & Dorland, L. (2017). Hap, slik… (verkeerde) weg…: Praktijkgericht onderzoek naar prevalentie van slikproblemen bij volwassenen met een verstandelijke beperking. Nederlands Tijdschrift voor de Zorg aan mensen met verstandelijke beperkingen (NTZ), 3, 207–218.
Hermans, H., & Evenhuis, H. M. (2014). Multimorbidity in older adults with intellectual disabilities. Research in Developmental Disabilities, 35(4), 776–783. https://doi.org/10.1016/j.ridd.2014.01.022.
Horiguchi, S., & Suzuki, Y. (2011). Screening Tests in Evaluating Swallowing. Japan Medical Association Journal, 54(1), 30–34.
Logemann, J. A. (1999). Behavioral management for oropharyngeal dysphagia. Folia Phoniatrica et Logopaedica, 51(4–5), 199–212. https://doi.org/10.1159/000021497.
Manduchi, B., Fainman, G. M., & Walshe, M. (2020). Interventions for feeding and swallowing disorders in adults with intellectual disability: A systematic review of the evidence. Dysphagia, 35(2), 207–219. https://doi.org/10.1007/s00455-019-10038-5.
McHugh, M. L. (2012). Interrater reliability: The kappa statistic. Biochemia Medica, 22(3), 276–282. http://www.ncbi.nlm.nih.gov/pubmed/23092060.
Moher, D., Liberati, A., Tetzlaff, J., Altman, D. G., The, P. R. I. S. M. A., Group, Altman, D. G., Antes, G., Atkins, D., Barbour, V., Barrowman, N., Berlin, J. A., Clark, J., Clarke, M., Cook, D., D’Amico, R., Deeks, J. J., Devereaux, P. J., Dickersin, K., Egger, M., & Tugwell, P. (2009). Preferred reporting items for systematic reviews and meta-analyses: The PRISMA statement. PLoS Medicine, 6(7), 1–6. https://doi.org/10.1371/journal.pmed.1000097.
Morabito, G., Romeo, C., & Romano, C. (2014). Functional aerophagia in children: A frequent, atypical disorder. Case Reports in Gastroenterology, 8(1), 123–128. https://doi.org/10.1159/000362441.
Nederlandse Vereniging voor Keel- Neus- Oorheelkunde en Heelkunde van het Hoofd-Halsgebied (NVKNO). (2017). Richtlijn Orofaryngeale Dysfagie. In Richtlijnendatabase. Available at: https://richtlijnendatabase.nl/richtlijn/orofaryngeale_dysfagie.
O’Leary, L., Maine, A., Ring, N., Reid, J., Speirs, L., Allan, L., Truesdale, M., & Taggart, L. (2023). A sco** review of the evidence for the use of screening tools in people with intellectual disabilities with dysphagia. Journal of Applied Research in Intellectual Disabilities, 36(3), 429–447. https://doi.org/10.1111/jar.13076.
Perez, C. M., Wagner, A. P., Ball, S. L., White, S. R., Clare, I. C. H., Holland, A. J., & Redley, M. (2017). Prognostic models for identifying adults with intellectual disabilities and mealtime support needs who are at greatest risk of Respiratory Infection and emergency hospitalisation. Journal of Intellectual Disability Research, 61(8), 737–754. https://doi.org/10.1111/jir.12376.
Robertson, J., Chadwick, D., Baines, S., Emerson, E., & Hatton, C. (2018). People with intellectual disabilities and dysphagia. Disability and Rehabilitation, 40(11), 1345–1360. https://doi.org/10.1080/09638288.2017.1297497.
Samuels, R., & Chadwick, D. D. (2006). Predictors of Asphyxiation risk in adults with intellectual disabilities and dysphagia. Journal of Intellectual Disability Research, 50(5), 362–370. https://doi.org/10.1111/j.1365-2788.2005.00784.x.
Schüller-Korevaar, R.M., van der Woude, T.S., Landsman, J. A., Fokkens, A. S., & Dekker, A. D. (2022). Periodieke screening, diagnostiek en behandeladviezen van dysfagie bij mensen met verstandelijke beperkingen. Praktijkervaringen met een cyclisch dysfagiewerkproces. Nederlands Tijdschrift voor de Zorg aan mensen met verstandelijke beperkingen (NTZ), 3, 82–94.
Sheppard, J. J., Hochman, R., & Baer, C. (2014). The Dysphagia Disorder Survey: Validation of an assessment for swallowing and feeding function in developmental disability. Research in Developmental Disabilities, 35(5), 929–942. https://doi.org/10.1016/j.ridd.2014.02.017.
Sheppard, J. J., Malandraki, G. A., Pifer, P., Cuff, J., Troche, M., Hemsley, B., Balandin, S., Mishra, A., & Hochman, R. (2017). Validation of the choking risk assessment and Pneumonia risk assessment for adults with intellectual and developmental disability (IDD). Research in Developmental Disabilities, 69, 61–76. https://doi.org/10.1016/j.ridd.2017.07.016.
Šimundić, A. M. (2009). Measures of diagnostic accuracy: Basic definitions. The Journal of the International Federation of Clinical Chemistry and Laboratory Medicine (EJIFCC), 19(4), 203–211.
Stewart, L. (2003). Development of the Nutrition and Swallowing Checklist, a screening tool for nutrition risk and swallowing risk in people with intellectual disability. Journal of Intellectual and Developmental Disability, 28(2), 171–187. https://doi.org/10.1080/1366825031000106945.
Thacker, A., Abdelnoor, A., Anderson, C., White, S., & Hollins, S. (2008). Indicators of choking risk in adults with learning disabilities: A questionnaire survey and interview study. Disability and Rehabilitation, 30(15), 1131–1138. https://doi.org/10.1080/09638280701461625.
Trevethan, R. (2017). Sensitivity, specificity, and predictive values: Foundations, pliabilities, and pitfalls in research and practice. Frontiers in Public Health, 5(307), 1–7. https://doi.org/10.3389/fpubh.2017.00307.
van der Woude, T.S., Schüller-Korevaar, R.M., Verheij-Jansen, N., Fokkens, A. S., & Dekker, A. D. (2021). Screeningsinstrument voor Dysfagie bij mensen met een Verstandelijke Beperking (SD-VB): Ontwikkeling en eerste validering. Nederlands Tijdschrift voor de Zorg aan mensen met verstandelijke beperkingen (NTZ), 2, 50–65.
van Groningen, B., & de Boer, C. (2016). Beschrijvende statistiek: Het berekenen en interpreteren van tabellen en statistieken. Boom uitgevers.
van Timmeren, E. A., van der Putten, A. A. J., van Schrojenstein Lantman-de Valk, H. M. J., van der Schans, C. P., & Waninge, A. (2016). Prevalence of reported physical health problems in people with severe or profound intellectual and motor disabilities: A cross-sectional study of medical records and care plans. Journal of Intellectual Disability Research, 60(11), 1109–1118. https://doi.org/10.1111/jir.12298.
van Timmeren, E. A., Deddens, A., van Schrojenstein Lantman-de Valk, H. M. J. J., van der Schans, C. P., Krijnen, W. P., Waninge, A., van der Putten, A. A. J. J., van Timmeren, D. E. A., Deddens, A., van Schrojenstein Lantman-de Valk, H. M. J. J., van der Schans, C. P., Krijnen, W. P., Waninge, A., & van der Putten, A. A. (2019). J. J. The convergent validity of a Dutch screening tool for dysphagia (Signaleringslijst Verslikken) for people with severe or profound intellectual and multiple disabilities. Journal of Applied Research in Intellectual Disabilities, 32(4), 994–1001. https://doi.org/10.1111/jar.12592.
Acknowledgements
The authors wish to thank all participants, their legal representatives and their caregivers for contributing to this study. We wish to thank Angelique Galema (secretariat, department PWO, Alliade) for administrative support, Jan Sijtsma (pharmacist, Alliade) for providing a list with medication that may have dysphagia-related side effects, Baukelina Vries (communication officer, department PWO, Alliade) for assistance with figures and tables.
Funding
This study was funded by the Department of Practice-oriented Scientific Research (PWO) of Alliade.
Author information
Authors and Affiliations
Contributions
T.S. van der Woude: Conceptualization, Methodology, Investigation, Resources, Data curation, Writing – original draft, Writing – review & editing, Project administration. R.M. Schüller-Korevaar: Conceptualization, Methodology, Investigation, Resources, Data curation, Writing – original draft, Writing – review & editing, Project administration. A.M. Ulgiati: Methodology, Software, Data curation, Writing – review & editing. G.J. Pavlis-Maldonado: Investigation, Writing – review & editing. J.H.M. Hovenkamp-Hermelink: Methodology, Formal analysis, Writing – original draft, Writing – review & editing, Supervision, Project administration. A. D. Dekker: Funding acquisition, Methodology, Resources, Writing – original draft, Writing – review & editing, Supervision, Project administration.
Corresponding author
Ethics declarations
Conflict of Interest
The authors have no conflicts of interest to declare.
Ethical Approval
The Medical Ethics Review Board of the University Medical Center Groningen concluded that the Dutch Medical Research Human Subjects Act did not apply to this study (part 1 + 2: METc 2020/35; part 3: METc 2020/252). The project has been registered in the UMCG Research Register (part 1 + 2: nr. 202000391; part 3 + 4: nr. 202100261) and has been approved by the Review and Advisory Committee Practice-oriented Scientific Research of Alliade (nr. PWO-TAC-2021-07). The study is conducted in accordance with the EU General Data Protection Regulation and the Declaration of Helsinki.
Informed Consent
Legal representatives were informed about the study with an information folder. After given consent, concordance with inclusion and exclusion criteria were double checked. To ensure sufficient diversity within the study group, differences in age, sex and level of intellectual disability were taken into account. SLTs collected data on basis of privacy by design and data minimization. Data were pseudonymized.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
van der Woude, T.S., Schüller-Korevaar, R.M., Ulgiati, A. et al. Screening Instrument for Dysphagia in People with an Intellectual Disability (SD-ID): Quick and Reliable Screening by Caregivers. J Dev Phys Disabil (2023). https://doi.org/10.1007/s10882-023-09938-0
Accepted:
Published:
DOI: https://doi.org/10.1007/s10882-023-09938-0