Abstract
The choice between radiotherapy (RT) and CO2 laser surgery (CO2-LS) for early glottic cancer remains controversial. We systematically examined electronic databases in order to identify prospective trials comparing patients who had undergone CO2-LS or RT to treat early glottic cancer. Eleven studies involving 1053 patients were included. In the selected literature, the parameter setting of CO2 laser equipment can be summarized as wavelength 10.6 µm, superpulsed mode, continuous setting, power tailored on target structures (1–3 W for subtle resections and 4–15 W for cutting a larger tumor), and approximately 2080–3900 W/cm2 of laser energy. Using RevMan 5.3, we estimated pooled odds ratios (ORs) for dichotomous variables and pooled mean differences (MDs) for continuous variables, along with associated 95% confidence intervals (CIs). The heterogeneity in the treatment variables was measured using Higgins’ inconsistency test and expressed as I2 values. The continuous variables were then depicted as histograms developed using PlotDigitizer 2.6.8. Compared to patients treated with CO2-LS, those treated with RT had better jitter (MD 1.27%, 95% CI 1.21 ~ 1.32, P < 0.001), and high scores on the “Grade (MD 6.54, 95% CI 5.31 ~ 7.76, P < 0.001), Breathiness (MD 9.08, 95% CI 4.02 ~ 14.13, P < 0.001), Asthenia (MD 2.13, 95% CI 0.29 ~ 3.98, P = 0.02), and Strain (MD 3.32, 95% CI 0.57 ~ 6.07, P = 0.02)” scale. Patients treated with CO2-LS had worse local control rates (OR 3.14, 95% CI 1.52 ~ 6.48, P = 0.002) while lower incidence of second primary tumor (OR 0.30, 95% CI 0.15 ~ 0.61, P < 0.001). It is hoped that retrospective analysis can provide suggestions for early glottis patients to choose personalized treatment.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The primary treatment for early glottic carcinoma (T1-T2) is RT or surgery. RT can achieve local control of the tumor, improve overall survival, and preserve breathing, airway integrity, and phonation [1, 2]. However, non-standardized RT can lead to recurrence in 5–35% of patients with early glottic carcinoma; this recurrence occurred mainly when the pretreatment tumor lay near dense lymph nodes and nerve tissue [3]. Patients who experience recurrence are also treated using transoral CO2-LS of the larynx, endolaryngeal cordectomy with cold instruments, or open partial laryngectomy. Although patients who undergo open partial laryngectomy experience good oncological results, this surgery is expensive, it can reduce voice quality, and it is associated with higher risk of postoperative complications [4, 5].
More recently, early glottic carcinoma has been treated using either CO2-LS or RT, since both these treatments are associated with good oncological and survival outcomes [6]. However, many patients may prefer CO2-LS over RT due to its association with minimal morbidity and high rate of laryngeal preservation, radiotherapy as the further adjuvant therapy after surgery after a [7, 8]. Furthermore, CO2-LS is considered to be a salvage treatment for recurrent laryngeal cancer after RT failure, since it can decrease the length of treatment and hospital stay, as well as reduce the incidence of side effects [9,10,11]. Nevertheless, the ongoing debate about the superior treatment for early glottic cancer continues, especially due to the lack of clinical data from prospective randomized trials.
A meta-analysis involving retrospective studies reported no significant differences between CO2-LS and RT with respect to local control of the tumor or overall survival [12]. Another study reported that transoral CO2-LS is an effective treatment for recurrent laryngeal cancer, and that is associated with high overall survival and high rates of local tumor control and larynx preservation [1]. Second meta-analysis showed that RT may be associated with longer maximum phonation time and lower fundamental frequency (f0) than laser surgery in the treatment of T1a glottic carcinoma [13].
In order to gain a better understanding of the efficacy of these two treatments, we performed a systematic review and meta-analysis of prospective trials and compared the voice quality and oncological outcomes of patients with early glottic carcinoma who underwent CO2-LS or RT. Here we assumed that CO2-LS is superior to RT on both voice quality and oncological outcomes.
Materials and methods
Search strategy
We systematically examined electronic databases, including Medline and PubMed (from 1946), Embase and OvidSP (from 1974), and the Cochrane Central Register of Controlled Trials (from 1965) in order to identify prospective trials comparing patients who had undergone CO2-LS or RT to treat early glottic cancer. The following search terms were used in combination with Boolean operators (AND or OR): “glottic cancer[All Fields],” “glottic carcinoma[All Fields],” glottic tumor[All Fields],” “vocal cord cancer[All Fields],” “vocal cord carcinoma[All Fields],” “vocal cord tumor[All Fields],” “laryngeal neoplasms[All Fields],” “larynx cancer[All Fields],” “larynx carcinoma[All Fields],” “larynx tumor[All Fields],” “laryngeal cancer[All Fields],” “laryngeal carcinoma[All Fields],” “laryngeal tumor[All Fields],” “transoral laser surgery[All Fields],” “transoral laser microsurgery[All Fields],” “transoral CO2 laser microsurgery[All Fields],” “CO2 laser cordectomy[All Fields],” “CO2 transoral microsurgery[All Fields],” “CO2 laser-assisted endoscopic surgery[All Fields],” “endoscopic resection[All Fields],” “surgery[All Fields],” “laser surgery[All Fields],” “gas lasers[All Fields],” “laser therapy[All Fields],” and “cordectomy[All Fields].” Only studies published in English before April 27, 2021, were considered. There were no restrictions based on year of publication or country of origin. All references cited in eligible publications were screened in order to ensure that relevant studies were not overlooked.
Study selection
After systematically examining the records indexed in the electronic databases, we identified studies comparing the efficacy of using CO2-LS and RT, or a combination of the two, to treat patients with early-stage glottic carcinoma according to the criteria in the original references. After excluding duplicate records, we reviewed the titles and abstracts, followed by the full text to identify prospective comparative studies for our meta-analysis. We included only studies involving patients with a confirmed diagnosis of early glottic carcinoma. The retrospective, ongoing or single-arm studies were excluded.
Data extraction
Three authors (Y. Y., Y.-L. W., and J.-X. W.) independently extracted data from included studies according to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses. Y. Y., a Ph.D. student, has been working in surgical treatment of head and neck sub-specialty for 18 years. He is well-experienced in the diagnosis and treatment of early pharyngeal cancer and CO2-LS of early vocal cord cancer. Y.-L. W., an M.D., has been working in clinical otolaryngology for 14 years. He engages in observing and evaluating voice after head and neck tumor radiation therapy, as well as collecting and analyzing clinical data. J.-X. W. has been working in clinical otolaryngology for 8 years. He is responsible for the follow-up of discharged patients and the speech function recovery of postoperative patients. We extracted data on voice quality, oncologic outcomes, and quality of life from each included study. For the purpose of this meta-analysis, we considered all patients who had undergone both CO2-LS as the intervention group, and those who had undergone RT as the control group.
In the efficacy comparisons, the primary outcome was voice quality, which included the following variables: jitter, shimmer, f0, noise/harmonic ratio, maximum phonation time, normalized noise energy, and scores on the “Grade, Roughness, Breathiness, Asthenia, and Strain” (GRBAS) scale [14]. The secondary outcomes included self-assessment of voice quality and voice-related quality of life scores, as well as oncological outcomes such as incidence of local tumor control, recurrence, second primary tumors, and death.
Selection criteria
Epidemiological studies comparing CO2-LS to RT in patients with early-stage glottic carcinoma were performed. After excluding all duplicated studies, prospective comparative studies were selected from the reading of titles and abstracts. When it was not definite whether the study would be included, the full text was screened for more detailed analysis. Studies include patients with a confirmed diagnosis of early glottic carcinoma. The intervention group was considered the patients submitted to CO2-LS and RT. The control group was considered the patients that were submitted to radiotherapy.
Data extraction
Three authors (Y. Y., Y.-L. W., and J.-X. W.) used a predefined protocol to independently identify the studies. For comparing patients undergoing CO2-LS or RT, the primary outcome was voice quality including following variables: Jitter, Shimmer, f0, noise/harmonic ratio (NHR), maximum phonation time (MPT), normalized noise energy (NNE), and GRBAS scores with Grade, Roughness, Breathiness, Asthenia, and Strain. The second outcomes included self-assessment of voice quality (VHI), voice-related quality of life (VRQOL) score, and the oncological outcomes such as incidence of local control, recurrence, death, and second primary tumors.
Quality assessment
The quality of the methodology used in the included studies was evaluated using RevMan 5.3 (RevMan; The Cochrane Collaboration, Oxford, UK). The risk of bias in the randomized trials was independently assessed by two authors (L.-Z. W. and F.-T. H.) based on previously described methods [15], which took into account random sequence generation, intervention allocation, blinding of participants, assessments of outcomes (including incomplete outcomes), and selective reporting in all included studies. L.-Z. W. has been working in clinical otolaryngology for more than 20 years. He is expert in postoperative voice function recovery work. F.-T. H has been working in clinical otolaryngology for over 5 years and is in charge of the follow-up of postoperative patients.
Power analysis
G*Power software (latest ver. 3.1.9.7; Heinrich-Heine-Universität Düsseldorf, Düsseldorf, Germany) is a free statistical software specifically designed for calculating statistical power (including sample size). In our study, G*Power software was used to calculate the statistical power of meta-analysis. For each study, the null hypothesis of equal positive proportions in two populations was tested, with a significance level (α) set as 0.05. This two-tailed test made sure that the impact can be interpreted in either direction. The statistical power of each study was calculated based on the number of proposed study groups.
Statistical analysis
Using RevMan 5.3, we estimated pooled odds ratios (ORs) for dichotomous variables and pooled mean differences (MDs) for continuous variables, along with associated 95% confidence intervals (CIs). The heterogeneity in the treatment variables was measured using Higgins’ inconsistency test and expressed as I2 values: An I2 value of 25% indicated low heterogeneity, 50% indicated moderate heterogeneity, and 75% indicated high heterogeneity. We used the inverse-variance fixed effects model for outcomes showing low heterogeneity (< 25%), and the DerSimonian and Laird random effects model for outcomes showing moderate to high heterogeneity (> 50%). We estimated means and standard deviations for continuous variables that were published as medians and interquartile ranges using an online tool (http://www.comp.hkbu.edu.hk/~xwan/median2mean.html) and previously established methods [16, 17]. The continuous variables were then depicted as histograms developed using PlotDigitizer 2.6.8 (version of 27 October 2015, Sun Microsystems, Philippe Zeller, French). P < 0.05 was set as the level of significance.
Results
Search strategy
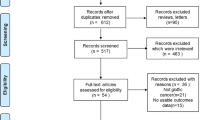
A total of 2806 studies were identified from the databases examined (Fig. 1). After removing duplicates and reviewing the titles and abstracts of the remaining studies, 23 prospective comparative studies were retained for the full-text analysis. After considering the eligibility criteria, eleven unique studies involving 1053 patients were included in the final meta-analysis.
We excluded a total of 13 studies: four ongoing protocols, four studies involving patients with superficial benign lesions, one study using hematoxylin–eosin staining, one prospective single-arm trail, one study involving patients with recurrent respiratory papillomas, one study where patients received interventions related to phonatory compensation mechanisms after CO2-LS, and one study where margin excisions were performed during transoral laser microsurgery (Fig. 1).
Characteristics of included studies
Of the eleven studies included [11, 14, 18,19,20,21,22,23,24,25,26], nine studies [11, 19,20,21,22,23,24,25,26] were prospective comparative or cohort studies, while the other two were randomized, parallel-group studies [14, 18] (Table 1). The effect of CO2-LS treatment was compared to full-dose radiotherapy in four studies [19, 21, 23, 26], to 2 Gy/d radiotherapy in two other studies [14, 22], and to 225 cGy/session radiotherapy in two other studies [11, 24]. The other studies [18, 20, 25] compared CO2-LS treatment with 6-MV or 60Co photon treatment, or to 225 cGy/d and 2.5 Gy/fraction radiotherapy. Patient follow-up was > 24 months in all included studies.
Quality assessment
Only one study [14] described the method of random sequence generation with low selection bias. Six studies [14, 20, 22, 23, 25, 26] reported the method used for allocation concealment. Unfortunately, there were no studies demonstrated how they blinded the participants and the outcome assessments. Almost all included studies, except one, showed the high risk of attrition [11] and reporting bias [19], respectively. Other bias was considered low in all included studies (Fig. 2).
Voice quality assessment
A pooled analysis based on data from four studies [20, 24,25,26] showed that patients who had undergone RT had lower jitter scores (MD 1.27, 95% CI 1.21 to 1.32, P < 0.001; Fig. 3A) than those who had undergone CO2-LS. There were no significant differences in shimmer score (Fig. 3B), f0 values (Fig. 3C) based on data from four studies [20, 24,25,26], or NNE (Fig. 3D) based on data from two studies [20, 24]. There was only one study that reported the results of NHR [25] and MPT [24], respectively, and found that patients treated with RT showed lower NHR and MPT compared to those treated with CO2-LS. The GRBAS scale was used to conduct an auditory-perceptual evaluation. A total of four studies [14, 23, 24, 26] reported that RT was associated with significantly higher Grade scores than CO2-LS (MD 6.54, 95% CI 5.31 to 7.76, P < 0.001; Fig. 4A). Similarly, RT was associated with high scores for Breathiness (3 studies, 169 patients; MD 9.08, 95% CI 4.02 to 14.13, P < 0.001; Fig. 4C), Asthenia (3 studies, 133 patients; MD 2.13, 95% CI 0.29 to 3.98, P = 0.02; Fig. 4D), and Strain (3 studies, 133 patients; MD 3.32, 95% CI 0.57 to 6.07, P = 0.02; Fig. 4E). However, there were no significant differences in roughness (Fig. 4B) based on data from two studies [14, 24].
Life quality assessment
Only one study [23] included in this meta-analysis reported results related to self-assessment of voice quality and voice-related quality of life scores. Another study [21] found that CO2-LS resulted in less likely to be understood all the time (Performance Status Scale for Head and Neck Cancer Patients: understandability score 100; OR = 12.2; P = 0.03) and a higher likelihood of having a VHI-10 score of 10 or more (OR = 16.2; P = 0.001). Nevertheless, Taylor et al. [19] also reported that VHI-10 ranged from 0 to 11 (median 6) in the CO2-LS group and 0 to 34 (median 7) in the RT group during the last work up. Hence, patients treated with RT reported better self-assessment of voice quality, while those treated with CO2-LS reported better voice-related quality of life.
Oncological outcomes
Based on data from six studies [11, 14, 19, 20, 22, 25], there were no significant differences in recurrence rates between patients treated with CO2-LS or RT (P = 0.54; Fig. 5A). Pooled analysis showed that patients treated with RT had lower incidence of local tumor control (MD 3.14, 95% CI 1.52 to 6.48, P = 0.002; Fig. 5B) but increased the risk of second primary tumors (MD 0.30, 95% CI 0.15 to 0.61, P < 0.001; Fig. 5D) than those treated with CO2-LS. No statistical differences were observed between the two groups in the incidence of death (P = 0.11; Fig. 5C).
Power analysis
As shown in Table 2, there were the results of pooled risk for voice quality when CO2-LS versus RT. In the meta-analysis of jitter scores, 3 of 4 studies [24,25,26] achieved 80% power. As for the shipper score, only 1 of 4 studies [26] achieved 80% power. In the meta-analysis of f0 values, 2 out of 4 studies [25, 26] achieved 80% power. The power of 2 studies [20, 24] in NNE’s meta-analysis did not exceed 80%.
The results of pooled risk for GRBAS when CO2-LS versus RT are shown in Table 3. In the meta-analysis of Grade scores, 5 out of 6 studies [14, 24, 26, 27 (1) and (2)] achieved 80% efficacy. As for Roughness, the power of 2 studies [14, 24] did not reach 80%. In the meta-analysis of scores for Breathiness, 4 studies [14, 25, 27 (1) and (2)] all achieved 80% power. In Asthenia’s meta-analysis, 2 out of 3 studies [14, 26] achieved 80% power. Only 1 out of 3 studies in the meta-analysis of Strong [26] achieved 80% power.
Discussion
In this meta-analysis, we aimed to compare the efficacy of CO2-LS or RT for treating patients with early glottic carcinoma. The collected data showed that patients treated with CO2-LS had a better quality of life and were able to achieve local control of the tumor than those treated with RT. However, patients treated with RT had better overall voice quality, reflected in lower jitter, shimmer, and f0, as well as lower noise/harmonic ratios and GRBAS scores. These findings indicate that CO2-LS is associated with better local control rates and quality of life for patients with early glottic cancer.
Although total laryngectomy was previously considered the primary treatment for recurrent laryngeal cancer after RT [22, 23], it is associated with high incidence of postoperative complications, so more radical and invasive procedures are needed. CO2-LS has many advantages over total laryngectomy, including precise cutting, bloodless operation, short operation time and hospital stay, reduced cost of hospitalization, and decreased recurrence rates [24,25,26]. Therefore, CO2-LS has recently begun to be used as a salvage surgery for patients with recurrent early glottic carcinoma. A treatment goal for patients with early glottic cancer is maintaining and improving voice quality. Some studies reported no differences in voice quality after RT or CO2-LS, while others reported better voice quality after RT [13, 27, 28]. RT can allow more precise, local treatment at the tumor location and reduce damage to normal cells, which is crucial for maintaining normal glottis function [29,30,31]. This may help explain the higher voice quality after RT than after CO2-LS in our study, and also reflects the one-sidedness of the assumptions in the “Introduction” section. On the other hand, patients in our analysis showed higher voice-related quality of life scores after CO2-LS than after RT. This may reflect that the procedure was associated with shorter operation time, shorter hospital stay, lower hospitalization costs, and lower recurrence rates than RT.
Oncological results are the main outcomes used to evaluate the treatment of cancer. In a retrospective study [32], revision transoral LS is confirmed the oncological radicality in most cases, even in the case of positive, close, or non-evaluable margins. One study reported high 5-year rates of 75–84% for local tumor control, overall laryngeal preservation, overall survival, and disease-specific survival after CO2-LS [33]. Other studies showed similar rates of local tumor control with CO2-LS or RT [34, 35]. The pooled results of prospective studies in the present meta-analysis showed that CO2-LS was associated with better local control rates than RT, but the two techniques were associated with similar rates of recurrence, death, and second primary tumors.
As far as we know, this is the first meta-analysis to include prospective comparative trials and exclude all retrospective studies. Furthermore, we objectively analyzed oncologic outcomes, as well as voice and life quality after treatment with CO2-LS and RT in a total of 826 participants. Our findings suggest that both CO2-LS and RT are excellent options for the treatment of patients with early glottic cancer. Although patients treated with CO2-LS may have better local control rates and quality of life, those treated with RT may have superior voice quality. Therefore, clinicians should consider each patient’s situation before recommending treatment with CO2-LS or RT. Further large, high-quality, double-blind, prospective controlled trials are needed in order to gain a better understanding of the efficacy of both treatments.
Meta-analysis is a statistical method that combines multiple homogeneous studies on the same topic using quantitative methods to obtain overall results. It can conduct a significance test to analyze whether the interventions and exposures are meaningful or not. Therefore, ensuring the statistical power of the study is crucial. We calculated the statistical efficiency of this meta-analysis. Since there were 1–2 studies with a statistical power less than 80% in each meta-analysis, it indicated that the statistical efficiency of meta-analysis in this study needed to be improved.
Conclusion
Neither CO2-LS nor RT can solve all the problems in the treatment of patients with early glottic cancer patients. Although patients treated with CO2-LS had significant better local control rates and quality of life, those treated with RT should be associated with recovery of voice quality. Therefore, clinicians must consider the specific situation of the individual with early glottic cancer before recommending treatment with more comprehensive and cautious to apply CO2-LS or RT for early glottic cancer patients according to the specific situation of the individual.
References
Zhong A, Xu X, Fan H, Wang L, Niu Y (2015) Transoral laser microsurgery for recurrent laryngeal carcinoma after primary treatment: a systematic review and meta.analysis. J Cancer Res Ther 11:173–178
Guimarães AV, Dedivitis RA, Matos LL, Aires FT, Cernea CR (2018) Comparison between transoral laser surgery and radiotherapy in the treatment of early glottic cancer: a systematic review and meta-analysis. Sci Rep 8:11900
Holsinger FC, Kies MS, Diaz EM Jr, Gillenwater AM, Lewin JS, Ginsberg LE, Glisson BS, Garden AS, Ark N, Lin HY, Lee JJ, El-Naggar AK, Hong WK, Shin DM, Khuri FR (2009) Durable long-term remission with chemotherapy alone for stage II to IV laryngeal cancer. J Clin Oncol 27:1976–1982
Lester SE, Rigby MH, Taylor SM (2011) Transoral laser microsurgery outcomes with early glottic cancer: the Dalhousie University experience. J Laryngol Otol 125:509–512
Warner L, Chudasama J, Kelly CG, Loughran S, McKenzie K, Wight R, Dey P (2014) Radiotherapy versus open surgery versus endolaryngeal surgery (with or without laser) for early laryngeal squamous cell cancer. Cochrane Database Syst Rev 2014:CD002027
Cabrera-Sarmiento JA, Vázquez-Barro JC, González-Botas JH, Chiesa-Estomba C, Mayo-Yáñez M (2021) T1b glottic tumor and anterior commissure involvement: Is the transoral CO2 laser microsurgery a safe option? Ear Nose Throat J 100:68S-72S
Vander Pooreleven V, Meulemans J, Van Lierde C, Nuyts S, Delaere P (2021) Current indications for adjuvant treatment following transoral laser microsurgery of early intermediate laryngeal cancer. Curr Opin Otolaryngol Head Neck Surg 29:79–85
Song W, Caffier F, Nawka T, Ermakova T, Martin A, Mürbe D, Caffier PP (2021) T1a glottic cancer: advances in vocal outcome assessment after transoral CO2-laser microsurgery using the VEM. J Clin Med 10:1250
Chien P-J, Hung L-T, Wang L-W, Yang M-H, Chu P-Y (2021) Oncologic results and quality of life in patients with T3 glottic cancer after transoral laser microsurgery. Eur Arch Otorhinolaryngol 278:2983–2992
Campo F, Zocchi J, Ralli M, De Seta D, Russo FY, Angeletti D, Minni A, Greco A, Pellini R, de Vincentiis M (2021) Laser microsurgery versus radiotherapy versus open partial laryngectomy for T2 laryngeal carcinoma: a systematic review of oncological outcomes. Ear Nose Throat J 100:51S-58S
Lois-Ortega Y, García-Curdi F, Sebastián-Cortés JM, De Miguel-García F, Vallés-Varela H, Campo AM-D (2020) Radiotherapy versus laser microsurgery in the treatment of early glottic cancer. Acta Otolaryngol 140:954–958
Dey P, Arnold D, Wight R, MacKenzie K, Kelly C, Wilson J (2002) Radiotherapy versus open surgery versus endolaryngeal surgery (with or without laser) for early laryngeal squamous cell cancer. Cochrane Database Syst Rev 2:CD002027
Huang G, Luo M, Zhang J, Liu H (2017) The voice quality after laser surgery versus radiotherapy of T1a glottic carcinoma: systematic review and meta-analysis. OncoTargets Ther 10:2403–2410
Aaltonen LM, Rautiainen N, Sellman J, Saarilahti K, Mäkitie A, Rihkanen H, Laranne J, Kleemola L, Wigren T, Sala E, Lindholm P, Grenman R, Joensuu H (2014) Voice quality after treatment of early vocal cord cancer: a randomized trial comparing laser surgery with radiation therapy. Int J Radiat Oncol Biol Phys 90:255–260
Yu M-G, **g R, Mo Y-J, Lin F, Du X-K, Ge W-Y, Dai H-J, Hu Z-K, Zhang S-S, Pan L-H (2019) Non-intubated anesthesia in patients undergoing video-assisted thoracoscopic surgery: a systematic review and meta-analysis. PLoS one 14:e0224737
Luo D, Wan X, Liu J, Tong T (2018) Optimally estimating the sample mean from the sample size, median, mid-range, and/or mid-quartile range. Stat Meth Med Res 27:1785–1805
Wan X, Wang W, Liu J, Tong T (2014) Estimating the sample mean and standard deviation from the sample size, median, range and/or interquartile range. BMC Med Res Methodol 14:135
Zhang Y, Wang B, Sun G, Zhang G, Lu L, Liang G (2018) Carbon dioxide laser microsurgery versus low-temperature plasma radiofrequency ablation for T1a glottic cancer: a single-blind randomized clinical trial. Biomed Res Int 2018:4295960
Taylor SM, Kerr P, Fung K, Aneeshkumar MK, Wilke D, Jiang Y, Scott J, Phillips J, Hart RD, Trites JRB, Rigby MH (2013) Treatment of T1b glottic SCC: laser vs. radiation–a Canadian multicenter study. J Otolaryngol Head Neck Surg 42:22
Van Gogh CDL, Verdonck-De Leeuw IM, Wedler-Peeters J, Langendijk JA, Mahieu HF (2012) Prospective evaluation of voice outcome during the first two years in male patients treated by radiotherapy or laser surgery for T1a glottic carcinoma. Eur Arch Otorhinolaryngol 269:1647–1652
Kujath M, Kerr P, Myers C, Bammeke F, Lambert P, Cooke A, Sutherland D (2011) Functional outcomes and laryngectomy-free survival after transoral CO2 laser microsurgery for stage 1 and 2 glottic carcinoma. J Otolaryngol Head Neck Surg 40:S49–S58
Mahler V, Boysen M, Brøndbo K (2010) Radiotherapy or CO2 laser surgery as treatment of T(1a) glottic carcinoma? Eur Arch Otorhinolaryngol 267:743–750
Oridate N, Homma A, Suzuki S, Nakamaru Y, Suzuki F, Hatakeyama H, Taki S, Sakashita T, Nishizawa N, Furuta Y, Fukuda S (2009) Voice-related quality of life after treatment of laryngeal cancer. Arch Otolaryngol Head Neck Surg 135:363–368
Núñez Batalla F, Caminero Cueva MJ, Señaris González B, LlorentePendás JL, Gorriz Gil C, Llames AL, Alonso Pantiga R, Suárez Nieto C (2008) Voice quality after endoscopic laser surgery and radiotherapy for early glottic cancer: objective measurements emphasizing the Voice Handicap Index. Eur Arch Otorhinolaryngol 265:543–548
Krengli M, Policarpo M, Manfredda I, Aluffi P, Gambaro G, Panella M, Pia F (2004) Voice quality after treatment for T1a glottic carcinoma–radiotherapy versus laser cordectomy. Acta Oncol 43:284–289
Rydell R, Schalén L, Fex S, Elner A (1995) Voice evaluation before and after laser excision vs. radiotherapy of T1A glottic carcinoma. Acta Otolaryngol 115:560–565
Kim JH, Kim WS, Koh YW, Kim S-H, Byeon HK, Choi EC (2018) Oncologic and functional outcomes of salvage supracricoid partial laryngectomy. Acta Otolaryngol 138:1117–1122
Bertolin A, Lionello M, Zanotti C, Franz L, Giacomelli L, Rizzotto G, Marioni G (2021) Oncological and functional outcomes of primary and salvage total Laryngectomy. Laryngoscope 131:E569–E575
Hendriksma M, van Loon Y, Klop WMC, Hakkesteegt MM, Heijnen BJ, El Hasnaoui I, de Jong M, Langeveld TPM, van Benthem PPG, de Jong RJB, Sjögren EV (2019) Quality of life and voice outcome of patients treated with transoral CO2 laser microsurgery for early glottic carcinoma (T1–T2): a 2-year follow-up study. Eur Arch Otorhinolaryngol 276:805–814
Strieth S, Ernst BP, Both I, Hirth D, Pfisterer LN, Künzel J, Eder K (2019) Randomized controlled single-blinded clinical trial of functional voice outcome after vascular targeting KTP laser microsurgery of early laryngeal cancer. Head Neck 41:899–907
Luo C, Lv K, Liu Q, Wen Y, Lin M, Wang Z, Zhu X, Jiang A, Wen W, Lei W (2021) Comparison of laser microsurgery and open partial laryngectomy for T1–2 laryngeal cancer treatment. Ann Transl Med 9:464
Caudell JJ, Torres-Roca JF, Gillies RJ, Enderling H, Kim S, Rishi A, Moros EG, Harrison LB (2017) The future of personalised radiotherapy for head and neck cancer. Lancet Oncol 18:e266–e273
Pollard JM, Wen Z, Sadagopan R, Wang J, Ibbott GS (2017) The future of image-guided radiotherapy will be MR guided. Br J Radiol 90:20160667
Saraniti C, Montana F, Chianetta E, Greco G, Verro B (2022) Impact of resection margin status and revision transoral laser microsurgery in early glottic cancer: analysis of organ preservation and local disease control on a cohort of 153 patients. Braz J Otorhinolaryngol 88:669–674
Abshire D, Lang MK (2018) The evolution of radiation therapy in treating cancer. Semin Oncol Nurs 34:151–157
Funding
Self-funded by the authors for a literature review.
Author information
Authors and Affiliations
Contributions
Guang-wu Huang designed and directed the overall study. Yong Yang carried out literature searches, drafted, revised, and approved the manuscript. Yong-li Wang and Ju-xin Wang participated in data analysis. Li-zhi Wei and Fang-ting Huang sorted data and assessed the included trials for quality.
Corresponding author
Ethics declarations
Ethical approval
Non applicable.
Informed consent
Non applicable.
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Yang, Y., Wang, Yl., Wei, Lz. et al. Is CO2 laser microsurgery better than radiotherapy in early glottic cancer: a meta-analysis. Lasers Med Sci 38, 223 (2023). https://doi.org/10.1007/s10103-023-03890-3
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s10103-023-03890-3