Abstract
Purpose
Staphylococcus aureus is one of the most common pathogens causing bloodstream infection. A rapid characterisation of resistance to methicillin and, occasionally, to aminoglycosides for particular indications, is therefore crucial to quickly adapt the treatment and improve the clinical outcomes of septic patients. Among analytical technologies, targeted liquid chromatography-tandem mass spectrometry (LC-MS/MS) has emerged as a promising tool to detect resistance mechanisms in clinical samples.
Methods
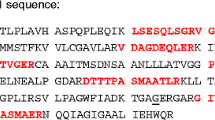
A rapid proteomic method was developed to detect and quantify the most clinically relevant antimicrobial resistance effectors in S. aureus in the context of sepsis: PBP2a, PBP2c, APH(3’)-III, ANT(4’)-I, and AAC(6’)-APH(2’’), directly from positive blood cultures and in less than 70 min including a 30-min cefoxitin-induction step. The method was tested on spiked blood culture bottles inoculated with 124 S.aureus, accounting for the known genomic diversity of SCCmec types and the genetic background of the strains.
Results
This method provided 99% agreement for PBP2a (n = 98/99 strains) detection. Agreement was 100% for PBP2c (n = 5/5), APH(3’)-III (n = 16/16), and ANT(4’)-I (n = 20/20), and 94% for AAC(6')-APH(2'') (n = 16/17). Across the entire strain collection, 100% negative agreement was reported for each of the 5 resistance proteins. Additionally, relative quantification of ANT(4’)-I expression allowed to discriminate kanamycin-susceptible and -resistant strains, in all strains harbouring the ant(4’)-Ia gene.
Conclusion
The LC-MS/MS method presented herein demonstrates its ability to provide a reliable determination of S. aureus resistance mechanisms, directly from positive blood cultures and in a short turnaround time, as required in clinical laboratories.





Similar content being viewed by others
Data availability
MRM raw data and transition lists are available via PASSEL with the accession number PASS05841 (https://db.systemsbiology.net/sbeams/cgi/PeptideAtlas/PASS_View). The 124 S.aureus genomes are available on ENA (accession numbers in Supplementary Table 1).
References
Wisplinghoff H, Bischoff T, Tallent SM, Seifert H, Wenzel RP, Edmond MB (2004) Nosocomial bloodstream infections in US hospitals: analysis of 24,179 cases from a prospective nationwide surveillance study. Clin Infect Dis 39:309–317. https://doi.org/10.1086/421946
Yaw LK, Robinson JO, Ho KM (2014) A comparison of long-term outcomes after meticillin-resistant and meticillin-sensitive Staphylococcus aureus bacteraemia: an observational cohort study. Lancet Infect Dis 14:967–975. https://doi.org/10.1016/S1473-3099(14)70876-X
Joo E-J, Park DA, Kang C-I, Chung DR, Song J-H, Lee SM, Peck KR (2019) Reevaluation of the impact of methicillin-resistance on outcomes in patients with Staphylococcus aureus bacteremia and endocarditis. Korean J Intern Med 34:1347–1362. https://doi.org/10.3904/kjim.2017.098
Reynolds PE, Brown DFJ (1985) Penicillin-binding proteins of β-lactam-resistant strains of Staphylococcus aureus. FEBS Lett 192:28–32. https://doi.org/10.1016/0014-5793(85)80036-3
Hartman BJ, Tomasz A (1984) Low-affinity penicillin-binding protein associated with beta-lactam resistance in Staphylococcus aureus. J Bacteriol 158:513–516
Lim D, Strynadka NCJ (2002) Structural basis for the beta lactam resistance of PBP2a from methicillin-resistant Staphylococcus aureus. Nat Struct Biol 9:870–876. https://doi.org/10.1038/nsb858
García-Álvarez L, Holden MTG, Lindsay H, Webb CR, Brown DFJ, Curran MD, Walpole E, Brooks K, Pickard DJ, Teale C, Parkhill J, Bentley SD et al (2011) Meticillin-resistant Staphylococcus aureus with a novel mecA homologue in human and bovine populations in the UK and Denmark: a descriptive study. Lancet Infect Dis 11:595–603. https://doi.org/10.1016/S1473-3099(11)70126-8
Lakhundi S, Zhang K (2018) Methicillin-resistant staphylococcus aureus: molecular characterization, evolution, and epidemiology. Clin Microbiol Rev 31:e00020-e118. https://doi.org/10.1128/CMR.00020-18
Wolska-Gębarzewska M, Międzobrodzki J, Kosecka-Strojek M (2023) Current types of staphylococcal cassette chromosome mec (SCCmec) in clinically relevant coagulase-negative staphylococcal (CoNS) species. Crit Rev Microbiol 0:1–17. https://doi.org/10.1080/1040841X.2023.2274841
Garau J, Bouza E, Chastre J, Gudiol F, Harbarth S (2009) Management of methicillin-resistant Staphylococcus aureus infections. Clin Microbiol Infect 15:125–136. https://doi.org/10.1111/j.1469-0691.2009.02701.x
Delgado V, Ajmone Marsan N, de Waha S, Bonaros N, Brida M, Burri H, Caselli S, Doenst T, Ederhy S, Erba PA, Foldager D, Fosbøl EL et al (2023) 2023 ESC Guidelines for the management of endocarditis: Developed by the task force on the management of endocarditis of the European Society of Cardiology (ESC) Endorsed by the European Association for Cardio-Thoracic Surgery (EACTS) and the European Association of Nuclear Medicine (EANM). Eur Heart J 44:3948–4042. https://doi.org/10.1093/eurheartj/ehad193
Rahimi F (2016) Characterization of resistance to aminoglycosides in methicillin-resistant staphylococcus aureus strains isolated from a tertiary care hospital in Tehran, Iran. Jundishapur J Microbiol 9:e29237. https://doi.org/10.5812/jjm.29237
Liakopoulos A, Foka A, Vourli S, Zerva L, Tsiapara F, Protonotariou E, Dailiana Z, Economou M, Papoutsidou E, Koutsia-Carouzou C, Anastassiou ED, Diza E et al (2011) Aminoglycoside-resistant staphylococci in Greece: prevalence and resistance mechanisms. Eur J Clin Microbiol Infect Dis 30:701–705. https://doi.org/10.1007/s10096-010-1132-7
Schmitz F-J, Fluit AC, Gondolf M, Beyrau R, Lindenlauf E, Verhoef J, Heinz H-P, Jones ME (1999) The prevalence of aminoglycoside resistance and corresponding resistance genes in clinical isolates of staphylococci from 19 European hospitals. J Antimicrob Chemother 43:253–259. https://doi.org/10.1093/jac/43.2.253
Khosravi AD, Jenabi A, Montazeri EA (2017) Distribution of genes encoding resistance to aminoglycoside modifying enzymes in methicillin-resistant Staphylococcus aureus (MRSA) strains. Kaohsiung J Med Sci 33:587–593. https://doi.org/10.1016/j.kjms.2017.08.001
Yao C-J, Li Y-L, Pu M-J, Luo L-H, **ong Q, **e F-J, Li T-L, Feng P-M (2021) Aminoglycosides with anti-MRSA activity: a concise review. Curr Top Med Chem 21:2483–2499. https://doi.org/10.2174/1568026621666211004093647
Timbrook TT, Morton JB, McConeghy KW, Caffrey AR, Mylonakis E, LaPlante KL (2017) The effect of molecular rapid diagnostic testing on clinical outcomes in bloodstream infections: a systematic review and meta-analysis. Clin Infect Dis 64:15–23. https://doi.org/10.1093/cid/ciw649
Kumar A, Ellis P, Arabi Y, Roberts D, Light B, Parrillo JE, Dodek P, Wood G, Kumar A, Simon D, Peters C, Ahsan M et al (2009) Initiation of inappropriate antimicrobial therapy results in a fivefold reduction of survival in human septic shock. Chest 136:1237–1248. https://doi.org/10.1378/chest.09-0087
Seymour CW, Gesten F, Prescott HC, Friedrich ME, Iwashyna TJ, Phillips GS, Lemeshow S, Osborn T, Terry KM, Levy MM (2017) Time to treatment and mortality during mandated emergency care for sepsis. N Engl J Med 376:2235–2244. https://doi.org/10.1056/NEJMoa1703058
Ohnuma T, Chihara S, Costin B, Treggiari MM, Bartz RR, Raghunathan K, Krishnamoorthy V (2023) Association of appropriate empirical antimicrobial therapy with in-hospital mortality in patients with bloodstream infections in the US. JAMA Netw Open 6:e2249353. https://doi.org/10.1001/jamanetworkopen.2022.49353
Rhoads DD, Wang H, Karichu J, Richter SS (2016) The presence of a single MALDI-TOF mass spectral peak predicts methicillin resistance in staphylococci. Diagn Microbiol Infect Dis 86:257–261. https://doi.org/10.1016/j.diagmicrobio.2016.08.001
Tang W, Ranganathan N, Shahrezaei V, Larrouy-Maumus G (2019) MALDI-TOF mass spectrometry on intact bacteria combined with a refined analysis framework allows accurate classification of MSSA and MRSA. PLoS ONE 14:e0218951. https://doi.org/10.1371/journal.pone.0218951
Yu J, Tien N, Liu Y-C, Cho D-Y, Chen J-W, Tsai Y-T, Huang Y-C, Chao H-J, Chen C-J (2022) Rapid Identification of methicillin-resistant staphylococcus aureus Using MALDI-TOF MS and machine learning from over 20,000 clinical isolates. Microbiol Spectr 10:e00483-e522. https://doi.org/10.1128/spectrum.00483-22
Neil JR, Verma A, Kronewitter SR, McGee WM, Mullen C, Viirtola M, Kotovuori A, Friedrich H, Finell J, Rannisto J, Syka JEP, Stephenson JL (2021) Rapid MRSA detection via tandem mass spectrometry of the intact 80 kDa PBP2a resistance protein. Sci Rep 11:18309. https://doi.org/10.1038/s41598-021-97844-w
Sanchini A (2022) Recent developments in phenotypic and molecular diagnostic methods for antimicrobial resistance detection in staphylococcus aureus: a narrative review. Diagnostics 12:208. https://doi.org/10.3390/diagnostics12010208
Burrack-Lange SC, Personne Y, Huber M, Winkler E, Weile J, Knabbe C, Görig J, Rohde H (2018) Multicenter assessment of the rapid Unyvero Blood Culture molecular assay. J Med Microbiol 67:1294–1301. https://doi.org/10.1099/jmm.0.000804
Wang H, Drake SK, Youn J-H, Rosenberg AZ, Chen Y, Gucek M, Suffredini AF, Dekker JP (2017) Peptide markers for rapid detection of KPC carbapenemase by LC-MS/MS. Sci Rep 7:2531. https://doi.org/10.1038/s41598-017-02749-2
Wang H, Chen Y, Strich JR, Drake SK, Youn J-H, Rosenberg AZ, Gucek M, McGann PT, Suffredini AF, Dekker JP (2019) Rapid detection of colistin resistance protein MCR-1 by LC–MS/MS. Clin Proteomics 16:8. https://doi.org/10.1186/s12014-019-9228-2
Foudraine DE, Dekker LJM, Strepis N, Nispeling SJ, Raaphorst MN, Kloezen W, Colle P, Verbon A, Klaassen CHW, Luider TM, Goessens WHF (2022) Using targeted liquid chromatography-tandem mass spectrometry to rapidly detect β-Lactam, aminoglycoside, and fluoroquinolone resistance mechanisms in blood cultures growing E. coli or K. pneumoniae. Front Microbiol 13:887420. https://doi.org/10.3389/fmicb.2022.887420
Foudraine DE, Aarents CNM, Wattel AA, van Boxtel R, Strepis N, Ten Kate MT, Verbon A, Luider TM, Klaassen CHW, Hays J, Dekker LJM, Tommassen J et al (2022) Liquid chromatography-tandem mass spectrometry analysis demonstrates a decrease in Porins and increase in CMY-2 β-Lactamases in Escherichia coli exposed to increasing concentrations of Meropenem. Front Microbiol 13:793738. https://doi.org/10.3389/fmicb.2022.793738
Foudraine DE, Strepis N, Klaassen CHW, Raaphorst MN, Verbon A, Luider TM, Goessens WHF, Dekker LJM (2021) Rapid and accurate detection of aminoglycoside-modifying enzymes and 16S rRNA methyltransferases by targeted liquid chromatography-tandem mass spectrometry. J Clin Microbiol 59:e0046421. https://doi.org/10.1128/JCM.00464-21
Foudraine DE, Strepis N, Stingl C, ten Kate MT, Verbon A, Klaassen CHW, Goessens WHF, Luider TM, Dekker LJM (2021) Exploring antimicrobial resistance to beta-lactams, aminoglycosides and fluoroquinolones in E. coli and K. pneumoniae using proteogenomics. Sci Rep 11:12472. https://doi.org/10.1038/s41598-021-91905-w
Foudraine DE, Dekker LJM, Strepis N, Bexkens ML, Klaassen CHW, Luider TM, Goessens WHF (2019) Accurate detection of the four most prevalent Carbapenemases in E. coli and K. pneumoniae by high-resolution mass spectrometry. Front Microbiol 10. https://www.frontiersin.org/articles/10.3389/fmicb.2019.02760
Strich JR, Wang H, Cissé OH, Youn J-H, Drake SK, Chen Y, Rosenberg AZ, Gucek M, McGann PT, Dekker JP, Suffredini AF (2019) Identification of the OXA-48 Carbapenemase family by use of tryptic peptides and liquid chromatography-tandem mass spectrometry. J Clin Microbiol 57:e01240-18. https://doi.org/10.1128/JCM.01240-18
Charretier Y, Dauwalder O, Franceschi C, Degout-Charmette E, Zambardi G, Cecchini T, Bardet C, Lacoux X, Dufour P, Veron L, Rostaing H, Lanet V et al (2015) Rapid bacterial identification, resistance, virulence and type profiling using selected reaction monitoring mass spectrometry. Sci Rep 5:13944. https://doi.org/10.1038/srep13944
Cecchini T, Yoon E-J, Charretier Y, Bardet C, Beaulieu C, Lacoux X, Docquier J-D, Lemoine J, Courvalin P, Grillot-Courvalin C, Charrier J-P (2018) Deciphering multifactorial resistance phenotypes in Acinetobacter baumannii by genomics and targeted label-free proteomics. Mol Cell Proteomics 17:442–456. https://doi.org/10.1074/mcp.RA117.000107
Karlsson R, Thorsell A, Gomila M, Salvà-Serra F, Jakobsson HE, Gonzales-Siles L, Jaén-Luchoro D, Skovbjerg S, Fuchs J, Karlsson A, Boulund F, Johnning A et al (2020) Discovery of species-unique peptide biomarkers of bacterial pathogens by tandem mass spectrometry-based proteoty** *. Mol Cell Proteomics 19:518–528. https://doi.org/10.1074/mcp.RA119.001667
Deforet F, Jehanne Q, Bénéjat L, Aptel J, Prat R, Desbiolles C, Ducournau A, Jauvain M, Bonnet R, Vandenesch F, Lemoine J, Lehours P (2023) Combined genomic-proteomic approach in the identification of Campylobacter coli amoxicillin-clavulanic acid resistance mechanism in clinical isolates. Front Microbiol 14. https://www.frontiersin.org/articles/10.3389/fmicb.2023.1285236
Carrière R, Rasigade J-P, Vandenesch F, Robin F, Lemoine J (2023) ECCMID 2023 - Correlation between porin expression and ertapenem resistance in K. pneumoniae using proteomics, abstr P-0548. ECCMID 2023
Cecchini T, Carrière R, Desbiolles C, Prat R, Wreyford L, Deforet F, Gregson M, L’Aour Dufour P, Macavei I, Peyrache E, Arquier D, Carvalho G et al (2023) ECCMID 2023 - Move aside genomics: using proteomics for rapid sepsis diagnosis, abstr P-0506. ECCMID 2023
Fournier D, Carrière R, Bour M, Grisot E, Triponney P, Muller C, Lemoine J, Jeannot K, Plésiat P (2021) Mechanisms of resistance to Ceftolozane/Tazobactam in Pseudomonas aeruginosa: results of the GERPA multicenter study. Antimicrob Agents Chemother 65:e01117-e1120. https://doi.org/10.1128/AAC.01117-20
Petit RA, Read TD (2018) Staphylococcus aureus viewed from the perspective of 40,000+ genomes. PeerJ 6:e5261. https://doi.org/10.7717/peerj.5261
MacLean B, Tomazela DM, Shulman N, Chambers M, Finney GL, Frewen B, Kern R, Tabb DL, Liebler DC, MacCoss MJ (2010) Skyline: an open source document editor for creating and analyzing targeted proteomics experiments. Bioinformatics 26:966–968. https://doi.org/10.1093/bioinformatics/btq054
Gurdeep Singh R, Tanca A, Palomba A, Van der Jeugt F, Verschaffelt P, Uzzau S, Martens L, Dawyndt P, Mesuere B (2019) Unipept 4.0: functional analysis of metaproteome data. J Proteome Res 18:606–615. https://doi.org/10.1021/acs.jproteome.8b00716
Pivard M, Bastien S, Macavei I, Mouton N, Rasigade J-P, Couzon F, Youenou B, Tristan A, Carrière R, Moreau K, Lemoine J, Vandenesch F (2023) Targeted proteomics links virulence factor expression with clinical severity in staphylococcal pneumonia. Front Cell Infect Microbiol 13:1162617. https://doi.org/10.3389/fcimb.2023.1162617
McKinney TK, Sharma VK, Craig WA, Archer GL (2001) Transcription of the gene mediating methicillin resistance in staphylococcus aureus(mecA) is corepressed but not coinduced by CognatemecA and β-lactamase regulators. J Bacteriol 183:6862–6868. https://doi.org/10.1128/JB.183.23.6862-6868.2001
Dupieux C, Bouchiat C, Larsen AR, Pichon B, Holmes M, Teale C, Edwards G, Hill R, Decousser J-W, Trouillet-Assant S, Petersen A, Skov R et al (2017) Detection of mecC-Positive Staphylococcus aureus: what to expect from immunological tests targeting PBP2a? J Clin Microbiol 55:1961–1963. https://doi.org/10.1128/JCM.00068-17
Kim C, Mwangi M, Chung M, Milheirço C, de Lencastre H, Tomasz A (2013) The mechanism of heterogeneous beta-lactam resistance in MRSA: key role of the stringent stress response. PLoS ONE 8:e82814. https://doi.org/10.1371/journal.pone.0082814
Aedo S, Tomasz A (2016) Role of the stringent stress response in the antibiotic resistance phenotype of Methicillin-Resistant Staphylococcus aureus. Antimicrob Agents Chemother 60:2311–2317. https://doi.org/10.1128/AAC.02697-15
Geissmann T, Chevalier C, Cros M-J, Boisset S, Fechter P, Noirot C, Schrenzel J, François P, Vandenesch F, Gaspin C, Romby P (2009) A search for small noncoding RNAs in Staphylococcus aureus reveals a conserved sequence motif for regulation. Nucleic Acids Res 37:7239. https://doi.org/10.1093/nar/gkp668
Hassan HM, Fridovich I (1978) Superoxide radical and the oxygen enhancement of the toxicity of paraquat in Escherichia coli. J Biol Chem 253:8143–8148. https://doi.org/10.1016/S0021-9258(17)34373-9
Chambers HF, Hackbarth CJ (1987) Effect of NaCl and nafcillin on penicillin-binding protein 2a and heterogeneous expression of methicillin resistance in Staphylococcus aureus. Antimicrob Agents Chemother 31:1982–1988. https://doi.org/10.1128/AAC.31.12.1982
Boyle-Vavra S, Yin S, Challapalli M, Daum RS (2003) Transcriptional induction of the penicillin-binding protein 2 gene in staphylococcus aureus by cell wall-active antibiotics oxacillin and vancomycin. Antimicrob Agents Chemother 47:1028–1036. https://doi.org/10.1128/AAC.47.3.1028-1036.2003
Ludwig C, Claassen M, Schmidt A, Aebersold R (2012) Estimation of absolute protein quantities of unlabeled samples by selected reaction monitoring mass spectrometry. Mol Cell Proteomics 11(M111):013987. https://doi.org/10.1074/mcp.M111.013987
Hackbarth CJ, Chambers HF (1993) blaI and blaR1 regulate beta-lactamase and PBP 2a production in methicillin-resistant Staphylococcus aureus. Antimicrob Agents Chemother 37:1144–1149
Ryffel C, Strässle A, Kayser FH, Berger-Bächi B (1994) Mechanisms of heteroresistance in methicillin-resistant Staphylococcus aureus. Antimicrob Agents Chemother 38:724–728
Niemeyer DM, Pucci MJ, Thanassi JA, Sharma VK, Archer GL (1996) Role of mecA transcriptional regulation in the phenotypic expression of methicillin resistance in Staphylococcus aureus. J Bacteriol 178:5464–5471
Bai J, Zhu X, Zhao K, Yan Y, Xu T, Wang J, Zheng J, Huang W, Shi L, Shang Y, Lv Z, Wang X et al (2019) The role of ArlRS in regulating oxacillin susceptibility in methicillin-resistant Staphylococcus aureus indicates it is a potential target for antimicrobial resistance breakers. Emerg Microbes Infect 8:503–515. https://doi.org/10.1080/22221751.2019.1595984
Villanueva M, Roch M, Lasa I, Renzoni A, Kelley WL (2021) The role of ArlRS and VraSR in regulating ceftaroline hypersusceptibility in methicillin-resistant staphylococcus aureus. Antibiotics 10:821. https://doi.org/10.3390/antibiotics10070821
Thumanu K, Cha J, Fisher JF, Perrins R, Mobashery S, Wharton C (2006) Discrete steps in sensing of beta-lactam antibiotics by the BlaR1 protein of the methicillin-resistant Staphylococcus aureus bacterium. Proc Natl Acad Sci U S A 103:10630–10635. https://doi.org/10.1073/pnas.0601971103
Cha J, Vakulenko SB, Mobashery S (2007) Characterization of the beta-lactam antibiotic sensor domain of the MecR1 signal sensor/transducer protein from methicillin-resistant Staphylococcus aureus. Biochemistry 46:7822–7831. https://doi.org/10.1021/bi7005459
Hiramatsu K, Ito T, Tsubakishita S, Sasaki T, Takeuchi F, Morimoto Y, Katayama Y, Matsuo M, Kuwahara-Arai K, Hishinuma T, Baba T (2013) Genomic basis for methicillin resistance in staphylococcus aureus. Infect Chemother 45:117–136. https://doi.org/10.3947/ic.2013.45.2.117
Liu J, Chen D, Peters BM, Li L, Li B, Xu Z, Shirliff ME (2016) Staphylococcal chromosomal cassettes mec (SCCmec): a mobile genetic element in methicillin-resistant Staphylococcus aureus. Microb Pathog 101:56–67. https://doi.org/10.1016/j.micpath.2016.10.028
Galimand M, Courvalin P, Lambert T (2003) Plasmid-mediated high-level resistance to aminoglycosides in enterobacteriaceae due to 16S rRNA methylation. Antimicrob Agents Chemother 47(8):2565–2571. https://doi.org/10.1128/aac.47.8.2565-2571.2003
Doi Y, Arakawa Y (2007) 16S ribosomal RNA methylation: emerging resistance mechanism against aminoglycosides. Clin Infect Dis 45:88–94. https://doi.org/10.1086/518605
Timms AR, Steingrimsdottir H, Lehmann AR, Bridges BA (1992) Mutant sequences in the rpsL gene of Escherichia coli B/r: mechanistic implications for spontaneous and ultraviolet light mutagenesis. Mol Gen Genet 232:89–96. https://doi.org/10.1007/BF00299141
Wilcox SK, Cavey GS, Pearson JD (2001) Single ribosomal protein mutations in antibiotic-resistant bacteria analyzed by mass spectrometry. Antimicrob Agents Chemother 45:3046–3055. https://doi.org/10.1128/AAC.45.11.3046-3055.2001
Acknowledgements
We would like to thank anyone involved in the IdBIORIV project, whether at the Institut des Sciences Analytiques, at the Infectious Agents Institute, at the French National Reference Centre for Staphylococci or at the Centre International de Recherche en Infectiologie. We thank Patricia Martins-Simoes and Sylvere Bastien for valuable technical help. We thank Sciex company for providing the technical support and the instruments used in the present work. We also thank Shanez Haouari from the Hospices Civils de Lyon (France) for her help in manuscript preparation.
Funding
This study and the IdBIORIV project were supported financially by the French country through the Agence Nationale de la Recherche and the « investissement d’avenir» program (ANR-18-RHUS-0013).
Author information
Authors and Affiliations
Contributions
FD, RC, PLD, CDC, AT, TC, OD, JL and FV contributed to the study conception and design. Material preparation, data collection and analysis were performed by FD, RC, PLD, RP, CD, NC and AR with the support of TC and OD. The first draft of the manuscript was written by FD, FV and JL and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Competing interest
The authors declare the following conflicts of interest: F.D, J.L and F.V have filled a patent regarding the method to improve the sensitivity of MRSA detection; R.C., J.L and F.V are co-founders of Weezion company. All other authors declare no conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Deforet, F., Carrière, R., Dufour, P.L. et al. Proteomic assay for rapid characterisation of Staphylococcus aureus antimicrobial resistance mechanisms directly from blood cultures. Eur J Clin Microbiol Infect Dis (2024). https://doi.org/10.1007/s10096-024-04811-0
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s10096-024-04811-0