Abstract
Background
The study aimed to identify, enlist, and analyze cases of unisystem LCH in the maxillofacial pediatric population to understand the clinical presentation and encourage the consideration of this rare disease in the differential diagnosis. Langerhans cell histiocytosis (LCH) is an aggressive benign condition affecting mainly the pediatric population. It can be easily masked as periodontal disease in the maxillofacial region. Early diagnosis and a systemic evaluation are of utmost importance.
Methodology
We are presenting a complete review of literature in the pediatric population according to PRISMA guidelines for clinicopathologic, histopathological, immunohistochemistry, and treatment for unisystem LCH. The risk of bias assessment across studies was done using a Case series appraisal checklist by Guo et al. 53
Results
Forty-nine articles (152 cases) were selected which met our inclusion and exclusion criteria to be included in our review. Most of the patients fall in 6–12 years of age with the involvement of the mandibular body region in 40.79% cases. This disease mainly presents as erythematous gingiva, pain, swelling, and mobile teeth. Management can range from minimal intervention to chemotherapy and surgery.
Conclusion and practical implications
Although this is a rare condition, it should be considered especially in the pediatric population with periodontitis type lesions and floating teeth and comprehensive management should be followed. Early diagnosis of the disease is very important.




Similar content being viewed by others
References
Lichtenstein L (1964) Histiocytosis X (eosinophilic granuloma of bone, ‘Letterer–Siwe disease and Schuller–Christian disease’): further observations of pathological and clinical importance. J Bone Joint Surg 46-A:76–90
Cochrane LA, Prince M, Clarke K (2003) Langerhans cell histiocytosis in the pediatric population: presentation and treatment of head and neck manifestations. J Otolaryngol 32(1):33–37
Cisternino A, Asa’ad F (2015) Fusco N et al Role of multidisciplinary approach in a case of Langerhans cell histiocytosis with initial periodontal manifestations. Int J Clin Exp Pathol 8(10):13539–13545
Ragab RR (1975) Rake 0. Eosinophilic granuloma with bilateral involvement. Oral Surg Med Oral Pathol 4:73–79
Rapidis AD, Langdon JD, Harvey PW, Patel MF (1978) Histiocytosis X. An analysis of 50 cases. Int J Oral Surg 7(2):76–84
Cohen M, Zornoza J, Cangir A, Murray J, Wallace S (1980) Direct injection of methylprednisolone sodium succinate in the treatment of solitary eosinophilic granuloma of bone. Radiol 136:289–293
Hartman KS (1980) Histiocytosis X: a review of 114 cases with oral involvement. Oral Surg Oral Med Oral Pathol 49:38
Roper M, Kelly D, Richard T, Parmley KSM, Hicks JN (1981) Eosinophilic Granuloma of the Palatal Mucosa in a Nine-Week-Old Infant. Med Pediatr Oncol 9:153–156
Chuong R, Kaban L (1985) Diagnosis and Treatment of Jaw tumors of children. J Oral Maxillofac Surg 43:323–332
Jones LR, Toth BB, Cangir A (1989) Treatment for solitary eosinophilic granuloma of the mandible by steroid injec- tion: report of a case. J Oral Maxillofac Surg 47:306–309
Loh HS, Quah TC (1990) Histiocytosis X (Langerhans-cellhistiocytosis) of the palate. Case report. Aust Dent J 35(2):117–120
Sayed SE, Brewin TB (1992) Histiocytosis X: Does Radiotherapy Still Have a Role? Clin Oncol 4:27–31
Hanapiah F, Yaacob H, Shah K, Hussain A (1993) Histiocytosis X: Evidence for a genetic Etiology. J Nihon Univ Sch Dent 35:171–174
Hermans R, De Foer I, Smet MH, Leysen J, Feenstra L, Fossion E, Baert AL (1994) Eosinophilic granuloma of the head and neck: CT and MRI features in three cases. PediatrRadiol 24:33–36
Roychoudhury A, Shah N, Parkash H, Mukhopadhyay S, Chopra P (1998) Eosinophilic granuloma of the jaws. Br J Oral Maxillofac Surg 36:380–383
Schepman KP, Radden BG, Van der Waal I (1998) Langerhans’ cell histiocytosis of the jaw bones. Report of 11 cases. Aust Dent J 43:238–241
Ardekian L, Peled M, Rosen D, Rachmiel A, Abu el-Naaj I, Laufer D (1999) Clinical and radiographic features of eosino- philicgranulomain the jaws: review of 41 lesions treated by surgery and low-dose radiotherapy. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 87:238–242
Warner BF, Luna MA, Newland JR (2000) Temporomandibular joint neoplasms and pseudotumors. Adv Anat Pathol 7(6):365–381
Namai T, Yusa H, Yoshida H (2001) Sponta- neous remission of a solitary eosinophilic granuloma of the mandible after biopsy: a case report. J Oral Maxillofac Surg 59:1485–1492
Bartnick A, Friedrich RE, Roeser K, Schmelzle R (2002) Oral Langerhans cell histiocytosis. J Craniomaxillofac Surg 30:91–96
Eckardt A, Schultze A (2003) Maxillofacial manifestations of Langerhans cell histiocytosis: A clinical and therapeutic analysis of 10 patients. Oral Oncol 39(7):687–694
Key SJ, O'Brien CJ, Silvester KC, Crean SJ (2004) Eosinophilic granuloma: resolution of maxillofacial bony lesions fol- lowing minimal intervention. Report of three cases and a review of the literature. J Craniomaxillofac Surg 32:170–175
Pilecki S, Pufal J, Gierach M, Laskowska K, Lasek W, Wysocki M, Drewa S (2004) Langerhans’ cell histiocytosis of the mandible in bone scintigraphy and CT. Nuclear Med Rev 7(2):183–186
Putters TF, de Visscher JG, van Veen A, Spijkervet FK (2005) Intralesional infiltration of corticosteroids in the treatment of local isedlangerhans' cell histiocytosis of the mandible Report of known cases and three new cases. Int J Oral Maxillofac Surg 34:571–575
Li Z, Li ZB, Zhang W, Li JR, Wang SP, Cheng Y, Wei MX (2006) Eosinophilic granuloma of the jaws: An analysis of clinical and radiographic presentation. Oral Oncol 42(6):574–580
Ramani P, Chandrasekar T, Baig MF et al (2007) Langerhans cell histiocytosis of the mandible in a six-year-old child. Indian J Dermatol Venereol Leprol 73:114–116
Bansal D, Marwaha RK, Trehan A, Gupta V, Varma N (2008) Langerhans’ Cell Histiocytosis: Experience from a Single Center. Indian Pediatr 45:685–688
Moralis A, Kunkel A, Kleinsasser N et al (2008) Intralesionalcortico-steroid therapy for mandibular Langerhans cell histiocytosispreserving the intralesional tooth germ. Oral Maxillofac Surg 12:105
Jalil AA, Lau SH (2009) Oral Langerhans cell histiocytosis in Malaysian children: a 40-year experience. Int J Paediatr Dent 19:349–353
Muramatsu T, Hall GL, Hashimoto S, Miyauchi J, Shimono M (2010) Clinico-pathologic conference: Case 4. Langerhans cell histiocytosis (LCH). Head Neck Pathol 4:343–346
Park JW, Chung JW (2010) Long-term treatment of Langerhans cell histiocytosis of the mandibular condyle with indomethacin. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 109:e13–e21
Baş B, Duran H, Şenyurt Ö, Günhan O (2011) Eosinophilic granuloma: Resolution of lesion after biopsy. J Craniofac Surg 22:2409–2412
Martins MA, Gheno JL, Sant’AnaFilho M, Pinto DS Jr, Tenis CA, Martins MD et al (2011) Rare case of unifocal Langerhans cell histiocytosis in four-month-old child. Int J Pediatr Otorhinolaryngol 75:963–967
Shetty SK, Mamatha GS, Desai RS, Sable DM, Deshmukh VL, Ajwani HR (2012) Bilateral gingival enlargement of the posterior mandible in an adolescent child. Oral Surg Oral Med Oral Pathol Oral Radiol 114:406–410
Hutchison A, Jain S, Hyam D, Dahlstro JE (June 2012) Tennis Racquets In The Jaw: Eosinophilic Granuloma. Pathology 44(4):387–388
Cho YA, Yoon HJ, Hong SD, Lee J, Hong SP (2013) Hypothetical pathogenesis of eosinophilic infiltration in Langerhans cell histiocytosis of the jaw. Oral Surg Oral Med Oral Pathol Oral Radiol 116:734–742
Felstead AM, Main BG, Thomas SJ, Hughes CW (2013) Recurrent Langerhans cell histiocytosis of the mandible. Br J Oral Maxillofac Surg 51:264–265
Lee SH, Yoon HJ (2013) Intralesional infiltration of corticosteroids in the treatment of localized Langerhans cell histiocytosis of the mandible: Report of two cases. Oral Surg Oral Med Oral Pathol Oral Radiol 116:e255–e260
Agarwal P, Kaushal M (2014) An unusual presentation of Langerhans cell histiocytosis. J Cytol 31:227–229
Sherwani RK, Akhtar K, Qadri S, Ray PS (2014) Eosinophilic granuloma of the mandible: A diagnostic dilemma. BMJ Case Rep 2014:bcr2013200274
Divya KS (2014) Oral manifestion of Langerhans cell histiocytosis mimicking inflammation. Indian J Dent Res 25:228–230
Lima EN, de Araújo EM, de Oliveira PT, de Medeiros AM (2014) Oral Langerhans cell histiocytosis: case report with follow-up of ten years. Braz J Otorhinolaryngol 80:366–367
Liu J, Liu D, Zhou Y, Chen Q, Zeng X, ** X (2014) Langerhans cell histiocytosis with widespread ulcers and masses on the palate. Indian J Dermatol Venereol Leprol 80(5):462–463
Mani V, Vinod VS, George A, Sivaprasad K (Jan–Mar 2015) K. Eosinophilic Granuloma of Mandibular Condyle: Resection and Complete Regeneration. J Maxillofac Oral Surg 14(1):107–110
Azariah EDS, ChanDraSEkaran D, ChinnaSwami R, Balasubramaniams JE (2016) "Histiocytosis X" – A Rare Case Report. J Clin Diagn Res 10(10):ZD19–ZD22
Kannan K, Alwithanani N, Salama M, Kumar M, Uthappa R, Ahamed M et al (2016) Eosinophilic granuloma in jaw bone: A pare pediatric case report. Ethiop J Health Sci 26:487–490
Felstead AM, Main BG, Thomas SJ, Hughes CW (2013) Recurrent Langerhans cell histiocytosis of the mandible. Br J Oral Maxillofac Surg 51:264–265
Rao DG, Trivedi MV, Havale R, Shrutha SP (2017) A rare and unusual case report of Langerhans cell histiocytosis. J Oral Maxillofac Pathol 21:140–144
Dantas MVM, Souza PBRN, Gabrielli MAC (2019) l. Diagnosis and management of eosinophilic granuloma of the jaw: a case report. Rev Gaúch Odontol 67:e20190029
Izzetti R, De Marco E, Caramella D (2019) Cone Beam CT study of a case of eosinophilic granuloma of the mandible in a young patient. BMJ Case Rep 12:e228455
Kim JE, Yi WJ, Heo MS, Lee SS, Choi SC, Huh K (2019) Langerhans cell histiocytosis of the jaw, a mimicker of osteomyelitis on CT and MR images. A retrospective analysis. Medicine 98:27
Nezafati S, Yazdani J, Shahi SH, Mehryari M, Hajmohammadi E (2019) Outcome of Surgery as Sole Treatment of Eosinophilic Granuloma of Jaws. J Dent Shiraz Univ Med Sci 20(3):210–214
Guo B, Moga C, Harstall C (2016) Schopflocher D.A principal component analysis is conducted for a case series quality appraisal checklist. J Clin Epidemiol 69:199–207
Writing Group of the Histiocyte Society (1987) Histiocytosis syndromes in children. Lancet 1(8526):208–209
Eden OB (1998) Oncology and terminal care. In: Campbell AGM, McIntosh N (eds) Forfar and ArNeil‘s: textbook of pediatrics. Churchill Livingstone, New York, pp 884–934
Emile JF, Abla O, Fraitag S et al (2016) Revised classification of histiocytosis and neoplasms of the macrophage-dendritic cell lineages. Blood 127(22):2672–2681
Guyot-Goubin A, Donadieu J, Barkaoui M, Bellec S, Thomas C, Clavel J (2008) Descriptive epidemiology of childhood Langerhans cell histiocytosis in France, 2000-2004. Pediatr Blood Cancer 51(1):71–75
Aricò M, Haupt R, Russotto VS et al (2001) Langerhans cell histiocytosis in two generations: a new family and review of the literature. Med Pediatr Oncol 36(2):314–316
Stålemark H, Laurencikas E, Karis J, Gavhed D, Fadeel B, Henter JI (2008) Incidence of Langerhans cell histiocytosis in children: a population-based study. Pediatr Blood Cancer 51(1):76–81
Buchmann L, Emami A, Wei JL (2006) Primary head and neck Langerhans cell histiocytosis in children. Otolaryngol Head Neck Surg 135:312–317
Nicholson HS, Egeler RM, Nesbit ME (1998) The epidemiology of Langerhans cell histiocytosis. Hematol Oncol Clin North Am 12(2):379–384
Lombardi T, Hauser C, Budtz-Jörgensen E (1993) Langerhans cells: structure, function and role in oral pathological conditions. J Oral Pathol Med 22(5):193–202
Vassallo R, Ryu JH, Colby TV, Hartman T, Limper AH (2000) Pulmonary Langerhans'-cell histiocytosis. N Engl J Med 342(26):1969–1978
Badalian-Very G, Vergilio JA, Degar BA, MacConaill LE, Brandner B, Calicchio ML, Kuo FC, Ligon AH, Stevenson KE, Kehoe SM, Garraway LA, Hahn WC, Meyerson M, Fleming MD, Rollins BJ (2010) Recurrent BRAF mutations in Langerhans cell histiocytosis. Blood 116(11):1919–1923
Berres ML, Lim KP, Peters T et al (2014) BRAF-V600E expression in precursor versus differentiated dendritic cells defines clinically distinct LCH risk groups. J Exp Med 211(4):669–683
Snyder SR, Merkow LP, White NS (1973) Eosinophilic granuloma of bone: report of case. J Oral Surg 31:712–715
Storrs J (1976) Bilateral eosinophilic granuloma of the mandible. Oral Surg Oral Med Oral Pathol 41:93–100
Sahm F, Capper D, Preusser M, Meyer J, Stenzinger A, Lasitschka F, Berghoff AS, Habel A, Schneider M, Kulozik A, Anagnostopoulos I, Müllauer L, Mechtersheimer G, von Deimling A (2012) BRAFV600E mutant protein is expressed in cells of variable maturation in Langerhans cell histiocytosis. Blood 120(12):e28–e34
Grois N, Fahrner B, Arceci RJ, Henter JI, McClain K, Lassmann H, Nanduri V, Prosch H, Prayer D (2010) Central nervous system disease in Langerhans cell histiocytosis. J Pediatr 156(6):873–881
Haupt R, Minkov M, Astigarraga I et al (2013) Euro HistioNetwork.Langerhans cell histiocytosis (LCH): guidelines for diagnosis, clinical work-up, and treatment for patients till the age of 18 years. Pediatr Blood Cancer 60(2):175–118
Dagenais M, Pharoah MJ, Sikorski PA (1992) The radiographic characteristics of histiocytosis X. A study of 29 cases that involve the jaws. Oral Surg Oral Med Oral Pathol 74:230–236
Valladeau J, Ravel O, Dezutter-Damuyant C, Moore K, Klei-imeer M, Lin Y et al (2000) Langerin, a novel C-type lectin specific to Langerhans cells, is an endocytic receptor that induces the for- mation of Birbeck granules. Immunity 12:71–81
SuonitaKhung J-FB, Amzallag-Bellenger E, Lambilliote A, Ares GS, Cotton A (2013) Skeletal involvement in Langerhans cell histiocytosis. Nathalie Boutry Insights Imag 4(5):569–579
Kitano M, Landini G, Semba I et al (1990) Eosinophilic granuloma showing rapid regression. Report of a mandibular case with application of a modified PNA staining method for demonstration of Langerhans’ cell histiocytosis. Acta Pathol Jpn 40:588–595
Broadbent V, Pritchard J, Davies EG, Levinsky RJ, Heaf D, Atherton DJ, Pincott JR, Tucker S (1984) Spontaneous remission of multi-system histiocytosis X. Lancet 1:253–254
Raney RB, D’Angio GJ (1989) Langerhans’ cell histiocytosis(histiocytosis X): experience at the Children’s Hospital of Philadelphia. Med Pediatr Oncol 17:20–28
Egeler RM, Thompson RC Jr, Voûte PA, Nesbit ME Jr (1992 Nov-Dec) Intralesional infiltration of corticosteroids in localized Langerhans' celhistiocytosis. J Pediatr Orthop 12(6):811–814
Baptista AM, Camargo AF, Camargo OP (2012) Does adjunctive chemotherapy reduce remission rates compared to cortisone alone in unifocal or multifocal histiocytosis of bone? Clin Orthop Relat Res 470(3):663–669
Alajbeg I, Vucicevic Boras V, Femenic R, Cekic-Arambasin A et al (2006) Unrecognized oral manifestations of Langerhans cell histiocytosis which progressed to systemic disease. Oral Oncol Extra 42(1):10–13
Krooks J, Minkov M, Weatherall AG (2018) Langerhans cell histiocytosis in children: History, classification, pathobiology, clinical manifestations, and prognosis. J Am Acad Dermatol 78(6):1035–1044
Acknowledgements
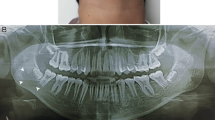
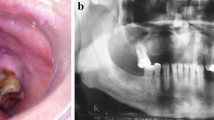
We offer our sincere thanks to Dr. Daisy, Additional Professor, Pediatrics, for doing a systemic examination of the patients. We would also like to thank our patients for letting us use their photographs in the contribution of the scientific literature.
Why is this paper important?
-
As this disease mimics periodontitis, the dentist needs to keep this entity as one of the differential diagnosis in cases of extensive periodontitis.
-
Oral-cavity LCH can be a precursor to systemic LCH and systemic or multisystem LCH which has a poorer prognosis, knowing this disease can help in early diagnosis of its any severe form [79].
-
As most child dental problems are addressed by pediatric dentists, if they are versed with a broader picture, misdiagnosis or delayed diagnosis can be avoided.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
All procedures performed in the participants were according to the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards.
Ethics approval
This is a systematic review and Institutional Ethical Clearance was not required for this study. However, consent was taken from both patients for release of their photographs.
Consent to participate
Informed consent was obtained from both participants included in the study.
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Chugh, A., Kaur, A., Kumar Patnana, A. et al. Unisystem Langerhans cell histiocytosis in maxillofacial region in pediatrics: comprehensive and systematic review. Oral Maxillofac Surg 25, 429–444 (2021). https://doi.org/10.1007/s10006-021-00949-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10006-021-00949-9