Abstract
Purpose
Risser stage is widely used as a marker for skeletal maturity (SM) and thereby an indirect measure for the risk of progression of adolescent idiopathic scoliosis (AIS). The Scoliosis Research Society recommends bracing for Risser stages 0–2 as Risser stage 3 or above is considered low risk. Very few studies have assessed the risk of progression during bracing in Risser stages 3–4. The objective of the current study is to determine if Risser stages 3–4 provide a meaningful cutoff in terms of progression risk in patients with AIS treated with night-time bracing.
Methods
AIS patients treated with night-time brace from 2005 to 2018 with a Cobb angle between 25 and 40 degrees and Risser stages 0–4 were retrospectively included. Curve progression (> 5 degrees increase) was monitored until surgery or SM. Skeletal maturity was defined as either 2 years postmenarchal, no height development or closed ulnar epiphyseal plates on radiographs.
Results
One hundred and thirty-five patients were included (Risser stages 0–2: n = 86 and 3–4: n = 49). Overall, radiographic curve progression occurred in 52% while progression beyond 45 degrees was seen in 35%. The progression rate in the Risser 0–2 group was 60% and 37% in the Risser 3–4 group (p = 0.012). In multivariate logistic regression analysis, adjusted for Risser stages and age, only premenarchal status showed a statistically significant association with progression (OR: 2.68, 95%CI 1.08–6.67).
Conclusion
Risser stage does not provide a clinically meaningful differentiation of progression risk in AIS patients treated with a night-time brace. Risk assessment should include other more reliable measures of skeletal growth potential.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Bracing is the standard treatment of adolescent idiopathic scoliosis (AIS) in skeletal immature patients with main curves greater than 25 degrees [1]. The full-time brace has shown superiority compared with observation in terms of preventing curve progression [2]. This comprehensive full-time brace treatment (> 18 h daily) can be challenging regarding patient compliance [3, 4], leading to higher rates of curve progression and need for surgical treatment [5, 6]. Price et al. [7] introduced the Charleston Night-time Bending Brace in 1990. The night-time brace has shown superiority regarding compliance (> 90%) compared with full-time braces [4]. This brace is optimally worn for a minimum of 8-h every night until skeletal maturity (SM). Risser staging is used as an indicator for SM and was first described in 1958 [8]. Several other indicators of skeletal growth have been suggested [9,10,11,12,13], but the Risser stage is still widely used and is practical since the crista apophysis can be included in a standard spinal X-ray. The general assumption is that low Risser stages (0–2) are seen in skeletally immature patients with a high risk of curve progression compared with the more mature patients with high Risser stages (3–5) and a low risk of curve progression [6, 14,15,16]. The Scoliosis Research Society (SRS) and The International Scientific Society on Scoliosis Orthopaedic and Rehabilitation Treatment (SOSORT) have published general guidelines for initiation of brace treatment [14, 15]. For SRS, one of these brace recommendations is a Risser stage between 0 and 2 while SOSORT recommends bracing for Risser stages 0–3. At our institution, we still initiate brace treatment in select patients with Risser stage 3 or 4, who we believe have remaining skeletal growth. This assessment relies on age, information on clinical findings such as growth spurt, menarchal status and parent’s height.
The aim of the present study was to assess if Risser stage 3 or 4 provides a clinically meaningful cutoff point in terms of progression risk in AIS patients treated with a night-time brace. To our knowledge, no studies have previously assessed this question.
Materials and methods
We conducted a retrospective cohort study approved by the National Health and Medical Authority and The National Data Protection Agency (May 20, 2020, #31-1521-327; October 21, 2021, #P-2021-779).
Adolescent idiopathic scoliosis was defined as a Cobb angle of at least 10° in the absence of underlying congenital or neuromuscular abnormalities and age of ≥ 10 years at the time of diagnosis [14].
Subjects
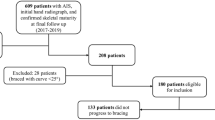
We consecutively included all AIS patients treated with a night-time brace between January 1, 2005, and December 31, 2018, at a single tertiary center. A total of 135 patients were included for final analysis (Fig. 1). Additional inclusion criteria were according to the current SRS and SOSORT guidelines in terms of brace initiation [14, 15]: age greater than 10 years at brace prescription, no prior treatment and primary curve between 25 and 40 degrees. Moreover, patients with Risser stages between 0 and 4 and any menarchal status at brace initiation were all included. We excluded patients who were treated with other braces than a night-time brace and patients who discontinued brace treatment due to discomfort. Patient selection is illustrated in a flowchart (Fig. 1).
Electronic medical records were used to obtain patient demographics such as age, sex, menarchal status, date of brace—initiation and discontinuation.
The following standing anteroposterior radiographic parameters were obtained: Risser stage, major Cobb angle and curve types. Thoracic curves had an apex above Th12, thoracolumbar/lumbar curves at Th12 or below and double curves with both curves above 30 degrees. All patients had out-of-brace radiographs at brace initiation and subsequently every 6–9 months, with one-night out-of-brace before radiographs. Brace treatment continued until SM or surgery. In cases of doubt of skeletal maturity status, we used hand X-rays to determine the Sanders maturity stage. There was a minimum of 1-year follow-up after brace termination.
Skeletal maturity and progression
We defined SM as either 2 years after menarche, less than 1-cm change in height between two consecutive in-hospital patient visits more than 6 months apart or closed ulnar epiphyseal plate on wrist radiographs (Sanders stage 7)[9, 15].
The main outcome of the current study was progression rate in patients undergoing brace treatment. Progression was defined as a radiographic Cobb angle increase of > 5° between brace initiation and brace discontinuation. Patients with a Cobb angle increase of < 6° were categorized as having no progression.
To determine Risser stages pre-brace on radiograph, we initially used the new “Risser + ” grading system [17] that combines the North American and European Risser classifications. Additionally, we categorized Risser stages into two groups of Risser 0–2 and Risser 3–4.
Night-time brace
All patients were treated with the providence night-time brace. Compliance was assessed through patient reports at in-hospital control visits. Minor compliance problems were defined as patient-reported discomfort with the brace, e.g., pain and trouble slee**, whereas major compliance problems were defined as premature brace discontinuation.
Statistical analysis
All statistical analyses were conducted using R, version 4.2.0 (R Development Core Team, Vienna, Austria, 2020). Data are reported as either means (± SD), medians [IQR] or proportions (%). Distribution of data was assessed with histograms and Q–Q plots, whereof Student’s t-test and Wilcoxon’s rank-sum test were used to compare Gaussian and non-Gaussian distributed data, respectively. In comparison with categorical variables, Pearson’s X2 test was used for larger observations and Fisher’s exact test for less than 5 expected values in individual cells. Kruskal–Wallis test was used to compare proportions for non-Gaussian distributed data with three groups or more. Uni- and multivariate logistic regression analysis compared progression with other variables. Results were reported as odds ratios (OR) with 95% confidence interval (CI). P-values of < 0.05 were considered statistically significant.
Results
Subjects
Eighty-six patients were in the Risser 0–2 group and 49 patients in the Risser 3–4 group. Patients were stratified into groups of no progression and progression (Tables 1 and 2).
Skeletal maturity and progression
Overall, we found progression in 70 (52%) patients. Forty-three (34%) patients underwent fusion surgery at the 2-year follow-up. Progression occurred in 52 (60%) patients in the Risser 0–2 group and in 18 (37%) patients in the Risser 3–4 group (p = 0.012) (Table 3 and Fig. 2). The patients who progressed in the Risser 3–4 group (Table 2) were younger (14.1 ± 1.1 years vs. 14.8 ± 1.0, p = 0.028) and were more often double curves (p = 0.046) with a higher rate of premenarchal status (28% vs. 10%, p = < 0.001) compared with non-progressive Risser 3–4 patients. Univariate analysis showed statistically significant odds of progression in both Risser group (OR: 0.38, 95%CI 0.18–0.78), premenarchal status (OR: 4.37, 95%CI 1.92–9.72) and age (OR: 0.63, 95%CI 0.47–0.84) (Table 4). In multivariate logistic regression analysis, only premenarchal status showed a statistically significant association with progression (OR: 2.68, 95%CI 1.08–6.67) (Table 4).
Discussion
The present study aimed to evaluate the clinical utility of Risser staging as a predictor of curve progression in patients with AIS. We found a substantial progression rate of 37% in the Risser 3–4 group. This is the first study to report on curve progression in a Risser 3 and 4 AIS cohort treated with night-time bracing. The progression rate in Risser 0–2 was 60% similar to other night-time brace studies [18, 19].
Patients who progressed in the Risser 3–4 group were predominantly younger, premenarchal and had thoracic curves compared with patients who did not progress. These findings are consistent with the previous results by Sun et al. [20] who found progressive curves in younger patients who were more often premenarchal with main thoracic curve patterns. The significant age difference in our cohort could be a potential confounder in terms of curve progression. Negrini et al. [21] examined patients with Risser stages 4–5 and reported curve improvement in 48% (n = 11) of patients treated with full-time brace (> 18 h). However, only one patient progressed more than 5°. In a non-brace population, Kawasaki et al. [16] reported a progression rate of 15% (n = 8) in patients with Risser stages 4–5.
To improve the prediction of curve progression, it seems that Risser stages should be used in conjunction with other SM factors including skeletal age, chronologic age and time since menarche [22].
In the multivariate analysis, we found no significant association between Risser stage and progression when accounting for age and menarche. Premenarchal status was strongly associated with progression, and one-fifth of female patients in the Risser 3–4 group were premenarchal. Kawasaki et al. [16] found a limited correlation between Risser stage and menarchal status. Ohrt-Nissen et al. [19] found an association between premenarchal status and progression in patients treated with a night-time brace. In contrast, a systematic review by Bogaart et al. [23] found inconclusive evidence regarding premenarchal status being a predictor of progression in patients treated with a full-time brace. Moradi et al. [24] recommended additional studies evaluating premenarchal state to better understand the effect on progression risk in AIS patients. Sanders staging has shown a better ability to determine SM in AIS patients compared with Risser stages and Greulich and Pyle skeletal ages [10]. Olecranon ossification centers using the Sauvegrain method have been proposed to complement the assessment of skeletal age [11, 12]. In addition, proximal humerus ossification may be more accurate in determining SM than Risser stages [13]. Combining all available SM factors provides a better insight of actual SM status for the individual patient. Negrini et al. [21] and Kawasaki et al. [16] included patients with Risser stages above 2. However, their cohort is not comparable to ours since the patients either had braces worn for 18 h + or no brace treatment at all. Therefore, one might speculate if the high progression rate in the Risser 3–4 group is a consequence of the night-time brace.
Night-time brace
Ruffilli et al. [18] conducted a systematic review on the effect of night-time bracing. Of the seven included studies, five of them reported no difference in curve progression compared to full-time bracing. The included studies looked at AIS patients with Risser stages 0–2 treated with a night-time brace and report progression rates similar to our findings. We found a progression rate of 60% in the Risser 0–2 group, and the studies in the systematic review found progression rates between 27 and 69%. None of the night-time brace studies in the review included patients with Risser stage 3 or 4. Ruffili et al. [18] concluded that low methodological quality of all the included studies did not allow firm conclusions about the efficacy of the night-time brace.
Strengths and limitations
We do acknowledge some limitations in the current study. There is no school screening program in Denmark, and patients are first referred for tertiary evaluation when they show advanced signs of scoliosis. Therefore, patients are more skeletally mature and with bigger curves [25]. Hence, there is a selection bias toward referral of patients who have already shown a tendency toward progression. Likely, there are non-progressive Risser stages 3 and 4 patients in society that are never referred to our institution and thereby are not a part of this study. Exact Risser grading was not possible due to lack of visibility of the most lateral part of the iliac crest on radiographs. Consequently, we could not differentiate between Risser stages 0, 1 and 2. This was a non-comparative study that did not include full-time braced patients. We cannot extrapolate our results to full-time bracing and can only conclude on progression risk for patients treated with a night-time brace. The retrospective study design only allows for conclusions on association and not causal correlation.
We do believe our findings to be of significance to both clinicians and patients. This is one of the largest night-time brace studies on AIS patients. We found a substantial progression rate in the Risser 3–4 group and argue that the assessment of progression risk cannot rely solely on this parameter. The interpretation of SRS and SOSORT guidelines for brace initiation should be with this in mind.
In conclusion, we found that Risser stages 3–4 in night-time braced AIS patients do not provide a clinically meaningful differentiation of progression risk since the progression rate in this group was high. We encourage clinicians to look at multiple SM factors when considering progression risk in AIS patients.
Availability of data and materials
The datasets generated during and/or analyzed during the current study are not publicly available due to national data protection law.
Code availability
Code can be made available upon reasonable request.
References
Weinstein SL, Dolan LA, Cheng JCY, Danielsson A, Morcuende JA (2008) Adolescent idiopathic scoliosis. Lancet (Lond, Engl) 371(9623):1527–1537. https://doi.org/10.1016/S0140-6736(08)60658-3
Weinstein SL, Dolan LA, Wright JG, Dobbs MB (2013) Effects of bracing in adolescents with idiopathic scoliosis. N Engl J Med 369(16):1512–1521. https://doi.org/10.1056/NEJMoa1307337
Roland d’Amato C, Griggs S, McCoy B (2001) Nighttime bracing with the providence brace in adolescent girls with idiopathic scoliosis. Spine 26(18):2006–2012. https://doi.org/10.1097/00007632-200109150-00014
Antoine L, Nathan D, Laure M, Briac C, Jean-François M, Corinne B (2020) Compliance with night-time overcorrection bracing in adolescent idiopathic scoliosis: result from a cohort follow-up. Med Eng Phys 77(2020):137–141. https://doi.org/10.1016/j.medengphy.2020.01.003
Aulisa AG, Giordano M, Falciglia F, Marzetti E, Poscia A, Guzzanti V (2014) Correlation between compliance and brace treatment in juvenile and adolescent idiopathic scoliosis: SOSORT 2014 award winner. Scoliosis 9(1):6. https://doi.org/10.1186/1748-7161-9-6
El Hawary R, Zaaroor-Regev D, Floman Y, Lonner BS, Alkhalife YI, Betz RR (2019) Brace treatment in adolescent idiopathic scoliosis: risk factors for failure—a literature review. Spine J 19(12):1917–1925. https://doi.org/10.1016/j.spinee.2019.07.008
Price CT, Scott DS, Reed FE, Riddick MF (1990) Nighttime bracing for adolescent idiopathic scoliosis with the Charleston bending brace. Preliminary report. Spine 15(12):1294–1299. https://doi.org/10.1097/00007632-199012000-00011
Risser JC (1958) The Iliac apophysis; an invaluable sign in the management of scoliosis. Clin Orthop 11:111–119
Sanders JO, Khoury JG, Kishan S, Browne RH, Mooney JF, Arnold KD, McConnell SJ, Bauman JA, Finegold DN (2008) Predicting scoliosis progression from skeletal maturity: a simplified classification during adolescence. J Bone Joint Surg-Am 90(3):540–553. https://doi.org/10.2106/JBJS.G.00004
Sanders JO, Browne RH, McConnell SJ, Margraf SA, Cooney TE, Finegold DN (2007) Maturity assessment and curve progression in girls with idiopathic scoliosis. J Bone Joint Surg 89(1):64–73. https://doi.org/10.2106/JBJS.F.00067
Diméglio A, Charles YP, Daures J-P, de Rosa V, Kaboré B (2005) Accuracy of the Sauvegrain method in determining skeletal age during puberty. J Bone Joint Surg Am 87(8):1689–1696. https://doi.org/10.2106/JBJS.D.02418
Sinkler MA, Furdock RJ, Chen DB, Sattar A, Liu RW (2022) The systematic isolation of key parameters for estimating skeletal maturity on lateral elbow radiographs. J Bone Joint Surg 104(22):1993–1999. https://doi.org/10.2106/JBJS.22.00312
Li DT, Cui JJ, DeVries S, Nicholson AD, Li E, Petit L, Kahan JB, Sanders JO, Liu RW, Cooperman DR, Smith BG (2018) Humeral head ossification predicts peak height velocity timing and percentage of growth remaining in children. J Pediatr Ortho 38(9):e546–e550. https://doi.org/10.1097/BPO.0000000000001232
Negrini S, Donzelli S, Aulisa AG, Czaprowski D, Schreiber S, de Mauroy JC, Diers H, Grivas TB, Knott P, Kotwicki T, Lebel A, Marti C, Maruyama T, O’Brien J, Price N, Parent E, Rigo M, Romano M, Stikeleather L, Wynne J, Zaina F (2018) 2016 SOSORT guidelines: orthopaedic and rehabilitation treatment of idiopathic scoliosis during growth. Scoli Spinal Disord 13(1):3. https://doi.org/10.1186/s13013-017-0145-8
Richards BS, Bernstein RM, D’Amato CR, Thompson GH (2005) Standardization of criteria for adolescent idiopathic scoliosis brace studies. Spine 30(18):2068–2075. https://doi.org/10.1097/01.brs.0000178819.90239.d0
Kawasaki S, Shigematsu H, Tanaka M, Suga Y, Yamamoto Y, Tanaka Y (2020) Is brace treatment unnecessary for cases of adolescent idiopathic scoliosis above Risser sign 3? J Orthop Sci 25(6):975–979. https://doi.org/10.1016/j.jos.2020.01.007
Troy MJ, Miller PE, Price N, Talwalkar V, Zaina F, Donzelli S, Negrini S, Hresko MT (2019) The “Risser+” grade: a new grading system to classify skeletal maturity in idiopathic scoliosis. Eur Spine J 28(3):559–566. https://doi.org/10.1007/s00586-018-5821-8
Ruffilli A, Fiore M, Barile F, Pasini S, Faldini C (2021) Evaluation of night-time bracing efficacy in the treatment of adolescent idiopathic scoliosis: a systematic review. Spine Deform 9(3):671–678. https://doi.org/10.1007/s43390-020-00248-5
Ohrt-Nissen S, Hallager DW, Gehrchen M, Dahl B (2016) Flexibility predicts curve progression in providence night time bracing of patients with adolescent idiopathic scoliosis. Spine 41(22):1724–1730. https://doi.org/10.1097/BRS.0000000000001634
Sun X, Wang B, Qiu Y, Zhu Z, Zhu F, Yu Y, Qian B, Ma W, Liu Z, Mao S (2010) Outcomes and predictors of brace treatment for girls with adolescent idiopathic scoliosis. Orthop Surg 2(4):285–290. https://doi.org/10.1111/j.1757-7861.2010.00101.x
Negrini S, Donzelli S, Lusini M, Zaina F (2012) Bracing can reduce high degree curves and improve aesthetics immediately after the end of growth. Final results of a retrospective case series. Stud Health Technol Inf 176:393–396
Hacquebord JH, Leopold SS (2012) In brief: the Risser classification: a classic tool for the clinician treating adolescent idiopathic scoliosis. Clin Orthop Relat Res 470(8):2335–2338. https://doi.org/10.1007/s11999-012-2371-y
van den Bogaart M, van Royen BJ, Haanstra TM, de Kleuver M, Faraj SSA (2019) Predictive factors for brace treatment outcome in adolescent idiopathic scoliosis: a best-evidence synthesis. Eur Spine J 28(3):511–525. https://doi.org/10.1007/s00586-018-05870-6
Moradi V, Babaee T, Shariat A, Khosravi M, Saeedi M, Parent-Nichols J, Cleland JA (2022) Predictive factors for outcomes of overcorrection nighttime bracing in adolescent idiopathic scoliosis: a systematic review. Asian Spine J 16(4):598–610. https://doi.org/10.31616/asj.2021.0037
Ohrt-Nissen S, Hallager DW, Henriksen JL, Gehrchen M, Dahl B (2016) Curve magnitude in patients referred for evaluation of adolescent idiopathic scoliosis: five years’ experience from a system without school screening. Spine Deform 4(2):120–124. https://doi.org/10.1016/j.jspd.2015.10.001
Acknowledgements
Thank you to all contributing authors.
Funding
Open access funding provided by Royal Library, Copenhagen University Library. No external funding was received.
Author information
Authors and Affiliations
Contributions
MH helped in substantial contributions to the conception or design of the work. Substantial contributions to the acquisition, analysis and interpretation of data. Revising the work critically for important intellectual content. Final approval of the version to be published. NT, BD, TBA, MG and SON helped in substantial contributions to the conception or design of the work. Revising the work critically for important intellectual content. Final approval of the version to be published.
Corresponding author
Ethics declarations
Conflict of interest
MG helped in institutional grants from Cerapedics, institutional grants from NuVasive and institutional grants from Stryker; BD worked in Stryker (consultancy) and supported by The Alfred Benzon Foundation; the remaining authors report no conflicts of interest.
Ethical approval
This study was approved by the National Health and Medical Authority and The National Data Protection Agency.
Informed consent
This study includes no experimental investigation.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Heegaard, M., Tøndevold, N., Dahl, B. et al. Does Risser stage accurately predict the risk of curve progression in patients with adolescent idiopathic scoliosis treated with night-time bracing?. Eur Spine J 32, 3077–3083 (2023). https://doi.org/10.1007/s00586-023-07808-z
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00586-023-07808-z