Abstract
Objective
Women with gynecologic cancer may suffer from pelvic floor dysfunction (PFD). Before radiotherapy, prehabilitation with pelvic floor muscle exercises (PFME) and vaginal dilator (VD) might prevent it and foster sexual life. This study aims to explore the experience of gynecologic cancer patients getting external beam radiation treatments regarding barriers to and facilitators of adherence to a prehabilitation program to prevent PFD.
Methods
This qualitative research with thematic content analysis included 11 women with gynecologic cancer and different levels of adherence to PFME and VD. Participants were interviewed based on a semi-structured script. The information was analyzed manually, assisted with Nvivo12® software, and triangulated with open coding.
Results
High self-motivation, desire to improve their health, symptoms of improvement, availability of time, the desire to resume sexual life, and the support of the partner were facilitators of adherence. The instructional exercise audio, clarity of the information, and closer communication with the physical therapist were also valued. The main barriers were general malaise secondary to oncological treatments, forgetfulness, lack of time, misinformation, lack of coordination with the treatment team, discomfort with the VD, and a feeling of shame. Feedback from the attending physician was a facilitator when present or a barrier when absent.
Conclusion
These barriers and facilitators should be considered when designing and implementing preventive programs with PFME and VD. Behavioral counselling should consider the desire to remain sexually active; in such cases, including the partner in the therapeutic process is appraised. Otherwise, the focus should be on benefits for maintenance of pelvic floor function.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
According to the latest GLOBOCAN report (2018), gynecologic cancer represents 16.8% of all new cancers, with a 5-year prevalence of 3.7 million women, with cervical cancer being the most frequent type [1]. Treatments for these cancers include radiation therapy, chemotherapy, brachytherapy, and surgery [2]. Women receiving radiotherapy may present pelvic floor dysfunction (PFD), manifested with urinary incontinence, vaginal stenosis, fecal incontinence or sexual dysfunction. These clinical manifestations may last for years and, maybe, in some cases, irreversible [3,4,5]. Rehabilitative prevention programs are key to improving the quality of life and reducing the unwanted side effects of treatments [6, 7].
These programs should include pelvic floor muscle exercises (PFME) and vaginal dilators (VD). The first-line treatment in the prevention and treatment of pelvic floor dysfunctions is PFME [8, 9]. Similarly, the use of a vaginal dilator (VD) has proven to be effective in the prevention and treatment of vaginal stenosis, a recurrent problem in women undergoing radiotherapy [10,11,12], recommended in international guidelines [13,14,15]. Studies also agree that the success and maintenance of the results of this type of intervention depend on adherence [13, 16,17,18]. However, adherence reported in approaches using VD for stenosis prevention is low [13, 19].
The World Health Organization states that “the ability of patients to optimally follow treatment plans is frequently compromised by more than one barrier, usually related to different aspects of the problem” [20]. Based on this, the implementation of theory-based care models is recommended for increasing adherence, identifying the determinants or modifiers of adherence, and using patient-centered approaches to assess barriers to and facilitators of adherence [16, 21].
Studies in non-oncological populations show that common barriers to PFME are the lack of health insurance coverage and the belief of little benefit with performing exercises [22], forgetting how to perform them, or the fear of doing them wrongly [22, 23]; on the other hand, the reported facilitator was confidence in being able to perform the exercises [24]. Meanwhile, barriers for VD use are uncertainty about how and when to use it, considering it as a negative experience, lack of time or forgetfulness, doubts about its use, association with a sex toy, and need for privacy; among the facilitators for VD use are concern and care for stenosis, the belief that it will help, and the normalization of its use as part of medical treatments [25,26,27].
There is a need to deeply investigate these factors in the context of gynecologic cancer survivors as to foster adherence and improve clinical results. There is a scarcity of information specially when combining PFME and VD. The aim of this study is to explore the experience of gynecologic cancer survivors regarding barriers to and facilitators of adherence to a prehabilitation program to prevent PFD after radiotherapy.
Materials and methods
This is a qualitative study employing thematic analysis [28], which was reported following the guidelines of the Consolidated Criteria for Reporting Qualitative Studies (COREQ) [29]. This research was approved by the scientific ethics committee of the North Metropolitan Health Service (05/05/2017, folio AE nº 007/2017) and had the informed consent of all the participants. The information was treated anonymously, and the sensitive data of the participants were stored separately from the audio files, consents, and transcripts.
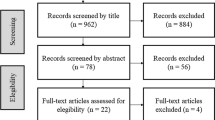
Semi-structured interviews were conducted with women participating in an educational program for the prevention of pelvic floor dysfunctions at the National Cancer Institute of Chile between August 2017 and September 2018. For inclusion in this study, they should be referred for pelvic radiation treatment, external beam, and/or brachytherapy, for gynecologic cancer. The women, aged 18–70, were first-time referrals for curative radiotherapy with or without previous or concomitant treatments, such as surgery and chemotherapy, and whose cognitive and functional capacity was sufficient to carry out their daily activities without dependence on other people (ECOG 0–1). The exclusion criteria were cancer stage IV, illiteracy, and observed vaginal prolapse that exceeded the hymenal area.
The program was based on sociocognitive theory [30, 31] and consisted of three face-to-face sessions and a 6-month follow-up. The first pre-radiotherapy face-to-face educational session was to instruct in the practice of home-based PFME, the delivery of a daily record booklet for registering PFME and VD use (Supplementary material), and instructional audio, which was sent to their mobile phone. The second face-to-face session was held approximately 1 month after radiotherapy. On that occasion, instructions were reinforced, as the correct performance of the exercises was verified, and a plastic cylindrical Berman Dilator Set® was given to each patient, which has four sizes of vaginal dilators and lubricant for domiciliary use. The third session was 3 months after the second and included only reinforcement. This protocol has previously been published [32, 33].
The interviews were conducted by a phone call performed by one interviewer (PAC) with training in the technique who wasn’t the treating professional. Each phone interview session took around 40 min. Participants were contacted at the end of the program after finishing the study protocol. Interviews were carried out, while new information appeared until data saturation was reached, following recommendations for qualitative studies with relatively homogeneous study populations and narrowly defined objectives [34,35,36]. An interview script was used based on the available knowledge on the topic, considering the following dimensions: [1] experience regarding the barriers to adherence to the practice of PFME; [2] experience regarding the barriers to adherence to the use of DV; [3] experience regarding the facilitators of adherence to the practice of PFME; [4] experience regarding facilitators of adherence to the use of DV; and [5] general experience in the program.
Participants
Considering all the women participating in the educational program (n = 56), an intentional theoretical sampling was carried out, selecting women with different degrees of adherence to the program. The level of adherence of the women was classified as “totally adherent” for those who attended all the face-to-face appointments and completed the study; “partially adherent,” for those who adhered to the practice of PFME but not to the use of DV; and “non-adherent,” for those who received the initial instructions but did not attend any subsequent sessions.
Analysis of the information
The analysis process considered the steps recommended by Braun and Clarke [28]. The interviews were audio-recorded and verbatim transcribed to facilitate the researchers’ immersion in the information and analysis. The information was incorporated into a database for thematic analysis performed manually and assisted by computer software NVivo12®.
Results
Eleven semi-structured interviews were conducted until the data was saturated, including women with different degrees of adherence. The participating women had an average age of 47.5 years (27–70 years), and most of them had a diagnosis of cervical cancer and at least 12 years of formal education (Table 1).
From the thematic analysis of the five explored dimensions, the information was grouped into five categories related to treatment, program, personal, social, and medical team. Nine barriers and nine facilitators were coded. In addition, four subcategories emerged in relation to the general experience in the program (Table 2).
Barriers to adherence to the practice of PFME and the use of VD
The adherent women perceived few barriers to the practice of exercises; some of them mentioned specific and temporary non-adherence due to some symptoms associated with discomfort secondary to oncological treatments. Fatigue, discouragement, and general malaise from radiotherapy or chemotherapy were the most frequently mentioned symptoms.
From the perspective of non-adherent women, their desertion of PFME was influenced by the misinformation of the procedures and lack of coordination with the team in charge of the program. Only indirectly did they manifest any personal responsibility in the decision not to attend. Regarding personal barriers, forgetfulness, loss of the instructional audio, and lack of time (due to work, assistance to other treatments, geographic distance, or family routines) were mentioned as factors that made adherence difficult.
Concerning the use of VD, women reported feeling fear of introducing a foreign element into their vagina in the context of aggressive disease and treatment; in addition, it reflected modesty/shame toward the device and its name, “vaginal dilator,” words that they avoided saying or forgot.
Finally, the absence of feedback from the medical team also negatively influenced the adherence to the program, being valued as a decisive factor when deciding whether or not to attend treatment.
Facilitators of adherence to the practice of PFME and use of VD
The facilitators assigned to the personal category highlighted that partially or fully adherent women were highly motivated. They reported that improved knowledge and well-observed results were an incentive to adhere. The availability of time appears as a facilitator, especially in women who were on medical leave or who could organize their daily routine to perform the exercises at home.
Some characteristics and resources of the program were mentioned as facilitators, for instance, the availability of audio with exercise instruction, remarked as a daily and easy-to-use resource, serving as a reminder and support to perform the exercises at home. In addition, they highlighted the clarity of the instructions and close relationship/rapport with the treating physical therapist, which reinforced commitment and reduced uncertainties and fears, generating a virtuous patient–caregiver alliance, even in those women whose advances were discreet.
In relation to the medical team, the physician feedback about PFME and VD was valued in the reports as a facilitator when it was present. We identified that the treating physician represents an authority in terms of health care, and his opinion was highly valued.
Finally, the desire to resume sexual life and the support of the partner were perceived as facilitators of adherence, especially when the partner showed interest in the procedures performed and encouraged the patient to persevere. The participation of the partner in a therapeutic context allowed to have a safe, intimate space, which reduced fears and expectations.
Program experience
The adherent women perceived that the program was a good experience and consider that it should be disseminated and accessible to other people. It is striking that three of them spontaneously reported having shared the instructional audio with relatives and friends, encouraging others to do PFME. They empowered themselves and became instructors of their peers, reaffirming with others the benefits of PFME and generating a virtuous circle of mutual feedback.
The strengthening of the couple’s relationship was another theme that emerged from their narratives; although it was not frequent, it had a connotation of intensity that is worth highlighting. In addition, as part of the experience in the program, they point out other benefits related to improving their body knowledge, validating the importance of exploring and knowing how their pelvic floor works and how to take care of it.
Finally, based on their experience in the program, some of them made recommendations to improve the program, aimed at the active integration of more actors into the process, in particular the medical team and the partner, as well as the consideration of other more easily accessible tools for older adults who do not use smartphones.
Discussion
This qualitative study contributes to the literature of the area by being one of the few to explore the barriers and facilitators of adherence to a program with PFME and VD to prevent pelvic floor dysfunctions among gynecological cancer women referred to radiotherapy. The main barriers to adherence were related to cancer treatment, lack of reinforcement by the medical team, and personal factors (forgetfulness, lack of time, modesty with the VD). Meanwhile, the main facilitators were personal (motivation, desire to resume sexual life), related to the program (positive results, good rapport with treating physical therapist), and social support (couple and medical team).
These results partially agree with previous studies. A systematic review published in 2017 showed strong evidence that the intention to participate, motivation, self-efficacy, and social support were predictive factors of adherence to physical therapy at home. However, it did not consider an oncological population or PFME [23]. Motivation and symptom improvement contributed to the permanence of the women in the program. A similar pattern was found in female non-cancer patients with urinary incontinence treated with PFME [21]. Regarding the facilitators to the use of VD, the review by Lee et al. (2018), in the oncological population, also agrees on the positive influence of motivation, expectation, and perceived symptoms improvement [27].
Considering adherence modifiers in the context of oncological disease, the role of the medical team becomes fundamental for patient’s adherence, revealing that the explicit interest of the treating physician regarding their rehabilitation can be a barrier when absent or a facilitator when present. This finding accounts for the doctor–patient relationship in the context of cancer. A qualitative study carried out in Brazil (2017) highlights that oncological patient expect dialogue, empathy, and kindness from the doctor, and they also tend to create more expectations in the relationship with the oncologist than with other health professionals: “The doctor is almost like a priest! He has to know how to guide his faithful!” [37].
The rapport established with the physiotherapist, the possibility of direct contact, and the information delivery method contributed to the adherence and safety feeling of the women in their daily lives, beyond the therapeutic space of the hospital treatment. These findings are consistent with another study in which women who had a closer interaction with health professionals adhered more to the use of VD [27].
Building an effective and empathetic therapeutic relationship is essential for adherence [23]. A collaborative bond motivated women to take charge of their health situation, adhering to interventions that they interpret as safe and beneficial for them. It has been shown that one of the barriers to the implementation of evidence-based programs is the lack of time and the high workload of physiotherapists, because it limits rapport. The symptoms improvement perceived by the adherent women highlight that person-centered care and good quality therapeutic communication are important for the success of the intervention, especially in the context of chronic and/or complex diseases such as cancer [38].
On the other hand, despite the fact that less than half of the women interviewed had a partner, their active and empathetic presence within the therapy was important, especially for VD adherence. This finding coincides with the results obtained from two similar qualitative studies [25, 39]. The results of a systematic review on the perception of the use of VD partially agree with our results, reporting as barriers to adherence that women felt uncomfortable, hard, annoying, and embarrassing [27]. However, in our study, the lack of understanding did not appear as a barrier, probably because the physical therapist spent more time instructing VD use and inserted it into their vagina, looking for the better fit size to start the therapy and reinforcing the patients’ confidence to use it. The shame for buying the VD was not reported in our study as it was free of cost and delivered in a discreet package.
In this study, the use of the VD was standardized as a treatment, not necessarily associated with sexual activity. It is very important to communicate this normalization even more in countries whose culture is still very conservative. A similar study with Australian women reported that the use of the vaginal dilator as a sex toy had a positive connotation for some women [25]. Consequently, it might be important to include in such preventative programs a discussion about patients’ taboos, including cultural and individual limiting beliefs regarding the proposed treatments.
Regarding the design of the program, the exercise audio facilitated the autonomous practice of PFME at home, contributing to obtain good therapeutic results with an intervention of only three face-to-face sessions in 6 months. This is relevant especially in the context of public health where resources are scarce, and it is imperative to design cost-effective care strategies, even more in times of health crisis such as the current COVID-19 pandemic, despite the fact that this study was implemented prior to this health situation.
Personal barriers such as forgetfulness and lack of time have been previously described in other studies on PFME [22], which might be associated with a lack of interest or sensitivity for caring for this part of the body. However, non-adherent women tended to externalize the causes of their desertion and did not declare their disinterest. On the other side, this study showed that some women felt empowered to share their learning and practice PFME with friends and family members, acting as an adherence facilitator. Shared learning should be considered for future implementations since patients can be references and learn from vicarious experience [40].
The planning and implementation of educational interventions in any health field should ideally be conceived from a theoretical perspective [41, 42]. In this approach, the sociocognitive theory was helpful in structuring the intervention. Although interventions based on theory do not have a guarantee of success, there is agreement that they guide implementation and achieve better clinical results [41, 43], with particular relevance in the context of adherence to physical therapy [41] and pelvic floor reeducation [8, 21]. This study could contribute to evidence-based practice by incorporating not only the aspects of the best available scientific evidence but also clinical expertise, the perspective of the user/patient, and the context [38].
One of the limitations of the study was the time elapsed between the interview and the last face-to-face contact session since, in the case of non-adherent women, it was greater than for adherent women. Moreover, the telephone interviews could have curtailed the possibility of having a more intimate space to deal with a sensitive issue in greater depth. In addition, the participants of this study received a basic plastic VD kit. Currently, there are more comfortable alternatives on the market, which could reduce the physical discomfort but are more expensive.
Based on the findings of this study, it is considered that the implementation of pelvic floor prehabilitation and reeducation programs based on PFME and VD in women with gynecologic cancer should consider temporary changes in symptoms throughout antineoplastic treatments, the incorporation of the partner in the therapeutic process, and the use of routine mobile applications, as well as the medical team’s commitment in the referral and motivation of patients. It is suggested to advance toward the investigation of the modifiers of adherence to physical therapy in other oncological populations, as well as the implementation and evaluation of pelvic floor reeducation programs based on theory in the male population, incorporating a look at the socio-structural factors involved.
Data availability
Data will be available upon request to the corresponding author by email.
References
Bray F, Ferlay J, Soerjomataram I, Siegel RL, Torre LA, Jemal A (2018) Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin 68(6):394–424. https://doi.org/10.3322/caac.21492
Asher A, Ng A, Engle J (2017) Principles of cancer rehabilitation. In Cardio-oncology: Principles, prevention and management. Elsevier Inc., pp 279–296. https://doi.org/10.1016/B978-0-12-803547-4.00019-7
Hofsjö A, Bergmark K, Blomgren B, Jahren H, Bohm-Starke N (2018) Radiotherapy for cervical cancer–impact on the vaginal epithelium and sexual function. Acta Oncol (Madr) 57(3):338–345. https://doi.org/10.1080/0284186X.2017.1400684
Ramaseshan AS, Felton J, Roque D, Rao G, Shipper AG, Sanses TVD (2018) Pelvic floor disorders in women with gynecologic malignancies: a systematic review. Int Urogynecol J 29(4):459–476. https://doi.org/10.1007/s00192-017-3467-4
Greear G, Lefkowits C, Parrillo LM, Flynn BJ (2016) Incontinence, voiding dysfunction, and other urologic complications after radiotherapy for gynecologic malignancies. Curr Bladder Dysfunct 11(2):88–97. https://doi.org/10.1007/s11884-016-0354-7
Schouten B, Van Hoof E, Vankrunkelsven P, Schrooten W, Bulens P, Buntinx F, et al (2016) Assessing cancer patients’ quality of life and supportive care needs: translation-revalidation of the CARES in Flemish and exhaustive evaluation of concurrent validity. BMC Health Serv Res 16(86). Available from: https://bmchealthservres.biomedcentral.com/track/pdf/, https://doi.org/10.1186/s12913-016-1335-4
Weare K (2015) Rehabilitation after gynecological cancer treatment. Int J Gynecol Obstet 131(Suppl 2):S164–6. https://doi.org/10.1016/j.ijgo.2015.06.015
Cacciari LP, Dumoulin C, Hay-Smith EJ (2019) Pelvic floor muscle training versus no treatment, or inactive control treatments, for urinary incontinence in women: a Cochrane systematic review abridged republication. Braz J Phys Ther 23:93–107. https://doi.org/10.1016/j.bjpt.2019.01.002
Dumoulin C, Alewijnse D, Bo K, Hagen S, Stark D, Van Kampen M, Herbert J, Hay-Smith J, Frawley H, McClurg D, Dean S (2015) Pelvic-floor-muscle training adherence: tools, measurements and strategies - 2011 ICS State-of-the-Science Seminar Research Paper II of IV. Neurourol Urodyn 34(7):615–621. https://doi.org/10.1002/nau.22794
Cerentini TM, Schlöttgen J, Viana da Rosa P, La Rosa VL, Vitale SG, Giampaolino P et al (2019) Clinical and psychological outcomes of the use of vaginal dilators after gynaecological brachytherapy: a Randomized Clinical Trial. Adv Ther 36:1936–49. https://doi.org/10.1007/s12325-019-01006-4
Kirchheiner K, Nout RA, Lindegaard JC, Haie-Meder C, Mahantshetty U, Segedin B et al (2016) Dose-effect relationship and risk factors for vaginal stenosis after definitive radio(chemo)therapy with image-guided brachytherapy for locally advanced cervical cancer in the EMBRACE study. Radiother Oncol 118(1):160–166. https://doi.org/10.1016/j.radonc.2015.12.025
Miccò M, Campitelli M, Sbarra M, Carra N, Barone R, Gui B et al (2020) DW-MRI predictive factors for radiation-induced vaginal stenosis in patients with cervical cancer. Clin Radiol 75(3):216–223. https://doi.org/10.1016/j.crad.2019.10.021
Miles T, Johnson N (2014) Vaginal dilator therapy for women receiving pelvic radiotherapy. Cochrane Database Syst Rev 9:CD007291
De Lima Matos SR, Cunha MLR, Podgaec S, Weltman E, Centrone AFY, Mafra ACCN (2019) Consensus for vaginal stenosis prevention in patients submitted to pelvic radiotherapy. PLoS One 14(8):1–15. https://doi.org/10.1371/journal.pone.0221054
Huffman LB, Hartenbach EM, Carter J, Rash JK, Kushner DM (2016) Maintaining sexual health throughout gynecologic cancer survivorship: a comprehensive review and clinical guide. Gynecologic Oncol 140:359–368. https://doi.org/10.1016/j.ygyno.2015.11.010
Dumoulin C, Hay-Smith J, Frawley H, McClurg D, Alewijnse D, Bo K et al (2014) consensus statement on improving pelvic floor muscle training adherence: International Continence Society 2011 State-of-the-Science Seminar. Neurourol Urodyn 2015:600–605. https://doi.org/10.1002/nau.22796
Lubotzky FP, Butow P, Hunt C, Costa DSJ, Laidsaar-Powell R, Carroll S et al (2019) A psychosexual rehabilitation booklet increases vaginal dilator adherence and knowledge in women undergoing pelvic radiation therapy for gynaecological or anorectal cancer: a randomised controlled trial. Clin Oncol 31(2):124–131. https://doi.org/10.1016/j.clon.2018.11.035
Jeffries SA, Robinson JW, Craighead PS, Keats MR (2006) An effective group psychoeducational intervention for improving compliance with vaginal dilation: a randomized controlled trial. Int J Radiat Oncol Biol Phys 65(2):404–411. https://doi.org/10.1016/j.ijrobp.2005.12.009
Law E, Kelvin JF, Thom B, Tom A, Carter J, Alektiar K et al (2015) Prospective study of vaginal dilator use adherence and efficacy following radiotherapy. Radiother Oncol 116(1):149–155. https://doi.org/10.1016/j.radonc.2015.06.018
World Health Organization (2003) Adherence to long-term therapies : evidence for action. World Health Organization. https://apps.who.int/iris/handle/10665/42682
Hay-Smith J, Dean S, Burgio K, McClurg D, Frawley H, Dumoulin C (2015) Pelvic-floor-muscle-training adherence “modifiers”: a review of primary qualitative studies - 2011 ICS State-of-the-Science Seminar research paper III of IV. Neurourol Urodyn 34(7):622–631. https://doi.org/10.1002/nau.22771
Washington BB, Raker CA, Sung VW (2011) Barriers to pelvic floor physical therapy utilization for treatment of female urinary incontinence. Am J Obs Gynecol 205(152):e1-9. https://doi.org/10.1016/j.ajog.2011.03.029
Essery R, Geraghty AWA, Kirby S, Yardley L (2017) Predictors of adherence to home-based physical therapies: a systematic review. Disabil Rehabil 39(6):519–534. https://doi.org/10.3109/09638288.2016.1153160
Sacomori C, Zomkowski K, dos Passos PI, Cardoso FL, Sperandio FF (2020) Adherence and effectiveness of a single instruction of pelvic floor exercises: a randomized clinical trial. Int Urogynecol J 31(5):951–959. https://doi.org/10.1007/s00192-019-04032-6
Bonner C, Nattress K, Anderson C, Carter J, Milross C, Philp S et al (2012) Chore or priority? Barriers and facilitators affecting dilator use after pelvic radiotherapy for gynaecological cancer. Support Care Cancer 20(10):2305–2313. https://doi.org/10.1007/s00520-011-1337-z
Vermeer WM, Bakker RM, Kenter GG, Stiggelbout AM, Ter Kuile MM (2016) Cervical cancer survivors’ and partners’ experiences with sexual dysfunction and psychosexual support. Support Care Cancer 24:1679–1687. https://doi.org/10.1007/s00520-015-2925-0
Lee Y (2018) Patients’ perception and adherence to vaginal dilator therapy: a systematic review and synthesis employing symbolic interactionism. Patient Prefer Adherence 12:551–60. https://doi.org/10.2147/PPA.S163273
Braun V, Clarke V, Bussey K, Bandura A, Carnagey NL, Anderson CA et al (2006) Using thematic analysis in psychology. Psychiatr Q 3:77–101. https://doi.org/10.1191/1478088706qp063oa
Tong A, Sainsbury P, Craig J (2007) Consolidated criteria for reporting qualitative research (COREQ): a 32-item checklist for interviews and focus groups. Int J Qual Heal Care 19(6):349–357
Bandura A (2001) Social cognitive theory: an agentic perspective. Annu Rev Psychol 52:1–26
Bandura A (1998) Health promotion from the perspective of social cognitive theory. Psychol Heal 13(4):623–649
Sacomori C, Araya-Castro P, Diaz-Guerrero P, Ferrada IA, Claudia Martínez-Varas A, Zomkowski K (2020) Pre-rehabilitation of the pelvic floor before radiation therapy for cervical cancer: a pilot study. Int Urogynecol J 31(11):2411–2418. https://doi.org/10.1007/s00192-020-04391-5
Araya-Castro P, Sacomori C, Diaz-Guerrero P, Gayán P, Román D, Sperandio FF (2020) Vaginal dilator and pelvic floor exercises for vaginal stenosis, sexual health and quality of life among cervical cancer patients treated with radiation: clinical report. J Sex Marital Ther 46(6):513–27. https://doi.org/10.1080/0092623X.2020.1760981
Ando H, Cousins R, Young C (2014) Achieving saturation in thematic analysis: development and refinement of a codebook. Compr Psychol 3(4):1–7
Hennink M, Kaiser BN. Sample sizes for saturation in qualitative research: a systematic review of empirical tests. Soc Sci Med [Internet]. 2022;292:114523. Available from: https://doi.org/10.1016/j.socscimed.2021.114523
Francis JJ, Johnston M, Robertson C, Glidewell L, Entwistle V, Eccles MP et al (2010) What is an adequate sample size? Operationalising data saturation for theory-based interview studies. Psychol Heal 25(10):1229–1245
Bastos LOA, de Andrade EN, Andrade EO (2017) The doctor-patient relationship in oncology: a study from the patient’s perspective. Rev Bioética 25(3):563–576. https://doi.org/10.1590/1983-80422017253213
Scurlock-Evans L, Upton P, Upton D (2014) Evidence-based practice in physiotherapy: a systematic review of barriers, enablers and interventions. Physiother 100(3):208–19. https://doi.org/10.1016/j.physio.2014.03.001
Bakker RM, Vermeer WM, Creutzberg CL, Mens JWM, Nout RA, ter Kuile MM (2015) Qualitative accounts of patients’ determinants of vaginal dilator use after pelvic radiotherapy. J Sex Med 12(3):764–773. https://doi.org/10.1111/jsm.12776
Bandura A (2005) The evolution of social cognitive theory. In: Smith KG, Hitt MA (eds) Great minds in management. Oxford University Press, Oxford, pp 9–35
Sirur R, Richardson J, Wishart L, Steven H (2009) The role of theory in increasing adherence to prescribed practice. Physiother Can 61:68–77
Prestwich A, Webb TL, Conner M (2014) Using theory to develop and test interventions to promote changes in health behaviour: evidence, issues, and recommendations. Curr Opin Psychol 5:1–5. https://doi.org/10.1016/j.copsyc.2015.02.011
National Cancer Institute, NIH. Theory at a glance: A guide for health promotion practice. US Government Printing Office, Washington, DC. Available at https://cancercontrol.cancer.gov/sites/default/files/2020-06/theory.pdf
Funding
This work was supported by I Concurso de Investigacion Interno de la Universidad Bernardo O’Higgins (Ref. UBO/VRIP 170202).
Author information
Authors and Affiliations
Contributions
PAC and CS contributed to the study conception and design. Material preparation and data collection were performed by PAC. Data analysis was performed by PAC and SR. The first draft of the manuscript was written by PAC, and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval
This research was approved by the scientific ethics committee of the North Metropolitan Health Service (05/05/2017, folio AE nº 007/2017), Santiago, Chile.
Consent to participate and for publication
The authors affirm that participants provided informed consent to participate and to publish the results of the research.
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Araya-Castro, P., Roa-Alcaino, S., Celedón, C. et al. Barriers to and facilitators of adherence to pelvic floor muscle exercises and vaginal dilator use among gynecologic cancer patients: a qualitative study. Support Care Cancer 30, 9289–9298 (2022). https://doi.org/10.1007/s00520-022-07344-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00520-022-07344-4