Abstract
Purpose
Both infertility and erectile dysfunction (ED) are known long-term consequences of cancer treatment in young male cancer survivors. In the present study, we aimed to assess whether sperm quality and sexual function in male cancer survivors are associated.
Methods
In this prospective study, n = 244 patients male cancer survivors who underwent sperm analysis and cryopreservation between 2008 and 2018 prior to the initiation of gonadotoxic treatment were invited. In total n = 50 had a follow-up sperm analysis and completed two questionnaires, the Aging Males’ Symptom Scale (AMS) and the International Index of Erectile Function (IIEF-EF). Differences between the individual parameters were analyzed using the Wilcoxon or Mann Whitney test.
Results
Azoospermia was present in n = 16/50 (32.0%) patients at time of follow-up. ED occurred in n = 9/43 (20.9%) patients and was observed more frequently in patients with oligo- or azoospermia than in those with normospermia, even though this association was not statistically significant. Sperm parameters (total sperm count, sperm concentration, progressive motility) did not differ between time of cryopreservation and time of follow-up. Mean total, somatic, psychological, and sexual AMS score was 23.6, 9.9, 6.6, and 6.8, respectively. Mean total IIEF-EF score was 27.3, indicating mainly mild ED.
Conclusions
More than one-third of cancer patients suffered from azoospermia, and ED was primarily present in this subgroup. We recommend implementing the screening of sexual dysfunction in the annual sperm testing that should be offered to all men after gonadotoxic treatment. Our study highlights the importance of counseling young cancer patients on both aspects—future infertility and sexual function—prior to treatment and at follow-up visits.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Survival rates of young cancer patients are constantly rising, reaching 5-year survival rates of up to 80–98% [1, 2], depending on cancer type and stage. This creates a new group of patients: cancer survivors who face the long-term consequences of their treatment (surgery, chemotherapy, immunotherapy, and/or radiotherapy), which include transient or permanent infertility [3]. During the last decades, the awareness of clinicians for this problem has risen. As a result, sperm cryopreservation prior to the initiation of gonadotoxic treatment is routinely offered to male cancer patients to fulfill their desire for children in their later lives [4].
However, fertility is only one facet of sexual function that is possibly impacted by cancer therapies, and few studies have aimed to understand the association between cancer and sexual function besides fertility, such as erectile dysfunction (ED). Male cancer survivors frequently suffer from ED [5], which depends on the type of cancer, and treatment regimes, but also age and comorbidities [6,7,8]. In testicular cancer patients, for example, the rate of ED was reported to be as high as 37% [9]. A Danish testicular cancer cohort study reported different rates and manifestations of ED according to the applied therapies. ED was described in men who underwent radiotherapy, BEP (bleomycin, etoposide, and platinum) chemotherapy with subsequent surgery, or more than one line of treatment. The latter group also reported orgasmic dysfunction, while the group treated with radiotherapy also reported decreased sexual satisfaction [10].
The varying prevalence and manifestation of ED in cancer survivors is partially explained by the multifactorial pathomechanisms involved. Surgery, particularly retroperitoneal lymphadenectomy (RPLND), and radiation may lead to neural damage and impede erection and ejaculation [11]. Due to Leydig cell damage, cancer treatment can further lead to hypoandrogenism, which may impair sexual function, even though the exact correlation needs to be further explored. Low testosterone levels have been reported in up to 26% of testicular cancer survivors [12, 13]. Besides the potential impact on sexual function, male hypoandrogenism also predisposes to the development of metabolic and cardiovascular diseases [14], which are again risk factors for ED. Besides biological mechanisms, the psychological impact of being diagnosed with and treated for cancer is another important—yet often neglected—factor [15].
A possible association between sperm quality and sexual function in male cancer survivors remains unclear. In infertile couples without a history of cancer, ED prevalence has been reported to increase as a function of sperm quality impairment [16]. It is plausible that a similar association exists for cancer survivors. Better understanding the joint occurrence of poor sperm quality and ED in cancer survivors could help clinicians to identify patients at risk.
In the present study, we aimed to assess the association of sperm quality and sexual function in cancer survivors.
Material and methods
Study population
This prospective study included patients who had their sperm samples cryopreserved between January 1, 2008, and July 1, 2018, at a tertiary hospital. All patients were invited for a follow-up visit including a novel sperm testing as well as two questionnaires. Initially, sperm cryopreservation had been performed immediately after the diagnosis of malignant or benign diseases that required surgery or, potentially, gonadotoxic treatment. Medical history, sociodemographic parameters, and laboratory data (i.e., age, body mass index (BMI), as well as the levels of thyroid-stimulating hormone (TSH), follicle-stimulating hormone (FSH), and luteinizing hormone (LH)) were obtained. Malignant diseases were classified according to the international guidelines, such as Ann Arbor staging (for hematological malignancies) or Union Internationale Contre le Cancer stadium (UICC), for testicular malignancies. The study was approved by the Local Review Board (IRB Number 1016/2020), and all patients gave written informed consent before recruitment.
Questionnaires
Two questionnaires on health-related quality of life (HRQoL) and sexual functioning—the Aging Males’ Symptom Scale (AMS) [17, 18] and the International Index of Erectile Function (IIEF-EF) [19, 20]—were completed by the participants at the time of follow-up sperm sampling. The AMS (a) assess symptoms of aging (independent from those which are disease-related) between groups of males under different conditions, (b) evaluates the severity of symptoms over time, and (c) measures changes pre- and post-androgen replacement therapy. It was developed in response to the lack of standardized scales to measure the severity of aging symptoms and their impact on HRQoL in males, specifically. The AMS scale consists of 17 items in three domains (psychological, somatic, and sexual) on a scale of 1–5. The total score for each of the domains is based on adding up the scores of the items of the respective domain. The cumulative score ranges from 17 to 85 points. The severity of the symptoms is defined as: no/low (17–26 points), mild (27–36 points), moderate (37–49 points), and severe (≥ 50 points). Sexual function can be evaluated by the IIEF-EF. The six items on the IIEF-EF include detailed questions concerning erection frequency, erection firmness, penetration ability, maintenance frequency, maintenance ability, and erection confidence. Participants needed to report sexual activity at least once during the 4 weeks before responding to the questions. Each item was based on a 5-point Likert scale. For each subject, the responses of all six items of the IIEF-EF were summed to a total EF score, with a range from 6 to 30. Scores lower than 26 indicated the presence of erectile dysfunction. The severity of ED was classified into five categories: no ED (EF score 26 to 30), mild (EF score 22 to 25), mild to moderate (EF score 17 to 21), moderate (EF score 11 to 16), and severe (EF score 6 to 10). Moreover, patients were asked concerning family planning including questions about fatherhood before and after gonadotoxic treatment and the total number of children.
Sperm analysis
Initial sperm samples were obtained by masturbation-induced ejaculation before gonadotoxic treatment. The time of ejaculation abstinence was recorded with the recommendation of an interval of at least 2–3 days. However, for urgent cases, sperm storage was performed regardless of the abstinence. Men with low total sperm counts were advised to provide one or more additional samples, again with an optimal abstinence time of 2–3 days in order to obtain sufficient numbers of sperms for cryopreservation. At the time of follow-up, another sperm sample was obtained by masturbation. Normozoospermia was defined for all samples in accordance with the 2010 WHO criteria (sperm concentration ≥ 15 million/mL, progressive motility ≥ 32%, and ≥ 4% normal morphology). Sperm samples obtained before 2010 (2008–2010) were evaluated following the 1999 WHO criteria and adjusted to the criteria of 2010.
Statistics
Analysis of variance (ANOVA) was performed for normally distributed raw data, which was presented as mean ± standard deviation (SD). For non-normal data distribution, the differences between the individual parameters of the groups were analyzed using the Wilcoxon or Mann Whitney test and presented as median (interquartile range (IQR)). To prevent alpha error accumulation, a Bonferroni correction was applied for multiple comparisons. To compare means, the paired t-test was applied. The Spearman’s rank correlation analysis was used to identify correlations between different parameters. A significance level of α = 0.05 was assumed for all statistical evaluations. The statistical analysis was conducted using IBM SPSS Statistics for Windows, Version 26.0 (IBM Corp., released in 2019; Armonk, NY: IBM Corp).
Results
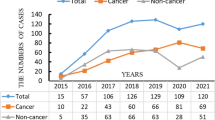
In total, n = 244 male cancer patients were eligible for the study inclusion as they underwent sperm cryopreservation before gonadotoxic treatment. At the time of screening, n = 27 patients had died of their underlying disease, and n = 77 were living abroad or in another state, leaving n = 126 patients for possible participation. Finally, n = 50 (39.6%) male cancer survivors followed the invitation to participate in this study and a follow-up visit including sperm sampling and two questionnaires. Demographic data are shown in Table 1. Median age (IQR) at time of cancer diagnosis and follow-up was 25.0 (19.8–29.0) and 30.0 (26.8–35.0) years, respectively, resulting in a median follow-up time of 64.0 (45.3–106.8) months. In sum, n = 24 (48.0%) patients suffered from hematological, nineteen (38.0%) from testicular, and seven from other malignancies (e.g., solid tumors, sarcoma). Most of the patients (84.0%) received chemotherapy, and 16.0% underwent radiotherapy or surgery. Out of the 19 patients with testicular malignancy, 15 underwent hemicastration alone, while four patients additionally underwent retroperitoneal lymphadenectomy. Two patients with retroperitoneal lymphadenectomy showed azoospermia without signs of erectile dysfunction at time of follow-up. Of note, these patients comprise a very small group not allowing interpretation of results. Patients with other malignancies underwent orthopedic surgeries of the lower extremity (n = 2) or no surgery (n = 5), whereas patients with hematological diseases underwent no surgery.
The mean total AMS score was 23.6 (9.3) indicating no/mild symptoms of aging. 15.9% of men experienced age-related symptoms. Mean somatic, psychological, and sexual AMS score was 9.9 (4.5), 6.6 (2.5), and 6.8 (3.5), respectively. Mean total IIEF-EF score was 27.3 (3.2), indicating the presence of ED in n = 9/43 (20.9%) of patients. We did not find a significant difference in the presence of ED between patients with hematological malignancies (n = 4/20, 20.0%) and patients with testicular malignancies (n = 4/17, 23.5%, p = 0.55). Also, there was no difference between normospermic and azoospermic patients with regard to ED/age-related symptoms.
Azoospermia and pathospermia were present in n = 16 (32.0%) and n = 21 (42.0%), respectively, according to the WHO 2010 criteria at the time of follow-up. Significantly more patients showed pathospermia at time of follow-up (n = 21, 42.0%) versus n = 13 (28.3%) at time of diagnosis (p = 0.006). When dividing the patients into the two subgroups normo- and pathospermia, we could not identify any significant differences in the presence/grade of ED, scores in the AMS, or other clinical parameters such as BMI, fatherhood at the time of diagnosis, or follow-up (Table 2). When comparing the single sperm parameters between the time of diagnosis and time of follow-up, no significant differences were identified (Table 3).
While initially only n = 2/42 (4.8%) patients reported fatherhood, n = 8/42 (19.0%) patients had a child at time of follow-up. At the same time, n = 25/41 (61.0%) patients expressed a desire to have children. Six patients achieved a spontaneous pregnancy within 5 years after cryopreservation, and three patients used the cryopreserved sperm for ART at our department.
Discussion
Our study shows a high prevalence of ED in young male cancer survivors, affecting more than 20% of the patients in our cohort. To our knowledge, our study is the first to assess the correlation between sperm quality and sexual function in cancer survivors. ED was observed more frequently in patients with oligo- or azoospermia than in those with normospermia, even though this association was not statistically significant. Almost one-third of the patients suffered from azoospermia at the time of follow up. At the same time, more than 60% expressed the desire to have children, emphasizing the importance of routine sperm cryopreservation prior to the initiation of gonadotoxic treatment.
In previous studies, the frequency of sexual dysfunction in cancer survivors varies widely. In our cohort, hematological malignancies accounted for almost half of the cases, showing an ED rate of 20%, similar to the rate described by Eeltink et al. for male Hodgkin lymphoma survivors [7]. In testicular cancer survivors, the prevalence of ED was reported to be higher, reaching up to 37% [9]. In our study, in this subgroup, ED occurred in 23.5%, confirming a higher prevalence in testicular cancer survivors, even though the difference between the two diagnostic groups did not reach statistical significance. The lower prevalence in our testicular cancer patients might be related to a different composition regarding cancer stage.
Another important factor influencing the probability of develo** ED is the therapeutical approach chosen. For example, different chemotherapeutical regimens seem to harm sexual function to varying extent. Eeltink et al. described lower IIEF-EF scores in male Hodgkin Lymphoma survivors treated according to the BEACOPP regimen than in those treated with doxorubicin, bleomycin, vinblastine, and dacarbazine [7]. In our cohort, 84% of all patients received chemotherapy, most frequently including cyclophosphamide. Comparing patients who had received a regime containing cyclophosphamide or cisplatin with those who were treated according to regimes free from these agents, we could not observe a difference in the ED rate, being 25% in both groups. Of note, the sample size might be too small for further interpretation.
Independently of cancer type, most studies described a correlation between age at cancer diagnosis and the prevalence or degree of sexual dysfunction, with an increased risk of persisting sexual problems for older patients [6, 8, 21]. This may partially be explained by the fact that sexual activity in general decreases with advancing age. Moreover, older patients suffer from a greater number of comorbidities, which may also influence sexual function directly [8, 21]. However, since our cohort consisted primarily of young patients under the age of 35 years, cases of ED observed in this study are unlikely to be driven by patient’s age or pre-existing comorbidities.
Besides the rather few studies demonstrating sexual dysfunction in cancer survivors, it has long been known that cancer treatments are potentially gonadotoxic and may lead to infertility. Nevertheless, the possible correlations between these two aspects of sexuality—e.g., sexual function and sperm quality—in cancer survivors have not been studied in detail so far. This is surprising, especially as in infertile couples without cancer history, an association between severity of sperm quality impairment and sexual function has been described by Lotti et al. in 2016 [16]. In fact, our data showed a similar trend for male cancer survivors, as those with oligo- or azoospermia showed lower ED scores than those with normospermia.
In our study, we primarily aimed to assess whether there is an association between sperm quality and sexual function in cancer survivors. The observed relationship is multifaceted, with several potential causes contributing. These include damage of testosterone-producing Leydig cells or local nerves, concomitant with germ cell damage, both induced by chemo- and radiotherapy, but also cancer localization and stage as well as psychological aspects.
In the study by Lotti et al., participants knew about their semen quality before answering the questionnaires assessing sexual function. This is a potential bias, as sexual function is strongly associated with psychological aspects. For infertile patients without a cancer history, sexual dysfunction following diagnosis of male factor infertility has been reported [22, 23]. The strong psychological association between fertility and sexuality is also highlighted by an interview study by Frederick et al., in which more than half of the included male childhood cancer survivors spontaneously expressed concerns about their fertility when asked about their sexual function [15]. Other studies found a higher incidence of male sexual dysfunction in patients suffering of anxiety disorders, in particular post-traumatic stress disorder (PTSD) [24,25,26,27]. Cancer has lately been recognized as one possible stressor inducing PTSD, with a prevalence of PTSD between 7 and 75% among cancer patients [28,29,30,31]. On the other hand, there is evidence to support that stress has a negative effect on semen quality in healthy men [32, 33]. In our study, we tried to reduce the bias linked to the psychological aspects by informing the participants about the results of their follow-up sperm analysis only once they had completed the two questionnaires. Nevertheless, they had been informed about their semen quality at time of cryopreservation, a knowledge that may have influenced their ED scores. It remains therefore unclear whether poor semen quality and ED are independently associated or whether the psychological consequences of knowing about one’s infertility led to ED. Future studies should therefore concentrate on elucidating the exact pathophysiological inter-relations between stress, semen quality, and erectile dysfunction, including more specific questionnaires on patients’ psychological status.
A strength of the study is that all sperm analyses were performed in the same IVF laboratory according to the WHO criteria, reducing the inter-observer variability. With AMS and IIEF-EF, we used validated questionnaires to evaluate ED. Reported scores have a high probability to reflect the long-term outcomes of these young patients, as the median follow-up time was as long as 5 years after cancer diagnosis and sperm cryopreservation.
A limitation of our study consists in the small sample size, which did not allow us to reach statistical significance for small effect sizes. Another aspect that—like in most other studies concerning ED in cancer survivors—could not be assessed regards sexual function before cancer diagnosis and treatment. Therefore, it remains unclear to what extent the reported sexual dysfunction is imputable to the disease and/or therapy. While in previous studies testicular cancer patients have been reported to show lower sperm count already at pre-treatment sperm analysis [34], little is known about the sexual function at that point. In order to reach a better understanding of the causal relationship between cancer, cancer treatment, and ED, future studies should assess the prevalence of ED at cancer diagnosis and compare it with the ED rates after completion of treatment.
Another possible limitation of our study is given by the lack of an age-matched control group. In fact, the reported prevalence of ED in the general population varies widely as a function of sociocultural context. In Germany, presenting a comparable sociocultural context, the prevalence of erectile problems in the general population aged between 26 and 35 years was reported to be as low as 7% [35]. The large difference to the prevalence we observed in cancer survivors of the same age group highlights the detrimental impact of cancer diagnosis and treatment on sexual function.
Conclusion
Overall, our study highlights the importance of counseling young cancer patients not only with regard to potential infertility, but also taking potential sexual problems into account. Given the high prevalence and the importance for the quality of life, clinicians should screen for sexual dysfunction in all male cancer survivors, especially in those presenting with oligo- or azoospermia. We recommend implementing the screening of sexual dysfunction in the annual sperm testing that should be offered to all men after gonadotoxic treatment. Future studies should investigate the association of semen quality and sexual function in larger cohorts, allowing to control for age, type of cancer, stage at diagnosis, and applied treatment.
Data availability
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
Code availability
The code generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
References
Stokes W, Amini A, Maroni PD et al (2017) Patterns of care and survival outcomes for adolescent and young adult patients with testicular seminoma in the United States: a National Cancer Database analysis. J Pediatr Urol 13:386.e1-386.e7
Tabakin AL, Shinder BM, Kim S et al (2020) Retroperitoneal lymph node dissection as primary treatment for men with testicular seminoma: utilization and survival analysis using the National Cancer Data Base, 2004–2014. Clin Genitourin Cancer 18:e194–e201
Mulder RL, Font-Gonzalez A, Green DM et al (2021) Fertility preservation for male patients with childhood, adolescent, and young adult cancer: recommendations from the PanCareLIFE Consortium and the International Late Effects of Childhood Cancer Guideline Harmonization Group. Lancet Oncol 22:e57–e67
Oktay K, Harvey BE, Partridge AH et al (2018) Fertility preservation in patients with cancer: ASCO clinical practice guideline update. J Clin Oncol 36:1994–2001
van Iersel L, Li Z, Chemaitilly W et al (2018) Erectile dysfunction in male survivors of childhood cancer. JAMA Oncol 4:1613–1616
Bersvendsen HS, Haugnes HS, Dahl AA et al (2020) Sexual function in long-term male lymphoma survivors after high-dose therapy with autologous stem-cell transplantation. Bone Marrow Transplant 55:891–905
Eeltink CM, Lissenberg-Witte BI, Incrocci L et al (2020) Self-reported sexual function in sexually active male hodgkin lymphoma survivors. Sex Med Today 8:428–435
Sun V, Grant M, Wendel CS et al (2016) Sexual function and health-related quality of life in long-term rectal cancer survivors. J Sex Med 13:1071–1079
Pallotti F, Petrozzi A, Cargnelutti F et al (2019) Long-term follow up of the erectile function of testicular cancer survivors. Front Endocrinol 10:196
Bandak M, Lauritsen J, Johansen C et al (2018) Sexual function in a nationwide cohort of 2,260 survivors of testicular cancer after 17 years of followup. J Urol 200:794–800
Kenney LB, Antal Z, Ginsberg JP et al (2018) Improving male reproductive health after childhood, adolescent, and young adult cancer: progress and future directions for survivorship research. J Clin Oncol 36:2160–2168
Lackner JE, Koller A, Schatzl G et al (2009) Androgen deficiency symptoms in testicular cancer survivors are associated with sexual problems but not with serum testosterone or therapy. Urology 74:825–829
Tal R, Stember DS, Logmanieh N et al (2014) Erectile dysfunction in men treated for testicular cancer. BJU Int 113:907–910
La Vignera S, Cannarella R, Duca Y et al (2019) Hypogonadism and sexual dysfunction in testicular tumor survivors: a systematic review. Front Endocrinol 10:264
Frederick NN, Recklitis CJ, Blackmon JE, Bober S (2016) Sexual dysfunction in young adult survivors of childhood cancer. Pediatr Blood Cancer 63:1622–1628
Lotti F, Corona G, Castellini G et al (2016) Semen quality impairment is associated with sexual dysfunction according to its severity. Hum Reprod 31:2668–2680
Heinemann LAJ, Zimmermann T, Vermeulen A, Thiel C, Hummel W (1999) A new ‘aging males’ symptoms’ rating scale. Aging Male 2(2):105–114. https://doi.org/10.3109/13685539909003173
Moore C, Huebler D, Zimmermann T et al (2004) The Aging Males’ Symptoms scale (AMS) as outcome measure for treatment of androgen deficiency. Eur Urol 46:80–87
Rosen RC, Riley A, Wagner G et al (1997) The international index of erectile function (IIEF): a multidimensional scale for assessment of erectile dysfunction. Urology 49:822–830
Cappelleri JC, Rosen RC, Smith MD et al (1999) Diagnostic evaluation of the erectile function domain of the International Index of Erectile Function. Urology 54:346–351
Greaves P, Sarker S-J, Chowdhury K et al (2014) Fertility and sexual function in long-term survivors of haematological malignancy: using patient-reported outcome measures to assess a neglected area of need in the late effects clinic. Br J Haematol 164:526–535
Bechoua S, Hamamah S, Scalici E (2016) Male infertility: an obstacle to sexuality? Andrology 4:395–403
Jamil S, Shoaib M, Aziz W, Ather MH (2020) Does male factor infertility impact on self-esteem and sexual relationship? Andrologia 52:e13460
Velurajah R, Brunckhorst O, Waqar M et al (2021) Erectile dysfunction in patients with anxiety disorders: a systematic review. Int J Impot Res. https://doi.org/10.1038/s41443-020-00405-4
Bird ER, Piccirillo M, Garcia N et al (2021) Relationship between posttraumatic stress disorder and sexual difficulties: a systematic review of veterans and military personnel. J Sex Med 18:1398–1426
Wang S-C, Chien W-C, Chung C-H et al (2021) Posttraumatic stress disorder and the risk of erectile dysfunction: a nationwide cohort study in Taiwan : PTSD and erectile dysfunction. Ann Gen Psychiatry 20:48
Bulut EC, Ertaş K, Bulut D, et al (2021) The effect of COVID-19 epidemic on the sexual function of healthcare professionals. Andrologia 53:e13971
Dahl AA, Østby-Deglum M, Oldenburg J et al (2016) Aspects of posttraumatic stress disorder in long-term testicular cancer survivors: cross-sectional and longitudinal findings. J Cancer Surviv 10:842–849
Cordova MJ, Riba MB, Spiegel D (2017) Post-traumatic stress disorder and cancer. Lancet Psychiatry 4:330–338
Alkan A, Guc ZG, Senler FC et al (2016) Breast cancer survivors suffer from persistent postmastectomy pain syndrome and posttraumatic stress disorder (ORTHUS study): a study of the palliative care working committee of the Turkish Oncology Group (TOG). Support Care Cancer 24:3747–3755
Selvi I, Basar H (2020) Subcapsular orchiectomy versus total orchiectomy and LHRH analogue in the treatment of hormone-sensitive metastatic prostate cancer: a different perspective in evaluation of the psychosocial effects. Support Care Cancer 28:4313–4326
Hall E, Burt VK (2012) Male fertility: psychiatric considerations. Fertil Steril 97:434–439
Nordkap L, Jensen TK, Hansen ÅM, et al (2016) Psychological stress and testicular function: a cross-sectional study of 1,215 Danish men. Fertil Steril 105:174-87.e1–2
Vomstein K, Reiser E, **gera GM et al (2021) Sperm banking before gonadotoxic treatment: is it worth the effort? Asian J Androl. https://doi.org/10.4103/aja.aja_16_21
Briken P, Matthiesen S, Pietras L et al (2020) Estimating the prevalence of sexual dysfunction using the new ICD-11 guidelines. Dtsch Arztebl Int 117:653–658
Funding
Open access funding provided by University of Innsbruck and Medical University of Innsbruck.
Author information
Authors and Affiliations
Contributions
ER: Conceptualization, methodology, validation, writing (original draft), visualization, and writing (review and editing). AZ: Methodology, writing (original draft), writing (review and editing), and project administration. KV: Conceptualization, methodology, validation, data curation, writing (original draft), visualization, and writing (review and editing. GMP: Methodology and writing (review and editing). ES: Data curation. ST: Methodology. BT: Conceptualization, resources, supervision, and writing (review and editing).
Corresponding author
Ethics declarations
Ethics approval
The study was approved by the Local Review Board (IRB Number 1016/2020).
Consent to participate
Informed consent was obtained from all individual participants included in the study.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Reiser, E., Zippl, A.L., Vomstein, K. et al. Sexual function in male cancer survivors is not correlated to sperm quality. Support Care Cancer 30, 5231–5237 (2022). https://doi.org/10.1007/s00520-022-06957-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00520-022-06957-z