Abstract
Vaccines represent the most important medical evolution in the last two centuries allowing prevention and formally eradication of a wide number of infectious diseases. Safety and effectiveness are main issues that still require an open discussion. A few clinical reports described a critical temporal relationship between vaccination and acute nephrotic syndrome, indirectly suggesting an association. For this review, the literature was reviewed to identify articles reporting associations of nephrotic syndrome with vaccines against a vast array of infectious diseases (including bacteria, virus and Sars-Cov-2). As specific aims, we evaluated effectiveness and safety in terms of occurrence of either “de novo” nephrotic syndrome in health subjects or “relapse” in those already affected by the disease. In total, 377 articles were found; 166 duplicates and 71 non-full text, animal studies or non-English language were removed. After excluding another 50 articles not containing relevant data on generic side effects or on relapses or new onset nephrotic syndrome, 90 articles met the search criteria. Overall, studies reported the effect of vaccines in 1015 patients, plus 4 nationwide epidemiologic investigations. Limited experience on vaccination of NS patients with measles, mumps, and rubella live attenuated vaccines does not allow any definitive conclusion on their safeness. VZV has been administered more frequently without side effects. Vaccines utilizing virus inactivated, recombinant, and toxoid can be utilized without risks in NS. Vaccines for influenza reduce the risk of infections during the pandemic and are associated with reduced risk of relapse of NS typically induced by the infection. Vaccines for SARS-CoV-2 (all kinds) offer a concrete approach to reduce the pandemic. “De novo” NS or recurrence are very rare and respond to common therapies.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The use of vaccines in nephrotic syndrome (NS) is a timely topic, discussed over many years. Patients with NS are, in fact, at high risk of develo** serious infectious complications based on immune-depression arising from hypogammaglobulinemia, urinary loss of complement factors, and immunosuppressive agents [1, 2]. Vaccines are the adequate answer to prevent infections provided that they achieve a sufficient titer of specific antibodies in circulation.
Safety and effectiveness are main issues that still require an open discussion. This is particularly true after the COVID pandemic that has re-proposed these questions in relation to the new anti-COVID mRNA formulations. Safety is particularly relevant to live attenuated preparations since patients may be exposed to the risk of develo** viral infection from the vaccine strains [3]. A second concern is about the possibility that post-vaccine serum conversion is limited by the presence of proteinuria and/or for the concomitance of immune suppressive therapies [4, 5]. Finally, vaccines have been proposed as triggers of idiopathic NS, either de novo episodes or recurrence based on case reports and association studies, a possibility that is critical in children for the intuitive reason that most vaccines are administered in childhood. Unfortunately, we lack a numerically comparable control population of children who did not receive vaccination since common vaccinations usually involve about 90–95% of children in Western countries.
We here present results deriving from a comprehensive review of the literature on effectiveness and safety of vaccines, including the previous suggested association with de novo or relapses of NS. A description of vaccine categories, types of production, or their administration precedes the analysis of data. The limited world-wide indications by deputed national organizations of public health for vaccination are presented at the end.
Vaccine categories
Vaccines may be classified in relation to the status of the antigen administered and include live, live attenuated, and inactivated virus/bacteria. They are prepared from purified crude or recombinant virus pool and may be conjugated with proteins or polysaccharides. Live vaccines (mycobacterium) should not be considered for their toxicity.
The live attenuated category includes Varicella, Measles, Mumps, rubella, Polio-Sabin, Typhoid, Yellow fever. They are produced by attenuating the power of living strains and are available as monovalent preparations or as part of combined formulations: measles–mumps (MM), measles–mumps–rubella (MMR), measles–mumps–rubella–varicella (MMRV).
Inactivated vaccines are simple killed virus/bacteria and include Hepatitis-A, Polio-Salk, Influenza, Papilloma virus, Rabies; a few of these are available as conjugated with proteins or polysaccharides (Haemophilus influenzae, Pneumococcal and Typhoid). Vaccines for Streptococcus pneumoniae are the most representative of this category since infections induced by Streptococcus pneumoniae represent the major cause of morbidity and mortality in children under 5 years [6]. Vaccines for pneumococcus exist as protein conjugated (PPV) and more recently as polysaccharide conjugated (PCV). PCV7 was first introduced in 2000 and then substituted by the PCV13 that immunizes against the 13 prevalent serotypes, covering 80–90% of all Streptococcus pneumoniae subtypes.
Vaccines for Tetanus and Diphtheria are toxoid and derive from inactivation with formaldehyde and purification of anatoxins from Clostridium tetani and Corynebacterium diptheria respectively. They are usually administered in combination with pertussis antigens, in a vaccination form (Diph–Te–Per) widely utilized around the word. In a different formulation, the two inactivated toxins are used in combination with Poliomyelites (REVAXIS).
Vaccines for Hepatitis B are produced starting from recombinant proteins. The mono-antigenic yeast-derived alum-adjuvanted hepatitis B vaccines (MAVs), containing a small HBsAg fragment, date back more than 35 years [7,8,9]. New tri-antigenic hepatitis B vaccines (TAV) containing HBV surface antigens resembling the HBV envelope are now in phase 3 clinical studies in neonates and children [10].
Vaccines for Neisseria meningitides Group C and B and for papilloma virus (HPV) are produced utilizing purified proteins. The former is of particular importance being responsible for cases of meningitides with poor clinical outcome [11]. The sero-group C meningitides vaccine conjugate (MCC) was first introduced in Europe in 1999 and offered to the whole pediatric population. Starting from 2014, the new 4CMenB vaccine was developed and introduced in many countries, soon covering more than 85% of the population of children under 12 months of age. A significant protection against the infection was soon reported [12]. Vaccines for HPV are multivalent and assemble capside proteins purified from several recombinant HPV types, including the most frequent virus variants implicated in pathologies of the genital apparatus (from warts to cervical dysplasia and cancer) and oro-pharyngeal cancer [13].
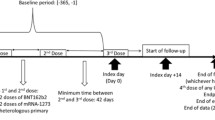
Finally, new anti-Sars-CoV-2 vaccines use different technologies: the EMA approved four vaccines, two composed of non-replicating mRNA (Pfizer-BioNTech BNT162b2 and Moderna mRNA1273) [14,15,16,17,18] and two others based on recombinant adenovirus vectors (Astrazenica ChAdOx1 and Jansen Ad26.COV2.S) [19, 20]. The former vaccines deliver nanoparticles of encapsulated single-strand non-replicating mRNA encoding for the spike antigen of the virus, the other two utilize adenovirus vectors, modified to express the SARS-CoV-2 spike protein on the cell surface. In Europe, only mRNA vaccines have been authorized for pediatric use so far.
Methods of research
Papers published up to July 2022 were selected utilizing the MEDLINE (via PubMed) database. We searched articles about vaccinations of any kind in patients with NS without limits of age. We crossed titles and key words through the MesH motor “Nephrotic Syndrome” OR “Idiopathic Nephrotic Syndrome” AND “vaccin*” (that includes vaccine/s and vaccination/s) or “COVID-19 vaccine” or “SARS-CoV-2 vaccine”. We excluded animal experiments and articles not available in English or that did not provide quantitative data. Case reports were included. Two independent researchers read papers and selected those considered of interest. The list was then merged and discussed.
Results
A total of 377 articles were obtained using the search criteria: 166 duplicates and 71 non full text, animal studies or not English languages were removed (see the PRISMA PICO diagram in Fig. 1). We removed another 50 articles not containing relevant data on generic side effects nor on relapses or new onset NS. The final result was a list of 90 records (14 for live attenuated, 26 for inactivated, 17 for recombinant, 3 for toxoid and 30 for SARS-CoV-2) overall reporting the effect of vaccines in 1015 patients, plus 5 nationwide epidemiologic investigations. The absence of any reported side effects following vaccinations was considered a surrogate for no relapse or “de novo” events in the included study. When possible, the incidence rate of relapse (Inc.) in any specific cohort of patients was calculated (Fig. 2).
Live attenuated virus
With the exception of Varicella-zoster, safety and recurrence of NS following live attenuated vaccines has been investigated in only a few recent studies, which utilized vaccination for single Mumps/Measles or for multiple strains, i.e., MR and MMR. In the year following vaccinations, authors reported seroconversion and adverse events for each vaccine type, including vaccine-associated infection and recurrence of NS. The results are reported separately in the sections below (Table 1).
Mumps
Kamei et al. [21] vaccinated 24 children with NS utilizing two vaccines prepared with different mumps strains (Torii and Hoshino): they reported seroconversion in the 50 and 42% of patients respectively, which decreased to 20% after 1 year (Table 1). No side effects were observed.
Measles alone/Measles–Rubella
Two children presenting an association of measles vaccine and NS were described in 1972: the first was a 21-month-old girl who developed “de novo” NS 9 days after vaccination, the second was a 4-year-old boy affected by NS who developed recurrence of the disease 4 days after measles vaccination [22]. In the Kamei study [21], 2 patients were vaccinated for measles alone and 31 received measles–rubella (MR). Seroconversion after MR was high for either measles (95%) and rubella (100%) and was maintained after 1 year. No side effects were observed. A good seroconversion following measles single vaccination has been confirmed in a recent report by Ayaj et al. [23], who vaccinated 76 children with NS (40 were steroid sensitive NS (SSNS), 36 had focal segmental glomerulosclerosis (FSGS)) and were in active treatment with steroids (SSNS) or with ciclosporin/tacrolimus (FSGS). The study did not furnish any details on either the time of the follow up or the occurrence of side effects, including recurrence of NS.
Measles–Mumps–Rubella
The unique case of NS following measles–mumps–rubella (MMR) has been reported in the literature in 1989. A 13-month-old girl developed “de novo” NS 6 days after vaccination and rapidly responded to steroids [24] (Table 1).
Varicella-zoster
Effectiveness and safety of varicella vaccines in NS have been more widely investigated than other live attenuated vaccines (Table 1). Data published in 1997 in a small group of 7 children with NS, demonstrated that a two-phase vaccination program is required in the majority of NS patients to obtain a satisfactory protection, and that the vaccine was safe [25]. Alpay et al. [26] compared 20 NS children vaccinated with the attenuated Varicella-zoster virus (VZV) vaccine (Varilrix, SmithKline Beecham) and 20 healthy, age-matched controls. Seroconversion was obtained after 8 weeks in 85% and 86% of NS and controls respectively, most of whom had positive antibody titers at 2 years of follow up. Recurrence of NS was observed in one child 20 days after vaccination (Inc. 5%). In 2003, the Southwest Pediatric Nephrology Study Group published the results of an open-label, multicenter clinical trial in 29 children who received 2 doses of VZV attenuated vaccine (Varilrix, Merck) and were followed for 2 years [27]. The study included patients on chronic steroid therapy and excluded other immunosuppressive regimens. All patients and controls demonstrated immunity after the first dose of vaccine and 91% maintained antibodies at 2 years of follow up. Seventeen children with NS relapsed during the 2 years of follow up and 6 within 2 weeks after vaccination (overall Inc. 62%). The study did not provide data on pre-vaccine relapse except for the early relapsers, all of whom had already relapsed in the 2–10 months (mean 3) before vaccination. The study by Kamei et al. [21] reported data on VZV in 42 children with NS: only 61.9% seroconverted after 1 vaccination and 76% after 2–3; NS recurred in 2 patients after 16 and 22 days from vaccination (Inc. 4.8%).
Conclusions
Single mumps and composite vaccinations for measles of NS patients seem safe but only a few reports are available in both cases. Considering the risk of infectious diseases induced by the vaccine itself, live attenuated should generally be avoided, at least in immunocompromised children and in those receiving immunosuppressive drugs. Their use in SSNS could be evaluated considering the context.
Regarding VZV vaccination in children with NS, we can conclude that this is a safe practice and produces sufficient seroconversion to guarantee protection over years. While a few cases of NS relapses following VZV vaccination have been reported, the pre/post vaccination incidence seems similar, not supporting a clear link between the two phenomena.
Inactivated bacteria/virus
Pneumococcal
Several studies have addressed either efficacy and side effects of PPV [28,29,30,31,32,33,34,35,36,37] and, more recently, of PCV in subjects affected by NS treated with both one dose [38, 39] and booster [40]. In the former case (PPV), vaccination was performed in 302 patients with SSNS and 13 with SRNS without side effects or recurrence of NS (reviewed by Goonewardene et al. [41]). PCV vaccines were found to be safe in 62 children with NS who received the first dose and booster [38, 40]; PCV13 [39] was given to 42 patients with NS without side effects (see Table 2).
In conclusion, PCV vaccines are safe and can be utilized in patients with NS.
Influenza
Annual influenza outbreaks significantly impact the clinical outcome of children with all types of NS, who are at high risk of severe infections and of possible relapses of NS secondary to the infection. Vaccines for influenza have also been associated with both relapse [42] and “de novo” NS [43, 44]; one case of “de novo” NS was characterized as membranous nephropathy [45]. Based on the H1N1 experience, many physicians indicate prophylaxis in children and their caregivers prior to the start of the influenza season, with vaccines that are timely produced each year after isolating virus strains [46, 47]. Studies have reported an adequate immunologic response to vaccines for influenza in children with NS [47], which was associated with reduced complications and relapses [48,49,50,51]. Angeletti et al. [52] followed for 24 months 9 children/young patients with NS who had received purified influenza vaccines and found an incidence of recurrence not different from the control group of NS not receiving influenza vaccines. A large study published in 2021 [51] recruited 306 children with NS: 102 were vaccinated, 204 were the control group who did not receive the vaccine. Recurrence of NS was much higher in the latter group compared to vaccinated children (Inc. 0.74% vs. 0.25%). As expected, vaccinated children presented fewer flu episodes compared to non-vaccinated (Inc. 12.7% vs. 25.4%), which corresponded to a markedly reduced risk of getting the disease. In parallel, vaccinated children also had a reduced risk of NS relapse (Inc. 0.22%), indirectly confirming that flu infection may be correlated with NS relapse. Consistently, during the year following the vaccination the 102 children vaccinated for influenza had fewer episodes of NS relapse compared to the year before vaccination, with a reduced risk of recurrence of NS in the post-vaccine versus the pre-vaccine period (Inc. 0.31%).
In conclusion, observational studies demonstrate that influenza vaccines are safe and reduce the risk of infections during the seasonal pandemic. Moreover, vaccines for influenza are also associated with a reduced risk of relapse of NS due to fewer influenza episodes typically related to NS relapse, without any additive risk linked to the vaccine itself.
Poliomyelites
See section on Diphteria–Tetanus (REVAXIS).
Vaccines containing recombinant and purified antigens
HBV
The interest in MAVs vaccines in NS, and more generally in glomerulonephritis, is related with the known association of HBV infection with membranous glomerulopathy, an autoimmune condition causing NS where HBV is deposited along the basal glomerular membrane and functions as an antigen. The development of MAVs and its use in clinical practice has produced a drastic decrease of HBV determined membranous glomerulopathy [53].
Studies in other forms of NS are scanty and, despite the wide utilization of MAVs in the whole population, reports on their association with idiopathic NS in children are limited to case reports describing “de novo” NS in three healthy children and a case of proteinuria recurrence in a patient with MCD [54,55,56,57] (Table 3). The unique observational study reported in the literature was performed in 41 children (age 1–10 years) with SSNS, some of whom (24/41) were on steroid therapy [58]. Seroconversion was higher in those patients not on therapy (76.5% vs. 37.5%). Early recurrence of NS (within 1 month after vaccination) was observed in 14 patients (5 on steroids and 9 not on any treatment, for an overall Inc. 34).
In conclusion, data on a potential association between HBV vaccines and NS are limited and refer to vaccines that are not currently administered as a first option. Data on recurrence or on new episodes of NS following TAV are not available yet, but considering the high number of children treated with this new vaccine there is a real possibility that this association does not exist.
Meningocuccus classes B–C
After the introduction of MCC in clinical practice in 1999, concerns emerged about the possibility that they could be associated with recurrence of NS (Table 3). In 2003, Abeyagunawardena et al. [59] reported an increased incidence of NS relapse in a cohort of 106 NS children during 12 months after vaccination compared to the pre-vaccination phase (Inc. 90% vs. 59%). Taylor et al. [60] followed 53 children with NS for 12 months after MCC vaccination and did not confirm the previous report (post vs. pre vaccine relapse Inc. 0.95 vs. 1.05) (Table 3). The successive development of the new multi-component meningococcal group B vaccine (4CMenB) has reduced the clinical use of MCC to areas where Neisseria meningitides Group C is endemic, limiting the interest on NS recurrence following this vaccine.
Also in the case of 4CMenB, there was variability of results concerning recurrence of NS (Table 3). De Serres et al. [61] compared the incidence of first hospitalization for NS in the province of Quebec and focused, in particular, on the region of Saguenay-Lac-Saint-Jean (SLSJ), an endemic area for group B meningitis, where vaccination with 4CMenB started earlier than in other regions of Canada. They found a sharp increase in the hospitalization for NS of children during the year following vaccination (13.3/100,000 inhabitants vs. 1.6/100,000 of the preceding 10 years), corresponding to 3.6 times higher rate of hospitalization for NS compared to the rest of the Quebec province and 8 times greater than during the eight years preceding the immunization campaign. Andrews et al. [62] evaluated the English hospital admissions for NS from 2005 to 2019, in a population of 2–23-month-old children stratified for age. They considered huge cohorts of children who received a first dose (2.35 million), a second dose (2.25 million) and a booster dose (1.78 million) and compared pre and post 4CMenB vaccine phases. No evidence of increased NS episodes was observed. Finally, NS was not reported to be a side effect of 4CMenB in large populations of children receiving the vaccine in the UK [63] and in Germany [64].
In conclusion, large epidemiologic studies have not confirmed the first Canadian report that was limited to a portion of Quebec.
Human papilloma virus
Vaccination for papilloma is indicated in females before the start of sexual activity around 12 years. No association of human papilloma virus (HPV) vaccines (of any kind) and NS is reported in the literature.
Pertussis
See section of Diphteria–Tetanus (Diph–Te–Per) below.
Toxoid or anatoxin
Diphtheria–tetanus–pertussis
The recent study by Ajay et al. [23] indicated sufficient seroprotection after three Diph–Te–Per doses given to 40 children with SSNS and 36 with FSGS. The comparative antibody titers were higher in SSNS than in FSGS. Incidence of recurrent episodes of NS was not reported.
Single reports of “de novo” NS have been described in association with mixture of diphtheria and tetanus vaccines (Table 3) in two adults: a man vaccinated with a mixture of diphtheria, tetanus, Haemophilus influenzae type B, and Pneumovax vaccines, 1 year after hematopoietic stem cell transplantation for acute myelogenous leukemia [65] and a second case of a 82-year-old female who developed NS (Minimal Changes was the histological diagnosis) 6 weeks after a booster dose of REVAXIS [66]. Angeletti et al. [52] prospectively followed for 24 months 9 children/young patients with NS who had received the diphtheria, tetanus, acellular pertussis vaccine combined with the inactivated poliovirus and found an incidence of recurrence not different from the control group of NS not receiving influenza vaccines.
Anti SARS-CoV-2mRNA and adenovirus vaccines
The SARS-CoV-2 pandemic has represented an extremely serious risk for public health during 2020–2021 and still has a relevant impact, in terms of the incidence of the new Omicron variants. The kidney has been one of the major targets of SARS-CoV-2, causing either “de novo” or relapses of inflammatory and autoimmune glomerulonephritis [67, 68]. Children with NS seemed protected from the first variant [69], whereas they are now more prone to be affected by Omicron even with a limited clinical impact [70]. We cannot exclude that immunosuppressed children with NS become persistent SARS-CoV-2 carriers, as studies on other conditions requiring prolonged immunomodulatory treatments have suggested [71]. Wide vaccination is a necessary step to limit SARS-CoV-2 dissemination.
New onset or recurrence of several forms of glomerulonephritis and NS in children and adults have been reported after vaccination with both mRNA and adenovirus vaccines re-opening “de facto” the broad and important question on the impact of SARS-CoV-2 vaccine in the renal arena [72, 73]. Generally speaking, it should be noted that the impressive number of vaccines distributed in the short period in the world reduces the numerical impact of side effects (in this case, recurrence of NS) since they represent an infinitesimal portion of vaccinated subjects. Considering the stringent temporal association between vaccination and NS in a few cases, we should, however, consider and discuss this possibility (Table 5).
SARS-CoV-2 mRNA
To date (July 2022), there are in the literature 66 cases of NS “de novo” or relapses that occurred in concomitance, or near to, the administration of a mRNA vaccine, where concomitance is defined as NS occurring within 1 month after vaccination [74,75,76,77,78,79,80,81,82,83,84,85,86,87,88,89]. The numerically most significant study (27 cases) was undertaken in Japan as part of a web-based survey within council members of the Japanese Society of Nephrology [89]. This study included children and adults with relapse and de novo NS with variable pathologic characteristics (12 MCD, 4 membranous nephropathy, 2 FSGS, 2 IgA nephropathy and various other cases). Of the 66 cases with de novo/relapse NS of the literature, 60 (Table 4) occurred after the Pfizer-BioNTech BNT162b2 vaccine with a numerical difference that probably reflects the larger use of this vaccine. Relapses of NS were more frequent than “de novo” episodes (41 vs. 19) and the age varied from 14 to 80 years with a median of 43 years (in the Pfizer-BioNTech BNT162b2). Lack of post-vaccine NS in children under 14 years reflects the only recent extension of vaccination under this age. Pathology pictures were available in at least 50% of cases: MCD and FSGS represented the prevalent findings but there were a few cases with membranous nephropathy, IgA and C3 glomerulonephritis. The outcome was good in the majority of cases after steroids associated with mycophenolate mofetil (MMF) (i.e., 28 had complete and 6 partial remission) or calcineurin inhibitors (CNI) in 4 patients; the chimeric anti-CD20 antibody rituximab was administered in 3 cases and the humanized anti-CD20 antibody obinutuzumab in 1 (Table 4). The outcome was not clearly reported in a significant number of patients (n = 28).
Among the 6 cases of NS associated with the Moderna mRNA 1273 vaccine, 4 were “de novo” NS and 2 were relapses. Complete remission was obtained with steroids alone (5) or in association with MMF (2) (Table 4) [82,83,84, 89].
SARS-CoV-2 adenovirus
Five relapses and 3 “de novo” NS have been reported in association with the Astrazeneca ChAdOx1 [90,91,92,93]. Patients’ characteristics and clinical details are the same as the patients group above (Table 4).
Conclusions
Vaccines for SARS-CoV-2 (all kinds) offer a concrete and safe approach to reduce the clinical impact of the pandemic in patients with NS. We strongly support their use in children and adults. Very rare episodes of “de novo” NS or recurrence may occur and generally respond to steroids, therefore, do not represent a numerical and clinical problem.
Indications for vaccinations by deputed organisms
Limited specific indications for vaccination in NS have been formulated over time by deputed medical organizations and official organisations of public health. The 2021 KDIGO Guidelines have integrated most of the issues above and recommend vaccination in NS for pneumococcal, annual influenza virus, and, more generally, accepted inactivated vaccines, while vaccines produced with live attenuated virus (measles, mumps, rubella, varicella, rotavirus) are not indicated, especially in patients receiving chronic immunosuppressive or cytotoxic agents [94]. The American Academy of Pediatrics (AAP) recommended immunizing NS children with pneumococcal PCV13 followed by PPSV23 vaccines after 8 weeks and 5 years from the time of the first dose [95]. The AAP also indicated to defer live attenuated vaccines in case of high steroids and immunosuppressor administration [95]. The Advisory Committee on Immunization Practices (ACIP) confirmed seasonal anti-flu yearly, while it was more restrictive about measles, mumps, rubella, varicella and rotavirus vaccines [96]. In almost all countries (with the limitation above reported by the AAP [95] and the UK Department of Health [97]), vaccinations of NS patients with live attenuated vaccines are not indicated. Moreover, the International Pediatric Nephrology Association [98] recently recommended to complete all vaccinations without delay in NS, including pneumococcal, meningococcal, Haemophilus influenzae, and VZV. Inactivated influenza vaccine was recommended annually. For immunocompromised patients, national vaccination guidelines were recommended for inactive and live attenuated vaccines. On the other hand, national vaccination programs were discouraged in subjects with steroid-resistant NS who usually were treated with daily immunosuppressive medication, including CNIs, MMF, and steroids.
Final considerations
We conclude that all types of vaccines (live attenuated, inactivated, vaccines containing recombinant and purified antigens, toxoid and anatoxins, and the recently developed vaccines for SARS-CoV-2) result safe in terms of both recurrence and “de novo” occurrence of NS. Immunization was effective for the majority of vaccine types, including in subjects with chronic immunosuppressive treatments. The following general considerations complete the synthesis on effectiveness: (1) patients who received vaccinations as a part of routine (not in the presence of proteinuria) have higher antibody titers than after the onset of NS; (2) the connection between specific serum immunoglobulin conversion with proteinuria is variable: HBV and varicella vaccines are an example of limited seroconversion during florid proteinuria (60–70%); for other vaccines such as anti-tetanus, diphtheria, pertussis, measles, mumps, rubella, the presence of proteinuria does not influence specific IgG levels; (3) the persistence of adequate antibody titers following different vaccination is also variable and it is strictly “vaccine type” dependent; vaccination with Pneumococcal conjugate, for example, maintains protection for 1 year, for other vaccines protection is maintained for longer periods.
Guidelines support the use of almost all vaccines in patients with NS with the exception of live attenuated especially in patients receiving chronic immunosuppressive treatments. All other vaccines can be utilized also in concomitance with immunosuppressive treatments with steroids, CNI and MMF. In patients with NS treated with monoclonal anti-CD20 antibodies, all types of vaccine should be provided at least 6 months after last infusion; during the pandemic, vaccines for SARS-CoV-2 should be provided, if possible, 3 months before the infusion of monoclonal anti-CD20 antibodies.
However, in the real-world practice, facts are distant from theory. Only a minority of parents accept to vaccinate their children affected by NS with vaccines that are permitted by guidelines and even doubt vaccinations (such as for influenza) that we know protect from complications of the pandemic and also from relapses of NS. Popular credence supported these concerns for years and we hope that evidence will change current distorted practice.
Based on the above presented data, we may conclude that (1) all types of vaccinations are safe in subjects with NS also in those patients receiving steroids, CNIs and MMF; (2) vaccinations (all kinds) are recommended by guidelines in NS, with the exception of vaccines produced with live attenuated virus (measles, mumps, rubella, varicella, rotavirus) in patients receiving chronic immunosuppressive or cytotoxic agents; (3) vaccinations for annual influenza virus reduce the number of recurrences in patients with NS; and (4) vaccines for SARS-CoV-2 (all kinds) offer a concrete and safe approach to reduce the clinical impact of the pandemic in patients with NS without any risk of recurrence of the disease.
Data availability
Not applicable.
Code availability
Not applicable.
References
McIntyre P, Craig JC (1998) Prevention of serious bacterial infection in children with nephrotic syndrome. J Paediatr Child Health 34:314–317
Kemper MJ, Altrogge H, Ganschow R, Müller-Wiefel DE (2002) Serum levels of immunoglobulins and IgG subclasses in steroid sensitive nephrotic syndrome. Pediatr Nephrol 17:413–417
Banerjee S, Dissanayake PV, Abeyagunawardena AS (2016) Vaccinations in children on immunosuppressive medications for renal disease. Pediatr Nephrol 31:1437–1448
Broyer M, Tete MJ, Guest G, Gagnadoux MF, Rouzioux C (1997) Varicella and zoster in children after kidney transplantation: long-term results of vaccination. Pediatrics 99:35–39
Meadow SR, Weller RO, Archibald RW (1969) Fatal systemic measles in a child receiving cyclophosphamide for nephrotic syndrome. Lancet 2:876–878
Thadchanamoorthy V, Dayasiri K (2021) Review on pneumococcal infection in children. Cureus 13:e14913
Mantan M, Pandharikar N, Yadav S, Chakravarti A, Sethi GR (2013) Seroprotection for hepatitis B in children with nephrotic syndrome. Pediatr Nephrol 28:2125–2130
La Manna A, Polito C, Foglia AC, Di Toro A, Cafaro MR, Del Gado R (1992) Reduced response to hepatitis B virus vaccination in boys with steroid-sensitive nephrotic syndrome. Pediatr Nephrol 6:251–253
Neupane N, Krishnamurthy S, Jagadisan B, Dhodapkar R (2019) Hepatitis B seroprotection in pediatric nephrotic syndrome. Indian Pediatr 56:659–662
Vesikari T, Langley JM, Segall N, Ward BJ, Cooper C, Poliquin G, Smith B, Gantt S, McElhaney JE, Dionne M, van Damme P, Leroux-Roels I, Leroux-Roels G, Machluf N, Spaans JN, Yassin-Rajkumar B, Anderson DE, Popovic V, Diaz-Mitoma F, PROTECT Study Group (2021) Immunogenicity and safety of a tri-antigenic versus a mono-antigenic hepatitis B vaccine in adults (PROTECT): a randomised, double-blind, phase 3 trial. Lancet Infect Dis 21:1271–1281
Miller E, Salisbury D, Ramsay M (2001) Planning, registration, and implementation of an immunisation campaign against meningococcal serogroup C disease in the UK: a success story. Vaccine 20(Suppl 1):S58-67
Ladhani SN, Andrews N, Parikh SR, Campbell H, White J, Edelstein M, Bai X, Lucidarme J, Borrow R, Ramsay ME (2020) Vaccination of infants with meningococcal group B vaccine (4CMenB) in England. N Engl J Med 382:309–317
Tsang SH, Sampson JN, Schussler J, Porras C, Wagner S, Boland J, Cortes B, Lowy DR, Schiller JT, Schiffman M, Kemp TJ, Rodriguez AC, Quint W, Gail MH, Pinto LA, Gonzalez P, Hildesheim A, Kreimer AR, Herrero R, Costa Rica HPV Vaccine Trial (CVT) Group (2020) Durability of cross-protection by different schedules of the bivalent HPV vaccine: the CVT Trial. J Natl Cancer Inst 112:1030–1037
Polack FP, Thomas SJ, Kitchin N, Absalon J, Gurtman A, Lockhart S, Perez JL, Pérez Marc G, Moreira ED, Zerbini C, Bailey R, Swanson KA, Roychoudhury S, Koury K, Li P, Kalina WV, Cooper D, Frenck RW Jr, Hammitt LL, Türeci Ö, Nell H, Schaefer A, Ünal S, Tresnan DB, Mather S, Dormitzer PR, Şahin U, Jansen KU, Gruber WC, C4591001 Clinical Trial Group (2020) Safety and efficacy of the BNT162b2 mRNA Covid-19 vaccine. N Engl J Med 383:2603–2615
Baden LR, El Sahly HM, Essink B, Kotloff K, Frey S, Novak R, Diemert D, Spector SA, Rouphael N, Creech CB, McGettigan J, Khetan S, Segall N, Solis J, Brosz A, Fierro C, Schwartz H, Neuzil K, Corey L, Gilbert P, Janes H, Follmann D, Marovich M, Mascola J, Polakowski L, Ledgerwood J, Graham BS, Bennett H, Pajon R, Knightly C, Leav B, Deng W, Zhou H, Han S, Ivarsson M, Miller J, Zaks T, COVE Study Group (2021) Efficacy and safety of the mRNA-1273 SARS-CoV-2 vaccine. N Engl J Med 384:403–416
Voysey M, Clemens SAC, Madhi SA, Weckx LY et al (2021) Safety and efficacy of the ChAdOx1 nCoV-19 vaccine (AZD1222) against SARS-CoV-2: an interim analysis of four randomised controlled trials in Brazil, South Africa, and the UK. Lancet 397:99–111
Frenck RW Jr, Klein NP, Kitchin N, Gurtman A, Absalon J, Lockhart S, Perez JL, Walter EB, Senders S, Bailey R, Swanson KA, Ma H, Xu X, Koury K, Kalina WV, Cooper D, Jennings T, Brandon DM, Thomas SJ, Türeci Ö, Tresnan DB, Mather S, Dormitzer PR, Şahin U, Jansen KU, Gruber WC, C4591001 Clinical Trial Group (2021) Safety, immunogenicity, and efficacy of the BNT162b2 Covid-19 vaccine in adolescents. N Engl J Med 385:239–250
Ali K, Berman G, Zhou H, Deng W, Faughnan V, Coronado-Voges M, Ding B, Dooley J, Girard B, Hillebrand W, Pajon R, Miller JM, Leav B, McPhee R (2021) Evaluation of mRNA-1273 SARS-CoV-2 vaccine in adolescents. N Engl J Med 385:2241–2251
Ramasamy MN, Minassian AM, Ewer KJ, Flaxman AL et al (2021) Safety and immunogenicity of ChAdOx1 nCoV-19 vaccine administered in a prime-boost regimen in young and old adults (COV002): a single-blind, randomised, controlled, phase 2/3 trial. Lancet 396:1979–1993
Sadoff J, Gray G, Vandebosch A, Cárdenas V, Shukarev G, Grinsztejn B, Goepfert PA, Truyers C, Fennema H, Spiessens B, Offergeld K, Scheper G, Taylor KL, Robb ML, Treanor J, Barouch DH, Stoddard J, Ryser MF, Marovich MA, Neuzil KM, Corey L, Cauwenberghs N, Tanner T, Hardt K, Ruiz-Guiñazú J, Le Gars M, Schuitemaker H, Van Hoof J, Struyf F, Douoguih M, ENSEMBLE Study Group (2021) Safety and efficacy of single-dose Ad26.COV2.S vaccine against Covid-19. N Engl J Med 384:2187–2201
Kamei K, Miyairi I, Ishikura K, Ogura M, Shoji K, Funaki T, Ito R, Arai K, Abe J, Kawai T, Onodera M, Ito S (2018) Prospective study of live attenuated vaccines for patients with nephrotic syndrome receiving immunosuppressive agents. J Pediatr 196(217–222):e1
Kuzemko JA (1972) Measles vaccination and the nephrotic syndrome. Br Med J 4:665–666
Ajay M, Mantan M, Dabas A, Asraf A, Yadav S, Chakravarti A (2021) Seroprotection for Diphtheria, Pertussis, Tetanus and Measles in children with nephrotic syndrome. Indian Pediatr 58:233–236
Ahuja AS, Wright M (1989) MMR and the nephrotic syndrome. BMJ 299:796
Quien RM, Kaiser BA, Deforest A, Polinsky MS, Fisher M, Baluarte HJ (1997) Response to the varicella vaccine in children with nephrotic syndrome. J Pediatr 131:688–690
Alpay H, Yildiz N, Onar A, Temizer H, Ozçay S (2002) Varicella vaccination in children with steroid-sensitive nephrotic syndrome. Pediatr Nephrol 17:181–183
Furth SL, Arbus GS, Hogg R, Tarver J, Chan C, Fivush BA, Southwest Pediatric Nephrology Study Group (2003) Varicella vaccination in children with nephrotic syndrome: a report of the Southwest Pediatric Nephrology Study Group. J Pediatr 142:145–148
Spika JS, Halsey NA, Fish AJ, Lum GM, Lauer BA, Schiffman G, Giebink GS (1982) Serum antibody response to pneumococcal vaccine in children with nephrotic syndrome. Pediatrics 69:219–223
Garin EH, Barrett DJ (1988) Pneumococcal polysaccharide immunization in patients with active nephrotic syndrome. Nephron 50:383–388
Fikrig SM, Schiffman G, Phillipp JC, Moel DI (1978) Antibody response to capsular polysaccharide vaccine of Streptococcus pneumoniae in patients with nephrotic syndrome. J Infect Dis 137:818–821
Wilkes JC, Nelson JD, Worthen HG, Morris M, Hogg RJ (1982) Response to pneumococcal vaccination in children with nephrotic syndrome. Am J Kidney Dis 2:43–46
Tejani A, Fikrig S, Schiffman G, Gurumurthy K (1984) Persistence of protective pneumococcal antibody following vaccination in patients with the nephrotic syndrome. Am J Nephrol 4:32–37
Spika JS, Halsey NA, Le CT, Fish AJ, Lum GM, Lauer BA, Schiffman G, Giebink GS (1986) Decline of vaccine-induced antipneumococcal antibody in children with nephrotic syndrome. Am J Kidney Dis 7:466–470
Lee HJ, Kang JH, Henrichsen J, Konradsen HB, Jang SH, Shin HY, Ahn HS, Choi Y, Hessel L, Nam SW (1995) Immunogenicity and safety of a 23-valent pneumococcal polysaccharide vaccine in healthy children and in children at increased risk of pneumococcal infection. Vaccine 13:1533–1538
Güven AG, Akman S, Bahat E, Senyurt M, Yüzbey S, Uguz A, Yegin O (2004) Rapid decline of anti-pneumococcal antibody levels in nephrotic children. Pediatr Nephrol 19:61–65
Ulinski T, Leroy S, Dubrel M, Danon S, Bensman A (2008) High serological response to pneumococcal vaccine in nephrotic children at disease onset on high-dose prednisone. Pediatr Nephrol 23:1107–1113
Aoun B, Wannous H, Azéma C, Ulinski T (2010) Polysaccharide pneumococcal vaccination of nephrotic children at disease onset-long-term data. Pediatr Nephrol 25:1773–1774
Liakou CD, Askiti V, Mitsioni A, Stefanidis CJ, Theodoridou MC, Spoulou VI (2011) Safety, immunogenicity and kinetics of immune response to 7-valent pneumococcal conjugate vaccine in children with idiopathic nephrotic syndrome. Vaccine 29:6834–6837
Pittet LF, Posfay-Barbe KM, Chehade H, Rudin C, Wilhelm-Bals A, Rodriguez M, Siegrist CA, Parvex P (2016) Optimizing seroprotection against pneumococcus in children with nephrotic syndrome using the 13-valent pneumococcal conjugate vaccine. Vaccine 34:4948–4954
Liakou CD, Askiti V, Mitsioni A, Stefanidis CJ, Theodoridou MC, Spoulou VI (2014) Safety and immunogenicity of booster immunization with 7-valent pneumococcal conjugate vaccine in children with idiopathic nephrotic syndrome. Vaccine 32:1394–1397
Goonewardene ST, Tang C, Tan LT, Chan KG, Lingham P, Lee LH, Goh BH, Pusparajah P (2019) Safety and efficacy of pneumococcal vaccination in pediatric nephrotic syndrome. Front Pediatr 7:339
Fernandes P, Jorge S, Lopes JA (2010) Relapse of nephrotic syndrome following the use of 2009 pandemic influenza A (H1N1) vaccine. Am J Kidney Dis 56:185–186
Kielstein JT, Termühlen L, Sohn J, Kliem v, (2000) Minimal change nephrotic syndrome in a 65-year-old patient following influenza vaccination. Clin Nephrol 54:246–248
Gutiérrez S, Dotto B, Petiti JP, De Paul AL, Dionisio de Cabalier ME, Torres AI, Mukdsi JH (2012) Minimal change disease following influenza vaccination and acute renal failure: just a coincidence? Nefrologia 32:414–415
Kutlucan A, Gonen I, Yildizhan E, Aydin Y, Sav T, Yildirim U (2012) Can influenza H1N1 vaccination lead to the membranous glomerulonephritis? Indian J Pathol Microbiol 55:239–241
Kim CO, Nam CM, Lee DC, Han SH, Lee JW (2010) Clinical predictors of novel influenza A (H1N1)infection in Korea. Yonsei Med J 51:895–900
Brydak LB, Machala M (2000) Humoral immune response to influenza vaccination in patients from high risk groups. Drugs 60:35–53
Poyrazoğlu HM, Düşünsel R, Gündüz Z, Patiroğlu T, Köklü S (2004) Antibody response to influenza A vaccination in children with nephrotic syndrome. Pediatr Nephrol 19:57–60
Tanaka S, Saikusa T, Katafuchi Y, Ushijima K, Ohtsu Y, Tsumura N, Ito Y (2015) Serologic response after vaccination against influenza (A/H1N1)pdm09 in children with renal disease receiving oral immunosuppressive drugs. Vaccine 33:5000–5004
Klifa R, Toubiana J, Michel A, Biebuyck N, Charbit M, Heidet L, Krid S, Krug P, Salomon R, Boyer O (2019) Influenza vaccination among children with idiopathic nephrotic syndrome: an investigation of practices. BMC Nephrol 20:65
Ishimori S, Ando T, Kikunaga K, Terano C, Sato M, Komaki F, Hamada R, Hamasaki Y, Araki Y, Gotoh Y, Nakanishi K, Nakazato H, Matsuyama T, Iijima K, Yoshikawa N, Ito S, Honda M, Ishikura K (2021) Influenza virus vaccination in pediatric nephrotic syndrome significantly reduces rate of relapse and influenza virus infection as assessed in a nationwide survey. Sci Rep 11:23305
Angeletti A, Bruschi M, Bianchin S, Bonato I, Montobbio C, Verrina E, Lugani F, Cravedi P, Ghiggeri GM (2021) Vaccines and disease relapses in children with nephrotic syndrome. Clin J Am Soc Nephrol 16:937–938
Liao MT, Chang MH, Lin FG, Tsai IJ, Chang YW, Tsau YK (2011) Universal hepatitis B vaccination reduces childhood hepatitis B virus-associated membranous nephropathy. Pediatrics 128:e600-604
Macário F, Freitas L, Correia J, Campos M, Marques A (1995) Nephrotic syndrome after recombinant hepatitis B vaccine. Clin Nephrol 43:349
Işlek I, Cengiz K, Cakir M, Küçüködük S (2000) Nephrotic syndrome following hepatitis B vaccination. Pediatr Nephrol 14:89–90
Ozdemir S, Bakkaloglu A, Oran O (1998) Nephrotic syndrome associated with recombinant hepatitis B vaccination: a causal relationship or just a mere association? Nephrol Dial Transplant 13:1888–1889
Pennesi M, Torre G, Del Santo M, Sonzogni A (2002) Glomerulonephritis after recombinant hepatitis B vaccine. Pediatr Infect Dis J 21:172–173
Yıldız N, Sever L, Kasapçopur Ö, Çullu F, Arısoy N, Çalışkan S (2013) Hepatitis B virus vaccination in children with steroid sensitive nephrotic syndrome: immunogenicity and safety? Vaccine 31:3309–3312
Abeyagunawardena AS, Goldblatt D, Andrews N, Trompeter RS (2003) Risk of relapse after meningococcal C conjugate vaccine in nephrotic syndrome. Lancet 362:449–450
Taylor B, Andrews N, Stowe J, Hamidi-Manesh L, Miller E (2007) No increased risk of relapse after meningococcal C conjugate vaccine in nephrotic syndrome. Arch Dis Child 92:887–889
De Serres G, Billard MN, Gariépy MC, Roy MC, Boucher FD, Gagné H, Belley S, Toth E, Landry M, Skowronski DM (2019) Nephrotic syndrome following four-component meningococcal B vaccination: epidemiologic investigation of a surveillance signal. Vaccine 37:4996–5002
Andrews N, Stowe J, Miller E (2020) Nephrotic syndrome in infants and toddlers before and after introduction of the meningococcal B vaccine programme in England: An ecological study. Vaccine 38:4816–4819
Bryan P, Seabroke S, Wong J, Donegan K, Webb E, Goldsmith C, Vipond C, Feavers I (2018) Safety of multicomponent meningococcal group B vaccine (4CMenB) in routine infant immunisation in the UK: a prospective surveillance study. Lancet Child Adolesc Health 2:395–403
Mentzer D, Oberle D, Keller-Stanislawski B (2018) Adverse events following immunisation with a meningococcal serogroup B vaccine: report from post-marketing surveillance, Germany, 2013 to 2016. Euro Surveill 23:17–00468
Humphreys BD, Vanguri VK, Henderson J, Antin JH (2006) Minimal-change nephrotic syndrome in a hematopoietic stem-cell transplant recipient. Nat Clin Pract Nephrol 2:535–539; quiz 540
Clajus C, Spiegel J, Bröcker V, Chatzikyrkou C, Kielstein JT (2009) Minimal change nephrotic syndrome in an 82 year old patient following a tetanus-diphteria-poliomyelitis-vaccination. BMC Nephrol 10:21
Melgosa M, Madrid A, Alvárez O, Lumbreras J, Nieto F, Parada E, Perez-Beltrán V, Spanish Pediatric Nephrology Association (2020) SARS-CoV-2 infection in Spanish children with chronic kidney pathologies. Pediatr Nephrol 35:1521–1524
Morello W, Vianello FA, Proverbio E, Peruzzi L, Pasini A, Montini G (2022) COVID-19 and idiopathic nephrotic syndrome in children: systematic review of the literature and recommendations from a highly affected area. Pediatr Nephrol 37:757–764
Angeletti A, Drovandi S, Sanguineri F, Santaniello M, Ferrando G, Forno R, Cipresso G, Caridi G, Riella LV, Cravedi P, Ghiggeri GM (2020) COVID-19 in children with nephrotic syndrome on anti-CD20 chronic immunosuppression. Clin J Am Soc Nephrol 15:1494–1495
Angeletti A, Bruschi M, Bigatti C, Palmeri S, Lugani F, Verrina E, Ghiggeri GM (2022) An update on COVID-19 in paediatric and young adults with nephrotic syndrome, receiving chronic immunosuppression during the Omicron pandemic. J Nephrol 35:1775–1776
Choi B, Choudhary MC, Regan J, Sparks JA, Padera RF, Qiu X, Solomon IH, Kuo HH, Boucau J, Bowman K, Adhikari UD, Winkler ML, Mueller AA, Hsu TY, Desjardins M, Baden LR, Chan BT, Walker BD, Lichterfeld M, Brigl M, Kwon DS, Kanjilal S, Richardson ET, Jonsson AH, Alter G, Barczak AK, Hanage WP, Yu XG, Gaiha GD, Seaman MS, Cernadas M, Li JZ (2020) Persistence and evolution of SARS-CoV-2 in an immunocompromised host. N Engl J Med 383:2291–2293
Li NL, Coates PT, Rovin BH (2021) COVID-19 vaccination followed by activation of glomerular diseases: does association equal causation? Kidney Int 100:959–965
Bomback AS, Kudose S, D’Agati VD (2021) De novo and relapsing glomerular diseases after COVID-19 vaccination: What Do We Know So Far? Am J Kidney Dis 78:477–480
Schwotzer N, Kissling S, Fakhouri F (2021) Letter regarding “Minimal change disease relapse following SARS-CoV-2 mRNA vaccine.” Kidney Int 100:458–459
D’Agati VD, Kudose S, Bomback AS, Adamidis A, Tartini A (2021) Minimal change disease and acute kidney injury following the Pfizer-BioNTech COVID-19 vaccine. Kidney Int 100:461–463
Dormann H, Knüppel-Ruppert A, Amann K, Erley C (2021) Nephrotic syndrome after vaccination against COVID-19: three new cases from Germany. Dtsch Arztebl Int 118:662–663
Lebedev L, Sapojnikov M, Wechsler A, Varadi-Levi R, Zamir D, Tobar A, Levin-Iaina N, Fytlovich S, Yagil Y (2021) Minimal change disease following the Pfizer-BioNTech COVID-19 vaccine. Am J Kidney Dis 78:142–145
Maas RJ, Gianotten S, van der Meijden WAG (2021) An additional case of minimal change disease following the Pfizer-BioNTech COVID-19 vaccine. Am J Kidney Dis 78:312
Weijers J, Alvarez C, Hermans MMH (2021) Post-vaccinal minimal change disease. Kidney Int 100:459–461
Kervella D, Jacquemont L, Chapelet-Debout A, Deltombe C, Ville S (2021) Minimal change disease relapse following SARS-CoV-2 mRNA vaccine. Kidney Int 100:457–458
Komaba H, Wada T, Fukagawa M (2021) Relapse of minimal change disease following the Pfizer-BioNTech COVID-19 vaccine. Am J Kidney Dis 78:469–470
Salem F, Rein JL, Yu SM, Abramson M, Cravedi P, Chung M (2021) Report of three cases of minimal change disease following the second dose of mRNA SARS-CoV-2 COVID-19 vaccine. Kidney Int Rep 6:2523–2524
Holzworth A, Couchot P, Cruz-Knight W, Brucculeri M (2021) Minimal change disease following the Moderna mRNA-1273 SARS-CoV-2 vaccine. Kidney Int 100:463–464
Thappy S, Thalappil SR, Abbarh S, Al-Mashdali A, Akhtar M, Alkadi MM (2021) Minimal change disease following the Moderna COVID-19 vaccine: first case report. BMC Nephrol 22:376
Kobayashi S, Fugo K, Yamazaki K, Terawaki H (2021) Minimal change disease soon after Pfizer-BioNTech COVID-19 vaccination. Clin Kidney J 14:2606–2607
Mancianti N, Guarnieri A, Tripodi S, Salvo DP, Garosi G (2021) Minimal change disease following vaccination for SARS-CoV-2. J Nephrol 34:1039–1040
Nakazawa E, Uchimura T, Hirai Y, Togashi H, Oyama Y, Inaba A, Shiga K, Ito S (2022) New-onset pediatric nephrotic syndrome following Pfizer-BioNTech SARS-CoV-2 vaccination: a case report and literature review. CEN Case Rep 11:242–246
Hummel A, Oniszczuk J, Kervella D, Charbit M, Guerrot D, Testa A, Philipponnet C, Chauvet C, Guincestre T, Brochard K, Benezech A, Figueres L, Belenfant X, Guarnieri A, Demoulin N, Benetti E, Miglinas M, Dessaix K, Morelle J, Angeletti A, Sellier-Leclerc AL, Ranchin B, Goussard G, Hudier L, Bacchetta J, Servais A, Audard V (2022) Idiopathic nephrotic syndrome relapse following SARS-CoV-2 vaccination: a series of 25 cases. Clin Kidney J 15:1574–1582
Nakagawa N, Maruyama S, Kashihara N, Narita I, Isaka Y (2022) New-onset and relapse of nephrotic syndrome following COVID-19 vaccination: a questionnaire survey in Japan. Clin Exp Nephrol 26:909–916
Leclerc S, Royal V, Lamarche C, Laurin LP (2021) Minimal change disease with severe acute kidney injury following the Oxford-AstraZeneca COVID-19 Vaccine: a case report. Am J Kidney Dis 78:607–610
Morlidge C, El-Kateb S, Jeevaratnam P, Thompson B (2021) Relapse of minimal change disease following the AstraZeneca COVID-19 vaccine. Kidney Int 100:459
Unver S, Haholu A, Yildirim S (2021) Nephrotic syndrome and acute kidney injury following CoronaVac anti-SARS-CoV-2 vaccine. Clin Kidney J 14:2608–2611
Biradar VG, Alqahtani MA, Nagaraj HC, Ahmed EA, Tripathi V, Botto-Tobar M, Atiglah HK (2022) Adult-onset nephrotic syndrome following coronavirus disease vaccination. Clin Kidney J 15:168–170
Radhakrishnan J, Cattran DC (2012) The KDIGO practice guideline on glomerulonephritis: reading between the (guide)lines—application to the individual patient. Kidney Int 82:840–856
Gipson DS, Massengill SF, Yao L, Nagaraj S, Smoyer WE, Mahan JD, Wigfall D, Miles P, Powell L, Lin JJ, Trachtman H, Greenbaum LA (2009) Management of childhood onset nephrotic syndrome. Pediatrics 124:747–757
Nuorti JP, Whitney CG, Centers for Disease Control and Prevention (CDC) (2010) Prevention of pneumococcal disease among infants and children - use of 13-valent pneumococcal conjugate vaccine and 23-valent pneumococcal polysaccharide vaccine - recommendations of the Advisory Committee on Immunization Practices (ACIP). MMWR Recomm Rep 59(11):1–18
McCaffrey J, Lennon R, Webb NJ (2016) The non-immunosuppressive management of childhood nephrotic syndrome. Pediatr Nephrol 31:1383–1402
Trautmann A, Vivarelli M, Samuel S, Gipson D, Sinha A, Schaefer F, Hui NK, Boyer O, Saleem MA, Feltran L, Müller-Deile J, Becker JU, Cano F, Xu H, Lim YN, Smoyer W, Anochie I, Nakanishi K, Hodson E, Haffner D, International Pediatric Nephrology Association (2020) IPNA clinical practice recommendations for the diagnosis and management of children with steroid-resistant nephrotic syndrome. Pediatr Nephrol 35:1529–1561
Acknowledgements
The submission of the present Manuscript was supported by the Italian Ministry of Health—5X1000 anno 2020.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no conflict of interest.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Angeletti, A., Lugani, F., La Porta, E. et al. Vaccines and nephrotic syndrome: efficacy and safety. Pediatr Nephrol 38, 2915–2928 (2023). https://doi.org/10.1007/s00467-022-05835-4
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00467-022-05835-4