Abstract
The purpose of this study is to investigate the diagnostic and prognostic role of cerebrospinal fluid (CSF) biomarkers in the diagnostic work-up of glucose transporter 1 (GLUT1) deficiency. Reported here is a systematic review according to PRISMA guidelines collecting clinical and biochemical data about all published patients who underwent CSF analysis. Clinical phenotypes were compared between groups defined by the levels of CSF glucose (≤ 2.2 mmol/L versus > 2.2 mmol/L), CSF/blood glucose ratio (≤ 0.45 versus > 0.45), and CSF lactate (≤ 1 mmol/L versus > 1 mmol/L). Five hundred sixty-two patients fulfilled the inclusion criteria with a mean age at the diagnosis of 8.6 ± 6.7 years. Patients with CSF glucose ≤ 2.2 mmol/L and CSF/blood glucose ratio ≤ 0.45 presented with an earlier onset of symptoms (16.4 ± 22.0 versus 54.4 ± 45.9 months, p < 0.01; 15.7 ± 23.8 versus 40.9 ± 38.0 months, p < 0.01) and received an earlier molecular genetic confirmation (92.1 ± 72.8 versus 157.1 ± 106.2 months, p < 0.01). CSF glucose ≤ 2.2 mmol/L was consistently associated with response to ketogenic diet (p = 0.018) and antiseizure medications (p = 0.025). CSF/blood glucose ratio ≤ 0.45 was significantly associated with absence seizures (p = 0.048), paroxysmal exercise‐induced dyskinesia (p = 0.046), and intellectual disability (p = 0.016) while CSF lactate > 1 mmol/L was associated with a response to antiseizure medications (p = 0.026) but not to ketogenic diet.
Conclusions:This systematic review supported the diagnostic usefulness of lumbar puncture for the early identification of patients with GLUT1 deficiency responsive to treatments especially if they present with co-occurring epilepsy, movement, and neurodevelopmental disorders.
What is Known: |
• Phenotypes of GLUT1 deficiency syndrome range between early epileptic and developmental encephalopathy to paroxysmal movement disorders and developmental impairment |
What is New: |
• CSF blood/glucose ratio may predict better than CSF glucose the diagnosis in children presenting with early onset absences |
• CSF blood/glucose ratio may predict better than CSF glucose the diagnosis in children presenting with paroxysmal exercise induced dyskinesia and intellectual disability. |
• CSF glucose may predict better than CSF blood/glucose and lactate the response to ketogenic diet and antiseizure medications. |
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Glucose transporter 1 (GLUT1) deficiency syndrome is a rare and treatable neurometabolic disorder with a multifaceted phenotypic spectrum ranging between early onset epileptic and developmental encephalopathy, early onset absence or myoclonic-atonic epilepsy, focal epilepsy, episodic choreoathetosis and spasticity, paroxysmal exercise-induced dyskinesia, intermittent ataxia, and various degrees of neurodevelopmental impairment [1, 2]. These presentations are caused by pathogenic variants of solute carrier family 2 member 1 (SLC2A1; OMIM 138140) gene encoding for the most important energy carrier of the brain across the blood-brain barrier (GLUT1) [1].
The early diagnosis of GLUT1 deficiency has remarkable prognostic implications because an effective treatment (e.g., ketogenic diet) may result in a complete resolution of motor symptoms and epileptic seizures [3]. Lumbar puncture has always represented the initial diagnostic step since the first descriptions of GLUT1 deficiency even if the increasing potentials of ultra-fast next-generation sequencing techniques, the recent validation of a less invasive blood test (e.g., METAGLUT1), and the detection of novel candidate cerebrospinal biomarkers (e.g., gluconic + galactonic acid, xylose-α1-3-glucose, and xylose-α1-3-xylose-α1-3-glucose) provided possible alternative diagnostic tools [4, 5].
The precise definition of the diagnostic strength and the prognostic role of each measurable CSF biomarker in the real-world practice still represent an important gap in the literature. This review aimed to evaluate whether CSF glucose, CSF/blood glucose ratio, and CSF lactate may impact the phenoty** process of patients with GLUT1 deficiency and guide therapeutic choices.
Materials and methods
We conducted a systematic review of published pediatric cases with a compatible clinical phenotype and a confirmed molecular genetic diagnosis of GLUT1 deficiency syndrome according to PRISMA guidelines (Fig. 1). A PubMed, Web of Science, and Scopus search was performed using the search terms (GLUT1 OR “glut 1” OR glut-1 OR “glucose transporter type 1”) AND (deficit* OR disorder) and filtered results for the age range 0–18 years and the temporal range January 1991–June 2023. Reference lists of each selected article and systematic reviews on the same focus were reviewed to collect additional papers.
Articles reporting patients without data about CSF analysis or without a molecular genetic diagnosis, articles without data reported on patient-by-patient basis, articles about studies not focusing on human beings, and articles that were not written in English were excluded from the analysis (Fig. 1).
Results were screened by title, abstract, and full text. Duplicates were excluded. Studies reporting overlap** cohorts were identified by comparing relevant features (i.e., number of subjects, time variables, outcomes, institution, and year). The studies with the most extensive reporting were selected for inclusion in our analysis.
Data on demographic features, epilepsy, movement disorders and developmental phenotypes, CSF biochemical markers, molecular genetic data, and neurological outcomes were collected for each of the patients satisfying the inclusion criteria.
Figure 1 summarizes the features of the selected articles. Study selection was performed independently by three authors (ECC, NC, and AB). Supplement 1 includes the complete data collection sheet including the main demographic, clinical, and biochemical data for each one of the published patients. Supplement 2 summarizes the distribution of the associated SLC2A1 gene variants. Supplement 3 illustrates the evaluation of the articles that was realized according to NIH-Quality Assessment Tool (https://www.nhlbi.nih.gov/health-topics/study-quality-assessment-tools). Supplement 4 and 5 report the risk of bias for each one of the selected article according to the RoB 2.0-Robvis tool (https://mcguinlu.shinyapps.io/robvis/). Supplement 6 includes PRISMA checklist.
Clinical data were compared between (1) patients with CSF glucose ≤ 2.2 and patients with CSF glucose > 2.2 mmol/L [2], (2) patients with CSF/blood glucose ratio ≤ 0.45 and patients with CSF/blood glucose ratio > 0.45 [2], and (3) patients with CSF lactate < 1 mmol/L and patients with CSF lactate > 1 mmol/L (Table 1). Cut-off values for CSF glucose and CSF /blood glucose ratio were taken from the literature [2]. Cut-off values of CSF glucose, CSF /blood glucose ratio, and CSF lactate were also calculated through receiver operating characteristic (ROC) curve analysis (sensitivity, specificity, and Youden index) within the cohort of published patients reported here.
Data extraction from all the selected articles was blindly performed by two authors (FM and GR). Controversies about study selection and data extraction were solved after a case-by-case discussion involving all the authors with the supervision of FP as Senior Author.
All statistical analyses were conducted using IBM SPSS Statistics version 25.0 (SPSS Inc., Chicago, IL, USA). Normality was assessed with the Kolmogorov-Smirnov test. Comparisons were performed using Mann–Whitney U test for non-normally distributed data and Fisher’s exact test for categorical variables. A p value < 0.05 represented statistical significance for all tests. Pairwise deletion was applied for each one of the analyzed parameters. Variables with missing data above a certain threshold (e.g., 20%) were scrutinized to decide on their processing.
The review was recorded in PROSPERO (https://www.crd.york.ac.uk/prospero/-CRD42023480301) on 7/11/2023, and the registered protocol was updated on 3/5/2024 to include an extension of the initially planned completion date.
Results
Patient characteristics
The screening of the literature resulted in 136 articles fulfilling all the inclusion criteria (60 case reports, 47 case series, 15 retrospective cohort studies, 9 prospective cohort studies, 4 case-control studies, and 1 survey). The quality of the article according to NIH-Quality Assessment Tool was judged as fair in 78, good in 44, and poor in 17 cases (Suppl. 3). A consistent risk of bias was assessed by RoB 2.0-Robvis tool (https://mcguinlu.shinyapps.io/robvis/) especially for the studies focused on the measurement of outcome.
Our search strategy yielded 562 patients with a confirmed genetic diagnosis of GLUT1 deficiency syndrome with a male/female ratio of 1.06 and a mean age at the diagnosis of 8.7 ± 6.7 years (range, 22 days–39 years; data available for 279 patients) (Fig. 1, Suppl. 1) [2, 3, 5,6,7,8,9,10,11,12,13,14,15,16,17,18,19,20,21,22,23,24,25,26,27,28,29,30,31,32,33,34,35,36,37,38,39,40,41,42,43,44,45,46,47,48,49,50,51,52,53,54,55,56,57,58,59,60,61,62,63,64,65,66,67,68,69,70,71,72,73,74,75,76,77,78,79,80,81,82,83,84,85,86,87,88,89,90,91,92,93,94,95,96,97,98,99,100,101,102,103,104,105,106,107,108,109,110,111,112,113,114,115,116,117,118,119,120,121,122,123,124,125,126,127,128,129,130,131,132,133,134,135,136,137,138,139,140].
Lumbar puncture was mostly performed before the molecular-genetic confirm (Suppl. 1).
Epileptic seizures were reported in 457 patients (Suppl. 1). Predominant seizure types at the onset mainly included absences (151 patients), myoclonic (95 patients), and generalized tonic-clonic seizures (97 patients) while focal onset was observed in 70 patients (Suppl. 1). EEG features were reported in 244 patients. The most frequent EEG patterns included diffuse spike and wave discharges (127 patients) with a frequency of 3–4 Hz being reported in 17 patients and a frequency of 1.5–2.5 Hz in 15 patients (Suppl. 1). Focal epileptiform abnormalities and slow abnormalities were respectively detected in 47 and 55 patients (Suppl. 1).
Data about the administered antiseizure medications were available for 208 published patients while details about the related therapeutic response were provided in 118 cases (seizures reduction reported in 53) (Suppl. 1). A remarkable proportion of them had received GLUT1 inhibitors such as valproate (95 patients), benzodiazepines (9 patients), phenobarbital (19 patients), or phenytoin (11 patients) before the diagnosis (Suppl. 1) with an apparently paradoxical efficacy in 26 patients.
Four hundred forty-eight patients presented with movement disorders mainly including intermittent or persistent ataxia (262 patients), dystonia (190 patients), paroxysmal exercise-induced dyskinesia (81 patients), and different pyramidal signs (78 patients) (Suppl. 1).
A neurodevelopmental disorder was diagnosed in 404 patients (Suppl. 1). An intellectual disability was assessed in 247 patients (25 patients had a borderline intelligence quotient (IQ) while different degrees of delay in the achievement of developmental milestones were reported in 78 patients (Suppl. 1) with the predominant involvement of language domains in 29 patients and of learning in other 31 cases (Suppl. 1)).
Details about the administration of ketogenic diet were reported for 379 patients; data about the response was available for 263 patients and 234 of them experienced a clinical improvement of epilepsy and/or movement disorders (Suppl. 1).
The duration of follow-up was reported for 89 patients (mean duration = 3.05 ± 3.95 years) (Suppl. 1). Data about long-term outcome were reported for a proportion of patients ranging between 23.9 and 37.9% (213 about epilepsy, 149 about movement disorders, and 135 about neurodevelopmental disorders) (Suppl. 1). A reduction/disappearance of seizures was reported in 158 patients while motor symptoms improved in 116 patients and cognitive/developmental gains occurred in 91 (Suppl. 1).
Published genotypes included 21 variants carried by 55.2% of patients (Supplement 2). Most commonly reported variants included c.997C>T (p.Arg333Trp), c.376C>T (p.Arg126Cys), c.283_284delinsAT (p.Ser95Ile), c.377G>A (p.Arg126His), and c.884C>T (p.Thr295Met). Most of the variants were scarcely correlated with the values of CSF biomarkers with a distribution covering all possible biochemical phenotypes. c.997C>T (p.Arg333Trp), c.457C>T (p.Arg153Cys), and c.884C>T (p.Thr295Met) were predominantly observed in patients with CSF glucose ≤ 2.2 mmol/L and in patients with CSF/blood glucose ratio ≤ 0.45 (Supplement 1). Conversely, c.283_284delinsAT (p.Ser95Ile) was mainly observed in patients with CSF glucose > 2.2 mmol/L (Supplement 1).
CSF biomarkers and associated phenotypes
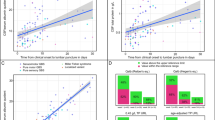
Table 1 and Figure 2 summarize the available data about levels of CSF biomarkers and associated phenotypes.
ROC analysis evidenced that CSF glucose had a sensitivity of 87%, a specificity of 100%, and a Youden index of 87% at 2.2 mmol/L. CSF/blood glucose ratio showed a sensitivity of 87%, a specificity of 100%, and a Youden index of 87% at values > 0.45. Sensitivity, specificity, and Youden index for CSF lactate at 1.0 ng/mL were 95%, 98%, and 93%, respectively.
Patients with CSF glucose ≤ 2.2 mmol/L and CSF/blood glucose ratio ≤ 0.45 presented with an earlier onset of symptoms and received an earlier molecular genetic confirm (Table 1).
Absence seizures, paroxysmal exercise-induced dyskinesia, and intellectual disability were significantly associated with a CSF/blood glucose ratio ≤ 0.45 with a relevant impact of sexual differences (Table 1).
The relationships between CSF parameters and developmental functions other than intelligent quotient were scarcely explorable because of the paucity of available data (Table 1; Supplement 1).
Positive response to ketogenic diet was more commonly reported in patients with CSF glucose ≤ 2.2 mmol/L. The same group had a significant response also to antiseizure medications but not to combined treatment (antiseizure medication + ketogenic diet) (Table 1). A significant response to antiseizure medications but not to ketogenic diet was observed in patients with CSF lactate higher than 1 mmol/L (Table 1).
Discussion
This systematic review suggested a relationship between the levels of CSF biomarkers and the distribution of some clinical parameters (age at the onset of symptoms, seizure and movement disorder types, cognitive profiles, and efficacy of available treatments) in patients with GLUT1 deficiency syndrome (Table 1).
The reliability of hypoglycorrhachia as diagnostic biomarker has been acquired since the last decade, when a retrospective analysis on 147 patients evidenced that CSF was below the 10th percentile of reference range in all published patients while CSF blood/glucose ratio was normal in 10% and data about CSF lactate were often not informative [141]. It was also evidenced that CSF glucose may range between 0.9 to 2.8 mmol/L in GLUT1 deficiency, and milder phenotypes may have CSF values between 2.2 and 2.9 mmol/L [1, 141]. Low CSF glucose mirrors the impoverishment of neuronal bioenergetic resources and might be better correlated with more severe phenotypes [142]. The herein reported data confirmed that hypoglycorrhachia was associated with factors having a relevant therapeutic and prognostic impact (e.g., earlier onset of symptoms and efficacy of ketogenic diet and/or antiseizure medications) (Table 1). The negative impact of hypoglycorrhachia on the develo** brain is probably independent by etiologies even if the severity of its effects may vary in the different age ranges [143,144,145,146]. The concept of “window of vulnerability” to the damages, induced by the low quote of glucose available to face the increased energy demands by the immature brain in the first months of life, might explain the worst outcome observed in late-treated patients with hypoglycorrhachia and earlier onset of symptoms [2, 108]. This window was placed by some authors between the first and the sixth month after birth and overlapped with the ideal timing for the beginning of ketogenic diet and the optimization of the related therapeutic results [2, 75].
CSF blood/glucose ratio may be considered an index of the degree of transporter function impairment with a higher sensitivity towards the detection of later onset and less severe phenotypes in which a residual activity of GLUT1 might be preserved [142]. The significant association of CSF/blood glucose ratio ≤ 0.45 with sex differences that was observed in published patients has no clear explanations (Table 1). No evident sex predisposition to GLUT1 deficiency was highlighted in the literature even if a negative regulation of GLUT1 protein mediated by estrogens has been reported in in vitro models [1, 147].
The association between low CSF/blood glucose ratio and absence seizures supported the results of previous studies that had highlighted the etiological role of SLC2A1 pathogenic variants in a proportion of cases ranging between 5.6% and 10% of all patients presenting with a childhood onset absence epilepsy [37, 105, 148]. Other authors had evidenced the same pathogenic role in a lower percentage of cases (1.4%) if the analyzed cohorts included patients with all types of idiopathic generalized epileptic syndromes [37, 105, 149]. In these cases, the indication for a lumbar puncture should be mandatory for children in which epilepsy is associated with other clinical hallmarks such as the predominance of seizures after periods of fasting, developmental impairment, or paroxysmal exercise-induced dyskinesia [105]. The lack of significance for seizure types other than absences might contraindicate the procedure especially if epilepsy is the only clinical manifestation [105, 149].
The pathomechanisms behind the higher frequency of early onset absences among patients with a lower CSF/blood/glucose ratio might result from a lower functional adaptability to energy deprivation of mutated neuronal transporters in the networks involving thalamus and connected cortical areas including posterior cingulate cortex, precuneus, angular gyrus, supramarginal gyrus, parietal superior, and occipital mid-region [37, 78, 105, 148, 149] (Table 1). Similar mechanisms might be involved in the impairment of astrocyte-to-neuron lactate shuttles in putamen and cortico-striatal pathways in patients with paroxysmal exercise-induced dyskinesia [78].
The assessed links between CSF/blood glucose ratio and intellectual disability are probably due to the lower ability of impaired cerebral GLUT1 to face the higher functional request of develo** brain, and it was firstly highlighted in a nationwide survey including 33 Japanese patients carrying missense variants of SLC2A1 [71]. A comparable correlation between CSF/blood glucose ratio and severity of speech and language impairment was not demonstrated in a smaller Italian series of eight patients [127].
Data from the analyzed literature did not demonstrate any association between lactate levels and developmental/clinical hallmarks of GLUT1 deficiency (Table 1) despite various basic/science and clinical studies highlighted the role of lactate in various cerebral networks, especially the ones involved in learning and memory [142, 150]. A better response to antiseizure medications was evidenced in patients with normal levels of lactate suggesting a less-compromised epilepsy phenotype in patients with a better basal energy metabolic compensation (Table 1).
The maintenance of lumbar puncture in the early diagnostic work-up of patients with GLUT1 deficiency syndrome, despite the increased quote of rapid turnaround time for genetic testing, has relevant prognostic implications because it still allows an earlier access to an effective disease-modifying treatment such as ketogenic diet. The herein reported data highlighted a more significant response to ketogenic in patients with CSF glucose ≤ 2.2 mmol/L while significance was not relevant in patients with low CSF/blood ratio (Table 1). Conversely, another recent systematic review of 230 published patients confirmed significant improvement in movement disorders in 104 out of 127 patients with better results in children with higher CSF/blood glucose ratio [3]. Another direct relationship between CSF/blood glucose ratio and total and verbal IQ improvement, after the introduction of ketogenic diet, was found in a smaller single center series of 14 patients [75].
Few correlations between genotypes and CSF glucose and CSF/blood glucose ratio may be highlighted. Variants c.997C>T (p.Arg333Trp) and c.457C>T (p.Arg153Cys) result in a less flexible and efficient glucose transport because of a higher quote of salt bridges stabilizing the conformation of GLUT1 protein and reducing electrostatic interactions during the activation of its intracellular and transmembrane segments [151]. The variant c.884C>T (p.Thr295Met) results in conformational changes that inhibit the access of glucose molecules in the exofacial site of the transporter [152].
Some limitations, mainly due to the predominant retrospective nature of the collected data, should be considered in the interpretation of the results of this systematic review: (a) differences in the ages of clinical evaluation, cerebrospinal fluid acquisition, achievement of molecular genetic confirm, and introduction of ketogenic diet or antiseizure medications; (b) lack of CSF measurements for a considerable number of published patients; and (c) differences in the methodologies used for the definition of phenotypic severity, clinical variability, response to treatments, and developmental outcome.
Conclusions
The analysis of the literature confirmed the usefulness of lumbar puncture for the early identification of patients with severe and mild phenotypes of GLUT1 deficiency and the subsequent prognostic implications of an earlier initiation of ketogenic diet. CSF analysis is easily and diffusively available diagnostic tool and contributes to a faster diagnostic work-up in patients with more severe phenotypes. The turnaround time of ultra-rapid next-generation sequencing techniques will not probably impact on the real-world therapeutic planning for the next few years. The results of this systematic review highlighted that a lumbar puncture should be strongly considered when severe developmental delay, paroxysmal exercise-induced dyskinesia, and early onset absences co-exist.
Abbreviations
- CSF:
-
Cerebrospinal fluid
- GLUT1:
-
Glucose transporter 1
- EEG:
-
Electroencephalogram
- FDG PET:
-
18-F-fluorodeoxyglucose positron emission tomography
- IQ:
-
Intelligence quotient
- SLC2A1:
-
Solute carrier family 2 member 1
- ADHD:
-
Attention deficit hyperactivity disorder
- F:
-
Female
- ID:
-
Intellectual disability
- IQ:
-
Intelligent quotient
- M:
-
Male
- N:
-
No
- NA:
-
Not available
- Y:
-
Yes
- M:
-
Mean
- SD:
-
Standard deviation
- PED:
-
Paroxysmal exercise‐induced dyskinesia
- GDD:
-
Global developmental delay
- ID:
-
Intellectual disability
References
Koch H, Weber YG (2019) The glucose transporter type 1 (GLUT1) syndromes. Epilepsy Behav 91:90–93
Klepper J, Leiendecker B (2007) GLUT1 deficiency syndrome–2007 update. Dev Med Child Neurol 49:707–16
Schwantje M, Verhagen LM, Hasselt PM, Fuchs SA (2020) Glucose transporter type 1 deficiency syndrome and the ketogenic diet. J Inherit Metab Dis 43:216–222
Mochel F, Gras D, Luton MP, Nizou M, Giovannini D, Delattre C, Aubart M, Barth M, De Saint-Martin A, Doummar D, Essid N, Garros A, Le Camus CH, Hoebeke C, The Tich SN, Perivier M, Rivera S, Rolland A, Roubertie A, Sarret C, Sevin C, Ville D, Sitbon M, Costa JM, Pons R, Garcia-Cazorla A, Vuillaumier S, Petit V, Boespflug-Tanguy O, De Vivo DC; MetaGLUT1 Study Group. Prospective multicenter validation of a simple blood test for the diagnosis of GLUT1 deficiency syndrome. Neurology. 2023; 100(23): e2360-e2373.
Peters TMA, Merx J, Kooijman PC, Noga M, de Boer S, van Gemert LA, Salden G, Engelke UFH, Lefeber DJ, van Outersterp RE, Berden G, Boltje TJ, Artuch R, Pías-Peleteiro L, García-Cazorla Á, Barić I, Thöny B, Oomens J, Martens J, Wevers RA, Verbeek MM, Coene KLM, Willemsen MAAP (2023) Novel cerebrospinal fluid biomarkers of glucose transporter type 1 deficiency syndrome: implications beyond the brain’s energy deficit. J Inherit Metab Dis. 46(1):66–75
Diomedi M, Gan-Or Z, Placidi F et al (2016) A 23 years follow-up study identifies GLUT1 deficiency syndrome initially diagnosed as complicated hereditary spastic paraplegia. Eur J Med Genet 59(11):564–568. https://doi.org/10.1016/j.ejmg.2016.10.003
Tornese G, Patti G, Pellegrin MC et al (2020) A case report of glucose transporter 1 deficiency syndrome with growth hormone deficiency diagnosed before starting ketogenic diet. Ital J Pediatr 46(1):119. https://doi.org/10.1186/s13052-020-00888-3
Çolak R, Alkan Özdemir S, Yangın Ergon E, Kağnıcı M, Çalkavur Ş (2017) A different SLC2A1 gene mutation in Glut 1 deficiency syndrome: c.734A>C. Balkan Med J. 34(6):580–583. https://doi.org/10.4274/balkanmedj.2016.1376
Ito Y, Oguni H, Ito S, Oguni M, Osawa M (2011) A modified Atkins diet is promising as a treatment for glucose transporter type 1 deficiency syndrome. Dev Med Child Neurol 53(7):658–663. https://doi.org/10.1111/j.1469-8749.2011.03961.x
Vermeer S, Koolen DA, Visser G et al (2007) A novel microdeletion in 1(p34.2p34.3), involving the SLC2A1 (GLUT1) gene, and severe delayed development. Dev Med Child Neurol. 49(5):380–384. https://doi.org/10.1111/j.1469-8749.2007.00380.x
Üstyol A, Takahashi S, Hatipoğlu HU, Duman MA, Elevli M, Selçuk-Duru HN (2019) A novel mutation in SLC2A1 gene causing GLUT-1 deficiency syndrome in a young adult patient. Turk J Pediatr 61(6):946–948. https://doi.org/10.24953/turkjped.2019.06.018
Weller CM, Leen WG, Neville BGR et al (2015) A novel SLC2A1 mutation linking hemiplegic migraine with alternating hemiplegia of childhood. Cephalalgia 35(1):10–15. https://doi.org/10.1177/0333102414532379
Gras D, Cousin C, Kappeler C et al (2017) A simple blood test expedites the diagnosis of glucose transporter type 1 deficiency syndrome. Ann Neurol 82(1):133–138. https://doi.org/10.1002/ana.24970
Ohshiro-Sasaki A, Shimbo H, Takano K, Wada T, Osaka H (2014) A three-year-old boy with glucose transporter type 1 deficiency syndrome presenting with episodic ataxia. Pediatr Neurol 50(1):99–100. https://doi.org/10.1016/j.pediatrneurol.2013.09.002
Mullen SA, Suls A, De Jonghe P, Berkovic SF, Scheffer IE (2010) Absence epilepsies with widely variable onset are a key feature of familial GLUT1 deficiency. Neurology 75(5):432–440. https://doi.org/10.1212/WNL.0b013e3181eb58b4
Tchapyjnikov D, Mikati MA (2018) Acetazolamide-responsive episodic ataxia without baseline deficits or seizures secondary to GLUT1 deficiency: a case report and review of the literature. Neurologist 23(1):17–18. https://doi.org/10.1097/NRL.0000000000000168
Akman CI, Engelstad K, Hinton VJ et al (2010) Acute hyperglycemia produces transient improvement in glucose transporter type 1 deficiency. Ann Neurol 67(1):31–40. https://doi.org/10.1002/ana.21797
Liu Y, Bao X, Wang D et al (2012) Allelic variations of glut-1 deficiency syndrome: the Chinese experience. Pediatr Neurol 47(1):30–34. https://doi.org/10.1016/j.pediatrneurol.2012.04.010
Bawazir WM, Gevers EF, Flatt JF et al (2012) An infant with pseudohyperkalemia, hemolysis, and seizures: cation-leaky GLUT1-deficiency syndrome due to a SLC2A1 mutation. J Clin Endocrinol Metab 97(6):E987-993. https://doi.org/10.1210/jc.2012-1399
Shibata T, Kobayashi K, Yoshinaga H, Ono H, Shinpo M, Kagitani-Shimono K (2017) Another case of glucose transporter 1 deficiency syndrome with periventricular calcification, cataracts, hemolysis, and pseudohyperkalemia. Neuropediatrics 48(5):390–393. https://doi.org/10.1055/s-0037-1603520
Yubero D, O’Callaghan M, Montero R et al (2014) Association between coenzyme Q10 and glucose transporter (GLUT1) deficiency. BMC Pediatr 14:284. https://doi.org/10.1186/s12887-014-0284-5
Friedman JRL, Thiele EA, Wang D et al (2006) Atypical GLUT1 deficiency with prominent movement disorder 1 responsive to ketogenic diet. Mov Disord 21(2):241–245. https://doi.org/10.1002/mds.20660
Brockmann K, Wang D, Korenke CG et al (2001) Autosomal dominant glut-1 deficiency syndrome and familial epilepsy. Ann Neurol 50(4):476–485. https://doi.org/10.1002/ana.1222
Klepper J, Willemsen M, Verrips A et al (2001) Autosomal dominant transmission of GLUT1 deficiency. Hum Mol Genet 10(1):63–68. https://doi.org/10.1093/hmg/10.1.63
Klepper J, Scheffer H, Elsaid MF, Kamsteeg EJ, Leferink M, Ben-Omran T (2009) Autosomal recessive inheritance of GLUT1 deficiency syndrome. Neuropediatrics 40(5):207–210. https://doi.org/10.1055/s-0030-1248264
Klepper J, Salas-Burgos A, Gertsen E, Fischbarg J (2005) Bench meets bedside: a 10-year-old girl and amino acid residue glycine 75 of the facilitative glucose transporter GLUT1. Biochemistry 44(38):12621–12626. https://doi.org/10.1021/bi051079t
Gaspard N, Suls A, Vilain C, De Jonghe P, Van Bogaert P (2011) “Benign” myoclonic epilepsy of infancy as the initial presentation of glucose transporter-1 deficiency. Epileptic Disord 13(3):300–303. https://doi.org/10.1684/epd.2011.0452
Vaudano AE, Olivotto S, Ruggieri A et al (2017) Brain correlates of spike and wave discharges in GLUT1 deficiency syndrome. Neuroimage Clin 13:446–454. https://doi.org/10.1016/j.nicl.2016.12.026
Belal T, Day-Salvatore DL, Chandra S (2018) Case 6: seizures and low cerebrospinal fluid glucose in a 4-day-old boy. Pediatr Rev 39(5):265–266. https://doi.org/10.1542/pir.2017-0154
Akasaka M, Kamei A, Araya N, Oyama K, Sasaki M (2018) Characteristic proton magnetic resonance spectroscopy in glucose transporter type 1 deficiency syndrome. Pediatr Int 60(10):978–979. https://doi.org/10.1111/ped.13672
Pérez-Dueñas B, Prior C, Ma Q et al (2009) Childhood chorea with cerebral hypotrophy: a treatable GLUT1 energy failure syndrome. Arch Neurol 66(11):1410–1414. https://doi.org/10.1001/archneurol.2009.236
Ito Y, Gertsen E, Oguni H et al (2005) Clinical presentation, EEG studies, and novel mutations in two cases of GLUT1 deficiency syndrome in Japan. Brain Dev 27(4):311–317. https://doi.org/10.1016/j.braindev.2004.09.010
Klepper J, Wang D, Fischbarg J et al (1999) Defective glucose transport across brain tissue barriers: a newly recognized neurological syndrome. Neurochem Res 24(4):587–594. https://doi.org/10.1023/a:1022544131826
Pawlik W, Okulewicz P, Pawlik J, Krzywińska-Zdeb E (2022) Diagnostic and clinical manifestation differences of glucose transporter type 1 deficiency syndrome in a family with SLC2A1 gene mutation. Int J Environ Res Public Health 19(6). https://doi.org/10.3390/ijerph19063279
Kim H, Lee JS, Lee Y et al (2019) Diagnostic challenges associated with GLUT1 deficiency: phenotypic variabilities and evolving clinical features. Yonsei Med J. 60(12):1209–1215. https://doi.org/10.3349/ymj.2019.60.12.1209
Ramm-Pettersen A, Stabell KE, Nakken KO, Selmer KK (2014) Does ketogenic diet improve cognitive function in patients with GLUT1-DS? A 6- to 17-month follow-up study. Epilepsy Behav 39:111–115. https://doi.org/10.1016/j.yebeh.2014.08.015
Arsov T, Mullen SA, Damiano JA et al (2012) Early onset absence epilepsy: 1 in 10 cases is caused by GLUT1 deficiency. Epilepsia 53(12):e204-207. https://doi.org/10.1111/epi.12007
von Moers A, Brockmann K, Wang D et al (2002) EEG features of glut-1 deficiency syndrome. Epilepsia 43(8):941–945. https://doi.org/10.1046/j.1528-1157.2002.50401.x
Anheim M, Maillart E, Vuillaumier-Barrot S et al (2011) Excellent response to acetazolamide in a case of paroxysmal dyskinesias due to GLUT1-deficiency. J Neurol 258(2):316–317. https://doi.org/10.1007/s00415-010-5702-5
Logel SN, Connor EL, Hsu DA, Fenske RJ, Paloian NJ, De Vivo DC (2021) Exploring diazoxide and continuous glucose monitoring as treatment for Glut1 deficiency syndrome. Ann Clin Transl Neurol 8(11):2205–2209. https://doi.org/10.1002/acn3.51462
Woo SB, Lee KH, Kang HC, Yang H, De Vivo DC, Kim SK (2012) First report of glucose transporter 1 deficiency syndrome in Korea with a novel splice site mutation. Gene 506(2):380–382. https://doi.org/10.1016/j.gene.2012.06.095
Fung EL wah, Ho YY, Hui J, et al. First report of GLUT1 deficiency syndrome in Chinese patients with novel and hot spot mutations in SLC2A1 gene. Brain Dev 2011;33(2):170-173. https://doi.org/10.1016/j.braindev.2010.03.009
Wolking S, Becker F, Bast T et al (2014) Focal epilepsy in glucose transporter type 1 (Glut1) defects: case reports and a review of literature. J Neurol 261(10):1881–1886. https://doi.org/10.1007/s00415-014-7433-5
Wang D, Yang H, Shi L et al (2008) Functional studies of the T295M mutation causing Glut1 deficiency: glucose efflux preferentially affected by T295M. Pediatr Res 64(5):538–543. https://doi.org/10.1203/PDR.0b013e318184d2b5
Mullen SA, Marini C, Suls A et al (2011) Glucose transporter 1 deficiency as a treatable cause of myoclonic astatic epilepsy. Arch Neurol 68(9):1152–1155. https://doi.org/10.1001/archneurol.2011.102
Mohammad SS, Coman D, Calvert S (2014) Glucose transporter 1 deficiency syndrome and hemiplegic migraines as a dominant presenting clinical feature. J Paediatr Child Health 50(12):1025–1026. https://doi.org/10.1111/jpc.12613
Appavu B, Mangum T, Obeid M (2015) Glucose transporter 1 deficiency: a treatable cause of opsoclonus and epileptic myoclonus. Pediatr Neurol 53(4):364–366. https://doi.org/10.1016/j.pediatrneurol.2015.05.019
Hoshino H, Takayama K, Ishii A, Takahashi Y, Kanemura H (2020) Glucose transporter type 1 deficiency syndrome associated with autoantibodies to glutamate receptors. Brain Dev 42(9):686–690. https://doi.org/10.1016/j.braindev.2020.05.010
Haberlandt E, Karall D, Jud V et al (2014) Glucose transporter type 1 deficiency syndrome effectively treated with modified Atkins diet. Neuropediatrics 45(2):117–119. https://doi.org/10.1055/s-0033-1349225
Koy A, Assmann B, Klepper J, Mayatepek E (2011) Glucose transporter type 1 deficiency syndrome with carbohydrate-responsive symptoms but without epilepsy. Dev Med Child Neurol 53(12):1154–1156. https://doi.org/10.1111/j.1469-8749.2011.04082
Gramer G, Wolf NI, Vater D et al (2012) Glucose transporter-1 (GLUT1) deficiency syndrome: diagnosis and treatment in late childhood. Neuropediatrics 43(3):168–171. https://doi.org/10.1055/s-0032-1315433
Leen WG, Klepper J, Verbeek MM et al (2010) Glucose transporter-1 deficiency syndrome: the expanding clinical and genetic spectrum of a treatable disorder. Brain 133(Pt 3):655–670. https://doi.org/10.1093/brain/awp336
Ismayilova N, Hacohen Y, MacKinnon AD, Elmslie F, Clarke A (2018) GLUT-1 deficiency presenting with seizures and reversible leukoencephalopathy on MRI imaging. Eur J Paediatr Neurol 22(6):1161–1164. https://doi.org/10.1016/j.ejpn.2018.02.002
Roulet-Perez E, Ballhausen D, Bonafé L, Cronel-Ohayon S, Maeder-Ingvar M (2008) Glut-1 deficiency syndrome masquerading as idiopathic generalized epilepsy. Epilepsia 49(11):1955–1958. https://doi.org/10.1111/j.1528-1167.2008.01654.x
Wang D, Pascual JM, Yang H et al (2005) Glut-1 deficiency syndrome: clinical, genetic, and therapeutic aspects. Ann Neurol 57(1):111–118. https://doi.org/10.1002/ana.20331
Overweg-Plandsoen WCG, Groener JEM, Wang D et al (2003) GLUT-1 deficiency without epilepsy–an exceptional case. J Inherit Metab Dis. 26(6):559–563. https://doi.org/10.1023/a:1025999914822
Rotstein M, Doran J, Yang H, Ullner PM, Engelstad K, De Vivo DC (2009) Glut1 deficiency and alternating hemiplegia of childhood. Neurology. 73(23):2042–2044. https://doi.org/10.1212/WNL.0b013e3181c55ebf
Graham JMJ (2012) GLUT1 deficiency syndrome as a cause of encephalopathy that includes cognitive disability, treatment-resistant infantile epilepsy and a complex movement disorder. Eur J Med Genet 55(5):332–334. https://doi.org/10.1016/j.ejmg.2011.11.009
Klepper J, Engelbrecht V, Scheffer H, van der Knaap MS, Fiedler A (2007) GLUT1 deficiency with delayed myelination responding to ketogenic diet. Pediatr Neurol 37(2):130–133. https://doi.org/10.1016/j.pediatrneurol.2007.03.009
Joshi C, Greenberg CR, De Vivo D, Wang D, Chan-Lui W, Booth FA (2008) GLUT1 deficiency without epilepsy: yet another case. J Child Neurol 23(7):832–834. https://doi.org/10.1177/0883073808314896
Rotstein M, Engelstad K, Yang H et al (2010) Glut1 deficiency: inheritance pattern determined by haploinsufficiency. Ann Neurol 68(6):955–958. https://doi.org/10.1002/ana.22088
Ramm-Pettersen A, Nakken KO, Skogseid IM et al (2013) Good outcome in patients with early dietary treatment of GLUT-1 deficiency syndrome: results from a retrospective Norwegian study. Dev Med Child Neurol 55(5):440–447. https://doi.org/10.1111/dmcn.12096
Nakagama Y, Isojima T, Mizuno Y, Takahashi N, Kitanaka S, Igarashi T (2012) Growth hormone deficiency: a possible complication of glucose transporter 1 deficiency? Acta Paediatr 101(6):e259-262. https://doi.org/10.1111/j.1651-2227.2012.02606.x
Pascual JM, Van Heertum RL, Wang D, Engelstad K, De Vivo DC (2002) Imaging the metabolic footprint of Glut1 deficiency on the brain. Ann Neurol 52(4):458–464. https://doi.org/10.1002/ana.10311
Gowda VK, Sheshu S (2015) Intermittent ataxia with early onset absence epilepsy in glucose transporter type 1 deficiency syndrome. Indian Pediatr 52(11):997
Madaan P, Jauhari P, Chakrabarty B, Gulati S (2019) Jeavons syndrome in a family with GLUT1-deficiency syndrome. Seizure 71:158–160. https://doi.org/10.1016/j.seizure.2019.07.011
Alter AS, Engelstad K, Hinton VJ et al (2015) Long-term clinical course of Glut1 deficiency syndrome. J Child Neurol 30(2):160–169. https://doi.org/10.1177/0883073814531822
Anand G, Padeniya A, Hanrahan D et al (2011) Milder phenotypes of glucose transporter type 1 deficiency syndrome. Dev Med Child Neurol 53(7):664–668. https://doi.org/10.1111/j.1469-8749.2011.03949.x
Ito S, Oguni H, Ito Y, Ishigaki K, Ohinata J, Osawa M (2008) Modified Atkins diet therapy for a case with glucose transporter type 1 deficiency syndrome. Brain Dev 30(3):226–228. https://doi.org/10.1016/j.braindev.2007.08.006
Takahashi S, Ohinata J, Suzuki N et al (2008) Molecular analysis and anticonvulsant therapy in two patients with glucose transporter 1 deficiency syndrome: a successful use of zonisamide for controlling the seizures. Epilepsy Res 80(1):18–22. https://doi.org/10.1016/j.eplepsyres.2008.03.010
Nakamura S, Osaka H, Muramatsu S, Aoki S, Jimbo EF, Yamagata T (2015) Mutational and functional analysis of glucose transporter I deficiency syndrome. Mol Genet Metab 116(3):157–162. https://doi.org/10.1016/j.ymgme.2015.08.006
Ito Y, Takahashi S, Kagitani-Shimono K et al (2015) Nationwide survey of glucose transporter-1 deficiency syndrome (GLUT-1DS) in Japan. Brain Dev 37(8):780–789. https://doi.org/10.1016/j.braindev.2014.11.006
Slaughter L, Vartzelis G, Arthur T (2009) New GLUT-1 mutation in a child with treatment-resistant epilepsy. Epilepsy Res 84(2–3):254–256. https://doi.org/10.1016/j.eplepsyres.2009.01.004
Juozapaite S, Praninskiene R, Burnyte B, Ambrozaityte L, Skerliene B (2017) Novel mutation in a patient with late onset GLUT1 deficiency syndrome. Brain Dev 39(4):352–355. https://doi.org/10.1016/j.braindev.2016.11.007
De Giorgis V, Masnada S, Varesio C et al (2019) Overall cognitive profiles in patients with GLUT1 deficiency syndrome. Brain Behav 9(3):e01224. https://doi.org/10.1002/brb3.1224
Lee MS, Kim YJ, Kim EJ, Lee MJ (2015) Overlap of autism spectrum disorder and glucose transporter 1 deficiency syndrome associated with a heterozygous deletion at the 1p34.2 region. J Neurol Sci. 356(1–2):212–214. https://doi.org/10.1016/j.jns.2015.06.041
Kitamura Y, Okumura A, Hayashi M et al (2012) Oxidative stress markers and phosphorus magnetic resonance spectroscopy in a patient with GLUT1 deficiency treated with modified Atkins diet. Brain Dev 34(5):372–375. https://doi.org/10.1016/j.braindev.2011.08.005
Suls A, Dedeken P, Goffin K et al (2008) Paroxysmal exercise-induced dyskinesia and epilepsy is due to mutations in SLC2A1, encoding the glucose transporter GLUT1. Brain 131(Pt 7):1831–1844. https://doi.org/10.1093/brain/awn113
Urbizu A, Cuenca-León E, Raspall-Chaure M et al (2010) Paroxysmal exercise-induced dyskinesia, writer’s cramp, migraine with aura and absence epilepsy in twin brothers with a novel SLC2A1 missense mutation. J Neurol Sci 295(1–2):110–113. https://doi.org/10.1016/j.jns.2010.05.017
Pearson TS, Pons R, Engelstad K, Kane SA, Goldberg ME, De Vivo DC (2017) Paroxysmal eye-head movements in Glut1 deficiency syndrome. Neurology 88(17):1666–1673. https://doi.org/10.1212/WNL.0000000000003867
Zorzi G, Castellotti B, Zibordi F, Gellera C, Nardocci N (2008) Paroxysmal movement disorders in GLUT1 deficiency syndrome. Neurology 71(2):146–148. https://doi.org/10.1212/01.wnl.0000316804.10020.ba
Reis S, Matias J, Machado R, Monteiro JP (2018) Paroxysmal ocular movements - an early sign in Glut1 deficiency syndrome. Metab Brain Dis 33(4):1381–1383. https://doi.org/10.1007/s11011-018-0225-3
Chambon R, Vuillaumier-Barrot S, Seta N, Wagner S, Sarret C (2013) Partial effectiveness of acetazolamide in a mild form of GLUT1 deficiency: a pediatric observation. Mov Disord 28(12):1749–51
Bourque DK, Cordeiro D, Nimmo GAM, Kobayashi J, Mercimek-Andrews S (2021) Phenotypic and genotypic spectrum of glucose transporter-1 deficiency syndrome. Can J Neurol Sci 48(6):826–830. https://doi.org/10.1017/cjn.2021.3
Parolin G, Drigo P, Toldo I et al (2011) Pre- and postprandial electroencephalography in glucose transporter type 1 deficiency syndrome: an illustrative case to discuss the concept of carbohydrate responsiveness. J Child Neurol 26(1):103–108. https://doi.org/10.1177/0883073810376444
Byrne S, Kearns J, Carolan R, Mc Menamin J, Klepper J, Webb D (2011) Refractory absence epilepsy associated with GLUT-1 deficiency syndrome. Epilepsia 52(5):1021–1024. https://doi.org/10.1111/j.1528-1167.2011.02989.x
Shiohama T, Fujii K, Takahashi S, Nakamura F, Kohno Y (2013) Reversible white matter lesions during ketogenic diet therapy in glucose transporter 1 deficiency syndrome. Pediatr Neurol 49(6):493–496. https://doi.org/10.1016/j.pediatrneurol.2013.06.004
Castellotti B, Ragona F, Freri E et al (2019) Screening of SLC2A1 in a large cohort of patients suspected for Glut1 deficiency syndrome: identification of novel variants and associated phenotypes. J Neurol 266(6):1439–1448. https://doi.org/10.1007/s00415-019-09280-6
Leary LD, Wang D, Nordli DRJ, Engelstad K, De Vivo DC (2003) Seizure characterization and electroencephalographic features in Glut-1 deficiency syndrome. Epilepsia 44(5):701–707. https://doi.org/10.1046/j.1528-1157.2003.05302.x
Klepper J, Scheffer H, Leiendecker B et al (2005) Seizure control and acceptance of the ketogenic diet in GLUT1 deficiency syndrome: a 2- to 5-year follow-up of 15 children enrolled prospectively. Neuropediatrics 36(5):302–308. https://doi.org/10.1055/s-2005-872843
Coman DJ, Sinclair KG, Burke CJ et al (2006) Seizures, ataxia, developmental delay and the general paediatrician: glucose transporter 1 deficiency syndrome. J Paediatr Child Health 42(5):263–267. https://doi.org/10.1111/j.1440-1754.2006.00852.x
Klepper J, Leiendecker B, Heussinger N, Lausch E, Bosch F (2016) Severe hypertriglyceridemia in Glut1D on ketogenic diet. Neuropediatrics 47(2):132–136. https://doi.org/10.1055/s-0036-1572413
Hashimoto N, Kagitani-Shimono K, Sakai N et al (2011) SLC2A1 gene analysis of Japanese patients with glucose transporter 1 deficiency syndrome. J Hum Genet 56(12):846–851. https://doi.org/10.1038/jhg.2011.115
De Giorgis V, Teutonico F, Cereda C et al (2015) Sporadic and familial glut1ds Italian patients: a wide clinical variability. Seizure 24:28–32. https://doi.org/10.1016/j.seizure.2014.11.009
Fujii T, Morimoto M, Yoshioka H et al (2011) T295M-associated Glut1 deficiency syndrome with normal erythrocyte 3-OMG uptake. Brain Dev 33(4):316–320. https://doi.org/10.1016/j.braindev.2010.06.012
Gumus H, Bayram AK, Kardas F et al (2015) The effects of ketogenic diet on seizures, cognitive functions, and other neurological disorders in classical phenotype of glucose transporter 1 deficiency syndrome. Neuropediatrics 46(5):313–320. https://doi.org/10.1055/s-0035-1558435
Tzadok M, Nissenkorn A, Porper K et al (2014) The many faces of Glut1 deficiency syndrome. J Child Neurol 29(3):349–359. https://doi.org/10.1177/0883073812471718
Ivanova N, Peycheva V, Kamenarova K et al (2018) Three novel SLC2A1 mutations in Bulgarian patients with different forms of genetic generalized epilepsy reflecting the clinical and genetic diversity of GLUT1-deficiency syndrome. Seizure 54:41–44. https://doi.org/10.1016/j.seizure.2017.11.014
Akman CI, Provenzano F, Wang D et al (2015) Topography of brain glucose hypometabolism and epileptic network in glucose transporter 1 deficiency. Epilepsy Res 110:206–215. https://doi.org/10.1016/j.eplepsyres.2014.11.007
Levy B, Wang D, Ullner PM et al (2010) Uncovering microdeletions in patients with severe Glut-1 deficiency syndrome using SNP oligonucleotide microarray analysis. Mol Genet Metab 100(2):129–135. https://doi.org/10.1016/j.ymgme.2010.03.007
Vieker S, Schmitt J, Längler A, Schmidt W, Klepper J (2012) Unusual sensitivity to steroid treatment in intractable childhood epilepsy suggests GLUT1 deficiency syndrome. Neuropediatrics 43(5):275–8. https://doi.org/10.1055/s-0032-1324399
Willemsen MA, Vissers LE, Verbeek MM et al (2017) Upstream SLC2A1 translation initiation causes GLUT1 deficiency syndrome. Eur J Hum Genet 25(6):771–774. https://doi.org/10.1038/ejhg.2017.45
Dozières-Puyravel B, Zaman S, Petrou S et al (2019) Usefulness of diagnostic tools in a GLUT1 deficiency syndrome patient with 2 inherited mutations. Brain Dev 41(9):808–811. https://doi.org/10.1016/j.braindev.2019.05.008
Gökben S, Yılmaz S, Klepper J, Serdaroğlu G, Tekgül H (2011) Video/EEG recording of myoclonic absences in GLUT1 deficiency syndrome with a hot-spot R126C mutation in the SLC2A1 gene. Epilepsy Behav 21(2):200–202. https://doi.org/10.1016/j.yebeh.2011.03.027
Lebon S, Suarez P, Alija S et al (2015) When should clinicians search for GLUT1 deficiency syndrome in childhood generalized epilepsies? Eur J Paediatr Neurol 19(2):170–175. https://doi.org/10.1016/j.ejpn.2014.11.009
Klepper J, Flörcken A, Fischbarg J, Voit T (2003) Effects of anticonvulsants on GLUT1-mediated glucose transport in GLUT1 deficiency syndrome in vitro. Eur J Pediatr 162(2):84–89. https://doi.org/10.1007/s00431-002-1112-8
Natsume J, Ishihara N, Azuma Y et al (2021) Lenticular nuclei to thalamic ratio on PET is useful for diagnosis of GLUT1 deficiency syndrome. Brain Dev 43(1):69–77. https://doi.org/10.1016/j.braindev.2020.07.001
Angeli M, Vergadi E, Niotakis G, Raissaki M, Galanakis E (2022) Abnormal gait and hypoglycorrhachia in a toddler with seizures. Pediatr Investig 6(1):47–49. https://doi.org/10.1002/ped4.12311
Barthold M, Jurkutat A, Goetz R, Schubring L, Spiegler J, Fries AS, Kiesel L, Klepper J (2023) Timing of ketogenic dietary therapy (KDT) introduction and its impact on cognitive profiles in children with Glut1-DS-A preliminary study. Children (Basel) 10(4):681. https://doi.org/10.3390/children10040681
Awaad Yasser, Berry Ian, Tomoum Hoda, Elsayed Solaf (2015) A novel frameshift mutation in SLC2A1 associated with a mild form of glucose transporter type 1-related movement disorder. J Pediatr Neurol 13:088–091. https://doi.org/10.1055/s-0035-1556765
Cappuccio G, Pinelli M, Alagia M, Donti T, Day-Salvatore DL, Veggiotti P, De Giorgis V, Lunghi S, Vari MS, Striano P, Brunetti-Pierri N, Kennedy AD, Elsea SH (2017) Biochemical phenoty** unravels novel metabolic abnormalities and potential biomarkers associated with treatment of GLUT1 deficiency with ketogenic diet. PLoS One 12(9):e0184022. https://doi.org/10.1371/journal.pone.0184022
Fujii T, Ho YY, Wang D, De Vivo DC, Miyajima T, Wong HY, Tsang PT, Shirasaka Y, Kudo T, Ito M (2007) Three Japanese patients with glucose transporter type 1 deficiency syndrome. Brain Dev 29(2):92–7. https://doi.org/10.1016/j.braindev.2006.07.007
Hu Q, Shen Y, Su T, Liu Y, Xu S (2021) Clinical and genetic characteristics of Chinese children with GLUT1 deficiency syndrome: case report and literature review. Front Genet 22(12):734481. https://doi.org/10.3389/fgene.2021.734481
Klepper J, Leiendecker B, Eltze C, Heussinger N (2016) Paroxysmal nonepileptic events in Glut1 deficiency. Mov Disord Clin Pract 3(6):607–610. https://doi.org/10.1002/mdc3.12387
Kraoua I, Benrhouma H, Vuillaumier-Barrot S, Klaa H, Youssef-Turki IB (2015) A case of progressive chorea resulting from GLUT1 deficiency. Mov Disord Clin Pract 2(4):424–425. https://doi.org/10.1002/mdc3.12191
Leen WG, Taher M, Verbeek MM, Kamsteeg EJ, van de Warrenburg BP, Willemsen MA (2014) GLUT1 deficiency syndrome into adulthood: a follow-up study. J Neurol 261(3):589–99. https://doi.org/10.1007/s00415-014-7240-z
Magrinelli F, Mulroy E, Schneider SA, Latorre A, Di Lazzaro G, Hennig A, Grünewald S, De Vivo DC, Bhatia KP (2020) Criss-cross gait: a clue to glucose transporter type 1 deficiency syndrome. Neurology. 95(11):500–501. https://doi.org/10.1212/WNL.0000000000010502
Messana T, Russo A, Vergaro R, Boni A, Santucci M, Pini A (2018) Glucose transporter type 1 deficiency syndrome: developmental delay and early-onset ataxia in a novel mutation of the SLC2A1 gene. J Pediatr Neurosci. 13(4):496–499. https://doi.org/10.4103/JPN.JPN_169_17
Nakamura S, Ito Y, Hayakawa H, Aoki S, Yamagata T, Osaka H (2023) Establishment of a flow cytometry screening method for patients with glucose transporter 1 deficiency syndrome. Mol Genet Metab Rep. 2(34):100954. https://doi.org/10.1016/j.ymgmr.2022.100954
Olivotto S, Duse A, Bova SM, Leonardi V, Biganzoli E, Milanese A, Cereda C, Bertoli S, Previtali R, Veggiotti P (2022) Glut1 deficiency syndrome throughout life: clinical phenotypes, intelligence, life achievements and quality of life in familial cases. Orphanet J Rare Dis 17(1):365. https://doi.org/10.1186/s13023-022-02513-4
Sánchez-Lijarcio O, Yubero D, Leal F, Couce ML, González Gutiérrez-Solana L, López-Laso E, García-Cazorla À, Pías-Peleteiro L, de Azua Brea B, Ibáñez-Micó S, Mateo-Martínez G, Troncoso-Schifferli M, Witting-Enriquez S, Ugarte M, Artuch R, Pérez B (2022) The clinical and biochemical hallmarks generally associated with GLUT1DS may be caused by defects in genes other than SLC2A1. Clin Genet. 102(1):40–55. https://doi.org/10.1111/cge.14138
Sen S, Keough K, Gibson J (2015) Clinical reasoning: novel GLUT1-DS mutation: refractory seizures and ataxia. Neurology 84(15):e111-4. https://doi.org/10.1212/WNL.0000000000001467
Tayebi N, Leon-Ricardo B, McCall K, Mehinovic E, Engelstad K, Huynh V, Turner TN, Weisenberg J, Thio LL, Hruz P, Williams RSB, De Vivo DC, Petit V, Haller G, Gurnett CA (2023) Quantitative determination of SLC2A1 variant functional effects in GLUT1 deficiency syndrome. Ann Clin Transl Neurol. 10(5):787–801. https://doi.org/10.1002/acn3.51767
Wang YY, Zhou YQ, Luo LJ, Wang CJ, Shen N, Li H, Wang JW (2022) Ketogenic diet therapy in children with epilepsy caused by SLC2A1 mutations: a single-center single-arm retrospective study. World J Pediatr https://doi.org/10.1007/s12519-022-00620-7
Zuhal Yapici, Pinar Topaloğlu, Cuneyt Turkmen, Mefkure Eraksoy, Sameer Zuberi (2022) A patient with glucose transporter type 1 deficiency syndrome: paroxysmal choreoathetosis and cerebral positron-emission tomography findings. Neurol Sci Neurophysiol 39(1):53–55. https://doi.org/10.4103/nsn.nsn_127_21
Weber YG, Storch A, Wuttke TV, Brockmann K, Kempfle J, Maljevic S, Margari L, Kamm C, Schneider SA, Huber SM, Pekrun A, Roebling R, Seebohm G, Koka S, Lang C, Kraft E, Blazevic D, Salvo-Vargas A, Fauler M, Mottaghy FM, Münchau A, Edwards MJ, Presicci A, Margari F, Gasser T, Lang F, Bhatia KP, Lehmann-Horn F, Lerche H (2008) GLUT1 mutations are a cause of paroxysmal exertion-induced dyskinesias and induce hemolytic anemia by a cation leak. J Clin Invest 118(6):2157–68. https://doi.org/10.1172/JCI34438
Zanaboni MP, Pasca L, Villa BV, Faggio A, Grumi S, Provenzi L, Varesio C, De Giorgis V (2021) Characterization of speech and language phenotype in GLUT1DS. Children (Basel) 8(5):344. https://doi.org/10.3390/children8050344
Hung PC, Huang WL (2021) Leukoencephalopathy in infancy with glucose transporter type 1 deficiency syndrome. Pediatr Neonatol 62(1):117–118. https://doi.org/10.1016/j.pedneo.2020.08.010
Mauri A, Duse A, Palm G, Previtali R, Bova SM, Olivotto S, Benedetti S, Coscia F, Veggiotti P, Cereda C (2022) Molecular genetics of GLUT1DS Italian pediatric cohort: 10 novel disease-related variants and structural analysis. Int J Mol Sci 23(21):13560. https://doi.org/10.3390/ijms232113560
Kolic I, Radic Nisevic J, Vlasic Cicvaric I, ButoracAhel I, LahTomulic K, Segulja S, BarabaDekanic K, Serifi S, Ovuka A, Prpic I (2021) GLUT1 deficiency syndrome-early treatment maintains cognitive development? (Literature Review and Case Report). Genes (Basel) 12(9):1379. https://doi.org/10.3390/genes12091379
Takahashi S, Tanaka R, Takeguchi R, Kuroda M, Akaba Y, Ito Y (2020) The role of molecular analysis of SLC2A1 in the diagnostic workup of glucose transporter 1 deficiency syndrome. J Neurol Sci 416:117041. https://doi.org/10.1016/j.jns.2020.117041
Yildirim Mirac, Babayiğit Ömür, Ilgaz Fatma, Yalnizoglu Dilek, Topçu Meral (2021) Glucose transporter type 1 deficiency syndrome: a single-center case series. Türk Nöroloji Dergisi 27:343–346. https://doi.org/10.4274/tnd.2021.12979
Di Vito L, Licchetta L, Pippucci T, Baldassari S, Stipa C, Mostacci B, Alvisi L, Tinuper P, Bisulli F (2018) Phenotype variability of GLUT1 deficiency syndrome: description of a case series with novel SLC2A1 gene mutations. Epilepsy Behav 79:169–173. https://doi.org/10.1016/j.yebeh.2017.12.012
Chow CK & Wong SN, & Ma CK, & Luk Ho (2017). Glucose transporter type 1 deficiency syndrome in a 4-year-old Chinese boy. 22. 46-49.
Thouin A, Crompton DE (2016) Glut1 deficiency syndrome: absence epilepsy and La Soupe du Jour. Pract Neurol 16(1):50–2. https://doi.org/10.1136/practneurol-2015-001194
Mongin M, Mezouar N, Dodet P, Vidailhet M, Roze E (2016) Paroxysmal exercise-induced dyskinesias caused by GLUT1 deficiency syndrome. Tremor Other Hyperkinet Mov (N Y) 4(6):371. https://doi.org/10.7916/D89W0F96.PMID:27351150;PMCID:PMC4790204
Chenouard A, Vuillaumier-Barrot S, Seta N, Kuster A (2015) A cause of permanent ketosis: GLUT-1 deficiency. JIMD Rep. 18:79–83. https://doi.org/10.1007/8904_2014_352
Larsen J, Johannesen KM, Ek J, Tang S, Marini C, Blichfeldt S, Kibaek M, von Spiczak S, Weckhuysen S, Frangu M, Neubauer BA, Uldall P, Striano P, Zara F; MAE working group of EuroEPINOMICS RES Consortium; Kleiss R, Simpson M, Muhle H, Nikanorova M, Jepsen B, Tommerup N, Stephani U, Guerrini R, Duno M, Hjalgrim H, Pal D, Helbig I, Møller RS. The role of SLC2A1 mutations in myoclonic astatic epilepsy and absence epilepsy, and the estimated frequency of GLUT1 deficiency syndrome. Epilepsia. 2015 56(12):e203-8. https://doi.org/10.1111/epi.13222
Roubergue A, Apartis E, Mesnage V, Doummar D, Trocello JM, Roze E, Taieb G, De Villemeur TB, Vuillaumier-Barrot S, Vidailhet M, Levy R (2011) Dystonic tremor caused by mutation of the glucose transporter gene GLUT1. J Inherit Metab Dis. 34(2):483–8. https://doi.org/10.1007/s10545-010-9264-6
Lankford J, Butler IJ, Koenig MK (2012) Glucose transporter type I deficiency causing mitochondrial dysfunction. J Child Neurol. 27(6):796–8. https://doi.org/10.1177/0883073811426503
Leen WG, Wevers RA, Kamsteeg EJ, Scheffer H, Verbeek M, Willemsen MA (2013) Cerebrospinal fluid analysis in the workup of GLUT1 deficiency syndrome a systematic review. JAMA Neurol. 70(11):1440–1444. https://doi.org/10.1001/jamaneurol.2013.3090
Nabatame S, Tanigawa J, Tominaga K, Kagitani-Shimono K, Yanagihara K, Imai K, Ando T, Tsuyusaki Y, Araya N, Matsufuji M, Natsume J, Yuge K, Bratkovic D, Arai H, Okinaga T, Matsushige T, Azuma Y, Ishihara N, Miyatake S, Kato M, Matsumoto N, Okamoto N, Takahashi S, Hattori S, Ozono K (2023) Association between cerebrospinal fluid parameters and developmental and neurological status in glucose transporter 1 deficiency syndrome. J Neurol Sci 15(447):120597. https://doi.org/10.1016/j.jns.2023.120597
Yu WH, Chen LW, Wang ST, Tu YF, Huang CC (2019) Developmental outcomes and prevalence of SLC2A1 variants in young infants with hypoglycorrhachia. Brain Dev 41(10):854–861. https://doi.org/10.1016/j.braindev.2019.07.004
Leen WG, Willemsen MA, Wevers RA, Verbeek MM (2012) Cerebrospinal fluid glucose and lactate: age-specific reference values and implications for clinical practice. PLoS One 7:e42745
Timmers ER, Klamer MR, Marapin RS, Lammertsma AA, de Jong BM, Dierckx RAJO, Tijssen MAJ (2023) [18F] FDG PET in conditions associated with hyperkinetic movement disorders and ataxia: a systematic review. Eur J Nucl Med Mol Imaging. 50(7):1954–1973
Mortaji S, Dozières-Puyravel B, Geraldes K, Perrot C, Quéméner V, Auvin S (2023) Uncommon use of intermittent glucose administration for infrequent non-epileptic paroxysmal events in GLUT1-DS. Eur J Paediatr Neurol. 45:19–21
Wang X, Zhang Y, Li Y, Tang M, Deng Q, Mao J, Du L (2021) Estrogen regulates glucose metabolism in cattle neutrophils through autophagy. Front Vet Sci 29(8):773514
Delorme C, Giron C, Bendetowicz D, Méneret A, Mariani LL, Roze E (2021) Current challenges in the pathophysiology, diagnosis, and treatment of paroxysmal movement disorders. Expert Rev Neurother 21:81–97
Kumar A, Lyzhko E, Hamid L, Srivastav A, Stephani U, Japaridze N (2023) Neuronal networks underlying ictal and subclinical discharges in childhood absence epilepsy. J Neurol 270(3):1402–1415
** C, Gao L, Li Y, Wu S, Lu X, Yang J, Cai Y (2017) Lanthanum damages learning and memory and suppresses astrocyte-neuron lactate shuttle in rat hippocampus. Exp Brain Res 235(12):3817–3832
Galochkina T, Ng Fuk Chong M, Challali L, Abbar S, Etchebest C (2019) New insights into GluT1 mechanics during glucose transfer. Sci Rep 9(1):998
Holman GD (2020) Structure, function and regulation of mammalian glucose transporters of the SLC2 family. Pflugers Arch 472(9):1155–1175
Author information
Authors and Affiliations
Contributions
MM planned the review, analyzed the literature data, wrote the first draft, and revised the paper. FM and GR collected and interpreted the literature data and realized the statistical analysis. EMCC, NC, and AB collected the literature data. MT analyzed the genetic data. FP revised the paper.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Communicated by Gregorio Milani
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Mastrangelo, M., Manti, F., Ricciardi, G. et al. The diagnostic and prognostic role of cerebrospinal fluid biomarkers in glucose transporter 1 deficiency: a systematic review. Eur J Pediatr (2024). https://doi.org/10.1007/s00431-024-05657-6
Received:
Revised:
Accepted:
Published:
DOI: https://doi.org/10.1007/s00431-024-05657-6