Abstract
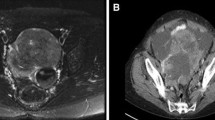
Cauda equina neuroendocrine tumors (CENETs) are neoplasms of uncertain histogenesis with overlap** features between those of paragangliomas (PGs) and visceral neuroendocrine tumors (NETs). We have explored their biological relationship to both subsets of neuroendocrine neoplasms. The clinical and radiological features of a cohort of 23 CENETs were analyzed. A total of 21 cases were included in tissue microarrays, along with a control group of 38 PGs and 83 NETs. An extensive panel of antibodies was used to assess epithelial phenotype (cytokeratins, E-cadherin, EpCAM, Claudin-4, EMA, CD138), neuronal and neuroendocrine features (synaptophysin, chromogranin A, INSM1, neurofilaments, NeuN, internexin-α, calretinin), chromaffin differentiation (GATA3, Phox2b, tyrosine hydroxylase), and possible histogenesis (Sox2, T-brachyury, Oct3/4, Sox10). The cohort included 5 women (22%) and 18 men (78%). The average age at the time of surgery was 48.3 years (range from 21 to 80 years). The average diameter of the tumors was 39.27 mm, and invasion of surrounding structures was observed in 6/21 (29%) tumors. Follow-up was available in 16 patients (median 46.5 months). One tumor recurred after 19 months. No metastatic behavior and no endocrine activity were observed. Compared to control groups, CENETs lacked expression of epithelial adhesion molecules (EpCAM, CD138, E-cadherin, Claudin-4), and at the same time, they lacked features of chromaffin differentiation (GATA3, Phox2b, tyrosine hydroxylase). We observed no loss of SDHB. Cytokeratin expression was present in all CENETs. All the CENETs showed variable cytoplasmic expression of T-brachyury and limited nuclear expression of Sox2. These findings support the unique nature of the neoplasm with respect to NETs and PGs.



Similar content being viewed by others
Data availability
The results of immunohistochemistry of individual tumors together with clinical data are available in the form of a supplementary table (Supplementary Table 2). The clinical, radiological, and pathological data of individual CENETs and the histology images (in the form of “*.svs” formatted image files) used and analysed during the current study are available from the corresponding author on reasonable request.
References
Moran CA, Rush W, Mena H (1997) Primary spinal paragangliomas: a clinicopathological and immunohistochemical study of 30 cases. Histopathology 31:167–173. https://doi.org/10.1046/j.1365-2559.1997.2300841.x
Ramani B, Gupta R, Wu J, Barreto J, Bollen AW, Tihan T, Mummaneni PV, Ames C, Clark A, Oberheim Bush NA, Butowski N, Phillips D, King BE, Bator SM, Treynor EC, Zherebitskiy V, Quinn PS, Walker JB, Pekmezci M et al (2020) The immunohistochemical, DNA methylation, and chromosomal copy number profile of cauda equina paraganglioma is distinct from extra-spinal paraganglioma. Acta Neuropathol 140:907–917. https://doi.org/10.1007/s00401-020-02221-y
Schweizer L, Thierfelder F, Thomas C, Soschinski P, Suwala A, Stichel D, Wefers AK, Wessels L, Misch M, Kim HY, Jodicke R, Teichmann D, Kaul D, Kahn J, Bockmayr M, Hasselblatt M, Younsi A, Unterberg A, Knie B et al (2020) Molecular characterization of CNS paragangliomas identifies cauda equina paragangliomas as a distinct tumor entity. Acta Neuropathol 140:893–906. https://doi.org/10.1007/s00401-020-02218-7
Miliaras GC, Kyritsis AP, Polyzoidis KS (2003) Cauda equina paraganglioma: a review. J Neuro-Oncol 65:177–190. https://doi.org/10.1023/b:neon.0000003753.27452.20
Fishbein L, Leshchiner I, Walter V, Danilova L, Robertson AG, Johnson AR, Lichtenberg TM, Murray BA, Ghayee HK, Else T, Ling S, Jefferys SR, de Cubas AA, Wenz B, Korpershoek E, Amelio AL, Makowski L, Rathmell WK, Gimenez-Roqueplo AP, Giordano TJ, Asa SL, Tischler AS, Cancer Genome Atlas Research N, Pacak K, Nathanson KL, Wilkerson MD (2017) Comprehensive molecular characterization of pheochromocytoma and paraganglioma. Cancer Cell 31:181-193. https://doi.org/10.1016/j.ccell.2017.01.001
Mamilla D, Manukyan I, Fetsch PA, Pacak K, Miettinen M (2020) Immunohistochemical distinction of paragangliomas from epithelial neuroendocrine tumors-gangliocytic duodenal and cauda equina paragangliomas align with epithelial neuroendocrine tumors. Hum Pathol 103:72–82. https://doi.org/10.1016/j.humpath.2020.07.010
Kimura N, Shiga K, Kaneko K, Sugisawa C, Katabami T, Naruse M (2020) The diagnostic dilemma of GATA3 immunohistochemistry in pheochromocytoma and paraganglioma. Endocr Pathol 31:95–100. https://doi.org/10.1007/s12022-020-09618-1
Miettinen M, McCue PA, Sarlomo-Rikala M, Rys J, Czapiewski P, Wazny K, Langfort R, Waloszczyk P, Biernat W, Lasota J, Wang Z (2014) GATA3: a multispecific but potentially useful marker in surgical pathology: a systematic analysis of 2500 epithelial and nonepithelial tumors. Am J Surg Pathol 38:13–22. https://doi.org/10.1097/PAS.0b013e3182a0218f
Mete O, Asa SL, Gill AJ, Kimura N, de Krijger RR, Tischler A (2022) Overview of the 2022 WHO Classification of Paragangliomas and Pheochromocytomas. Endocr Pathol 33:90–114. https://doi.org/10.1007/s12022-022-09704-6
Furlan A, Dyachuk V, Kastriti ME, Calvo-Enrique L, Abdo H, Hadjab S, Chontorotzea T, Akkuratova N, Usoskin D, Kamenev D, Petersen J, Sunadome K, Memic F, Marklund U, Fried K, Topilko P, Lallemend F, Kharchenko PV, Ernfors P, Adameyko I (2017) Multipotent peripheral glial cells generate neuroendocrine cells of the adrenal medulla. Science:357. https://doi.org/10.1126/science.aal3753
Simoes-Costa M, Bronner ME (2015) Establishing neural crest identity: a gene regulatory recipe. Development 142:242–257. https://doi.org/10.1242/dev.105445
Kloppel G (2017) Neuroendocrine neoplasms: dichotomy, origin and classifications. Visc Med 33:324–330. https://doi.org/10.1159/000481390
Wildner H, Gierl MS, Strehle M, Pla P, Birchmeier C (2008) Insm1 (IA-1) is a crucial component of the transcriptional network that controls differentiation of the sympatho-adrenal lineage. Development 135:473–481. https://doi.org/10.1242/dev.011783
Gehart H, van Es JH, Hamer K, Beumer J, Kretzschmar K, Dekkers JF, Rios A, Clevers H (2019) Identification of enteroendocrine regulators by real-time single-cell differentiation map** cell 176:1158-1173 e1116. https://doi.org/10.1016/j.cell.2018.12.029
Alexander RE, Cheng L, Grignon DJ, Idrees MT (2014) Cytoplasmic OCT4 staining is a sensitive marker of neuroendocrine differentiation. Hum Pathol 45:27–32. https://doi.org/10.1016/j.humpath.2013.08.006
Zhang PJ, Genega EM, Tomaszewski JE, Pasha TL, LiVolsi VA (2003) The role of calretinin, inhibin, melan-A, BCL-2, and C-kit in differentiating adrenal cortical and medullary tumors: an immunohistochemical study Mod Pathol 16:591-597. https://doi.org/10.1097/01.MP.0000073134.60541.E8
Yang J, Antin P, Berx G, Blanpain C, Brabletz T, Bronner M, Campbell K, Cano A, Casanova J, Christofori G, Dedhar S, Derynck R, Ford HL, Fuxe J, Garcia de Herreros A, Goodall GJ, Hadjantonakis AK, Huang RYJ, Kalcheim C, Kalluri R, Kang Y, Khew-Goodall Y, Levine H, Liu J, Longmore GD, Mani SA, Massague J, Mayor R, McClay D, Mostov KE, Newgreen DF, Nieto MA, Puisieux A, Runyan R, Savagner P, Stanger B, Stemmler MP, Takahashi Y, Takeichi M, Theveneau E, Thiery JP, Thompson EW, Weinberg RA, Williams ED, **ng J, Zhou BP, Sheng G, Association EMTI (2020) Guidelines and definitions for research on epithelial-mesenchymal transition Nat Rev Mol Cell Biol 21:341-8. https://doi.org/10.1038/s41580-020-0237-9
Asa SL, Mete O (2020) Cytokeratin profiles in pituitary neuroendocrine tumors hum pathol. https://doi.org/10.1016/j.humpath.2020.10.004
Chetty R, Asa SL (2004) Pancreatic endocrine tumour with cytoplasmic keratin whorls. Is the term “rhabdoid” appropriate? J Clin Pathol 57:1106–1110. https://doi.org/10.1136/jcp.2004.018309
Miyazaki T, Aishima S, Fu**o M, Ozono K, Kubo Y, Ushijima Y, Osoegawa T, Ihara E, Tetsuhide I, Ohtsuka T, Nakamura M, Oda Y (2018) Neuroendocrine tumor of the pancreas with rhabdoid feature. Virchows Arch 473:247–252. https://doi.org/10.1007/s00428-018-2398-x
Bardag-Gorce F, Riley N, Nguyen V, Montgomery RO, French BA, Li J, van Leeuwen FW, Lungo W, McPhaul LW, French SW (2003) The mechanism of cytokeratin aggresome formation: the role of mutant ubiquitin (UBB+1). Exp Mol Pathol 74:160–167. https://doi.org/10.1016/s0014-4800(02)00024-2
Gammill LS, Bronner-Fraser M (2002) Genomic analysis of neural crest induction Development 129:5731-5741. https://doi.org/10.1242/dev.00175
Lignell A, Kerosuo L, Streichan SJ, Cai L, Bronner ME (2017) Identification of a neural crest stem cell niche by Spatial Genomic Analysis. Nat Commun 8:1830. https://doi.org/10.1038/s41467-017-01561-w
Gown AM, Boyd HC, Chang Y, Ferguson M, Reichler B, Tippens D (1988) Smooth muscle cells can express cytokeratins of “simple” epithelium. Immunocytochemical and biochemical studies in vitro and in vivo. Am J Pathol 132:223–232
Iwatsuki H, Suda M (2010) Transient expression of keratin during neuronal development in the adult rabbit spinal ganglion. Anat Sci Int 85:46–55. https://doi.org/10.1007/s12565-009-0054-x
Tseng IC, Yeh MM, Yang CY, Jeng YM (2015) NKX6-1 Is a novel immunohistochemical marker for pancreatic and duodenal neuroendocrine tumors Am J Surg Pathol 39:850-857. https://doi.org/10.1097/PAS.0000000000000435
An Z, Liu P, Zheng J, Si C, Li T, Chen Y, Ma T, Zhang MQ, Zhou Q, Ding S (2019) Sox2 and Klf4 as the functional core in pluripotency induction without exogenous. Cell Rep 29:1986–2000 e1988. https://doi.org/10.1016/j.celrep.2019.10.026
Kimura N, Shiga K, Kaneko KI, Oki Y, Sugisawa C, Saito J, Tawara S, Akahori H, Sogabe S, Yamashita T, Takekoshi K, Naruse M, Katabami T (2021) Immunohistochemical expression of choline acetyltransferase and catecholamine-synthesizing enzymes in head-and-neck and thoracoabdominal paragangliomas and pheochromocytomas. Endocr Pathol 32:442–451. https://doi.org/10.1007/s12022-021-09694-x
Lee JP, Hung YP, O'Dorisio TM, Howe JR, Hornick JL, Bellizzi AM (2017) Examination of PHOX2B in adult neuroendocrine neoplasms reveals relatively frequent expression in phaeochromocytomas and paragangliomas Histopathology 71:503-510. https://doi.org/10.1111/his.13243
Barresi V, Ieni A, Branca G, Tuccari G (2014) Brachyury: a diagnostic marker for the differential diagnosis of chordoma and hemangioblastoma versus neoplastic histological mimickers. Dis Markers 2014:514753. https://doi.org/10.1155/2014/514753
Chen M, Wu Y, Zhang H, Li S, Zhou J, Shen J (2020) The roles of embryonic transcription factor BRACHYURY in tumorigenesis and progression Front. Oncol 10:961. https://doi.org/10.3389/fonc.2020.00961
Lee KH, Kim EY, Yun JS, Park YL, Do SI, Chae SW, Park CH (2018) Prognostic significance of expression of epithelial-mesenchymal transition driver brachyury in breast cancer and its association with subtype and characteristics. Oncol Lett 15:1037–1045. https://doi.org/10.3892/ol.2017.7402
Pinto F, Pertega-Gomes N, Pereira MS, Vizcaino JR, Monteiro P, Henrique RM, Baltazar F, Andrade RP, Reis RM (2014) T-box transcription factor brachyury is associated with prostate cancer progression and aggressiveness. Clin Cancer Res 20:4949–4961. https://doi.org/10.1158/1078-0432.CCR-14-0421
Bockmayr M, Korner M, Schweizer L, Schuller U (2021) Cauda equina paragangliomas express HOXB13. Neuropathol Appl Neurobiol 47:889–890. https://doi.org/10.1111/nan.12713
Zeltser L, Desplan C, Heintz N (1996) Hoxb-13: a new Hox gene in a distant region of the HOXB cluster maintains colinearity. Development 122:2475–2484. https://doi.org/10.1242/dev.122.8.2475
Rocha M, Beiriger A, Kushkowski EE, Miyashita T, Singh N, Venkataraman V, Prince VE (2020) From head to tail: regionalization of the neural crest. Development:147. https://doi.org/10.1242/dev.193888
Gouti M, Delile J, Stamataki D, Wymeersch FJ, Huang Y, Kleinjung J, Wilson V, Briscoe J (2017) A gene regulatory network balances neural and mesoderm specification during vertebrate trunk development Dev Cell 41:243-261 e247. https://doi.org/10.1016/j.devcel.2017.04.002
Koch F, Scholze M, Wittler L, Schifferl D, Sudheer S, Grote P, Timmermann B, Macura K, Herrmann BG (2017) Antagonistic activities of Sox2 and brachyury control the fate choice of neuro-mesodermal progenitors Dev. Cell 42:514–526 e517. https://doi.org/10.1016/j.devcel.2017.07.021
Acknowledgements
We would like to thank Prof. Pavel Dundr, M.D., Ph.D. for performing immunohistochemical detection of T-brachyury in his laboratory. The authors are grateful to Ian McColl, M.D., Ph.D. for assistance with the manuscript.
Funding
This study was supported by the Ministry of Health, Czech Republic, project No. NV19-01-00435, by the project BBMRI-CZ LM2018125 and the Cooperation Program, research area DIAG. The funding sources were not involved in the study design, collection, analysis, or interpretation of data; on the writing of the report; or on the decision to submit the article for publication.
Author information
Authors and Affiliations
Contributions
JS, FG, and TC conceived the study; JS, TC, TS, and BV designed the study, LM, MT, BR, and MW reviewed case files of their institutions, procured the cases and helped with study design; JS and AK performed morphological assessment; PK was responsible for implementation and performing of immunohistochemical procedures; JS and MM analyzed results of immunohistochemistry; RD reviewed radiological data; DN, SR, JK, PV, Miroslav Kaiser, and Martin Kanta supplied clinical, radiological and biochemical data of the patients, analyzed them and helped to interpret them; JD supplied clinical data for control groups; JS and FG performed data analysis. All the authors contributed in writing and reviewing the manuscript.
Corresponding author
Ethics declarations
Ethics approval
The study was conducted in accordance with the Declaration of Helsinki and with the approval of the ethical committee of University Hospital Hradec Kralove (reference no. 202101P06 and no. 202109P01)
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Supplementary Table 1
Antibodies and details of immunohistochemical reactions used in the study (DOCX 28 kb)
Supplementary Table 2
Immunohistochemistry results, clinical and morphological data (XLSX 42 kb)
Supplementary Table 3
Radiological characteristics of the cohort (DOCX 14 kb)

Supplementary Figure 1
Immunoreactivity of NKX6.1 and HoxB13 in CENETs (PNG 7531 kb)
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Soukup, J., Manethova, M., Kohout, A. et al. Cauda equina neuroendocrine tumors show biological features distinct from other paragangliomas and visceral neuroendocrine tumors. Virchows Arch 482, 325–338 (2023). https://doi.org/10.1007/s00428-022-03441-1
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00428-022-03441-1