Abstract
Purpose
The impact of perineal descent (PD) on functional outcome and quality of life after ventral mesh rectopexy (VMR) is unknown. The purpose of this study was to analyze the effect of PD on the functional outcome and quality of life (QOL) after VMR.
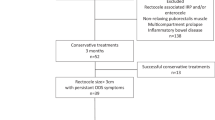
Methods
A retrospective analysis was performed on fifty-five patients who underwent robotic VMR between 2018 and 2021. Pre and postoperative data along with radiological studies were gathered from a prospectively maintained database. The Cleveland Clinic Constipation score (CCCS), the Rome IV criteria and the 36-Item Short-Form Health Survey (SF-36), were used to measure functional results and QOL.
Results
All 55 patients (mean age 57.8 years) were female. Most patients had radiological findings of severe PD (n = 31) as opposed to mild/moderate PD (n = 24). CCCS significantly improved at 3 months and 1 year post-VMR (mean difference = -4.4 and -5.4 respectively, p < 0.001) with no significant difference between the two groups. The percentage of functional constipation Rome IV criteria only showed an improved outcome at 3 months for severe PD and at 1 year for mild/moderate PD (difference = -58.1% and -54.2% respectively, p < 0.05). Only the SF-36 subscale bodily pain significantly improved in the mild/moderate PD group (mean difference = 16.7, p = 0.002) 3 months post-VMR which subsided after one year (mean difference = 5.5, p = 0.068).
Conclusion
Severe PD may impact the functional outcome of constipation without an evident effect on QOL after VMR. The results, however, remain inconclusive and further research is warranted.





Similar content being viewed by others
Data availability
All data is available upon request.
References
Makela-Kaikkonen J, Rautio T, Ohinmaa A, Koivurova S, Ohtonen P, Sintonen H, Makela J (2019) Cost-analysis and quality of life after laparoscopic and robotic ventral mesh rectopexy for posterior compartment prolapse: A randomized trial. Tech Coloproctol 23(5):461–470. https://doi.org/10.1007/s10151-019-01991-2
Samaranayake CB, Luo C, Plank AW, Merrie AE, Plank LD, Bissett IP (2010) Systematic review on ventral rectopexy for rectal prolapse and intussusception. Colorectal Dis 12(6):504–512. https://doi.org/10.1111/j.1463-1318.2009.01934.x
Emile SH, Elfeki HA, Youssef M, Farid M, Wexner SD (2017) Abdominal rectopexy for the treatment of internal rectal prolapse: A systematic review and meta-analysis. Colorectal Dis 19(1):O13–O24. https://doi.org/10.1111/codi.13574
D’Hoore A, Cadoni R, Penninckx F (2004) Long-term outcome of laparoscopic ventral rectopexy for total rectal prolapse. Br J Surg 91(11):1500–1505. https://doi.org/10.1002/bjs.4779
Mantoo S, Podevin J, Regenet N, Rigaud J, Lehur PA, Meurette G (2013) Is robotic-assisted ventral mesh rectopexy superior to laparoscopic ventral mesh rectopexy in the management of obstructed defaecation? Colorectal Dis 15(8):e469–e475. https://doi.org/10.1111/codi.12251
Laitakari KE, Makela-Kaikkonen JK, Kossi J, Kairaluoma M, Koivurova S, Pollari L, Ohtonen P, Rautio TT (2022) Mid-term functional and quality of life outcomes of robotic and laparoscopic ventral mesh rectopexy: Multicenter comparative matched-pair analyses. Tech Coloproctol 26(4):253–260. https://doi.org/10.1007/s10151-021-02563-z
Parks AG, Porter NH, Hardcastle J (1966) The syndrome of the descending perineum. Proc R Soc Med 59(6):477–482
Felt-Bersma RJ, Tiersma ES, Cuesta MA (2008) Rectal prolapse, rectal intussusception, rectocele, solitary rectal ulcer syndrome, and enterocele. Gastroenterol Clin North Am 37(3)645–68, ix. https://doi.org/10.1016/j.gtc.2008.06.001
Ellis CN, Essani R (2012) Treatment of obstructed defecation. Clin Colon Rectal Surg 25(1):24–33. https://doi.org/10.1055/s-0032-1301756
Khaikin M, Wexner SD (2006) Treatment strategies in obstructed defecation and fecal incontinence. World J Gastroenterol 12(20):3168–3173. https://doi.org/10.3748/wjg.v12.i20.3168
Schawkat K, Heinrich H, Parker HL, Barth BK, Mathew RP, Weishaupt D, Fox M, Reiner CS (2018) How to define pathologic pelvic floor descent in MR defecography during defecation? Abdom Radiol (NY) 43(12):3233–3240. https://doi.org/10.1007/s00261-018-1652-7
D’Hoore A (2017) Fine-tuning indications for laparoscopic ventral mesh rectopexy. Tech Coloproctol 21(8):593–594. https://doi.org/10.1007/s10151-017-1678-9
Makela-Kaikkonen JK, Rautio TT, Koivurova S, Paakko E, Ohtonen P, Biancari F, Makela JT (2016) Anatomical and functional changes to the pelvic floor after robotic versus laparoscopic ventral rectopexy: A randomised study. Int Urogynecol J 27(12):1837–1845. https://doi.org/10.1007/s00192-016-3048-y
Gurland BH, Khatri G, Ram R, Hull TL, Kocjancic E, Quiroz LH, Sayed RFE, Jambhekar KR, Chernyak V, Paspulati RM, Sheth VR, Steiner AM, Kamath A, Shobeiri SA, Weinstein MM, Bordeianou L, D. Members of the Expert Workgroup on Magnetic Resonance Imaging of Pelvic Floor (2021) Consensus definitions and interpretation templates for magnetic resonance imaging of defecatory pelvic floor disorders: Proceedings of the consensus meeting of the pelvic floor disorders consortium of the american society of colon and rectal surgeons, the society of abdominal radiology, the international continence society, the american urogynecologic society, the international urogynecological association, and the society of gynecologic surgeons. AJR Am J Roentgenol 217(4):800–812. https://doi.org/10.2214/AJR.21.26488
Boyadzhyan L, Raman SS, Raz S (2008) Role of static and dynamic MR imaging in surgical pelvic floor dysfunction. Radiographics 28(4):949–967. https://doi.org/10.1148/rg.284075139
Agachan F, Chen T, Pfeifer J, Reissman P, Wexner SD (1996) A constipation scoring system to simplify evaluation and management of constipated patients. Dis Colon Rectum 39(6):681–685. https://doi.org/10.1007/BF02056950
Schmulson MJ, Drossman DA (2017) What is new in Rome IV. J Neurogastroenterol Motil 23(2):151–163. https://doi.org/10.5056/jnm16214
Ware JE Jr, Sherbourne CD (1992) The MOS 36-item short-form health survey (SF-36). I. Conceptual framework and item selection. Med Care 30(6):473–83
Koo TK, Li MY (2016) A guideline of selecting and reporting intraclass correlation coefficients for reliability research. J Chiropr Med 15(2):155–163. https://doi.org/10.1016/j.jcm.2016.02.012
Van den Broeck S, Jacquemyn Y, Hubens G, De Schepper H, Vermandel A, Komen N (2022) Rectocele: victim of availability bias? Results of a Belgian survey of colorectal and gynecological surgeons. Int Urogynecol J 33(12):3505–3517. https://doi.org/10.1007/s00192-022-05118-4
Aziz I, Whitehead WE, Palsson OS, Tornblom H, Simren M (2020) An approach to the diagnosis and management of Rome IV functional disorders of chronic constipation. Expert Rev Gastroenterol Hepatol 14(1):39–46. https://doi.org/10.1080/17474124.2020.1708718
Tsunoda A, Takahashi T, Matsuda S, Oka N, Kusanagi H (2020) Midterm functional outcome after laparoscopic ventral rectopexy for external rectal prolapse. Asian J Endosc Surg 13(1):25–32. https://doi.org/10.1111/ases.12701
Brunner M, Roth H, Gunther K, Grutzmann R, Matzel KE (2018) Ventral rectopexy with biological mesh: short-term functional results. Int J Colorectal Dis 33(4):449–457. https://doi.org/10.1007/s00384-018-2972-3
Abdelnaby M, Fathy M, Abdallah E, Balata M, Arnous M, Mikhail HM, Emile SH (2021) Laparoscopic ventral mesh rectopexy versus transvaginal posterior colporrhaphy in Management of Anterior Rectocele. J Gastrointest Surg 25(8):2035–2046. https://doi.org/10.1007/s11605-020-04823-z
Naldini G, Fabiani B, Sturiale A, Russo E, Simoncini T (2021) Advantages of robotic surgery in the treatment of complex pelvic organs prolapse. Updates Surg 73(3):1115–1124. https://doi.org/10.1007/s13304-020-00913-4
Tsunoda A, Takahashi T, Ohta T, Kusanagi H (2016) Quality of life after laparoscopic ventral rectopexy. Color Dis 18(8):O301–O310. https://doi.org/10.1111/codi.13247
Barber MD, Walters MD, Bump RC (2005) Short forms of two condition-specific quality-of-life questionnaires for women with pelvic floor disorders (PFDI-20 and PFIQ-7). Am J Obstet Gynecol 193(1):103–113. https://doi.org/10.1016/j.ajog.2004.12.025
Rogers RG, Coates KW, Kammerer-Doak D, Khalsa S, Qualls C (2003) A short form of the Pelvic Organ Prolapse/Urinary Incontinence Sexual Questionnaire (PISQ-12). Int Urogynecol J Pelvic Floor Dysfunct 14(3):164–8; discussion 168. https://doi.org/10.1007/s00192-003-1063-2
Mehmood RK, Parker J, Bhuvimanian L, Qasem E, Mohammed AA, Zeeshan M, Grugel K, Carter P, Ahmed S (2014) Short-term outcome of laparoscopic versus robotic ventral mesh rectopexy for full-thickness rectal prolapse. Is robotic superior? Int J Color Dis 29(9):1113–8. https://doi.org/10.1007/s00384-014-1937-4
Picchia S, Rengo M, Bellini D, Caruso D, Pironti E, Floris R, Laghi A (2019) Dynamic MR of the pelvic floor: Influence of alternative methods to draw the pubococcygeal line (PCL) on the grading of pelvic floor descent. Eur J Radiol Open 6:187–191. https://doi.org/10.1016/j.ejro.2019.05.002
Landmann RG, Wexner SD (2008) Paradoxical puborectalis contraction and increased perineal descent. Clin Colon Rectal Surg 21(2):138–145. https://doi.org/10.1055/s-2008-1075863
Korula DR, Chandramohan A, John R, Eapen A (2021) Barium defecating proctography and dynamic magnetic resonance proctography: their role and patient’s perception. J Clin Imaging Sci 11:31. https://doi.org/10.25259/JCIS_56_2021
Funding
No funding was obtained for this study.
Author information
Authors and Affiliations
Contributions
Sylvie Van den Broeck and Niels Komen conceived, planned, and supervised the research. Ali Al-Nejar, Sylvie Van den Broeck, Niels Komen, and Quinten Smets established and contributed to the database. Ali Al-Nejar, Sylvie Van den Broeck and Maarten Spinhoven performed the measurements of the radiographic images. Ali Al-Nejar and Sylvie Van den Broeck performed the analysis of the measurements. Ali Al-Nejar, Sylvie Van den Broeck, Niels Komen, Philip Plaeke and Guy Hubens contributed to the analysis and interpretation of the results. Ali Al-Nejar drafted the manuscript and designed the figures and tables. All authors provided critical feedback and helped shape the research, analysis and manuscript.
Corresponding author
Ethics declarations
Ethics approval
Approval was obtained from the ethics committee of University Hospital of Antwerp. The procedures used in this study adhere to the tenets of the Declaration of Helsinki.
Consent to participate
Informed consent was obtained from all individual participants included in the study.
Competing interests
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Al-Nejar, A., Van den Broeck, S., Smets, Q. et al. Ventral mesh rectopexy. Does a descending perineum impact functional results and quality of life?. Langenbecks Arch Surg 409, 44 (2024). https://doi.org/10.1007/s00423-024-03236-9
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s00423-024-03236-9