Abstract
Purpose
Fluorescence-based imaging has found application in several fields of elective surgery, but there is still a lack of evidence in the literature about its use in emergency setting. The present review critically summarizes currently available applications and limitations of indocyanine green (ICG) fluorescence in abdominal emergencies including acute cholecystitis, mesenteric ischemia, and trauma surgery.
Methods
A systematic review was performed according to the PRISMA statement identifying articles about the use of ICG fluorescence in the management of the most common general surgery emergency. Only studies focusing on the use of ICG fluorescence for the management of acute surgical conditions in adults were included.
Results
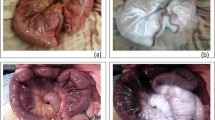
Thirty-six articles were considered for qualitative analysis. The most frequent disease was occlusive or non-occlusive mesenteric ischemia followed by acute cholecystitis. Benefits from using ICG for acute cholecystitis were reported in 48% of cases (clear identification of biliary structures and a safer surgical procedure). In one hundred and twenty cases that concerned the use of ICG for occlusive or non-occlusive mesenteric ischemia, ICG injection led to a modification of the surgical decision in 44 patients (36.6%). Three studies evaluated the use of ICG in trauma patients to assess the viability of bowel or parenchymatous organs in abdominal trauma, to evaluate the perfusion-related tissue impairment in extremity or craniofacial trauma, and to reassess the efficacy of surgical procedures performed in terms of vascularization. ICG injection led to a modification of the surgical decision in 50 patients (23.9%).
Conclusion
ICG fluorescence is a safe and feasible tool also in an emergency setting. There is increasing evidence that the use of ICG fluorescence during abdominal surgery could facilitate intra-operative decision-making and improve patient outcomes, even in the field of emergency surgery.



Similar content being viewed by others
Data availability
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
References
Kitai T, Inomoto T, Miwa M, Shikayama T (2005) Fluorescence navigation with indocyanine green for detecting sentinel lymph nodes in breast cancer. Breast Cancer 12(3):211–215. https://doi.org/10.2325/jbcs.12.211
Ris F, Hompes R, Cunningham C, Lindsey I, Guy R, Jones O, George B, Cahill RA, Mortensen NJ (2014) Near-infrared (NIR) perfusion angiography in minimally invasive colorectal surgery. Surg Endosc 28(7):2221–2226. https://doi.org/10.1007/s00464-014-3432-y
Alander JT, Kaartinen I, Laakso A, Patila T, Spillmann T, Tuchin VV, Venermo M, Valisuo P (2012) A review of indocyanine green fluorescent imaging in surgery. Int J Biomed Imaging. https://doi.org/10.1155/2012/940585
Liberati A, Altman DG, Tetzlaff J, Mulrow C, Gotzsche PC, Ioannidis JP, Clarke M, Devereaux PJ, Kleijnen J, Moher D (2009) The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: explanation and elaboration. J Clin Epidemiol 62(10):e1-34. https://doi.org/10.1016/j.jclinepi.2009.06.006
Moher D, Liberati A, Tetzlaff J, Altman DG, Group P (2009) Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med 6(7):e1000097. https://doi.org/10.1371/journal.pmed.1000097
Wells GA, Shea B, O’Connell D, Peterson J, Welch V, Losos M et al The Newcastle-Ottawa Scale (NOS) for assessing the quality if nonrandomized studies in meta-analyses. Available from: http://www.ohri.ca/programs/clinical_epidemiology/oxford.htm. Accessed 19 Oct 2009
Lockwood C, Porritt K, Munn Z, Rittenmeyer L, Salmond S, Bjerrum M et al (2017) Chapter 2: systematic reviews of qualitative evidence. In: Aromataris E, Munn Z (eds) JBI reviewer's manual. Adelaide, SA, JBI
Clavien PA, Barkun J, de Oliveira ML, Vauthey JN, Dindo D, Schulick RD, de Santibanes E, Pekolj J, Slankamenac K, Bassi C, Graf R, Vonlanthen R, Padbury R, Cameron JL, Makuuchi M (2009) The Clavien-Dindo classification of surgical complications: five-year experience. Ann Surg 250(2):187–196. https://doi.org/10.1097/SLA.0b013e3181b13ca2
Hozo SP, Djulbegovic B, Hozo I (2005) Estimating the mean and variance from the median, range, and the size of a sample. BMC Med Res Methodol 5:13. https://doi.org/10.1186/1471-2288-5-13
Di Maggio F, Hossain N, De Zanna A, Husain D, Bonomo L (2020) Near-infrared fluorescence cholangiography can be a useful adjunct during emergency cholecystectomies. Surg Innov 1553350620958562 10.1177/1553350620958562
Nitta T, Kataoka J, Ohta M, Ueda Y, Senpuku S, Kurashima Y, Shimizu T, Ishibashi T (2020) Laparoscopic cholecystectomy for cholecystitis using direct gallbladder indocyanine green injection fluorescence cholangiography: a case report. Ann Med Surg (Lond) 57:218–222. https://doi.org/10.1016/j.amsu.2020.07.057
Paludis H, Saukane E, Bobrovs E, Pupelis G (2020) Identification of biliovascular anatomy using indocyanine green fluorescent cholangiography in patients with acute cholecystitis. First experience in single institution. HPB (Oxford) 22:S278. https://doi.org/10.1016/j.hpb.2020.04.194
She WH, Cheung TT, Chan MY, Chu KW, Ma KW, Tsang SHY, Dai WC, Chan ACY, Lo CM (2022) Routine use of ICG to enhance operative safety in emergency laparoscopic cholecystectomy: a randomized controlled trial. Surg Endosc 36(6):4442–4451. https://doi.org/10.1007/s00464-021-08795-2
Tsutsui N, Yoshida M, Ito E, Ohdaira H, Kitajima M, Suzuki Y (2018) Laparoscopic cholecystectomy using the PINPOINT((R)) Endoscopic fluorescence imaging system with intraoperative fluorescent imaging for acute cholecystitis: a case report. Ann Med Surg (Lond) 35:146–148. https://doi.org/10.1016/j.amsu.2018.09.019
Alemanno G, Somigli R, Prosperi P, Bergamini C, Maltinti G, Giordano A, Valeri A (2016) Combination of diagnostic laparoscopy and intraoperative indocyanine green fluorescence angiography for the early detection of intestinal ischemia not detectable at CT scan. Int J Surg Case Rep 26:77–80. https://doi.org/10.1016/j.ijscr.2016.07.016
Daskalopoulou D, Kankam J, Plambeck J, Ambe PC, Zarras K (2018) Intraoperative real-time fluorescence angiography with indocyanine green for evaluation of intestinal viability during surgery for an incarcerated obturator hernia: a case report. Patient Saf Surg 12:24. https://doi.org/10.1186/s13037-018-0173-1
Ganguly A, Acharya A, Pai MV, Augustine AJ (2021) Assessment of bowel vascularity using indocyanine green fluorescence in incarcerated hernia. International Surgery Journal 8(9):2834. https://doi.org/10.18203/2349-2902.isj20213630
Irie T, Matsutani T, Hagiwara N, Nomura T, Fujita I, Kanazawa Y, Kakinuma D, Uchida E (2017) Successful treatment of non-occlusive mesenteric ischemia with indocyanine green fluorescence and open-abdomen management. Clin J Gastroenterol 10(6):514–518. https://doi.org/10.1007/s12328-017-0779-3
Ishizuka M, Nagata H, Takagi K, Iwasaki Y, Yamagishi H, Tanaka G, Kubota K (2015) Usefulness of intraoperative observation using a fluorescence imaging instrument for patients with nonocclusive mesenteric ischemia. Int Surg 100(4):593–599. https://doi.org/10.9738/INTSURG-D-14-00038.1
Karampinis I, Keese M, Jakob J, Stasiunaitis V, Gerken A, Attenberger U, Post S, Kienle P, Nowak K (2018) Indocyanine green tissue angiography can reduce extended bowel resections in acute mesenteric ischemia. J Gastrointest Surg 22(12):2117–2124. https://doi.org/10.1007/s11605-018-3855-1
Alexander K, Ismail M, Alexander M (2019) Use of ICG imaging to confirm bowel viability after upper mesenteric stenting in patient with acute mesenteric ischemia: case report. Int J Surg Case Rep 61:322–326. https://doi.org/10.1016/j.ijscr.2019.07.077
Mehdorn M, Ebel S, Kohler H, Gockel I, Jansen-Winkeln B (2021) Hyperspectral imaging and indocyanine green fluorescence angiography in acute mesenteric ischemia: a case report on how to visualize intestinal perfusion. Int J Surg Case Rep 82:105853. https://doi.org/10.1016/j.ijscr.2021.105853
Nakagawa Y, Kobayashi K, Kuwabara S, Shibuya H, Nishimaki T (2018) Use of indocyanine green fluorescence imaging to determine the area of bowel resection in non-occlusive mesenteric ischemia: a case report. Int J Surg Case Rep 51:352–357. https://doi.org/10.1016/j.ijscr.2018.09.024
Nakamoto H, Yokota R, Namba H, Yamada K, Hosoda M, Taguchi K (2021) Effectiveness of intraoperative indocyanine green fluorescence-navigated surgery for superior mesenteric vein thrombosis that developed during treatment for intravascular lymphoma: a case report. Am J Case Rep 22:e929549. https://doi.org/10.12659/AJCR.929549
Nitori N, Deguchi T, Kubota K, Yoshida M, Kato A, Kojima M, Kadomura T, Okada A, Okamura J, Kobayashi M, Sato T, Beck Y, Kitagawa Y, Kitajima M (2014) Successful treatment of non-occlusive mesenteric ischemia (NOMI) using the HyperEye Medical System for intraoperative visualization of the mesenteric and bowel circulation: report of a case. Surg Today 44(2):359–362. https://doi.org/10.1007/s00595-013-0503-y
Nowak K, Sandra-Petrescu F, Post S, Horisberger K (2015) Ischemic and injured bowel evaluation by fluorescence imaging. Colorectal Dis 17(Suppl 3):12–15. https://doi.org/10.1111/codi.13032
Ryu S, Yoshida M, Ohdaira H, Tsutsui N, Suzuki N, Ito E, Nakajima K, Yanagisawa S, Kitajima M, Suzuki Y (2016) A case of incarcerated femoral hernia with intestinal blood flow assessment by brightfield full-color near-infrared fluorescence camera: report of a case. Int J Surg Case Rep 29:234–236. https://doi.org/10.1016/j.ijscr.2016.11.041
Ryu S, Yoshida M, Ohdaira H, Tsutsui N, Suzuki N, Ito E, Nakajima K, Yanagisawa S, Kitajima M, Suzuki Y (2017) Blood flow evaluation using PINPOINT(R) in a case of incarcerated inguinal hernia: a case report. Asian J Endosc Surg 10(1):75–78. https://doi.org/10.1111/ases.12333
Ryu S, Yoshida M, Ohdaira H, Tsutsui N, Suzuki N, Ito E, Nakajima K, Yanagisawa S, Kitajima M, Suzuki Y (2016) Intestinal blood flow assessment by indocyanine green fluorescence imaging in a patient with the incarcerated umbilical hernia: report of a case. Ann Med Surg (Lond) 8:40–42. https://doi.org/10.1016/j.amsu.2016.04.020
Szoka N, Kahn M (2022) Acute-on-chronic mesenteric ischemia: the use of fluorescence guidance to diagnose a nonsurvivable injury. Case Rep Surg 2022:5459774. https://doi.org/10.1155/2022/5459774
Takeda M, Hiramatsu Y, Unnno N, Takahashi Y, Kikuchi H, Yamamoto N, Ohta M, Kamiya K, Sakaguchi T, Baba S, Konno H (2016) Intraoperative indocyanine green fluorescence angiography for diagnosis of nonocclusive mesenteric ischemia: a case report. International Surgery Journal 101:524–529. https://doi.org/10.9738/INTSURG-D-15-00039.1
Imai T, Tanaka Y, Sato Y, Mase J, Suetsugu T, Fukada M, Yasufuku I, Iwata Y, Imai H, Okumura N, Matsuhashi N, Takahashi T, Yoshida K (2021) Successful treatment of superior mesenteric artery thrombosis via preoperative interventional radiology and surgery using indocyanine green fluorescence. Clin J Gastroenterol 14(3):769–775. https://doi.org/10.1007/s12328-021-01368-9
Joosten JJ, Longchamp G, Khan MF, Lameris W, van Berge Henegouwen MI, Bemelman WA, Cahill RA, Hompes R, Ris F (2022) The use of fluorescence angiography to assess bowel viability in the acute setting: an international, multi-centre case series. Surg Endosc 36(10):7369–7375. https://doi.org/10.1007/s00464-022-09136-7
Liot E, Assalino M, Buchs NC, Schiltz B, Douissard J, Morel P, Ris F (2018) Does near-infrared (NIR) fluorescence angiography modify operative strategy during emergency procedures? Surg Endosc 32(10):4351–4356. https://doi.org/10.1007/s00464-018-6226-9
Sakata K, Kijima D, Furuhashi T, Morita K, Abe T (2018) A case report: Feasibility of a near infrared ray vision system (Photo dynamic eye®) for the postoperative ischemic complication of gallbladder carcinoma. Int J Surg Case Rep 53:312–315. https://doi.org/10.1016/j.ijscr.2018.11.007
Copaescu C, Birlog C, Turcu F, Saftoiu A (2021) A novel indocyanine green fluorescence-guided laparoscopic technique to map the site of obscure gastrointestinal haemorrhage. Chirurgia (Bucur) 16(1); 89–101 https://doi.org/10.21614/chirurgia.116.1.89
Kawachi J, Ogino H, Shimoyama R, Ichita C, Isogai N, Murata T, Miyake K, Nishida T, Fukai R, Kashiwagi H (2020) Intraoperative angiography with indocyanine green injection for precise localization and resection of small bowel bleeding. Acute Med Surg 7(1):e549. https://doi.org/10.1002/ams2.549
Ono H, Kusano M, Kawamata F, Danjo Y, Kawakami M, Nagashima K, Nishihara H (2016) Intraoperative localization of arteriovenous malformation of a jejunum with combined use of angiographic methods and indocyanine green injection: report of a new technique. Int J Surg Case Rep 29:137–140. https://doi.org/10.1016/j.ijscr.2016.10.030
Afifi I, Abdelrahman H, El-Faramawy A et al (2021) The use of Indocyanine green fluorescent in patients with abdominal trauma for better intraoperative decision-making and less bowel anastomosis leak: case series. J Surg Case Rep 2021(6):rjab235. https://doi.org/10.1093/jscr/rjab235
Green JM 3rd, Sabino J, Fleming M, Valerio I (2015) Intraoperative fluorescence angiography: a review of applications and outcomes in war-related trauma. Mil Med 180(3 Suppl):37–43. https://doi.org/10.7205/MILMED-D-14-00632
Keller DS, Boulton R, Rodriguez-Justo M, Cohen R, Chand M (2018) A novel application of indocyanine green immunofluorescence in emergent colorectal surgery. J Fluoresc 28(2):487–490. https://doi.org/10.1007/s10895-018-2230-7
Osterkamp JTF, Patel MQ, Steyn E, Svendsen L-B, Forgan T, Achiam MP (2021) Usability of fluorescence angiography with indocyanine green in the surgical management of penetrating abdominal trauma: a case series. International Journal of Surgery Open 30:100319. https://doi.org/10.1016/j.ijso.2021.02.001
Guerra F, Coletta D, Greco PA, Eugeni E, Patriti A (2021) The use of indocyanine green fluorescence to define bowel microcirculation during laparoscopic surgery for acute small bowel obstruction. Colorectal Dis 23(8):2189–2194. https://doi.org/10.1111/codi.15680
Nakashima K, Ryu S, Okamoto A, Hara K, Ishida K, Ito R, Nakabayashi Y (2022) Usefulness of blood flow evaluation with indocyanine green fluorescence imaging during laparoscopic surgery for strangulated bowel obstruction: a cohort study. Asian J Surg 45(3):867–873. https://doi.org/10.1016/j.asjsur.2021.08.020
Ryu S, Hara K, Goto K, Okamoto A, Kitagawa T, Marukuchi R, Ito R, Nakabayashi Y (2022) Fluorescence angiography vs. direct palpation for bowel viability evaluation with strangulated bowel obstruction. Langenbecks Arch Surg 407(2); 797–803 https://doi.org/10.1007/s00423-021-02358-8
Lütken CD, Achiam MP, Osterkamp J, Svendsen MB, Nerup N (2021) Quantification of fluorescence angiography: toward a reliable intraoperative assessment of tissue perfusion - a narrative review. Langenbecks Arch Surg 406(2):251–259. https://doi.org/10.1007/s00423-020-01966-0
Wada T, Kawada K, Takahashi R, Yoshitomi M, Hida K, Hasegawa S, Sakai Y (2017) ICG fluorescence imaging for quantitative evaluation of colonic perfusion in laparoscopic colorectal surgery. Surg Endosc 31(10):4184–4193. https://doi.org/10.1007/s00464-017-5475-3
Son GM, Kwon MS, Kim Y, Kim J, Kim SH, Lee JW (2019) Quantitative analysis of colon perfusion pattern using indocyanine green (ICG) angiography in laparoscopic colorectal surgery. Surg Endosc 33(5):1640–1649. https://doi.org/10.1007/s00464-018-6439-y
Trastulli S, Munzi G, Desiderio J, Cirocchi R, Rossi M, Parisi A (2021) Indocyanine green fluorescence angiography versus standard intraoperative methods for prevention of anastomotic leak in colorectal surgery: meta-analysis. Br J Surg 108(4):359–372. https://doi.org/10.1093/bjs/znaa139
Serban D, Badiu DC, Davitoiu D et al (2022) Systematic review of the role of indocyanine green near-infrared fluorescence in safe laparoscopic cholecystectomy (Review). Exp Ther Med 23(2):187. https://doi.org/10.3892/etm.2021.11110
Flum DR, Dellinger EP, Cheadle A, Chan L, Koepsell T (2003) Intraoperative cholangiography and risk of common bile duct injury during cholecystectomy. JAMA 289(13):1639–1644. https://doi.org/10.1001/jama.289.13.1639
Strasberg SM (2005) Biliary injury in laparoscopic surgery: part 2. Changing the culture of cholecystectomy. J Am Coll Surg 201(4); 604–611 https://doi.org/10.1016/j.jamcollsurg.2005.04.032
Buchs NC, Pugin F, Azagury DE, Jung M, Volonte F, Hagen ME, Morel P (2013) Real-time near-infrared fluorescent cholangiography could shorten operative time during robotic single-site cholecystectomy. Surg Endosc 27(10):3897–3901. https://doi.org/10.1007/s00464-013-3005-5
Sherwinter DA (2012) Identification of anomolous biliary anatomy using near-infrared cholangiography. J Gastrointest Surg 16(9):1814–1815. https://doi.org/10.1007/s11605-012-1945-z
van Dam DA, Ankersmit M, van de Ven P, van Rijswijk AS, Tuynman JB, Meijerink WJ (2015) Comparing near-infrared imaging with indocyanine green to conventional imaging during laparoscopic cholecystectomy: a prospective crossover study. J Laparoendosc Adv Surg Tech A 25(6):486–492. https://doi.org/10.1089/lap.2014.0248
Ishizawa T, Tamura S, Masuda K, Aoki T, Hasegawa K, Imamura H, Beck Y, Kokudo N (2009) Intraoperative fluorescent cholangiography using indocyanine green: a biliary road map for safe surgery. J Am Coll Surg 208(1):e1-4. https://doi.org/10.1016/j.jamcollsurg.2008.09.024
Pesce A, Piccolo G, La Greca G, Puleo S (2015) Utility of fluorescent cholangiography during laparoscopic cholecystectomy: a systematic review. World J Gastroenterol 21(25):7877–7883. https://doi.org/10.3748/wjg.v21.i25.7877
Osayi SN, Wendling MR, Drosdeck JM et al (2015) Near-infrared fluorescent cholangiography facilitates identification of biliary anatomy during laparoscopic cholecystectomy. Surg Endosc 29(2):368–375. https://doi.org/10.1007/s00464-014-3677-5
Turcotte J, Leydorf SD, Ali M, Feather C, Klune JR (2021) Indocyanine green does not decrease the need for bail-out operation in an acute care surgery population. Surgery 169(2):227–231. https://doi.org/10.1016/j.surg.2020.05.045
Zhang XD, Li T, ** L et al (2022) Zhonghua Yi Xue Za Zhi 102(20):1518–1522. https://doi.org/10.3760/cma.j.cn112137-20211210-02757
Garoufalia Z, Wexner SD (2023) Indocyanine green fluorescence guided surgery in colorectal surgery. J Clin Med 12(2):494. https://doi.org/10.3390/jcm12020494
Ellis CT, Maykel JA (2021) Defining anastomotic leak and the clinical relevance of leaks. Clin Colon Rectal Surg 34:359–365. https://doi.org/10.1055/s-0041-1735265
Lütken CD, Achiam MP, Svendsen MB et al (2020) Optimizing quantitative fluorescence angiography for visceral perfusion assessment. Surg Endosc 34:5223–5233. https://doi.org/10.1007/s00464-020-07821-z
Lütken CD, Achiam MP, Osterkamp J et al (2021) Quantification of fluorescence angiography: toward a reliable intraoperative assessment of tissue perfusion - a narrative review. Langenbecks Arch Surg 406(251):259. https://doi.org/10.1007/s00423-020-01966-0
Author information
Authors and Affiliations
Contributions
Fransvea P. Study conception and design, literature search, acquisition, interpretation and analysis of data, drafting and critically revising the article for important intellectual content and final approval of the version to be published. Fico V. literature search, acquisition, interpretation and analysis of data. D’Agostino L. Literature search, acquisition, interpretation and analysis of data. Costa G. Literature search, acquisition, interpretation and analysis of data. Puccioni C. Literature search, acquisition, interpretation and analysis of data. Biondi A. Literature search, acquisition, interpretation and analysis of data. BG.,GS. Drafting and critically revising the article for important intellectual content and final approval of the version to be published. Sganga G Drafting and critically revising the article for important intellectual content and final approval of the version to be published.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Declarations
Ethics approval and consent to participate.
Not applicable.
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Fransvea, P., Fico, V., Puccioni, C. et al. Application of fluorescence-guided surgery in the acute care setting: a systematic literature review. Langenbecks Arch Surg 408, 375 (2023). https://doi.org/10.1007/s00423-023-03109-7
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s00423-023-03109-7