Abstract
Purpose
Outline learning phases of robot-assisted laparoscopic surgery for rectal cancer and compare surgical and clinical outcomes between each phase of robot-assisted laparoscopic surgery and the mastery phase of conventional laparoscopic surgery.
Methods
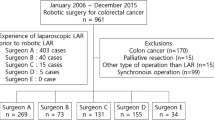
From 2015 to 2020, 210 patients underwent rectal cancer surgery at Sendai Medical Center. We performed conventional laparoscopic surgery in 110 patients and, laparoscopic surgery in 100 patients. The learning curve was evaluated using the cumulative summation method, risk-adjusted cumulative summation method, and logistic regression analysis.
Results
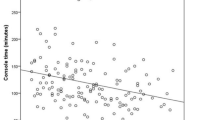
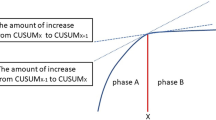
The risk-adjusted cumulative summation learning curve was divided into three phases: phase 1 (cases 1–48), phase 2 (cases 49–80), and phase 3 (cases 81–100). Duration of hospital stay (13.1 days vs. 18.0 days, respectively; p = 0.016) and surgery (209.1 min vs. 249.5 min, respectively; p = 0.045) were significantly shorter in phase 3 of the robot-assisted laparoscopic surgery group than in the conventional laparoscopic surgery group. Blood loss volume was significantly lower in phase 1 of the robot-assisted laparoscopic surgery group than in the conventional laparoscopic surgery group (17.7 ml vs. 79.7 ml, respectively; p = 0.036). The International Prostate Symptom Score was significantly lower in the robot-assisted laparoscopic surgery group (p = 0.0131).
Conclusions
Robot-assisted laparoscopic surgery for rectal cancer was safe and demonstrated better surgical and clinical outcomes, including a shorter hospital stay, less blood loss, and a shorter surgical duration, than conventional laparoscopic surgery. After experience with at least 80 cases, tactile familiarity can be acquired from visual information only (visual haptic feedback).
Clinical trial registration
UMIN reference no. UMIN000019857.


Similar content being viewed by others
Data availability
Data can be made available on request.
References
Heald RJ, Moran BJ, Ryall RD, Sexton R, MacFarlane JK (1998) Rectal cancer: the Basingstoke experience of total mesorectal excision, 1978–1997. Arch Surg 133(8):894–899
Fleshman J, Branda M, Sargent DJ, Boller AM, George V, Abbas M, Peters WR Jr, Maun D, Chang G, Herline A et al (2015) Effect of laparoscopic-assisted resection vs open resection of stage ii or iii rectal cancer on pathologic outcomes: the ACOSOG Z6051 randomized clinical trial. JAMA 314(13):1346–1355
Stevenson AR, Solomon MJ, Lumley JW, Hewett P, Clouston AD, Gebski VJ, Davies L, Wilson K, Hague W, Simes J et al (2015) Effect of laparoscopic-assisted resection vs open resection on pathological outcomes in rectal cancer: the ALaCaRT Randomized clinical trial. JAMA 314(13):1356–1363
van der Pas MH, Haglind E, Cuesta MA, Furst A, Lacy AM, Hop WC, Bonjer HJ, Group COcLoORIS (2013) Laparoscopic versus open surgery for rectal cancer (COLOR II): short-term outcomes of a randomised, phase 3 trial. Lancet Oncol 14(3):210–218
Kim NK, Kang J (2010) Optimal total mesorectal excision for rectal cancer: the role of robotic surgery from an expert’s view. J Korean Soc Coloproctol 26(6):377–387
Yamaguchi T, Kinugasa Y, Shiomi A, Tomioka H, Kagawa H, Yamakawa Y (2016) Robotic-assisted vs. conventional laparoscopic surgery for rectal cancer: short-term outcomes at a single center. Surg Today 46(8):957–962
Luca F, Valvo M, Ghezzi TL, Zuccaro M, Cenciarelli S, Trovato C, Sonzogni A, Biffi R (2013) Impact of robotic surgery on sexual and urinary functions after fully robotic nerve-sparing total mesorectal excision for rectal cancer. Ann Surg 257(4):672–678
Kim HJ, Choi GS, Park JS, Park SY, Yang CS, Lee HJ (2018) The impact of robotic surgery on quality of life, urinary and sexual function following total mesorectal excision for rectal cancer: a propensity score-matched analysis with laparoscopic surgery. Colorectal Dis 20(5):O103–O113
Oshio H, Oshima Y, Yunome G, Yano M, Okazaki S, Ashitomi Y, Musha H, Kamio Y, Motoi F (2021) Potential urinary function benefits of initial robotic surgery for rectal cancer in the introductory phase. J Robot Surg
Jayne D, Pigazzi A, Marshall H, Croft J, Corrigan N, Copeland J, Quirke P, West N, Rautio T, Thomassen N et al (2017) Effect of robotic-assisted vs conventional laparoscopic surgery on risk of conversion to open laparotomy among patients undergoing resection for rectal cancer: the ROLARR randomized clinical trial. JAMA 318(16):1569–1580
Corrigan N, Marshall H, Croft J, Copeland J, Jayne D, Brown J (2018) Exploring and adjusting for potential learning effects in ROLARR: a randomised controlled trial comparing robotic-assisted vs standard laparoscopic surgery for rectal cancer resection. Trials 19(1):339
Jimenez-Rodriguez RM, Diaz-Pavon JM, de la Portilla de Juan F, Prendes-Sillero E, Dussort HC, Padillo J (2013) Learning curve for robotic-assisted laparoscopic rectal cancer surgery. Int J Colorectal Dis 28(6):815–821
Park EJ, Kim CW, Cho MS, Kim DW, Min BS, Baik SH, Lee KY, Kim NK (2014) Is the learning curve of robotic low anterior resection shorter than laparoscopic low anterior resection for rectal cancer?: a comparative analysis of clinicopathologic outcomes between robotic and laparoscopic surgeries. Med (Baltimore) 93(25):e109
Yamaguchi T, Kinugasa Y, Shiomi A, Sato S, Yamakawa Y, Kagawa H, Tomioka H, Mori K (2015) Learning curve for robotic-assisted surgery for rectal cancer: use of the cumulative sum method. Surg Endosc 29(7):1679–1685
Park IJ, Choi GS, Lim KH, Kang BM, Jun SH (2009) Multidimensional analysis of the learning curve for laparoscopic resection in rectal cancer. J Gastrointest Surg 13(2):275–281
Tekkis PP, Senagore AJ, Delaney CP, Fazio VW (2005) Evaluation of the learning curve in laparoscopic colorectal surgery: comparison of right-sided and left-sided resections. Ann Surg 242(1):83–91
Park EJ, Kim CW, Cho MS, Baik SH, Kim DW, Min BS, Lee KY, Kim NK (2014) Multidimensional analyses of the learning curve of robotic low anterior resection for rectal cancer: 3-phase learning process comparison. Surg Endosc 28(10):2821–2831
Lee JM, Yang SY, Han YD, Cho MS, Hur H, Min BS, Lee KY, Kim NK (2021) Can better surgical outcomes be obtained in the learning process of robotic rectal cancer surgery? A propensity score-matched comparison between learning phases. Surg Endosc 35(2):770–778
Sugihara K, Kobayashi H, Kato T, Mori T, Mochizuki H, Kameoka S, Shirouzu K, Muto T (2006) Indication and benefit of pelvic sidewall dissection for rectal cancer. Dis Colon Rectum 49(11):1663–1672
Shida D, Kanemitsu Y, Hamaguchi T, Shimada Y (2019) Introducing the eighth edition of the tumor-node-metastasis classification as relevant to colorectal cancer anal cancer and appendiceal cancer a comparison study with the seventh edition of the tumor-node-metastasis and the Japanese Classification of Colorectal Appendiceal and Anal Carcinoma. Jpn J Clin Oncol 49(4):321–328
Dindo D, Demartines N, Clavien PA (2004) Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg 240(2):205–213
Oba A, Ishizawa T, Mise Y, Inoue Y, Ito H, Ono Y, Sato T, Takahashi Y, Saiura A (2019) Possible underestimation of blood loss during laparoscopic hepatectomy. BJS Open 3(3):336–343
Steiner SH, Cook RJ, Farewell VT, Treasure T (2000) Monitoring surgical performance using risk-adjusted cumulative sum charts. Biostat 1(4):441–452
Kim S, Yoon YS, Han HS, Cho JY, Choi Y, Lee B (2021) Evaluation of a single surgeon’s learning curve of laparoscopic pancreaticoduodenectomy: risk-adjusted cumulative summation analysis. Surg Endosc 35(6):2870–2878
Persiani R, Agnes A, Belia F, D’Ugo D, Biondi A (2021) The learning curve of TaTME for mid-low rectal cancer: a comprehensive analysis from a five-year institutional experience. Surg Endosc 35(11):6190–6200
Sakai Y, Kitano S (2015) Practice guidelines on endoscopic surgery for qualified surgeons by the endoscopic surgical skill qualification system. Asian J Endosc Surg 8(2):103–113
Nakanishi R, Fukunaga Y, Mukai T, Nagasaki T, Yamaguchi T, Akiyoshi T, Konishi T, Nagayama S, Ueno M (2021) Educational system for acquiring appropriate laparoscopic colorectal surgical skills: analysis in a Japanese high-volume cancer center. Surg Endosc 35(6):2660–2666
Melich G, Hong YK, Kim J, Hur H, Baik SH, Kim NK, Sender Liberman A, Min BS (2015) Simultaneous development of laparoscopy and robotics provides acceptable perioperative outcomes and shows robotics to have a faster learning curve and to be overall faster in rectal cancer surgery: analysis of novice MIS surgeon learning curves. Surg Endosc 29(3):558–568
Foo CC, Law WL (2016) The learning curve of robotic-assisted low rectal resection of a novice rectal surgeon. World J Surg 40(2):456–462
Guend H, Widmar M, Patel S, Nash GM, Paty PB, Guillem JG, Temple LK, Garcia-Aguilar J, Weiser MR (2017) Develo** a robotic colorectal cancer surgery program: understanding institutional and individual learning curves. Surg Endosc 31(7):2820–2828
Jimenez-Rodriguez RM, Rubio-Dorado-Manzanares M, Diaz-Pavon JM, Reyes-Diaz ML, Vazquez-Monchul JM, Garcia-Cabrera AM, Padillo J, De la Portilla F (2016) Learning curve in robotic rectal cancer surgery: current state of affairs. Int J Colorectal Dis 31(12):1807–1815
Lee JM, Yang SY, Han YD, Cho MS, Hur H, Min BS, Lee KY, Kim NK (2021) Can better surgical outcomes be obtained in the learning process of robotic rectal cancer surgery? A propensity score-matched comparison between learning phases. Surg Endosc Other Interv Tech 35(2):770–778
Kuhry E, Bonjer HJ, Haglind E, Hop WC, Veldkamp R, Cuesta MA, Jeekel J, Pahlman L, Morino M, Lacy A et al (2005) Impact of hospital case volume on short-term outcome after laparoscopic operation for colonic cancer. Surg Endosc 19(5):687–692
Katayama H, Inomata M, Mizusawa J, Nakamura K, Watanabe M, Akagi T, Yamamoto S, Ito M, Kinugasa Y, Okajima M et al (2021) Institutional variation in survival and morbidity in laparoscopic surgery for colon cancer: from the data of a randomized controlled trial comparing open and laparoscopic surgery (JCOG0404). Ann Gastroenterol Surg 5(6):823–831
Kawai K, Hata K, Tanaka T, Nishikawa T, Otani K, Murono K, Sasaki K, Kaneko M, Emoto S, Nozawa H (2018) Learning Curve of Robotic Rectal Surgery With Lateral Lymph Node Dissection: Cumulative Sum and Multiple Regression Analyses. J Surg Educ 75(6):1598–1605
Ishihara S, Kiyomatsu T, Kawai K, Tanaka T, Hata K, Kazama S, Sunami E, Nozawa H, Watanabe T (2018) The short-term outcomes of robotic sphincter-preserving surgery for rectal cancer: comparison with open and laparoscopic surgery using a propensity score analysis. Int J Colorectal Dis 33(8):1047–1055
Othman W, Lai ZA, Abril C, Barajas-Gamboa JS, Corcelles R, Kroh M, Qasaimeh MA (2021) Tactile sensing for minimally invasive surgery: conventional methods and potential emerging tactile technologies. Front Robot AI 8:705662
Zapata-Impata BS, Gil P, Mezouar Y, Torres F (2021) Generation of tactile data from 3D vision and target robotic grasps. IEEE Trans Haptics 14(1):57–67
Overtoom EM, Horeman T, Jansen FW, Dankelman J, Schreuder HWR (2019) Haptic feedback, force feedback, and force-sensing in simulation training for laparoscopy: a systematic overview. J Surg Educ 76(1):242–261
Acknowledgements
We thank Kazunori Takeda for designing the study. We thank Emily Woodhouse, PhD, and Leah Cannon, PhD, from Edanz (https://jp.edanz.com/ac) for editing a draft of this manuscript.
Author information
Authors and Affiliations
Contributions
H.O., Y.O., and G.Y. substantially contributed to the study conceptualization. T.K. and F.M. significantly contributed to data analysis and interpretation. F.M. substantially contributed to the manuscript drafting. All authors critically reviewed and revised the manuscript draft and approved the final version for submission.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethics approval
The study protocol was approved by the local ethics committees of Sendai Medical Center (reference number: 27–8). The research was conducted in accordance with the 1964 Declaration of Helsinki and its later amendments.
Patient consent
Informed consent was obtained from all patients.
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Oshio, H., Konta, T., Oshima, Y. et al. Learning curve of robotic rectal surgery using risk-adjusted cumulative summation: a 5-year institutional experience. Langenbecks Arch Surg 408, 89 (2023). https://doi.org/10.1007/s00423-023-02829-0
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s00423-023-02829-0