Abstract
Purpose
Long-term urinary outcomes for patients born with Hirschsprung disease (HD) and anorectal malformations (ARM) may impact their health and wellbeing into adulthood. This study describes self-reported long-term urinary outcomes in males with HD and ARM.
Methods
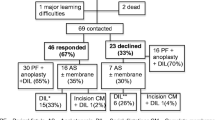
This was a prospective study of male patients in the Adult Colorectal Research Registry who completed surveys on urinary function between October 2019 and March 2022. Self-reported health and functional outcomes were summarized, and differences based on type of condition were compared.
Results
Sixty-seven patients completed the questionnaire (response rate: 59.1%), of which 17.9% (12) had HD and 82.1% (55) had an ARM. Rates of urinary incontinence and stress urinary incontinence were 16.4% (11) and 4.5% (3), respectively. On sub-analysis of patients with ARM, patients with sacral ratio (SR) of 0.4–0.69 reported higher UTI rates compared to those with SR ≥ 0.7 (57.9 vs 25.8%, p = 0.023). Renal failure rates were highest among patients with recto-bladder neck fistulas (66.0%, p = 0.012).
Conclusion
Patients with HD and ARM report a variety of urological sequelae in adulthood. Outcomes appear to be more common in patients with ARM and may be impacted by both anatomy and sacral ratios. Transitional care to monitor and manage renal and urological function is imperative.
Similar content being viewed by others
References
Sood S, Lim R, Collins L, Trajanovska M, Hutson JM, Teague WJ, King SK (2018) The long-term quality of life outcomes in adolescents with Hirschsprung disease. J Pediatr Surg 53(12):2430–2434. https://doi.org/10.1016/j.jpedsurg.2018.08.036
Roorda D, Witvliet MJ, Wellens LM, Schulten DV, Sloots CEJ, de Blaauw I, Broens PMA, Oosterlaan J, van Heurn LWE, van der Steeg AFW (2018) Long-term outcome and quality of life in patients with total colonic aganglionosis in the Netherlands. Colorectal Dis 20(8):719–726. https://doi.org/10.1111/codi.14095
Meinds RJ, van der Steeg AFW, Sloots CEJ, Witvliet MJ, de Blaauw I, van Gemert WG, Trzpis M, Broens PMA (2019) Long-term functional outcomes and quality of life in patients with Hirschsprung’s disease. Br J Surg 106(4):499–507. https://doi.org/10.1002/bjs.11059
Bjoersum-Meyer T, Kaalby L, Lund L, Christensen P, Jakobsen MS, Baatrup G, Qvist N, Ellebaek M (2021) Long-term functional urinary and sexual outcomes in patients with anorectal malformations-a systematic review. Eur Urol Open Sci 25:29–38. https://doi.org/10.1016/j.euros.2021.01.007
Bischoff A, Levitt MA, Peña A (2013) Update on the management of anorectal malformations. Pediatr Surg Int 29(9):899–904. https://doi.org/10.1007/s00383-013-3355-z
Strine AC, VanderBrink BA, Alam Z, Schulte M, Noh PH, DeFoor WR Jr, Minevich E, Sheldon CA, Frischer JS, Reddy PP (2017) Clinical and urodynamic outcomes in children with anorectal malformation subtype of recto-bladder neck fistula. J Pediatr Urol 13(4):376.e1-376.e6. https://doi.org/10.1016/j.jpurol.2017.06.008
Neuvonen M, Kyrklund K, Taskinen S, Koivusalo A, Rintala RJ, Pakarinen MP (2017) Lower urinary tract symptoms and sexual functions after endorectal pull-through for Hirschsprung disease: controlled long-term outcomes. J Pediatr Surg 52(8):1296–1301. https://doi.org/10.1016/j.jpedsurg.2017.02.013
De La Torre L, Langer JC (2010) Transanal endorectal pull-through for Hirschsprung disease: technique, controversies, pearls, pitfalls, and an organized approach to the management of postoperative obstructive symptoms. Semin Pediatr Surg 19(2):96–106. https://doi.org/10.1053/j.sempedsurg.2009.11.016
Harris PA, Taylor R, Thielke R, Payne J, Gonzalez N, Conde JG (2009) Research electronic data capture (REDCap)—A metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inform 42(2):377–381
Kyrklund K, Taskinen S, Rintala RJ, Pakarinen MP (2012) Lower urinary tract symptoms from childhood to adulthood: a population based study of 594 Finnish individuals 4 to 26 years old. J Urol 188(2):588–593. https://doi.org/10.1016/j.juro.2012.04.016
Giuliani S, Midrio P, De Filippo RE, Vidal E, Castagnetti M, Zanon GF, Gamba PG (2013) Anorectal malformation and associated end-stage renal disease: management from newborn to adult life. J Pediatr Surg 48(3):635–641. https://doi.org/10.1016/j.jpedsurg.2012.10.073
Bischoff A, DeFoor W, VanderBrink B, Goebel J, Hall J, Alonso M, Reddy P, Peña A (2015) End stage renal disease and kidney transplant in patients with anorectal malformation: is there an alternative route? Pediatr Surg Int 31(8):725–728. https://doi.org/10.1007/s00383-015-3734-8
Chong C, Hamza Y, Tan YW, Paul A, Garriboli M, Wright AJ, Olsburgh J, Taylor C, Sinha MD, Mishra P, Taghizadeh A (2022) Long-term urology outcomes of anorectal malformation. J Pediatr Urol 18:150.e1-150.e6. https://doi.org/10.1016/j.jpurol.2022.01.019
Hofmann AD, Duess JW, Puri P (2014) Congenital anomalies of the kidney and urinary tract (CAKUT) associated with Hirschsprung’s disease: a systematic review. Pediatr Surg Int 30(8):757–761. https://doi.org/10.1007/s00383-014-3529-3
Pini Prato A, Arnoldi R, Falconi I, Dusio MP, Ceccherini I, Tentori A, Felici E, Nozza P (2021) Congenital anomalies of the kidney and urinary tract in a cohort of 280 consecutive patients with Hirschsprung disease. Pediatr Nephrol 36(10):3151–3158. https://doi.org/10.1007/s00467-021-05061-4
Davidson JR, Kyrklund K, Eaton S, Pakarinen MP, Thompson DS, Cross K, Blackburn SC, De Coppi P, Curry J (2021) Long-term surgical and patient-reported outcomes of Hirschsprung disease. J Pediatr Surg 56(9):1502–1511. https://doi.org/10.1016/j.jpedsurg.2021.01.043
Granéli C, Marschall Sima H, Börjesson A, Hagelsteen K, Arnbjörnsson E, Stenström P (2019) Urinary tract anomalies and urinary tract dysfunction in children with Hirschsprung disease-Is follow-up indicated? J Pediatr Surg 54(10):2012–2016. https://doi.org/10.1016/j.jpedsurg.2018.12.006
Rosen N, Holder M (2022) What parents need to know about Hirschsprung disease. Semin Pediatr Surg 31:151159
Kyrklund K, Pakarinen MP, Taskinen S, Rintala RJ (2015) Bowel function and lower urinary tract symptoms in males with low anorectal malformations: an update of controlled, long-term outcomes. Int J Colorectal Dis 30(2):221–228. https://doi.org/10.1007/s00384-014-2074-9
Harwood R, Reid T, Salim A, Rachmani E, Siminas S, Horwood F, Almond SL, Corbett HJ (2021) Routine evaluation of vesico-ureteric reflux in children with anorectal malformation does not reduce the rate of urinary tract infection. J Pediatr Surg 56(10):1811–1815. https://doi.org/10.1016/j.jpedsurg.2021.02.062
Samuk I, Bischoff A, Hall J, Levitt M, Peña A (2016) Anorectal malformation with rectobladder neck fistula: a distinct and challenging malformation. J Pediatr Surg 51:1592e6
Tikkinen KA, Heikkilä J, Rintala RJ, Tammela TL, Taskinen S (2011) Lower urinary tract symptoms in adults treated for posterior urethral valves in childhood: matched cohort study. J Urol 186(2):660–666. https://doi.org/10.1016/j.juro.2011.03.150
Bartoli S, Aguzzi G, Tarricone R (2010) Impact on quality of life of urinary incontinence and overactive bladder: a systematic literature review. Urology 75(3):491–500. https://doi.org/10.1016/j.urology.2009.07.1325
Acker S, Peña A, Wilcox D, Alaniz V, Bischoff A (2019) Transition of care: a growing concern in adult patients born with colorectal anomalies. Pediatr Surg Int 35(2):233–237. https://doi.org/10.1007/s00383-018-4401-7
Wood D, Wood H (2021) Congenital lifelong urology. World J Urol 39(4):979–980. https://doi.org/10.1007/s00345-021-03686-6
Faure Walker N, Gill B, Olsburgh J, Gillatt D, Yap T, Michala L, Taylor C, Wood H, Wood D (2021) Age-related urologic problems in the complex urologic patient. World J Urol 39(4):1037–1044. https://doi.org/10.1007/s00345-020-03111-4
Funding
The authors did not receive support from any organization for the submitted work. The authors have no relevant financial or non-financial interests to disclose.
Author information
Authors and Affiliations
Contributions
MLR, AB, and DW were responsible for study design. MLR and JK collected data, MLR performed data analysis. MLR, and DW wrote the main manuscript text. All authors critically reviewed the manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Reppucci, M.L., Wehrli, L.A., Wilcox, D. et al. Patient-reported urinary outcomes in adult males with congenital colorectal conditions. Pediatr Surg Int 38, 1709–1716 (2022). https://doi.org/10.1007/s00383-022-05215-x
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00383-022-05215-x