Abstract
Purpose
Traditionally, the care of children and adults has been arbitrarily separated into pediatric and adult medicine and surgery. Despite progress in pediatric surgical techniques, patients born with congenital anomalies still suffer from significant functional sequelae, which persist into adulthood. We aim to describe some of the most common problems experienced by adult patients with congenital colorectal malformations.
Methods
Following IRB approval, we performed a retrospective database review of all adult patients who were treated by our group from 1983 until 2017.
Results
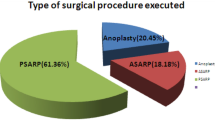
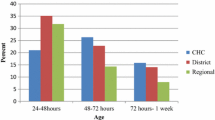
We identified 88 cases. 51 patients had ARM, 18 cloacas, 9 presacral masses, 3 HD, 2 spina bifida and 5 with other diagnoses (3 vaginal anomalies, 1 cloacal exstrophy, 1 obstructed seminal vesical). The specific problems addressed were: complications from previous operations (41), rectal prolapse (25), fecal incontinence (11), gynecologic concerns (12), urologic concerns (6), and recurrent recto urogenital fistula (3). We performed 83 surgical interventions, including 13 rectal prolapse repair, 13 continent appendicostomies, 44 PSARP or redo PSARP, 11 resections of presacral masses, 11 vaginoplasties, 2 examinations under anesthesia, and 2 Mitrofanoff procedures. Five patients were treated medically (bowel management program, obstetric, urologic evaluation).
Conclusion
There is a growing need to better prepare adult providers to assume the care of patients born with congenital colorectal disease as these patients transition to adulthood. A collaboration between specialized pediatric referral centers with adult colorectal surgeons, urologists and gynecologists is a potential pathway for the adequate transition of care.



Similar content being viewed by others
References
Pena A, DeVries PA (1982) Posterior sagittal anorectoplasty: important technical considerations and new applications. J Pediatr Surg 17:796–811
Bischoff A, Levitt MA, Pena A (2013) Update on the management of anorectal malformations. Pediatr Surg Int 29(9):899–904
Alam S, Lawal TA, Pena A et al (2011) Acquired posterior urethral diverticulum following surgery for anorectal malformations. J Pediatr Surg 46(6):1231–1235
Levitt MA, Bischoff A, Pena A (2011) Pitfalls and challenges of cloaca repair: hot to reduce the need for reoperations. J Pediatr Surg 46(6):1250–1255
Bischoff A, Levitt MA, Bauer C et al (2009) Treatment of fecal incontinence with a comprehensive bowel management program. J Pediatr Surg 44:1278–1284
Bischoff A, Levitt MA, Peña A (2009) Bowel Management for the treatment of pediatric fecal incontinence. Pediatr Surg Int 25:1027–1042
Bischoff A, Tovilla M (2010) A practical approach to the management of pediatric fecal incontinence. Semin Pediatr Surg 19:154–159
Rangel SJ, Lawal TA, Bischoff A et al (2011) The appendix as a conduit for antegrade continence enemas in patients with anorectal malformations: lessons learned from 163 cases treated over 18 years. J Pediatr Surg 46:1236–1242
Samuk I, Bischoff A, Hall J et al (2016) Anorectal malformation with rectobladder neck fistula: a distinct and challenging malformation. J Pediatr Surg 51:1592–1596
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Acker, S., Peña, A., Wilcox, D. et al. Transition of care: a growing concern in adult patients born with colorectal anomalies. Pediatr Surg Int 35, 233–237 (2019). https://doi.org/10.1007/s00383-018-4401-7
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00383-018-4401-7