Abstract
Background
Chimeric antigen receptor (CAR) T cells for refractory or relapsed (r/r) B cell no-Hodgkin lymphoma (NHL) patients have shown promising clinical effectiveness. However, the factors impacting the clinical response of CAR-T therapy have not been fully elucidated. We here investigate the independent influencing factors of the efficacy of CD19 CAR-T cell infusion in the treatment of r/r B-NHL and to establish an early prediction model.
Methods
A total of 43 r/r B-NHL patients were enrolled in this retrospective study. The patients’ general data were recorded, and the primary endpoint is the patients’ treatment response. The independent factors of complete remission (CR) and partial remission (PR) were investigated by univariate and binary logistic regression analysis, and the prediction model of the probability of CR was constructed according to the determined independent factors. Receiver operating characteristic (ROC) and calibration plot were used to assess the discrimination and calibration of the established model. Furthermore, we collected 15 participators to validate the model.
Results
Univariate analysis and binary logistic regression analysis of 43 patients showed that the ratio of central memory T cell (Tcm) and naïve T cell (Tn) in cytotoxic T cells (Tc) was an independent risk factor for response to CD19 CAR-T cell therapy in r/r B-NHL. On this basis, the area under the curve (AUC) of Tcm in the Tc and Tn in the Tc nomogram model was 0.914 (95%CI 0.832–0.996), the sensitivity was 83%, and the specificity was 74.2%, which had excellent predictive value. We did not found the difference of the progression-free survival (PFS).
Conclusions
The ratio of Tcm and Tn in Tc was found to be able to predict the treatment response of CD19 CAR-T cells in r/r B-NHL. We have established a nomogram model for the assessment of the CD19 CAR-T therapy response presented high specificity and sensitivity.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Implications for practice
A nomogram was developed to predict the therapeutic response of the CD19 CAR-T infusion product to lymphoma. Based on the receiver operating characteristic curves and the calibration curves, this nomogram identifies several variables with great predictive power for CD19 CAR-T infusion product responses to lymphoma, which provide the basis for clinical adjustment of the treatment plan.
Introduction
Chimeric antigen receptor T cell (CAR-T) therapy is different from conventional small molecule or biological therapy. It collects T cells from patients’ blood through single cell collection. It can express the chimeric antigen receptor (CAR) to recognize and attack tumor cells expressing specific antigens and after modification. At present, its efficacy in diffuse large B cell lymphoma (DLBCL) has been confirmed [1]. The US Food and Drug Administration (FDA) had approved three CD19 CAR-T products, axicabtagene ciloleucel, tisagenlecleucel and lisocabtagene maraleucel to treat refractory/relapsed B cell non-Hodgkin’s lymphoma (r/r B-NHL). Research has shown that the total effective rate (ORR) of treatment is 52 to 82%, and the complete effective rate (CR) is 40 to 58% [2, 3]. However, some patients are not sensitive to CAR-T therapy, and for those who are effective with CAR-T therapy, studies have found that 50% of patients experience recurrence eventually [4]. This is partly due to the heterogeneous influence of functional T cells, tumor microenvironment [5] and patient baseline status. In addition, early clinical response evaluation is also important to improve the cost-effectiveness due to the high cost of CAR-T therapy. Therefore, an early prediction model of treatment response is crucial for patients.
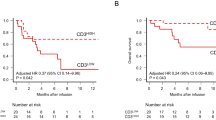
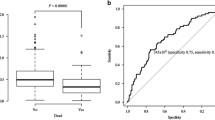
The factors that influence the clinical response to CAR-T therapy are not fully understood. Several studies have attempted to determine the impact of these clinical factors [5, Table 1 shows the patients’ baseline characteristics and the CD19 CAR-T cells they initially received. A total of 43 patients with r/r NHL were enrolled in training cohort, comprising 36 (83.7%) cases of diffuse large B cell lymphoma, 2 (4.7%) cases of mantle cell lymphoma, 2 (4.7%) cases of follicular lymphoma, 2 (4.7%) cases of B cell lymphoblastic lymphoma and 1 (2.2%) case of Burkitt’s lymphoma. There were approximately three times as many men as women, and the median age was 56 years (range 26–85 years). Moreover, ten patients (23.3%) had bone marrow involvement prior to CAR-T cell infusion, and 23 (62.7%) patients had a high tumor burden. Meanwhile, the median number of lines of therapy prior to CAR-T cell infusion was 3 (range, 1–7). The median dose of infused CAR-T cells was 3.82 × 10^6/kg (range, 0.85–12.79). Meanwhile, the median WBC, hemoglobin, platelet, LDH, CRP and ferritin counts before lymphodepletion (baseline blood count) were 3.97 × 10^9/L, 109 g/L, 154 × 10^9/L, 225.3U/L, 4.52 mg/L and 379 ng/ml. Before treatment, the median CD4/CD8 ratio of peripheral blood T cells was 1.1 (0.15–13.43), the median proportion of Treg cells was 5.71% (0.07–31.47), the proportion of Tcm in Th and Tc cells was 7.68% (0.38–62.95) and 31.88% (3.17–64.77), respectively. The proportion of Tn in Th and Tc cells was 13.55% (1.15–46.77) and 8.64% (0–48.68), respectively. The proportion of Teff in Th and Tc was 2.88% (0.16–50.38) and 33.43% (0–79.28), respectively. The proportion of Tem in Th and Tc cells was 34.11% (5.72–92) and 35.12% (0–84.97), respectively. Thirty-one (72.1%) patients achieved CR or PR one to three months after CAR-T cell infusion. Additionally, the patients characteristics of validation cohort are also presented in Table 1, including 14 DLBCL and 1 FL. To further explore the prognostic value, the long-term survival was compared between the ratio of Tcm in Tc and Tn in Tc. The median follow-up of this study was 9 months (1.37–74.83). In the training cohort, the difference between the proportion of Tcm in Tc (log rank p = 0.88) and Tn in Tc (log rank p = 0.96) does not cause the comparison difference of PFS (Supplementary Fig. 1). To search for possible factors for CD19 CAR-T treatment in r/r NHL patients, we first performed univariate logistic regression analysis on patients’ clinical characteristics (Table 2), baseline hematological parameters (Table 3) and the first infusion of CAR-T cells (Supplementary Table 2). The results of univariate analysis showed that the patient’s baseline tumor burden, ECOG score, the proportion of Treg cells in peripheral blood T cell subsets and the proportion of Tcm and Tn in Tc cells at diagnosis were significantly associated with remission (CR and PR) after CAR-T cell infusion (p < 0.05). As demonstrated in Fig. 3B–D, the proportion of Treg cells in the response group was significantly lower than in the non-response group (SD and PD). On the contrary, the proportion of Tcm and Tn in Tc cells was significantly higher than that in the non-response group. Although age and the proportion of Tn in Th cells shown in Fig. 3E present correlation with remission, the difference was not statistically significant. However, in Fig. 3A, the CD4/CD8 ratio was not different between the two groups, which may be related to the small sample size. The proportions of T cell subsets in NHL patients. A There was no significant difference in the proportion of CD4 + and CD8 + T cells between response and non-response group (p = 0.6268). B The proportion of Treg cells in the response group was significantly lower than in the non-response group (p < 0.05). C, D The proportion of Tcm and Tn in Tc cells was significantly higher than that in the non-response group (p < 0.05). E The proportion of Tn in the response group was higher than that in the non-response group, but the difference was not statistically significant (p > 0.05) To find out more about the independent factors for response to CD19 CAR-T therapy, the statistically significant factors from the above univariate analysis (univariate logistic p 0.05) were added to the binary logistic regression analysis (Supplementary Table 3). The results of the binary analysis showed that the changes in the proportions of T cell subsets collected from the patients’ peripheral blood before CD19 CAR-T infusion were significant independent factors for the therapeutic effect of CAR-T cells, among which the proportions of Tcm and Tn in Tc cells significantly influenced remission (p < 0.05) (Fig. 4A). ROC curve results showed that the AUC of Tcm in Tc and Tn in Tc for predicting the efficacy of CAR-T cell therapy was > 60%, the AUC of Tcm in Tc was 0.855 (95%CI 0.737–0.9730), and the AUC of Tn in Tc was 0.836 (95%CI 0.712–0.960) (Supplementary Table 4) (Fig. 4B). Discriminative ability of Tcm and Tn in Tc between CR and NR. A Multivariate logistic regression analysis showed that Tcm and Tn in Tc were closely related to CAR-T treatment response (p < 0.05). B The ROC curve showed the ability of the T subsets to discriminate between the response and non-response groups. Tcm and Tn in Tc represented good discriminative power with AUC > 0.6, respectively Potential biomarkers with concurrent AUC > 0.6 were identified based on the selection criteria of p < 0.05 between the remission and non-remission groups. We therefore selected Tcm in Tc cells and Tn in Tc cells as predictive biomarkers of early response after CD19 CAR-T therapy. Based on the baseline percentage of Tcm and Tn in Tc cells, we developed an early prediction model of the treatment effect to analyze the likelihood of remission. Then, to assess remission response in clinical practice, we developed a nomogram that could help predict the likelihood of CR and PR for each individual in clinical practice. Finally, we internally validated the original data and drew a calibration curve to further evaluate the authenticity and accuracy of the prediction model in the actual situation. The results showed good agreement between the likelihood of predicting remission and the observed early response (Figs. 5A and B). The total scores of Tcm and Tn were calculated in the nomogram, and the ROC curve was drawn to predict the treatment effect. The AUC result was 0.914 (95%CI 0.832–0.996), showing good predictive ability (Fig. 5C). Moreover, we further validated this predictive model in an independent cohort. The internal validation cohort consisted of 15 r/r B-NHL patients enrolled during a subsequent period of time. The baseline characteristics of the validation group are shown in Supplementary Table 1. According to the established predictive models for response, ROC curve results of validation cohort showed that the AUC of Tcm in Tc and Tn in Tc for predicting the efficacy of CAR-T cell therapy was > 60%, the AUC of Tcm in Tc was 0.860 (95%CI 0.6587–1.0000), and the AUC of Tn in Tc was 0.940 (95%CI 0.8137–1.0000) (Supplementary Fig. 2A). The ROC curve was drawn to predict the validation cohort treatment effect, and AUC result was 0.9301 (95%CI 0.8568–1.0), showing good predictive ability (Supplementary Fig. 2B). The results showed that the prediction model had high sensitivity and specificity in predicting the effect of CD19 CAR-T treatment (sensitivity 83%, specificity 74.2%), and the maximum Youden index was 0.742, and the prediction results were in good agreement with the actual situation (kappa, 0.616), indicating that the model has good predictive ability and has some clinical application value. The early prediction model nomogram and calibration curve. A A nomogram was created based on the proportion of Tcm and Tn in Tc to predict response to CAR-T treatment. B Calibration curves of the early predictive model comparing the predicted probability of response. C The total scores of Tcm and Tn were calculated by the nomogram prediction model, and the ROC curve was drawn to predict the response to CAR-T therapy. AUC = 0.914 (95%CI 0.832–0.996) Chimeric antigen receptor-modified T (CAR-T) cells have shown significant advantages in the treatment of hematological malignancies. The clinical trial data of our center have good therapeutic effects and are similar to the clinical effects of commercial CAR-T products [14]. However, some patients are not sensitive to CAR-T therapy, and for those who are effective with CAR-T therapy, studies have found that 50% of patients experience recurrence eventually. In this retrospective study, we analyzed patients’ clinical characteristics, baseline hematological parameters and the proportion of T cell subsets isolated from peripheral blood before treatment to identify independent risk factors affecting the efficacy of CAR-T cell therapy. Combined with univariate and multivariate analyses, it was found that the proportions of Tn and Tcm in patients’ peripheral blood CD8 + T cells were positively correlated with clinical outcome after CAR-T treatment. Therefore, we established an early prediction model to analyze the possibility of CR and PR in lymphoma patients based on the proportions of Tcm in Tc and Tn in Tc. This model helps to predict early treatment response in patients with r/r B-NHL. Based on this model, identification of T cell phenotypes prior to CAR-T manufacturing may lead to early intervention by enriching dominant cell subsets or consuming undesirable cell populations or functional states during manufacturing, thereby reducing the failure and relapse rates of CAR-T therapy in r/r NHL. With the advancement of CAR-T treatment technology, the target population for its treatment is constantly expanding. CAR-T treatment has moved from being considered a third-line treatment or greater to a second-line treatment. With the expansion of the target population for CAR-T treatment, there will inevitably be differences in the responses of different populations to CAR-T treatment. If biomarkers can be used to distinguish them, it can help select more suitable target patients or combine other methods to improve the treatment effect for patients with potential poor efficacy. In this study, the results of univariate analysis showed that the patient’s baseline tumor burden and ECOG score were significantly associated with remission (CR and PR) after CAR-T cell infusion (p < 0.05). Our results are basically consistent with other research findings. Vercellino et al. [8] analyzed the characteristics of 116 patients at the time of decision (TD) to use commercial CAR (axicabtagene ciloleucel, n = 49; tisagenlecleucel n = 67) and at the time of treatment (TT) and found that the risk factors for early progression of TD and TT during treatment were extranodal (EN) site involvement (≥ 2 sites) and lymphoma burden (LDH, TMTV). This reminds us that disease control before administering CAR-T cells is crucial for better response. Some biomarkers mainly choose to exclude patients who have many potential negative factors that may affect the efficacy of CAR-T through a reverse thinking approach. The research team retrospectively analyzed 34 paired samples in a dual-target CAR-T clinical study and found that 38.2% of patients had low expression of NOXA before CAR-T treatment. Patients with low expression of NOXA received CAR-T treatment, and their PFS and OS were significantly reduced compared to those with high expression of NOXA. ORR and CR rates were also affected [15]. Interestingly, the team’s research found that low expression of NOXA can be reversed by HDACi inhibitors. The HDACi inhibitor Chidamide, independently developed in China, can enhance the killing activity of CAR-T against tumor cells by reversing the low expression of NOXA to high expression [15]. The reversible biomarker provides a foundation for subsequent clinical conversion. The cellular and molecular diversity of CAR-T cell products is an important factor in the efficacy of CD19 CAR-T cell therapy in LBCL. In this study, we found that T cell heterogeneity in blood samples isolated for CAR-T product manufacturing had a profound impact on clinical outcomes. The high proportion of Tn and Tcm in CD8 + T cells was associated with an improved treatment response. This is consistent with Lamure et al. [16] who suggested that Tisa-cel response was associated with expansion of central memory CD8 + T populations, and Locke et al. [17] described results on the ZUMA-1 cohort that high percentages of naïve-like (CCR7 + CD45RA +) T cell were associated with a higher response rate. Deng et al. [18] found that product cells transfused into patients with durable CR at 3 months were rich in CD8 memory T cell phenotypes compared to PR/PD patients. And Zhang et al. [19] found that knocking out BATF shifts the population toward a more central memory subset and enhances the antitumor activity of CAR-T cells against solid tumors. CD19 CAR-T cells from completely responding individuals with chronic lymphocytic leukemia were enriched in memory-related genes, whereas CAR-T cells from non-responders upregulated effector- and exhaustion-related genes, suggesting that the quantity of Tcm cells is one of the major parameters for the persistence and activity of CAR-T cells [20, 21]. In addition, Lamure et al. [16] found that an increase in Treg cells appeared to be associated with non-response to treatment and could drive clinical relapse. In our study, the proportion of Treg cells was indeed negatively correlated with clinical outcome, although no statistically significant difference was found in the multivariate analysis, which was speculated to be due to the small sample size included, and further clarification is needed in larger cohort studies. This is similar to the finding for the CD4/CD8 ratio. Some investigators believe that the CD8 + T cell-mediated immune response to transgenic CAR-T cells after CAR-T cell infusion limits the persistence of CAR-T cells and increases the risk of relapse in some patients [22]. This study found that the proportion of CD4 + T cells was slightly higher than that of CD8 + T cells in the remission groups. Although this difference was not statistically significant, it also shows that the CD4/CD8 ratio may have an impact on clinical outcome. However, this study has some limitations. First, the number of patients is relatively small, and the predictive model we constructed needs to be further validated in larger prospective studies. In addition, most patients were discharged within 1–3 months after CAR-T treatment, and we only observed short-term efficacy after CAR-T treatment, not long-term outcomes. Articles indicate a positive correlation between the Tn or Tcm ratio and the persistence of CAR-T cells in vivo. There is a high proportion of Tn and memory T cell populations in the patient cohort with CAR-T cells persisting for more than 6 months and sustained remission [23]. We analyzed that our training cohort lasted for 3 years, so there was no difference in the observed results of PFS. Meanwhile, our study is limited to blood, and future studies and analyses of lymph node biopsy should be included to expand the content of this prediction model to comprehensively and deeply analyze the clinical outcomes of patients.Results
Clinical characteristics of the study population
Factors associated with CR and PR in r/r NHL patients after CAR-T therapy
Identification of independent factors influencing response to CAR-T therapy
Establishment and validation of an early prediction model for CD19 CAR-T treatment response
Discussion
Data availability
The data that support the findings of this study are available on request from the corresponding author.
Abbreviations
- AUC:
-
Area under the curve
- CAR-T:
-
Chimeric antigen receptor T cell
- CR:
-
Complete remission
- FDA:
-
Food and Drug Administration
- NR:
-
No response
- ORR:
-
Overall response rates
- PBMC:
-
Peripheral blood mononuclear cells
- PD:
-
Progressive disease
- PR:
-
Partial remission
- r/r B-NHL:
-
Refractory or relapsed B cell non-Hodgkin’s lymphoma
- ROC:
-
Receiver operating characteristic
- SD:
-
Stable disease
- Tc:
-
Cytotoxic T or CD8 + T cells
- Tcm:
-
Central memory T cell
- Tn:
-
Naïve T cell
References
Avanzi MP, Brentjens RJ (2017) Emerging role of CAR T cells in non-hodgkin’s lymphoma. J Natl Compr Cancer Netw JNCCN 15(11):1429–1437
Schuster SJ, Bishop MR, Tam CS, Waller EK, Borchmann P, McGuirk JP et al (2019) Tisagenlecleucel in adult relapsed or refractory diffuse large B-cell lymphoma. N Engl J Med 380(1):45–56
Locke FL, Ghobadi A, Jacobson CA, Miklos DB, Lekakis LJ, Oluwole OO et al (2019) Long-term safety and activity of axicabtagene ciloleucel in refractory large B-cell lymphoma (ZUMA-1): a single-arm, multicentre, phase 1–2 trial. Lancet Oncol 20(1):31–42
Schuster SJ, Tam CS, Borchmann P, Worel N, McGuirk JP, Holte H et al (2021) Long-term clinical outcomes of tisagenlecleucel in patients with relapsed or refractory aggressive B-cell lymphomas (JULIET): a multicentre, open-label, single-arm, phase 2 study. Lancet Oncol 22(10):1403–1415
Yan ZX, Li L, Wang W, OuYang BS, Cheng S, Wang L et al (2019) Clinical efficacy and tumor microenvironment influence in a dose-escalation study of anti-CD19 chimeric antigen receptor T cells in refractory B-cell non-hodgkin’s lymphoma. Clin Cancer Res Off J Am Assoc Cancer Res 25(23):6995–7003
Jia Q, Qin D, He F, **e Q, Ying Z, Zhang Y et al (2021) Peripheral eosinophil counts predict efficacy of anti-CD19 CAR-T cell therapy against B-lineage non-Hodgkin lymphoma. Theranostics 11(10):4699–4709
Jackson Z, Hong C, Schauner R, Dropulic B, Caimi PF, de Lima M et al (2022) Sequential single cell transcriptional and protein marker profiling reveals TIGIT as a marker of CD19 CAR-T cell dysfunction in patients with non-Hodgkin’s lymphoma. Cancer Discov 12:1886–2190
Vercellino L, Di Blasi R, Kanoun S, Tessoulin B, Rossi C, D’Aveni-Piney M et al (2020) Predictive factors of early progression after CAR T-cell therapy in relapsed/refractory diffuse large B-cell lymphoma. Blood Adv 4(22):5607–5615
Gu J, Liu S, Cui W, Dai H, Cui Q, Yin J et al (2022) Identification of the predictive models for the treatment response of refractory/relapsed B-cell all patients receiving CAR-T therapy. Front Immunol 13:858590
Dean EA, Mhaskar RS, Lu H, Mousa MS, Krivenko GS, Lazaryan A et al (2020) High metabolic tumor volume is associated with decreased efficacy of axicabtagene ciloleucel in large B-cell lymphoma. Blood Adv 4(14):3268–3276
Shouval R, Alarcon Tomas A, Fein JA, Flynn JR, Markovits E, Mayer S et al (2022) Impact of TP53 genomic alterations in large B-cell lymphoma treated with CD19-chimeric antigen receptor T-cell therapy. J Clin Oncol Off J Am Soc Clin Oncol 40(4):369–381
Green MR, Neelapu SS (2020) Not so FASt: tumor cells resisting death drive CAR T-cell dysfunction. Cancer Discov 10(4):492–494
Golubovskaya V, Wu L (2016) Different subsets of T cells memory effector functions and CAR-T immunotherapy. Cancers 8(3):36
Cao Y, Lu W, Sun R, ** X, Cheng L, He X et al (2019) Anti-CD19 chimeric antigen receptor T Cells in combination with nivolumab are safe and effective against relapsed/refractory B-cell non-hodgkin lymphoma. Front Oncol 9:767
Yan X, Chen D, Wang Y, Guo Y, Tong C, Wei J et al (2022) Identification of NOXA as a pivotal regulator of resistance to CAR T-cell therapy in B-cell malignancies. Signal Transduct Target Ther 7(1):98
Lamure S, Van Laethem F, De Verbizier D, Lozano C, Gehlkopf E, Tudesq JJ et al (2021) Clinical and product features associated with outcome of DLBCL patients to CD19-targeted CAR T-Cell therapy. Cancers 13(17):4279
Locke FL, Rossi JM, Neelapu SS, Jacobson CA, Miklos DB, Ghobadi A et al (2020) Tumor burden, inflammation, and product attributes determine outcomes of axicabtagene ciloleucel in large B-cell lymphoma. Blood Adv 4(19):4898–4911
Deng Q, Han G, Puebla-Osorio N, Ma MCJ, Strati P, Chasen B et al (2020) Characteristics of anti-CD19 CAR T cell infusion products associated with efficacy and toxicity in patients with large B cell lymphomas. Nat Med 26(12):1878–1887
Zhang X, Zhang C, Qiao M, Cheng C, Tang N, Lu S et al (2022) Depletion of BATF in CAR-T cells enhances antitumor activity by inducing resistance against exhaustion and formation of central memory cells. Cancer Cell 40(11):1407–22.e7
Depil S, Duchateau P, Grupp SA, Mufti G, Poirot L (2020) ‘Off-the-shelf’ allogeneic CAR T cells: development and challenges. Nat Rev Drug Discov 19(3):185–199
Fraietta JA, Lacey SF, Orlando EJ, Pruteanu-Malinici I, Gohil M, Lundh S et al (2018) Determinants of response and resistance to CD19 chimeric antigen receptor (CAR) T cell therapy of chronic lymphocytic leukemia. Nat Med 24(5):563–571
Turtle CJ, Hanafi LA, Berger C, Gooley TA, Cherian S, Hudecek M et al (2016) CD19 CAR-T cells of defined CD4+:CD8+ composition in adult B cell ALL patients. J Clin Investig 126(6):2123–2138
Chen GM, Chen C, Das RK, Gao P, Chen CH, Bandyopadhyay S et al (2021) Integrative bulk and single-cell profiling of premanufacture T-cell populations reveals factors mediating long-term persistence of CAR T-cell therapy. Cancer Discov 11(9):2186–2199
Acknowledgements
Not applicable
Funding
This work was supported by grants from the General Project of the National Natural Science Foundation of China (81970180 to MZ), the Science and Technology Project of Tian** Municipal Health Committee (TJWJ2022QN030 to MZ), the Key Projects of Tian** Applied Basic Research and Multi-Investment Fund (21JCZDJC01240), the Science and Technology Project of Tian** Municipal Health Committee (TJWJ2022XK018 to MZ), Tian** Municipal Science and Technology Commission Grant (21JCQNJC00070) and the Key Science and Technology Support Project of Tian** Science and Technology Bureau (20YFZCSY00800 to MZ), as well as Tian** Key Medical Discipline (Specialty) Construction Project (TJYXZDXK-056B).
Author information
Contributions
XMZ, RS and MZ wrote the manuscript. YFZ, XPC, RTG, YZ and XZL have substantively revised the manuscript. CCL and MFZ conceived this review and are accountable for all aspects of the work. The final manuscript read and approved by all authors.
Corresponding authors
Ethics declarations
Conflict of interest
All authors declare that there are no conflicts of interest.
Ethical approval
The study was approved by the Ethics Committee of Tian** First Central Hospital. And our study complies with the Declaration of Helsinki. The need for informed consent was waived due to the retrospective nature of the study because the data were anonymously analyzed. Written informed consent was obtained from the individual for the publication of any potentially identifiable images or data included in this article.
Consent for publication
Not applicable.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Zhang, X., Sun, R., Zhang, M. et al. A CAR-T response prediction model for r/r B-NHL patients based on a T cell subset nomogram. Cancer Immunol Immunother 73, 33 (2024). https://doi.org/10.1007/s00262-023-03618-w
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s00262-023-03618-w