Abstract
The predictors of treatment outcome after emergency extracorporeal shockwave lithotripsy (SWL) are not well characterized. Therefore, based on a large prospective cohort, we aimed to develop and validate a nomogram for predicting treatment outcome after emergency SWL in patients with symptomatic ureteral stones. The development cohort included 358 patients with symptomatic ureteral stones who underwent emergency SWL between June 2020 and August 2021 in our hospital. One hundred and twenty-nine patients with symptomatic ureteral stones participated in the validation cohort from September 2021 to April 2022. The data were prospectively recorded. The backward stepwise selection was applied using the likelihood ratio test with Akaike’s information criterion as the stop** rule. The efficacy of this predictive model was assessed concerning its clinical usefulness, calibration, and discrimination. Finally, 15.6% (56/358) of patients in the development cohort and 14.0% (18/129) of those in the validation cohort suffered from stone-free failure after emergency SWL. We identified four predictors for stone-free failure: stone size, stone density, skin to stone distance (SSD), and degree of hydronephrosis. This model showed good discrimination with an area under the receiver operating characteristic (AUROC) curves of 0.935 (0.899–0.971) and good calibration (P = 0.059). The decision curve analysis showed that the model was clinically valuable. In this large prospective cohort, we found that stone size, stone density, SSD, and degree of hydronephrosis were predictors of treatment outcome after emergency SWL. This nomogram will be helpful in preoperative risk stratification to provide individualized treatment recommendations for each patient. Furthermore, early identification and appropriate management of patients may increase the success rate of emergency SWL during the COVID-19 pandemic.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Urolithiasis is one of the most prevalent urological diseases. It is estimated that about 13% of the population will be affected by urinary stones during their lifetime [1, 2]. The upper urinary tract stone is the most common site. A large proportion of patients with ureteral stones might experience acute renal colic, severe infection, and renal function impairment; if it is not appropriately managed, patients may suffer more severe consequences, and thereby require intervention.
Emergency extracorporeal shockwave lithotripsy (SWL) is an essential strategy for symptomatic ureteral stones and is widely preferred as a safe means of managing acute renal colic. It is also highly accepted for its ease of management and low cost [3]. Compared to SWL, medicine, indwelling double-J tube, or nephrostomy might only rapidly relieve symptoms such as pain but not directly deal with the stone [4, 5]. Only three studies with small sample sizes assessed the effectiveness of emergency SWL for ureteral calculi during acute renal colic. Panah et al. retrospectively reported the results after emergency SWL of 97 patients presenting with their first episode of ureteral colic; 73.2% (71) patients experienced stone free after emergency SWL, and stone size and Hounsfield units are important factors in predicting success [6]. Likewise, Kurkar et al. prospectively studied 86 patients with persistent renal colic and single ureteral stone, the stone-free rate after emergency SWL were 44.2%. Lower stone density was the single predictor of successful stone clearance [7]. Ghalayini et al. aimed to assess the efficacy of SWL for ureteral calculi during acute renal colic; they retrospectively analyzed 108 patients from 2002 to 2007. They confirmed that the complete fragmentation rate after a single emergency SWL session was 52%, and stone size was the only predictive factor for retreatment [8]. The conclusions addressing this issue are inconsistent, and none of the studies have been validated. In addition, several potential risk factors, such as hydronephrosis and skin to stone distance (SSD) which might affect the treatment outcome, have not been explored [9, 10]. It is worth noting that nearly half to one-third of patients suffered from failure after emergency SWL; therefore, exploring the predictors of treatment outcome of emergency SWL in patients with symptomatic ureteral stones is necessary.
It is widely acknowledged that the COVID-19 pandemic had a significant impact on healthcare services around the globe. COVID-19 is a contagious viral infection, primarily infecting the pulmonary system with respiratory symptoms. Droplets and close contact are the main routes of transmission, thus creating significant risk to those present in the operating room during procedures involving general anesthesia and endotracheal intubation. Therefore, the question remains for urologists regarding how to treat ureteral stones during the COVID-19 pandemic most safely. Emergency SWL has more benefits in reducing the need for general anesthesia, airway manipulation, and body fluid exposure than ureteroscopic lithotripsy (URS) as an ambulatory intervention [11].
Establishing a nomogram based on the predictive model is accepted as a reliable tool for predicting risk by analyzing and illustrating significant predictors of critical clinical consequences, which gives a numerical probability of the event for precision treatment [12]. Moreover, in our study, SWL can be guided by real-time ultrasound avoiding X-ray radiation exposure and can deal with both radiopaque and radiolucent stones. Therefore, we aimed to develop and validate a nomogram to predict the treatment outcome of emergency SWL in patients with symptomatic ureteral stones during the COVID-19 pandemic.
Methods
Study design
This prospective study was conducted at Sheng**g Hospital of China Medical University from June 2020 to April 2022. Finally, the development cohort of this study comprised 358 consecutive patients who underwent SWL for ureteral stones at our center between June 2020 and August 2021. The validation cohort comprised 129 consecutive patients from September 2021 to April 2022 using the same inclusion and exclusion criteria (Fig. 1).
Ethical approval (2020PS520K) was provided by the Ethics Committee of Sheng**g Hospital Affiliated China Medical University. All of the eligible individuals gave their informed permission. ChiCTR2000033789 is the registry’s UIN for clinical research. The 1975 Declaration of Helsinki’s ethical principles were followed by the study procedure.
Inclusion and exclusion criteria
Inclusion criteria: patients with symptomatic ureteral stone (renal colic episode), ureteral stone with a size between 6 and 20 mm, either radiopaque or radiolucent stones were included, age ≥ 18 years, body mass index (BMI) < 30 kg/m2, stone density < 1000 Hounsfield’s units (HU), and skin to stone distance less than 11 cm. Recurrent or first-time stone formers were both eligible; stones with a low likelihood of spontaneous passage, persistent pain despite adequate analgesic medication; persistent obstruction, stone growth, and infection.
Exclusion criteria: pregnancy, coagulopathy, uncontrolled urinary tract infection, severe skeletal malformations, which prevent targeting of the stone; arterial aneurysm in the vicinity of the stone, multiple or bilateral ureteral stones; anatomical obstruction distal to the stone or congenital genitourinary anomaly (such as horseshoe kidney or ileal conduit), patients with internal stent/nephrostomy insertion before treatment for the resolution of urinary tract obstruction, transplanted kidney, solitary kidney, renal insufficiency (elevated creatinine).
The technique of SWL
SWL was performed using a third-generation electromagnetic lithotripter (XYS.SUI-6B, Shenzhen New Element Medical Equipment Technology Development Co., Ltd, Shenzhen, China). The focal depth was more than 110 mm; the focal area was ± 7 mm (radial) and ± 45–50 mm (axial), and the focal pressure was 6–30 MPa. The procedure was performed in a supine (proximal ureteral stone) or prone (middle or distal ureteral stone) position without anesthesia or sedation requirements. Stone localization and real-time monitoring during the procedure were performed by ultrasound (DC40, Shenzhen Mindray Bio-Medical Electronic Co., Ltd, Shenzhen, China). The shock frequency was 60–90 (shock waves/min). The total number of shock waves applied for one session was between 1500 and 2500, or the session was stopped when a significant stone fragmentation was detected. The voltage applied per session ranged from 10 to 16 kV with a stepwise power ram** strategy (power ram** was conducted during the first 200 shock waves). All procedures in the SWL group were outpatient procedures.
Before the procedure, careful control of pain to limit pain-induced movements and excessive respiratory excursions was needed. The patients received nonsteroidal anti-inflammatory (e.g., flurbiprofen 50 mg or ketorolac 30 mg by intravenous injection) or opioid drugs (pethidine 50 mg by intramuscular injection) for pain control prior to SWL when the VAS score was greater than 4, and the patients requested pain relief. Antibiotic prophylaxis was applied in case of increased bacterial burden (infectious stones or bacteriuria). A mild laxative (e.g., polyethylene glycol electrolytes powder) was taken the day before the procedure if it was difficult to locate the stone due to bowel interference. After the procedure, all patients were instructed to drink fluids and increase physical activity; ɑ-blockers and analgesics were also taken regularly. SWL was performed by senior expert doctors having vast experience after the patients provided informed consent.
Baseline characteristics and follow-up
Patient demographics (age, gender, and body mass index [BMI]), comorbidity (hypertension, diabetes mellitus, and coronary heart disease), previous history of urinary stone, stone characteristics (stone side, stone size, stone density, skin to stone distance (SSD), and grade of hydronephrosis), treatment outcome (stone-free rate [SFR] was evaluated at 1 month after SWL) were determined.
Proximal ureteral stone was defined as located between the pelvic–ureteral junction and the upper border of sacroiliac junction. Middle ureteral stone was defined as between upper border and lower border of the sacroiliac junction (include iliac vessel crossing). Distal ureteral stone was defined as the stone located between the lower border of sacroiliac junction and the orifice of ureter in bladder. The size of the stone was indicated as the largest diameter measured by computed tomography (CT). Skin to stone distance (SSD) was measured by a real-time ultrasound monitor when SWL was in process. The degree of hydronephrosis was assessed using a CT scan and was categorized as grade 0–4. The kidney without calix or pelvic dilatation was grade 0, those with pelvic dilation alone were grade 1, those with mild calix dilation were grade 2, those with severe calix dilation were grade 3, and those with calix dilation accompanied by renal parenchyma atrophy were grade 4. Stone density was measured by mean attenuation value (MAV) of computed tomography (CT) in Hounsfield units (the stone in the maximal diameter, where the elliptical region of interest incorporated the largest cross-sectional area of stone without including adjacent soft tissue).
Emergency SWL was defined as performed within 24 h of the onset of renal colic. The failure of emergency SWL was defined as no pain relief or recurrence (intermittent episodes of pain) within 1 month after the procedure or stone-free failure at 1 month SWL. The stone-free failure was defined as there was evidence of clinically significant stone fragments (≥ 4 mm) on a plain X-ray of urinary tract (KUB) and urinary ultrasound at 1 month after SWL. Cases converted to URS or PCNL after one session within 1 month were defined as failure too. Post-procedural follow-up visits were performed 1 month after SWL using both KUB and ultrasound.
Statistical analysis
Data were analyzed using IBM SPSS Statistics for Windows, version 22.0. (IBM Corporation), R software (version 3.0.1; https://www.r-project.org/), and STATA 15.0. (Stata Corp., College Station, TX, USA). In this investigation, R's 'rms' and 'glmnet' packages were employed. All of the stated statistical significance levels were two sided, and statistical significance was defined as a probability (P) value of less than 0.05.
The Kolmogorov–Smirnov test was used to assess if continuous variables were normal. Continuous variables with a normally distributed distribution were shown as the mean ± SD, whereas those without a normally distributed distribution were shown as the median (interquartile range). The Student’s t test for independent samples was used to compare the means of two continuously distributed normally distributed variables. To compare two continuous non-normally distributed variables, the Mann–Whitney U test was applied. In categorical variables, the number (percentage) is reported. The comparison of categorical variables was conducted using the Chi-squared and Fisher’s exact tests.
A predictive nomogram with regression coefficients was constructed using multivariate unconditional logistic regression analysis. With Akaike’s information criterion serving as the stop** criteria, the likelihood ratio test was used to apply the backward stepwise selection. This model’s effectiveness was evaluated in the independent validation cohort. The validation cohort was subjected to the logistic regression formula used in the development cohort, and the probability for each patient was determined using this method. The area under the receiver operating characteristic (AUROC) curve was used to estimate the model’s discriminating performance. In contrast to 1.0, which implies perfect discrimination, an AUROC of 0.5 showed no discrimination. The model’s calibration was evaluated using calibration plots, the unreliability test, and the Hosmer–Lemeshow (H–L) Chi-square statistic. A slope on the 45-degree line showed that the calibration was perfect. By measuring the net benefits at various threshold probabilities in the validation cohort, decision curve analysis was done to assess the model’s clinical applicability.
Results
Finally, 358 patients were included in the development cohort, and 129 were included in the validation cohort. The median age of patients in development was 51.0 years, and the validation cohort was 49.0 years. Most patients were male in either development (68.4%) or validation cohort (71.3%). The median BMI was 24.1 kg/m2 and 24.4 kg/m2 in the development and validation cohorts. There were 15.6% (56/358) and 14.0% (18/129) patients who suffered from stone-free failure after SWL in the development and validation cohort, respectively (Table 1).
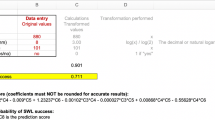
Compared with the stone-free success group, the patients who suffered from stone-free failure had a higher BMI (26.2 kg/m2 vs. 23.9 kg/m2, P = 0.068), larger stone size (13 mm vs. 9 mm, P < 0.001), higher stone density (674 Hu vs. 589 Hu, P < 0.001), larger SSD (98 mm vs. 78 mm, P < 0.001) (Table 2), higher grade of hydronephrosis (G3 or G4, 26.8% vs. 4.0%, P < 0.001) (Table 2). A predictive nomogram with regression coefficients was created using multivariate binary unconditional logistic regression. Backward stepwise selection was performed, and Akaike’s information criteria was used as the stop** rule for the likelihood ratio test using Akaike’s information test. The outcome was displayed in the final model (stone location, stone size, stone MAV, grade of hydronephrosis, and SSD). Based on these findings, we constructed a model to predict stone-free failure following SWL (Table 3 and Fig. 2).
Nomogram to predict stone-free failure after extracorporeal shockwave lithotripsy. Each clinicopathologic factor corresponds to a specific point by drawing a line straight upward to the points axis. After summing the points located on the total points axis, the sum represents the probability of stone-free failure after extracorporeal shockwave lithotripsy by drawing a line straight down to the risk axis. G grade, SSD skin to stone distance
By connecting a line directly upward to the point's axis, a particular point that represents each clinicopathologic feature is identified. By drawing a straight line down to the risk axis, the likelihood of a failure of stones is represented by the sum of the points on the total points axis. Consider a patient, for instance, who had the following characteristics: G1 hydronephrosis (0 points), SSD of 100 mm, stone density of 800 Hu, stone diameter of 10 mm (47 points), and so on (63 points). The patient was given a score of 137, and it was estimated that 30% of attempts to remove stones would fail. This estimated result can be utilized to make treatment plan decisions (Supplementary Fig. 1).
The cutoff value for risk probability in this model was 0.186, with a sensitivity of 83.9% and specificity of 88.4%. The AUROC values of the development and validation cohorts were 0.935 and 0.865, respectively (Fig. 3A, B and Table 3). With a P value of 0.678, the calibration invalidation unreliability test statistic was − 0.006. (Fig. 3C). With a P value of 0.059 and an H–L Chi-square statistic of 17.77, the calibration appeared to be accurate. The decision curve demonstrated that the cutoff value was included if the threshold probability for a patient varied from 0 to 90%. This nomogram performed better than either the “treat all” or “treat none” strategy in predicting stone-free failure after SWL. The net benefit was comparable within this range, (Fig. 3D).
Discussion
During the COVID-19 pandemic, emergency SWL is preferred for symptomatic ureteral stones as an ambulatory intervention [11, 13]. However, nearly half to one-third of patients suffered from failure after emergency SWL [6,7,8]; therefore, based on a large and prospective cohort study, we investigated the treatment outcome of emergency SWL guided by real-time ultrasound in patients with symptomatic ureteral stone, and identified four predictive factors including the stone size, stone density, SSD, and degree of hydronephrosis, and the results have also been validated externally.
As reported by previous studies, the failure incidence of emergency SWL is high in patients with ureteral stones [14,15,16,17]. Panah reported that the failure rate of emergency SWL is 26.8% (26/97) [6], while Ghalayini found that the failure rate was as high as 48% (52/108) [8]. However, in this study, the failure incidence after emergency SWL in the development and validation cohorts was 15.6% (56/358) and 14% (18/129), which is lower than the results of the previous study. The possible reason is that the process of SWL was guided by real-time ultrasound instead of intermittent X-ray, which is more accurate in location of the stone. On the other hand, this study also included patients with radiolucent stone, which is often characterized by lower stone density and more easily fragmented, thereby improving the treatment outcome of emergence SWL [18, 19].
Stone size has been previously reported as an independent risk factor for pain control and stone removal [6, 8]. Ghalayini et al. retrospectively assessed the efficacy of SWL for ureteral stones based on 108 patients with acute renal colic. About 52% (56) of the patients who underwent emergency SWL had totally fragmented stones were completely fragmentation. They believed that emergency SWL for obstructing ureteral stones has a satisfactory success rate, and stone size may be the main predictive factor for retreatment [8]. As a probable explanation, larger stone size is associated with more severe ureteral congestion, which might aggravate the degree of edema and increase the difficulty of lithotripter operation [20, 21].
Another predictor for emergency SWL involvement is the Hounsfield units of the stone density [7]. Kurkal et al. prospectively studied 86 patients with persistent renal colic to evaluate the efficacy and the predicting variables for successful early SWL [7]. In their study, the stone-free rate after the first emergency SWL session was 44.2%, and the predictor for both successful pain control and stone clearance was low stone density. From their perspective, emergency SWL effectively manages ureteral stones presented by renal colic with low HU, which is consistent with our study. As we know, stone density is an essential factor for clinicians to evaluate stone conditions. Moreover, the success of SWL depends on the efficacy of the lithotripter and the following factors, including the composition (hardness) of the stones according to the EAU Guidelines [5, 22, 23].
This study demonstrated that SSD is a predictor of the successful outcome after emergency SWL in ureteral stone. In line with this, Pareek et al. reported SSD might predict the outcome of patients after SWL with lower pole kidney stones [9]. In addition, Patel et al. conducted more comprehensive research; they retrospectively analyzed 83 patients to determine whether SSD independently predicted the SWL success regardless of stone location. In their study, 51 patients were stone free, 32 had residual stones, and SSD was the only independent predictor of treatment outcome via multivariate analysis [24].
Usually, patients with ureteral stones might have various degrees of hydronephrosis due to urinary obstruction. Ureteral obstruction results in decreased renal function and reduced ureteral peristalsis and pressure, ultimately affecting ureteral stone migration. Previous studies have reported that the possibility of ESWL treatment success decreases with more severe obstruction [25]. Consistent with this, El-Assmy et al. conducted a prospective randomized study to investigate the relation between the degree of stone-induced hydronephrosis and the outcome of SWL in 284 patients with lumbar ureteral stones, which found that the presence of hydronephrosis increases the retreatment rate. It prolongs the time to stone free [10].
There are still several limitations. First, it is an observational study from a single-center study. Second, this study had an external temporal validation, which tested a model from older data on newer data. Therefore, a multicenter cohort with standardization of the approach is required to validate this model. Lastly, the heterogenicity in ethnic characteristics between the Eastern and Western cohorts should be considered; thus, a Western cohort will need to be validated for the universal use of this model. Finally, this study’s results may apply only to patients treated during the COVID-19 pandemic. During this period, indications for treatment were changed in relation to the necessity to avoid hospitalization and procedures for anesthesia. Future studies with guideline indications are needed to confirm these results. Nevertheless, this is the first nomogram to predict the treatment outcome after emergency SWL based on a large prospective cohort. These findings assist in the decision-making strategy of guiding the treatment choice for symptomatic patients with ureteral stones; doctors and patients can make personalized predictions through this easy-to-use model during the COVID-19 pandemic.
Conclusion
In this large prospective cohort, we found that stone size, stone density, SSD, and degree of hydronephrosis were predictors of treatment outcome after emergency SWL. This nomogram will be helpful in preoperative risk stratification to provide individualized treatment recommendations for each patient. Furthermore, early identification and appropriate management of patients may increase the success rate of emergency SWL during the COVID-19 pandemic.
Data Availability
The datasets generated during the current study are available from the corresponding author on reasonable request.
References
Yuruk E, Tefekli A, Sari E, Karadag MA, Tepeler A, Binbay M, Muslumanoglu AY (2009) Does previous extracorporeal shock wave lithotripsy affect the performance and outcome of percutaneous nephrolithotomy? J Urol 181(2):663–667
de la Rosette J, Denstedt J, Geavlete P, Keeley F, Matsuda T, Pearle M, Preminger G, Traxer O, CROES URS Study Group (2014) The clinical research office of the endourological society ureteroscopy global study: indications, complications, and outcomes in 11,885 patients. J Endourol 28(2):131–139
Cornelius J, Zumbühl D, Afferi L, Mordasini L, Di Bona C, Zamboni S, Moschini M, Pozzi E, Salonia A, Mattei A, Danuser H, Baumeister P (2021) Immediate shockwave lithotripsy vs delayed shockwave lithotripsy after urgent ureteral stenting in patients with ureteral or pyeloureteral urolithiasis: a matched-pair analysis. J Endourol 35(5):721–727
Türk C, Petřík A, Sarica K, Seitz C, Skolarikos A, Straub M, Knoll T (2016) EAU guidelines on interventional treatment for urolithiasis. Eur Urol 69(3):475–482
Bucci S, Umari P, Rizzo M, Pavan N, Liguori G, Barbone F, Trombetta C (2018) Emergency extracorporeal shockwave lithotripsy as opposed to delayed shockwave lithotripsy for the treatment of acute renal colic due to obstructive ureteral stone: a prospective randomized trial. Minerva Urol Nefrol 70(5):526–533
Panah A, Patel S, Bourdoumis A, Kachrilas S, Buchholz N, Masood J (2013) Factors predicting success of emergency extracorporeal shockwave lithotripsy (eSWL) in ureteric calculi–a single centre experience from the United Kingdom (UK). Urolithiasis 41(5):437–441
Kurkar A, Elderwy AA, Osman MM, Abdelkawi IF, Shalaby MM, Abdelhafez MF (2022) Predictors of successful emergency shock wave lithotripsy for acute renal colic. Urolithiasis 50(4):481–485
Ghalayini IF, Al-Ghazo MA, Khader YS (2008) Evaluation of emergency extracorporeal shock wave lithotripsy for obstructing ureteral stones. Int Braz J Urol 34(4):433–440
Pareek G, Hedican SP, Lee FT Jr, Nakada SY (2005) Shock wave lithotripsy success determined by skin-to-stone distance on computed tomography. Urology 66(5):941–944
El-Assmy A, El-Nahas AR, Youssef RF, El-Hefnawy AS, Sheir KZ (2007) Impact of the degree of hydronephrosis on the efficacy of in situ extracorporeal shock-wave lithotripsy for proximal ureteral calculi. Scand J Urol Nephrol 41(3):208–213
Shivakumar N, Nantha Kumar D, Joshi H (2022) The impact of early COVID-19 pandemic on the presentation and management of urinary calculi across the globe: a systematic review. J Endourol 36(9):1255–1264
Bai S, Wu B, Yao Z, Zhu X, Jiang Y, Wang H (2020) Development and validation of a clinical model to predict intraoperative hemodynamic instability in patients with pheochromocytomas surgery. Endocr J 67(1):81–89
Hiller SC, Dauw CA, Ghani KR (2020) Kidney stone care and the COVID-19 pandemic: challenges and opportunities. J Urol 204(6):1122–1124
Seitz C, Fajkovi H, Remzi M, Waldert M, Ozsoy M, Kramer G, Marberger M (2006) Rapid extracorporeal shock wave lithotripsy treatment after a first colic episode correlates with accelerated ureteral stone clearance. Eur Urol 49(6):1099–1105
Eisner BH, Reese A, Sheth S, Stoller ML (2009) Ureteral stone location at emergency room presentation with colic. J Urol 182(1):165–168
Dasgupta R, Hegarty N, Thomas K (2009) Emergency shock wave lithotripsy for ureteric stones. Curr Opin Urol 19(2):196–199
Kravchick S, Bunkin I, Stepnov E, Peled R, Agulansky L, Cytron S (2005) Emergency extracorporeal shockwave lithotripsy for acute renal colic caused by upper urinary tract stones. J Endourol 19(1):1–4
Kumar A, Mohanty NK, Jain M, Prakash S, Arora RP (2010) A prospective randomized comparison between early (< 48 hours of onset of colicky pain) versus delayed shockwave lithotripsy for symptomatic upper ureteral calculi: a single center experience. J Endourol 24(12):2059–2066
Zhang LW, Fei X, Song Y (2021) The clinical efficacy of novel vacuum suction ureteroscopic lithotripsy in the treatment of upper ureteral calculi. World J Urol 39(11):4261–4265
Park J, Suh B, Lee MS, Woo SH, Shin DW (2016) National practice pattern and time trends in treatment of upper urinary tract calculi in Korea: a nationwide population-based study. J Korean Med Sci 31(12):1989–1995
Tombal B, Mawlawi H, Feyaerts A, Wese FX, Opsomer R, Van Cangh PJ (2005) Prospective randomized evaluation of emergency extracorporeal shock wave lithotripsy (SWL) on the short-time outcome of symptomatic ureteral stones. Eur Urol 47(6):855–859
Arcaniolo D, De Sio M, Rassweiler J, Nicholas J, Lima E, Carrieri G, Liatsikos E, Mirone V, Monga M, Autorino R (2017) Emergent versus delayed lithotripsy for obstructing ureteral stones: a cumulative analysis of comparative studies. Urolithiasis 45(6):563–572
Smith-Bindman R, Moghadassi M, Griffey RT, Camargo CA Jr, Bailitz J, Beland M, Miglioretti DL (2015) Computed tomography radiation dose in patients with suspected urolithiasis. JAMA Intern Med 175(8):1413–1416
Patel T, Kozakowski K, Hruby G, Gupta M (2009) Skin to stone distance is an independent predictor of stone-free status following shockwave lithotripsy. J Endourol 23(9):1383–1385
Delakas D, Karyotis I, Daskalopoulos G, Lianos E, Mavromanolakis E (2003) Independent predictors of failure of shockwave lithotripsy for ureteral stones employing a second-generation lithotripter. J Endourol 17(4):201–205
Acknowledgements
We thank International Science Editing (http://www.internationalscienceediting.com) for editing this manuscript. The authors would like to thank all of the study participants. We give special thanks to all the colleagues at the Department of Urology of Sheng**g Hospital for their help and support.
Funding
This study was financially supported by Natural Science Foundation of Liaoning Education Department (QN2019013), Natural Science Foundation of Liaoning Science and Technology Department (2020-BS-093), and the 345 Talent Project of Sheng**g Hospital.
Author information
Authors and Affiliations
Contributions
SB and ZL had full access to all the data in the study and take responsibility for the integrity of the data and the accuracy of the data analysis. SB and ZL: protocol/project development. LZ, JL, CP, YZ, ZL, and SB: data collection or management. LZ, ZL, and SB: data analysis. LZ, ZL, and SB: manuscript writing/editing.
Corresponding authors
Ethics declarations
Conflict of interest
Song Bai certifies that all conflicts of interest, including specific financial interests and relationships and affiliations relevant to the subject matter or materials discussed in the manuscript (e.g., employment/affiliation, grants or funding, consultancies, honoraria, stock ownership or options, expert testimony, royalties, or patents filed, received, or pending), are none.
Ethical approval
Ethical approval (2020PS520K) was provided by the Institutional Research and Ethics Committee of the Sheng**g Hospital Affiliated China Medical University. Informed consent was obtained from all eligible subjects. The clinical research registry UIN is ChiCTR2000033789. The study protocol conformed to the ethical guidelines of the 1975 Declaration of Helsinki.
Consent for publication
Informed consent from all eligible patients was obtained.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
240_2022_1401_MOESM1_ESM.tif
Supplementary file1 (TIF 346 KB) Example of nomogram to predict stone-free failure after extracorporeal shockwave lithotripsy. Abbreviations: G, grade; SSD, skin stone distance.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Zhang, L., Li, J., Pan, C. et al. Development and validation of a predictive model for treatment outcome after emergency extracorporeal shockwave lithotripsy in patients with symptomatic ureteral stones during the COVID-19 pandemic: in a large prospective cohort. Urolithiasis 51, 26 (2023). https://doi.org/10.1007/s00240-022-01401-7
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s00240-022-01401-7