Abstract
Rationale
Dopamine antagonists induce dopamine receptor supersensitivity. This may manifest in late-appearing movement disorders (tardive dyskinesia (TD). VMAT-2 inhibitors reduce dopaminergic transmission but have limited activity at postsynaptic receptors and so may have antipsychotic activity with lower risk of tardive dyskinesia.
Methods
We conducted a systematic database search from inception to September 2022 for articles describing the use of VMAT-2 inhibitors in psychosis. Inclusion criteria were as follows: Population: adults diagnosed with psychosis or schizophrenia; Intervention: treatment with tetrabenazine, deutetrabenazine or valbenazine; Comparison: comparison with placebo or/and antipsychotic drug; Outcomes: with efficacy outcomes (e.g. Brief Psychiatric Rating Scale (BPRS) change or clinician assessment) and adverse effects ratings (e.g. rating scale or clinician assessment or dropouts); and Studies: in randomised controlled trials and non-randomised studies.
Results
We identified 4892 records relating to VMAT-2 inhibitor use of which 5 (173 participants) met our a priori meta-analysis inclusion criteria. VMAT-2 inhibitors were more effective than placebo for the outcome ‘slight improvement’ (risk ratio (RR) = 1.77 (95% CI 1.03, 3.04)) but not for ‘moderate improvement’ (RR 2.81 (95% CI 0.27, 29.17). VMAT-2 inhibitors were as effective as active comparators on both measures for—‘slight improvement’ (RR 1.05 (95% CI 0.6, 1.81)) and ‘moderate improvement’ (RR 1.11 (95% CI 0.51, 2.42). Antipsychotic efficacy was also suggested by a narrative review of 37 studies excluded from the meta-analysis.
Conclusions
VMAT-2 inhibitors may have antipsychotic activity and may offer promise for treatment of psychosis with the potential for a reduced risk of TD.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
It is accepted that the symptoms of schizophrenia are at least in part caused by abnormalities in neuronal dopamine function. The core dysfunction appears to be an increase in presynaptic synthesis and release of striatal dopamine (DA) (Howes et al. 2017). Most currently available antipsychotics block postsynaptic dopamine 2 (D2) receptors (pimavanserin is the sole exception (Rissardo et al. 2022)) but do not significantly alter dopamine synthesis capacity at contemporary therapeutic doses (Jauhar et al. 2019). D2 antagonism may induce sensitivity of postsynaptic dopamine receptors (Chouinard et al. 1978; Fallon et al. 2012), and cessation of D2 antagonists may then expose the patient to the effects of both the inherent elevated DA synthesis and supersensitive postsynaptic D2 receptors. This drug-induced sensitivity and the absence of effect on the core pathological mechanism help explain the very high risks of relapse after stop** antipsychotics (90% at 2 years after a first episode) (Zipursky et al. 2014).
There are several potential pharmacological methods of countering increased synthesis of dopamine. These include directly decreasing synthesis, reducing intracellular transport, inhibiting vesicular storage, stimulating pre-synaptic (negative feedback) receptors and blocking post-synaptic receptors. Of these methods, only post-synaptic D2 antagonism is used clinically (although pre-synaptic blockade may also contribute via depolarization block) (Grace et al. 1997). However, there are licensed compounds available which affect vesicular monoamine uptake. Deutetrabenazine, tetrabenazine and valbenazine deplete vesicular storage of dopamine (as well as serotonin, noradrenaline and histamine) in presynaptic nerve terminals by reversibly inhibiting human vesicular monoamine transporter isoform 2 (VMAT-2 inhibitors). This inhibition results in a reduced inclusion of monoamines into synaptic vesicles, a corresponding depletion of functional monoamine stores and ultimately a reduction in neurotransmitter release. The three available VMAT-2 inhibitors have a broadly similar mode of action. Most is known about tetrabenazine—a drug that is more than 60 years old. Tetrabenazine preferentially depletes dopamine over serotonin and noradrenaline whilst also modestly reducing levels of acetylcholine, glutamate and aspartate (Stahl 2018b; Zheng et al. 2006).
VMAT-2 inhibitors do not appear to induce postsynaptic DA supersensitivity. Indeed, VMAT-2 inhibitors are used to treat tardive dyskinesia (TD)—a condition caused by chronic dopamine receptor blockade and a presumed consequent upregulation of D2 receptors and altered synaptic plasticity. Moreover, by reducing presynaptic dopamine storage and thus the amount released into the synaptic cleft, VMAT-2 inhibitors act more directly against excess stimulation of hypersensitive D1 and D2 receptors, the proposed pathological basis of TD.
VMAT-2 inhibitors are licensed only for the treatment of TD but tetrabenazine was at one time indicated as an antipsychotic. These drugs may offer the prospect of improved outcome in long-term treatment of psychosis; they may reduce the severity of psychotic symptoms but with a more limited effect on postsynaptic DA receptor sensitivity. We undertook a systematic review of studies of VMAT-2 inhibitors in people with psychosis and similar conditions.
Method
Meta-analysis
Study selection
A priori selection parameters
The criteria for inclusion in this review were as described in the following pre-defined PICOS tool. Population: adults (minimum of 18 years old, including older adults aged more than 65 years old) who were diagnosed with psychosis or schizophrenia (or broad equivalent in older studies). The diagnostic method was not restricted in any way. Intervention: treatment with dopamine synthesis inhibitors: tetrabenazine, deutetrabenazine or valbenazine. Any route of administration, dose, duration and co-intervention treatment was eligible. Comparison: placebo or/and antipsychotic drug. Outcomes: efficacy (e.g. Brief Psychiatric Rating Scale (BPRS) change or clinician assessment) and adverse effects (e.g. rating scale or clinician assessment or dropouts). Studies: randomised controlled trials and non-randomised studies.
Studies that did not meet the criteria listed above were examined for inclusion in a narrative review.
Search methods for identification of studies
The following databases were searched: EMBASE, EMBASE Classic, MEDLINE, PsycINFO, Psychiatry Online, PubMed and Web of Science. We also included all the citations from the top 10% of references in the Web of Science search.
All the databases (except PubMed) were searched from inception until November 2020 using the keyword terms below. Search terms were adapted to the thesaurus of each database.
Boolean operator | Search term |
OR | schizo* “dementia praecox” psychos?s psychotic |
AND | |
OR | valbenazine deutetrabenazine tetrabenazine “dopamine synthesis inhibitor*” “vesicular monoamine transport inhibitor*” |
These databases including PubMed were also searched for a second time using the terms ‘Nitoman’ and ‘R1-9569’ from inception until May 2021. This entire search was repeated for the last time in September 2022.
Medical Subject Headings (MeSH) terms were used where available; otherwise, free-text searching was used. Studies were limited to humans, and there were no restrictions in respect to language. Google Translate and native speakers were used to translate non-English language studies.
The reference sections of all studies retrieved were also searched for relevant studies.
Data collection and analysis
Selection of studies
Three authors (DT, AC and PW) screened study abstracts and titles and retrieved potentially relevant complete text papers for detailed examination. Disagreements about inclusion were resolved by discussion with a fourth author (OD).
Data collection and management
Two authors (AC and PW) extracted study data independently, and disagreements between the two were resolved by discussion with a third author (OD). For studies where relevant data were not available, the study authors were contacted via email. The following study characteristics were extracted for the meta-analysis section of this investigation: year of publication, country of origin, study design, main diagnosis, duration of treatment, number of participants (total, responders, remitters, dropouts for intervention and comparator), age range of participants, care setting, sex, intervention, comparator and outcome measure (baseline scores (SD) and endpoint score (SD) for intervention and comparator). Study-defined psychosis rating scale scores were extracted to determine response to treatment. Response was categorised as ‘slight improvement’ and ‘moderate improvement’, corresponding to Clinical Global Impressions Improvement Scale (CGI-I) scores 3 (minimally improved) and 2 (much improved), respectively. For example, ‘definite improvement’, ‘significant improvement’ or ‘marked improvement’ were categorised as CGI-I 2 and ‘slight improvement/response’ as CGI-I 3 (See supplementary Table S2).
Study authors were contacted to obtain missing information or to clarify the information available (AC).
Assessment of risk of bias in included studies
The Cochrane risk of bias tool (version 2) (Sterne et al. 2019) was completed independently by two authors (AC and PW), with disagreements resolved by a third author (OD). The assessment of the risk-of-bias was incorporated into the interpretation of the results.
Dealing with missing data and assessment of reporting biases
The impact of missing data in individual studies was explored by imputing missing values with reported reasons for their ‘missingness’ and synthesising these using STATA’s METAMISS command (White and Higgins 2007).
Assessment of heterogeneity
The presence and extent of heterogeneity were explored by visual inspection of forest plots and quantified using the I2 statistic. Funnel plots were constructed where possible to assess for missing studies.
Data synthesis, measures of treatment effect and unit of analysis issues
We performed a random-effects model using Der Simonian and Laird weights to synthesise results. We used risk ratios as the effect measure of interest with corresponding 95% confidence intervals and displayed results using forest plots. Separate analyses were conducted for those achieving at least slight or moderate improvement in psychotic symptoms. Crossover studies were assessed for evidence of carryover effects. If carryover effects were not present, then both periods were covered; otherwise, studies were analysed as parallel studies by using results only from the first period. When both periods from a crossover study were included, Becker–Balagtas estimates were computed and combined with odds ratios from parallel studies (Stedman et al. 2011). Meta-analysis and forest plots were conducted on Revman V 5.4 (Collaboration. 2020).
Sensitivity analyses
We performed different sensitivity analyses to assess robustness of the primary methods by varying analysis by effect size, model type, crossover study periods and missing observation imputation.
Narrative review
Post hoc, we decided to provide a narrative review of informative reports which did not meet inclusion criteria for the meta-analysis. We included in this review any report of the use of any VMAT-2 inhibitor in at least one person with a diagnosis of schizophrenia or psychosis (or any accepted symptom of psychosis) and where any evaluation of psychosis symptom severity was made.
Results
Meta-analysis
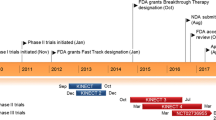
The results of the search and selection process of studies are described in the PRISMA flow diagram (Fig. 1). The search identified 4892 records of which five met the inclusion criteria of our pre-defined PICOS. The characteristics of included studies are shown in Table 1. Included studies were from Europe and North America and spanned a 52-year period. Only tetrabenazine studies were included in the meta-analysis as these were the only VMAT-2 inhibitor studies that fitted our inclusion criteria.
There was a total of 173 participants (before dropouts) allocated to tetrabenazine, active comparator or placebo in the included studies. Four of the studies (108 participants) used placebo as a comparator and two (76 participants) used active comparators (chlorpromazine or reserpine). One of these studies (Remington et al. 2012) used tetrabenazine or placebo augmentation of clozapine (or other antipsychotics) whilst another (Smith 1960) used both an active (reserpine) and a placebo comparator. Study responder categorisation by CGI-I score is described in the method and in detail in Supplementary Table S2. No data were available on numbers of patients achieving remission. Dropouts were reported for two of the placebo comparison studies and one of the active studies; the total number of dropouts was 23.
Study characteristics of included studies
See Table 1.
Synthesis
Clinical outcomes were divided into two categories, slight improvement and moderate improvement, as described. For VMAT-2 inhibitors versus placebo (see Figs. 2 and 3), there was a statistically significant advantage for the clinical outcome slight improvement (4 studies, 103 participants) (risk ratio (RR) 1.77 (95% CI 1.03, 3.04) but no advantage for the clinical outcome moderate improvement (RR) 5.00 (95% CI 0.27, 95.33). Both syntheses had no statistical heterogeneity (I2 = 0%). Sixty-eight participants (31 VMAT-2 inhibitors, 37 active comparators) were included in analysis comparing VMAT-2 inhibitors with an active comparator (see Figs. 4 and 5). For VMAT-2 inhibitors versus active comparator, see Figs. 4 and 5. There was no statistically significant difference for the clinical outcome ‘slight improvement’ (RR 1.05 (95% CI 0.6, 1.81)) or ‘moderate improvement’ (RR 1.11 (95% CI 0.51, 2.42). Both syntheses had no statistical heterogeneity (I2 = 0%).
Sensitivity analyses were performed by repeating the analyses with imputed missing outcome data, OR as effect size measure and inclusion of both periods in the crossover study (Figures S1, S2). Results of all sensitivity analyses were not significantly different to the original analyses except for inclusion of both periods of the crossover study which resulted in slightly larger effect (OR 3.45; 95% CI 1.16, 8.47) compared with analysis from the first period only (OR 2.45 95% CI 1.03, 5.87). The direction of effects did not change in any of the analyses (see figure S2).
We could not assess for publication bias visually using funnel plots because of the small number of studies included.
VMAT-2 inhibitors versus placebo
See Fig. 2
VMAT-2 inhibitors versus active comparator
See Fig. 4
Risk of bias
The Cochrane risk-of-bias assessments are summarised in Tables 2 and 3. One study was assessed as being at a low risk of bias; three had some concerns, and one had a high risk of bias (elaboration of these concerns are detailed in Table S3). No studies were excluded by risk-of-bias.
Synthesis studies—adverse events
Adverse effects reported in studies included in the systematic review are described in Tables 4 and 5.
Narrative review studies excluded from the meta-analysis
We identified 37 studies which did not meet our pre-defined criteria for inclusion in the meta-analysis but were considered informative. Our inclusion criteria were as described in the ‘Methods’ section. These studies were published over a period of 64 years (1958–2022). Tardive dyskinesia was co-existent with schizophrenia in seven of the 37 studies (Hauser et al. 2017; Josiassen et al. 2017; Kalian et al. 1993; Khurram et al. 2021; Lindenmayer et al. 2022; Lindenmayer et al. 2017; Lindenmayer et al. 2019); seven studies were placebo-controlled (Ashcroft et al. 1961; Hauser et al. 2017; Lindenmayer et al. 2017; Lingjaerde 1963; Remington et al. 2012; Smith 1960; Weckowicz et al. 1960). One study substituted reserpine (Brauchitsch) as a means of comparison. Treatment duration for tetrabenazine ranged from 2 days to 22 months and daily doses from 10 to 600mg (most were in the range 100–200mg/day) and for valbenazine from 3 to 48 weeks, at 25 to 80mg/day.
For many studies involving tetrabenazine (Table 6), it was somewhat unclear what prior or concurrent treatment had been or was given. Treatments reported as being prescribed before or alongside tetrabenazine included antipsychotics, reserpine, ECT, iproniazid, imipramine, barbiturates, promethazine, insulin, lobotomy and ‘special drug therapy’. ECT was employed as concurrent co-therapy in at least three studies (Lustig 1961; Shimizu et al. 1962; Voelkel and Dressler 1959). Two reports explicitly excluded the co-prescription of all other treatments (Borenstein et al. 1961; Heinze 1960).
Observations from these studies of tetrabenazine, most of which did not employ a contemporary comparator, suggested some antipsychotic action—most patients improved to some extent. In patients with schizophrenia or psychosis, tetrabenazine was moderately or greatly effective in, broadly speaking, three quarters of those treated. In one report, tetrabenazine was ineffective (Borenstein et al. 1961), and there was uncertain efficacy in a further four studies (Kammerer et al. 1962; Singer 1961; Stockhausen 1960c; Voelkel 1958).
Symptoms reported to have responded well included aggression and violence, negativity, restlessness, paranoia, delusions and hallucinosis. Conversely, autism, apathy, insomnia and lack of insight appear to have responded relatively less well. In the study in which some of the tetrabenazine-treated patients were switched to placebo (Brauchitsch), 14 of 23 relapsed after switching.
The most commonly reported adverse effects of tetrabenazine were parkinsonism (tremor, dystonia, akathisia/restlessness) and hypotension, both of which were noted to be dose-related. Depression was specifically mentioned as being observed in two studies and dysphoria (as part of ‘tetrabenazine malaise’ syndrome) in one. Suicidal ideation was not mentioned in any report. Gastrointestinal effects such as nausea (with resulting anorexia), vomiting, diarrhoea and constipation were commonly reported. Somnolence was also usually seen. Other reported adverse effects included insomnia and sleep disturbance. One study described the (apparently then well-known phenomenon) of ‘tetrabenazine malaise’—a syndrome consisting of dysphoria, irritability, fatigue and lethargy. More than one study reported the occurrence of ‘neuroleptic syndrome’ but without further clarification or description. Weight gain was reported in some studies. Many trials reported the occurrence of either dry mouth or hypersalivation, some tachycardia and some bradycardia.
The extent of participant withdrawal from treatment because of adverse effects was not described in most studies. Completion rates were generally very high when reported, but, given the age of most of the studies, it is likely possible that participants had little choice but to continue even when there was poor tolerability. Indeed, whilst most patients received oral medication, some studies administered tetrabenazine covertly or parenterally in those patients who refused treatment.
The six most recent studies examined the use of valbenazine in participants with both tardive dyskinesia and schizophrenia, but in each of these, the intention was to test efficacy in reducing the severity of TD (Table 7). The subjects included were chronically, but not acutely unwell and schizophrenia symptom severity change was not anticipated. Valbenazine was added to on-going antipsychotic treatment in five of these studies (Hauser et al. 2017; Josiassen et al. 2017; Khurram et al. 2021; Lindenmayer et al. 2017; Lindenmayer et al. 2019). Symptom ratings suggested that participants’ psychiatric illness remained stable during valbenazine treatment with negligible, albeit favourable, changes in PANSS scores that were not statistically different from those with placebo. There was no evidence from these trials that valbenazine had any worthwhile antipsychotic activity when added to existing antipsychotic treatment. However, this was not the objective of these studies; rather, they were safety studies designed in part to assess any potential detrimental adverse effects on participants’ mental state. Two recent case studies described apparent antipsychotic effects of valbenazine in treatment-resistant schizophrenia with TD: one for a patient not taking an antipsychotic (Lindenmayer et al. 2022) and the other taking clozapine (Khurram et al. 2021).
Valbenazine adverse effects in studies included in this review included somnolence, akathisia, dry mouth, urinary tract infection and headache, also arthralgia, headache, vomiting, anxiety, insomnia, fatigue, urinary tract infection and weight gain. Data on suicidal ideation differed—one study recorded lower rates than with placebo whilst another found the converse effect (possibly explained in this latter study by a higher baseline level in the valbenazine group).
Studies of the effect of deutetrabenazine in TD (Anderson et al. 2017; Fernandez et al. 2017) examined mixed populations of individuals, only some of whom had psychotic illness. The effect of deutetrabenazine on psychotic symptoms was not formally evaluated. Adverse effect incidence did not differ from placebo.
Discussion
This meta-analysis tentatively suggests tetrabenazine has some antipsychotic efficacy, although its relative efficacy compared with dopamine antagonists could not be determined. Our narrative review (albeit of studies of dubious quality) also suggests that VMAT-2 inhibitors are effective as antipsychotics. The major obstacle in clarifying the exact utility of VMAT-2 inhibitors in psychosis is the near absence of trials which meet today’s methodological standards. The number of studies meeting our inclusion criteria was small, and the power to reveal differences between treatments was correspondingly low. In the narrative review, study quality was poor with limited or confused description of trial design, little or no description of blinding, no or limited statistical analysis and widespread use of unvalidated rating scales and other assessments. Although valbenazine and deutetrabenazine have been evaluated in modern, well-conducted studies, these were studies of the treatment of tardive dyskinesia in patients with stable schizophrenia, rather than of their effect on schizophrenia per se. Changes in diagnostic criteria over the last 60 or so years also hamper the drawing of clear conclusions.
Our synthesis found low rates of study heterogeneity. This is likely to be because of the small numbers of studies with similar effects sizes included in the meta-analysis. This result is a reflection, in some case, of the poor quality and reporting of the studies especially as four of the five studies included in the meta-analysis synthesis were from over 60 years ago. Grading of recommendations assessment, development and evaluation (GRADE) of the quality of evidence and strength of recommendation for the clinical outcome of tetrabenazine in schizophrenia and psychosis were informally assessed. For the assessment of quality of evidence for placebo-controlled studies slight or moderate improvement outcomes, two of the studies included in the meta-analysis were controlled trials although the randomisation was generally of poor quality and two studies were not randomised, risk of bias had some or high concerns, studies were relatively consistent versus placebo, participants were from a large range of ages and from a mostly inpatient population (apart from the study of Remington et al. (2012) which was conducted in outpatients), confidence intervals were wide or very wide for the placebo analyses indicating some imprecision, and formal analysis of publication bias was not possible given the small number of studies. Lastly, the inclusion of the study by Remington et al. may well diminish our effect size estimate as participants were largely resistant to standard treatments, including clozapine, and so were perhaps less likely to respond to VMAT-2 inhibitors.
The quality of evidence for this intervention, after examining the body of evidence, is low. The strength of recommendation is weak because the difference between desirable and undesirable effects is difficult to determine given the lack of formal assessment of adverse effects for most studies; the quality of evidence is low; and, at current rates, medication costs are higher overall for tetrabenazine than for standard treatment with second generation antipsychotics (National Institute for Health and Care Excellence 2023).
Adverse effects reported for tetrabenazine in included clinical trials as ‘very common’ were sedation, somnolence, parkinsonism and depression, whilst ‘common’ side effects were akathisia, anxiety and insomnia (Niemann and Jankovic 2019). Other adverse effects reported included dysphagia, hyperprolactinaemia and psychotic exacerbation (Solmi et al. 2018). Deutetrabenazine is probably better tolerated than tetrabenazine; adverse effects of deutetrabenazine, except for insomnia, are seen at a similar frequency to placebo (Niemann and Jankovic 2019; Solmi et al. 2018). Valbenazine appears well tolerated with patient completion rates in clinical trials similar to placebo (Solmi et al. 2018). It can commonly cause somnolence, headache, fatigue, dry mouth, vomiting and akathisia (Niemann and Jankovic 2019). Psychiatric side effects such as depression and suicidality have not been observed as being more common than with placebo in short- and longer-term clinical trials of patients with a stable mental state (Solmi et al. 2018). All VMAT-2 inhibitors are associated with QTc prolongation (Niemann and Jankovic 2019; Solmi et al. 2018). Tetrabenazine, at a dose of 50mg, prolongs QTc by an average of 8 milliseconds (AOP Orphan Ltd. 2020), deutetrabenazine (at 24mg) by 4.5 milliseconds (Teva Pharmaceuticals USA 2017) and valbenazine (at 80mg) by 2.1 milliseconds (Thai-Cuarto et al. 2018).
There are several limitations to note. The age of many of the studies examined means that we cannot be certain of outcomes (scales used were outdated, varied and numerous), diagnosis (little detail given; diagnostic criteria have long since changed) or even the morality of the studies (few details on patient consent provided). Even in our meta-analysis, we were forced to invent new somewhat subjective categories of response to account for the varied assessments used, and this inevitably affected our ability to interpret outcomes. In many studies, it is likely that participants were treatment-resistant, and this too affected outcome interpretation. Lastly, the vast majority of studies of psychosis used tetrabenazine, and findings from those studies may not generalise to deutetrabenazine or valbenazine.
Our analysis might have been improved by the inclusion of studies of reserpine (another VMAT inhibitor), or at least the number of studies available for inclusion might have increased. However, we had concluded a priori that reserpine lacked the close similarity in mode of action shared by the three VMAT inhibitors ultimately included. Reserpine is an irreversible inhibitor of VMAT-1 and VMAT-2 both centrally and peripherally and so is likely to have a different efficacy and tolerability profile.
None of these drugs is currently licensed for psychosis. Tetrabenazine is licensed in the EU for the treatment of ‘movement disorders due to Huntington’s chorea, hemiballismus, senile chorea, and related neurological conditions’ (AOP Orphan Ltd. 2020). It is not licensed in the EU for the treatment of schizophrenia even though it was initially developed as an antipsychotic agent (Schreiber et al. 1999) and, as this review shows, improves symptoms of psychosis. In the USA, deutetrabenazine is approved for chorea associated with Huntington’s disease and valbenazine for the treatment of TD. It is perhaps relevant to note that VMAT-2 inhibitors are not drugs of choice for psychosis in Huntington’s disease (Anderson et al. 2018).
The question that remains concerns the potential for VMAT-2 inhibitors to treat psychosis with a lower the risk of tardive dyskinesia and without the risk of inducing post-synaptic receptor supersensitivity. VMAT-2 inhibitors appear to be effective antipsychotics and, given that they are used to treat TD, we might assume that they are unlikely to cause this condition (although DA antagonists also ‘treat’ (mask) TD if the dose of DA antagonist is increased (Glazer and Hafez 1990)). Likewise, we might assume that, having little or no interaction with post-synaptic receptors, VMAT-2 inhibitors are unlikely to sensitise or upregulate these receptors. However, denervation of pre-synaptic dopamine neurones does induce postsynaptic supersensitivity (Kostrzewa and Brus 2016; Mandel et al. 1993). In addition to this, some VMAT-2 inhibitors do in fact have weak antagonist activity at post-synaptic dopamine receptors. Animal studies show that tetrabenazine can displace the D2 ligand at 3H-spiperone (Login et al. 1982), and severe dystonic reactions to high dose tetrabenazine are thought to be caused by dopamine receptor antagonism (Burke et al. 1985). Deutetrabenazine and valbenazine have little or no affinity for D2 receptors (Stahl 2018a), although a metabolite of deutetrabenazine ([-]-α-deuterated dihydrotetrabenazine) has moderate activity at D2 and D3 receptors (Brar et al. 2023). This antagonist activity at dopamine receptors may explain the very occasional cases of tardive dyskinesia reported in long-term tetrabenazine use (we could find only two in the literature) (LeWitt 2013; Palermo et al. 2020). The overall risk of TD is probably minimal: a long-term study of 448 people taking tetrabenazine for a range of movement disorders reported no cases of TD (Kenney et al. 2007). Reserpine, too, is only very rarely causatively linked to TD (Uhrbrand and Faurbye 1960). Neither valbenazine nor deutetrabenazine have been associated with emergent TD.
We do not know the optimal dose of any VMAT-2 inhibitor in treating psychosis, and we can therefore not be clear about the adverse effect burden of these drugs at that so far ill-defined dose. The dose-related nature of adverse effects offers the possibility of discovering doses that are both well tolerated and effective in psychosis.
We conclude that VMAT-2 inhibition deserves further scrutiny as a potential method for achieving antipsychotic efficacy with a potential for reduced risk of TD or dopamine receptor supersensitivity. Ultimately, however, there are insufficient data to unequivocally support or refute the efficacy and safety of VMAT-2 inhibitors to treat psychosis compared with placebo or active comparators, especially newer antipsychotics. Rigorous controlled trials which meet modern clinical trials standards are needed to answer this question definitively. Whether or not such trials are conducted may depend on the clinical utility of emerging non-DA antagonist antipsychotics (Tsapakis et al. 2023) and risk of TD associated with their long-term use.
References
Anderson KE, Stamler D, Davis MD, Factor SA, Hauser RA, Isojärvi J, Jarskog LF, Jimenez-Shahed J, Kumar R, McEvoy JP, Ochudlo S, Ondo WG, Fernandez HH (2017) Deutetrabenazine for treatment of involuntary movements in patients with tardive dyskinesia (AIM-TD): a double-blind, randomised, placebo-controlled, phase 3 trial. Lancet Psychiatry 4:595–604
Anderson KE, van Duijn E, Craufurd D, Drazinic C, Edmondson M, Goodman N, van Kammen D, Loy C, Priller J, Goodman LV (2018) Clinical management of neuropsychiatric symptoms of huntington disease: expert-based consensus guidelines on agitation, anxiety, apathy, psychosis and sleep disorders. J Huntingt disease 7:355–366
AOP Orphan Ltd. (2020) Summary of product characteristics Tetrabenazine 25mg tablets, https://www.medicines.org.uk/emc/product/8961/smpc
Ashcroft GW, Macdougall EJ, Barker PA (1961) A comparison of tetrabenazine and chlorpromazine in chronic schizophrenia. J Ment Sci 107:287–293
Bertolotti P, Munarini D (1961) Therapeutic experiences in neuropsychiatry with a benzoquinolizine derivative (Ro 1-9569). Riv Sper Freniatr Med Leg Alien Ment 85:185–193
Borenstein P, Dabbah M, Kramarz P, Bles G (1961) Clinical biological and electroencephalographic study of tetrabenazine. Ann Med Psychol (Paris) 119(2):764–773
Brar S, Vijan A, Scott FL, Jimenez R, Zhang H, Grigoriadis DE, Loewen G (2023) Pharmacokinetic and pharmacologic characterization of the dihydrotetrabenazine isomers of deutetrabenazine and valbenazine. Clin Pharmacol Drug Dev 12:447–456
Brauchitsch H (n.d.) Untersuchung uber die klinische Wirkung des Tetrabenazin.
Burckard E, Medhaoui M, Montigneaux P, Pfitzenmeyer J, Pfitzenmeyer H, Schaetzel JC, Singer L, Geissmann P (1962) Clinical, biological and electroencephalographic study of the action of tetrabenazine (Ro 956) in various chronic psychoses. Ann Med Psychol (Paris) 120(1):115–119
Burke RE, Reches A, Traub MM, Ilson J, Swash M, Fahn S (1985) Tetrabenazine induces acute dystonic reactions. Ann Neurol 17:200–202
Chouinard G, Jones BD, Annable L (1978) Neuroleptic-induced supersensitivity psychosis. Am J Psychiatry 135:1409–1410
Collaboration. TC (2020) Review Manager (RevMan) [Computer program] Version, vol 5, p 4
Cwynar S, Rydzynski Z, Siuchninska H (1962) Our experience with the use of Nitoman in mental disorders. Pol Tyg Lek 17:633–635
Espinosa J (1960) Experiencias clínicas con un nuevo sicosedativo : el Ro 1-9569. Revista Española de Oto-Neuro-Oftalmologia y Neurochirurgia 19:14–19
Fallon P, Dursun S, Deakin B (2012) Drug-induced supersensitivity psychosis revisited: characteristics of relapse in treatment-compliant patients. Ther Adv Psychopharmacol 2:13–22
Fernandez HH, Factor SA, Hauser RA, Jimenez-Shahed J, Ondo WG, Jarskog LF, Meltzer HY, Woods SW, Bega D, LeDoux MS, Shprecher DR, Davis C, Davis MD, Stamler D, Anderson KE (2017) Randomized controlled trial of deutetrabenazine for tardive dyskinesia: the ARM-TD study. Neurology 88:2003–2010
Flegel H (1960) Klinische Erfahrungen mit Nitoman, einem neuartigen Psychopharmakon. Nervenarzt 31:556–557
Glazer WM, Hafez H (1990) A comparison of masking effects of haloperidol versus molindone in tardive dyskinesia. Schizophr Res 3:315–320
Gordon H, Lader M, Shivayogi M, Vermeulen J (1998) Treatment-resistant schizophrenia. Tetrabenazine and reserpine: a case-study. J Forens Psych 9:440–445
Grace AA, Bunney BS, Moore H, Todd CL (1997) Dopamine-cell depolarization block as a model for the therapeutic actions of antipsychotic drugs. Trends Neurosci 20:31–37
Haug JO, Stenstad F (1959) Terapeutiske Meddelelser: Preliminare kliniske forsök med tetrabenazin. Nordisk Psykiatrisk Tidsskrift 13(2):158–161
Hauser RA, Factor SA, Marder SR, Knesevich MA, Ramirez PM, Jimenez R, Burke J, Liang GS, O'Brien CF (2017) KINECT 3: a phase 3 randomized, double-blind, placebo-controlled trial of valbenazine for tardive dyskinesia. Am J Psychiatry 174:476–484
Heinze H (1960) Pharmacotherapy of the psychoses and general practice. Ther Ggw 99:200–204
Howes OD, McCutcheon R, Owen MJ, Murray RM (2017) The role of genes, stress, and dopamine in the development of schizophrenia. Biol Psychiatry 81:9–20
Jauhar S, Veronese M, Nour MM, Rogdaki M, Hathway P, Natesan S, Turkheimer F, Stone J, Egerton A, McGuire P, Kapur S, Howes OD (2019) The effects of antipsychotic treatment on presynaptic dopamine synthesis capacity in first-episode psychosis: a positron emission tomography study. Biol Psychiatry 85:79–87
Josiassen RC, Kane JM, Liang GS, Burke J, O'Brien CF (2017) Long-term safety and tolerability of valbenazine (NBI-98854) in subjects with tardive dyskinesia and a diagnosis of schizophrenia or mood disorder. Psychopharmacol Bull 47:61–68
Kalian M, Lerner V, Goldman M (1993) Atypical variants of tardive dyskinesia, treated by a combination of clozapine with propranolol and clozapine with tetrabenazine. J Nerv Ment Dis 181:649–651
Kammerer T, Singer L, Geissmann P, Wetta JM (1962) Use of a new neuroleptic: tetrabenazine. Clinical, biological and electroencephalographic results. Ann Med Psychol (Paris) 120(1):106–115
Kenney C, Hunter C, Jankovic J (2007) Long-term tolerability of tetrabenazine in the treatment of hyperkinetic movement disorders. Mov Disord 22:193–197
Khurram SK, Ames M, Muniz J (2021) Case report: valbenazine as a treatment for tardive dyskinesia and unexpected antipsychotic effects. J Clin Psychopharmacol 41:220–221
Kostrzewa RM, Brus R (2016) Lifelong rodent model of tardive dyskinesia-persistence after antipsychotic drug withdrawal. Curr Top Behav Neurosci 29:353–362
Lende N (1960) Psychosedative effects of tetrabenazine (RO 1-9569) on hyperactive and disturbed mentally retarded patients. Dis Nerv Syst 21(3)Suppl:118–119
LeWitt PA (2013) Tardive dyskinesia caused by tetrabenazine. Clin Neuropharmacol 36:92–93
Lindenmayer JP, Burke E, Tsuboyama G, Chahal Y, Grewal HK (2022) Valbenazine treatment of tardive dyskinesia and of positive symptoms. J Clin Psychopharmacol 42:109–111
Lindenmayer JP, Josiassen RC, Burke J, Siegert S, Wright C (2017) Psychiatric stability in subjects with tardive dyskinesia treated with valbenazine (NBI-98854). CNS Spectrums 22(1):68
Lindenmayer JP, Marder SR, Singer C, Comella C, Farahmand K, Burke J, Jimenez R, Siegert S (2019) Long-term valbenazine treatment in patients with schizophrenia/schizoaffective disorder or mood disorder and tardive dyskinesia. CNS Spectrums 24(1):214–215
Lingjaerde O (1959) Tetrabenazine, a new ataraxic with reserpine-like effect. Nord Med 62:1576–1578
Lingjaerde O (1963) Tetrabenazine (nitoman) in the treatment of psychoses. With a discussion on the central mode of action of tetrabenazine and reserpine. Acta Psychiatr Scand 39:1–109
Login IS, Cronin MJ, MacLeod RM (1982) Tetrabenazine has properties of a dopamine receptor antagonist. Ann Neurol 12:257–262
Lustig B (1961) Über Erfahrungen mit Nitoman in der Anstalt-psychiatrie V Internat Congr for Psychotherapy, Vienna
Mandel RJ, Hartgraves SL, Severson JA, Woodward JJ, Wilcox RE, Randall PK (1993) A quantitative estimate of the role of striatal D-2 receptor proliferation in dopaminergic behavioral supersensitivity: the contribution of mesolimbic dopamine to the magnitude of 6-OHDA lesion-induced agonist sensitivity in the rat. Behav Brain Res 59:53–64
Matsumoto Y, Totsuka S, Kato M, Inoue M, Okagami K (1966) Therapy of schizophrenia with tetrabenazine. Nihon Rinsho 24:1360–1364
Montagut JB (1960) Clinical experience with nitoman (Ro 1-9569) VIth National Congress of Neuropsychiatry, Barcelona
Narros Martin GC, L. J. (1960) Nitoman in chronic psychiatric patients the 6th National Neuro-Psychiatric Congress, Barcelona
National Institute for Health and Care Excellence (2023) British National Formulary (BNF) https://bnf.nice.org.uk/
Niemann N, Jankovic J (2019) Real-world experience with VMAT2 inhibitors. Clin Neuropharmacol 42:37–41
Palermo G, Mazzucchi S, Unti E, Bonuccelli U, Ceravolo R (2020) Tardive syndrome associated with tetrabenazine in Huntington disease: a case report. J Clin Psychopharmacol 40:628–630
Pomme B, Planche R, Girard J (1960) Clinical trials of a new psycho-sedative: tetrabenazine. Ann Med Psychol (Paris) 118(1):956–966
Reda GC, Germano V (1960) First clinical observations in psychiatry of a new benzoquinolizine derivative, tetrabenazine. Clin Ter 18:368–381
Remington G, Kapur S, Foussias G, Agid O, Mann S, Borlido C, Richards S, Javaid N (2012) Tetrabenazine augmentation in treatment-resistant schizophrenia: a 12-week, double-blind, placebo-controlled trial. J Clin Psychopharmacol 32:95–99
Rissardo JP, Durante Í, Sharon I, Fornari Caprara AL (2022) Pimavanserin and Parkinson’s disease psychosis: a narrative review. Brain Sci 12
Sacerdoti G (1960) First clinical experiences with tetrabenazine. Rass Studi Psichiatr 49:450–460
Schmitt W (1960) On the pharmacotherapy of psychoses: clinical research on tetrabenazine. Psychiatr Neurol (Basel) 140:23–29
Schreiber W, Krieg JC, Eichhorn T (1999) Reversal of tetrabenazine induced depression by selective noradrenaline (norepinephrine) reuptake inhibition. J Neurol Neurosurg Psychiatry 67:550
Shimizu J, Inoue T, Yamazaki H, Sato I (1962) The clinical use of tetrabenazine to schizophrenics. No To Shinkei 14:717–722
Singer L, Geissmann, P., & Wetta, J. M. (1961) Utilisation d'un nouveau neuroleptique, la tétrabénazine (Nitoman Roche). Premiers resultats thérapeutiques et électroencéphalographiques. Ann méd-psychol 119: 370.
Smith ME (1960) Clinical comparison of tetrabenazine (Ro 1-9569), reserpine and placebo in chronic schizophrenics. Dis Nerv Syst 21(3)):120–123
Solmi M, Pigato G, Kane JM, Correll CU (2018) Treatment of tardive dyskinesia with VMAT-2 inhibitors: a systematic review and meta-analysis of randomized controlled trials. Drug Des Devel Ther 12:1215–1238
Stahl SM (2018a) Comparing pharmacologic mechanism of action for the vesicular monoamine transporter 2 (VMAT2) inhibitors valbenazine and deutetrabenazine in treating tardive dyskinesia: does one have advantages over the other? CNS Spectr 23:239–247
Stahl SM (2018b) Mechanism of action of vesicular monoamine transporter 2 (VMAT2) inhibitors in tardive dyskinesia: reducing dopamine leads to less “go” and more “stop” from the motor striatum for robust therapeutic effects. CNS Spectrums 23:1–6
Stedman MR, Curtin F, Elbourne DR, Kesselheim AS, Brookhart MA (2011) Meta-analyses involving cross-over trials: methodological issues. Int J Epidemiol 40:1732–1734
Sterne JAC, Savović J, Page MJ, Elbers RG, Blencowe NS, Boutron I, Cates CJ, Cheng HY, Corbett MS, Eldridge SM, Emberson JR, Hernán MA, Hopewell S, Hróbjartsson A, Junqueira DR, Jüni P, Kirkham JJ, Lasserson T, Li T et al (2019) RoB 2: a revised tool for assessing risk of bias in randomised trials. BMJ 366:l4898
Stockhausen FG (1960a) Clinical studies with tetrabenazine (Ro 1-9569). Dis Nerv Syst 21(3):115–117
Stockhausen FG (1960b) Erfahrungen mit <Nitoman>. Europ Neurol 140:61–62
Stockhausen FG (1960c) Klinische Erfahrungen mit Nitoman (Ro 1–9569). Pharmacol 2:157–161
Stumpf W (1960) Untersuchungen über <Nitoman>. Eur Neurol 140:63–68
Teva Pharmaceuticals USA I (2017) Highlights of prescribing information. Austedo (deutetrabenazine) tablets for oral use.
Thai-Cuarto D, O’Brien CF, Jimenez R, Liang GS, Burke J (2018) Cardiovascular profile of valbenazine: analysis of pooled data from three randomized, double-blind, placebo-controlled trials. Drug Saf 41:429–440
Tsapakis EM, Diakaki K, Miliaras A, Fountoulakis KN (2023) Novel compounds in the treatment of schizophrenia-a selective review. Brain Sci 13
Uhrbrand L, Faurbye A (1960) Reversible and irreversible dyskinesia after treatment with perphenazine, chlorpromazine, reserpine and electroconvulsive therapy. Psychopharmacol 1:408–418
Voelkel A, Dressler J (1959) Klinisch-psychiatrische Erfahrungen mit dem Benzochinolizinderivat RO 1-9569. Nervenarzt 30:322–325
Voelkel VA (1958) Klinische Wirkung von Pharmaka mit Einfluß auf den Monoaminstoffwechsel des Gehirns. Confin neurol 18:144–149
Weckowicz TE, Ward T, Hoffer A (1960) Trial of Ro 1-9569/12 on a group of apathetic chronic schizophrenic patients. Am J Psychiatry 116:930–931
White I, Higgins J (2007) Metamiss Stata module to perform meta-analysis with missing data Statistical Software Components S456869. Boston College Department of Economics
Zheng G, Dwoskin LP, Crooks PA (2006) Vesicular monoamine transporter 2: role as a novel target for drug development. Aaps j 8:E682–E692
Zipursky RB, Menezes NM, Streiner DL (2014) Risk of symptom recurrence with medication discontinuation in first-episode psychosis: a systematic review. Schizophr Res 152:408–414
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
DT has received research funding from Janssen and speaking honoraria from Janssen, Viatris and Otsuka. OH is a part-time employee and stock-holder of H Lundbeck A/s and has received investigator-initiated research funding from and/or participated in advisory/speaker meetings organised by Angellini, Autifony, Biogen, Boehringer-Ingelheim, Eli Lilly, Heptares, Global Medical Education, Invicro, Jansenn, Lundbeck, Neurocrine, Otsuka, Sunovion, Recordati, Roche and Viatris/Mylan. OH has a patent for the use of dopaminergic imaging. The remaining authors declare no conflict of interest.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Connolly, A., Wallman, P., Dzahini, O. et al. Meta-analysis and systematic review of vesicular monoamine transporter (VMAT-2) inhibitors in schizophrenia and psychosis. Psychopharmacology 241, 225–241 (2024). https://doi.org/10.1007/s00213-023-06488-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00213-023-06488-3