Abstract
Summary
There is imminent refracture risk in elderly individuals for up to six years, with a decline thereafter except in women below 75 who face a constant elevated risk. Elderly men with fractures face the highest mortality risk, particularly those with hip and vertebral fractures. Targeted monitoring and treatment strategies are recommended.
Purpose
Current management and interventions for osteoporotic fractures typically focus on bone mineral density loss, resulting in suboptimal evaluation of fracture risk. The aim of the study is to understand the progression of fractures to refractures and mortality in the elderly using multi-state models to better target those at risk.
Methods
This prospective, observational study analysed data from the AGES-Reykjavik cohort of Icelandic elderly, using multi-state models to analyse the evolution of fractures into refractures and mortality, and to estimate the probability of future events in subjects based on prognostic factors.
Results
At baseline, 4778 older individuals aged 65 years and older were included. Elderly men, and elderly women above 80 years of age, had a distinct imminent refracture risk that lasted between 2–6 years, followed by a sharp decline. However, elderly women below 75 continued to maintain a nearly constant refracture risk profile for ten years. Hip (30–63%) and vertebral (24–55%) fractures carried the highest 5-year mortality burden for elderly men and women, regardless of age, and for elderly men over 80, lower leg fractures also posed a significant mortality risk.
Conclusion
The risk of refracture significantly increases in the first six years following the initial fracture. Elderly women, who experience fractures at a younger age, should be closely monitored to address their long-term elevated refracture risk. Elderly men, especially those with hip and vertebral fractures, face substantial mortality risk and require prioritized monitoring and treatment.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Osteoporotic fractures are placing an unequivocal strain on healthcare systems globally in terms of cost and health-related quality of life. The annual incidence of new osteoporotic fractures alarmingly increased 23% from 3.5 million in 2010 to 4.3 million in 2019 in the European Union alone, and this number is expected to increase by a further 25% by 2034 [1, 2]. The associated cost of osteoporotic fractures has also increased, and there is a rapidly increasing treatment gap, which reached as high as 71% in 2019. [2] This treatment gap will exacerbate the public health burden of disability, morbidity and mortality posed by osteoporotic fractures. Moreover, Iceland boasts one of the highest employment rates for senior workers, with a 65% employment rate for individuals aged 55–74 years as of 2021 [3]. This high employment rate highlights the significant contributions that older adults make to Iceland’s workforce. This dependency on the senior workforce underscores the critical need for improved intervention and management of osteoporotic fractures, as the consequences of such fractures can be irreversible.
Sustaining osteoporotic fractures increases the likelihood of both refractures and mortality. The risk of refracture is the highest within the first year [4], and remains elevated for as long as 25 years after the first fracture [5]. Hip and vertebral fractures have particularly high risks of refracture [6,7,8], and refractures further exacerbate this excess mortality risk [9]. Unfortunately, healthcare settings tend to myopically focus on the loss of bone mineral density alone, leading to poor evaluation of the risk associated with osteoporotic fractures. The risk of refracture and mortality after the first fracture is not constant [10], and tends to cluster within the first five years [11]. This is commonly referred to as the 'imminent risk' phase. [12] Unfortunately, there is a paucity of data on this crucial period following a fracture.
The aim of this study is to determine the optimal time for intervention by assessing the progression of fractures to refractures and mortality in the elderly. The study investigated three different multi-state fracture progression models with varying levels of complexity. The first model was a simple fracture-death model, followed by a fracture-refracture-death model. The third model was a further refinement of the fracture-refracture-death model that considered the fracture location. Collectively, these models can predict the probabilities of fracture, refracture and mortality events occurring in the elderly given specific prognostic factors. By accurately assessing the overall risk of osteoporotic fractures, effective prevention and intervention strategies can be implemented to better target the elderly at risk and to optimally mitigate the progression of fractures.
Methods
Study population
The study data was obtained from the Age, Gene/Environment Susceptibility-Reykjavik (AGES-Reykjavik) study, being conducted in Iceland since 2002. The full cohort consists of 5764 elderly men and women. The current analysis included all subjects for whom CT data at baseline was available. Participants, who either did not provide informed consent (n = 49), did not undergo a CT scan (n = 862), did not have height or weight measurements (n = 3) or did not meet any combination of the three criteria (n = 72), were excluded. Since this is an ongoing study, the last follow-up for the purpose of this investigation was at 16.6 years. Subjects were not lost to follow-up during the study, except for cases of death and migration. However, the loss due to migration is expected to be insignificant. Demographic data such as age, gender, body mass index (BMI), prior fracture, and integral volumetric BMD (vBMD) derived from CT scans were collected. Information on osteoporotic status or comorbidities were not obtained.
Fracture and mortality ascertainment
Incident and prevalent fractures were verified from the Icelandic fracture registry according to the International Classification of Diseases version 9 (ICD-9) and 10 (ICD-10) diagnostic codes that define low trauma fractures at the hip, spine, lower leg, and forearm (detailed in Online Resource 1). These fractures were then grouped into the four aforementioned fracture locations. Prior fractures were defined as prevalent fractures occurring before study enrolment. The first incident fracture was defined as an index fracture and a refracture was defined as any fracture event occurring after the index fracture. Subsequent fractures that occurred after the second incident fracture were not utilized for this investigation due to its low frequency. To avoid duplicate inclusions of similar events, the initial instance of a fracture is recorded as the earliest occurrence. Subsequent fractures at the same anatomical location are recognized as new fractures only if they occur at least 90 days after the prior occurrence. Mortality of the subjects enrolled into the study was recorded and verified from the Icelandic registry.
Statistical analysis
Baseline characteristics, reported as mean and standard deviation, were calculated for all continuous variables, while ratios and percentages were calculated for nominal variables. T-tests were used to compare group differences between men and women for all the prognostic factors. Stratified multi-state Cox regression models were applied using the “clock-reset” approach [13]. Prognostic factors were stratified into categorical covariates with transition-specific baseline hazards and were used in the multi-state Cox regression models as covariates (see Table A2; Online Resource 2). Three multi-state models were evaluated (Fig. 1). These models were used to predict the transition-specific probabilities of future events (fracture, refracture and death) for four reference men and women based on their age as follows; young-old man under 75 years old (Myoung), old-old man over 79 years old (Mold), young-old woman under 75 years old (Wyoung) and old-old woman over 79 years old (Wold). The first multi-state model (Model 1) was created with three states: (1) all subjects start at study enrolment in a healthy state, denoted as ‘Entry’; (2) after enrolment, subjects enter into ‘Fracture’ state upon sustaining incident fracture; and (3) subjects who died during the course of the study follow-up with or without sustaining any fracture enter the absorbing state ‘Death’ (Fig. 1A). The second multi-state model (Model 2) had four states: (1) similar to the three-state fracture-death model, subjects start from ‘Entry’; (2) upon entry, the first incident fracture sustained by subjects will lead them to the ‘Index Fracture’ state; (3) subjects then enter ‘Refracture’ state if they sustain the second incident fracture and (4) subjects can enter the absorbing state ‘Death’ from any of the preceding three states (Fig. 1B). The third multi-state model (Model 3) was constructed with seven possible outcomes: (1) subjects start from ‘Entry’; (2–5) subjects that sustain their first incident fracture will enter either ‘Hip Fracture’, ‘Spine Fracture’, ‘Lower Leg Fracture’ or ‘Forearm Fracture’; (6) similar to the four-state model, they then enter the “Refracture’ state if they sustain a second incident fracture and (7) lastly enter the absorbing state ‘Death’ from any of the preceding states (Fig. 1C).
Stacked transition probability plots over a 15-year horizon were generated to predict patient-specific probabilities for each transition for the simple fracture-death model. The ‘death’ state was further stratified into two states; death after a fracture and death by other causes to better visualize the effects of fracture on death. For the second (fracture-refracture-death model) and third model (second model stratified by fracture location), the transition probabilities over a 10-year horizon were plotted. These probabilities were plotted. A p-value of 0.05 was considered to be significant. Multi-state modelling was executed with the R ‘mstate’ package. All other data management and statistical analyses were performed using Python (version 3.8.5) and R (version 3.4.5 for Windows) programming environments.
Results
The current analysis included 4778 subjects aged 65 years and older at study entry (mean age 76.3 ± 5.5 years old), with a median follow-up of 12 years for participants who died before the end of study. Index incident fracture occurred in 29.3% (n = 1404) and refracture in 12.0% (n = 572) of the subjects (Fig. 2). 45.1% (n = 2154) of the subjects died without sustaining incident fractures prior to the end of follow-up and 25.5% (n = 1220) did not have either event (fracture or death) (Fig. 2). Baseline characteristics of subjects showed no significant differences in age, BMI or vBMD between alive and dead groups or between men and women (see Table A3; Online Resource 2). On the contrary, the presence of prior fractures was significantly higher among deceased subjects and in women (see Table A3; Online Resource 2). To better understand the factors contributing to fracture and mortality rates, the impact of individual prognostic factors was also analyzed in detail (Tables A4-5; Fig. A1 ; Online Resource 2).
Model 1: Impact of fracture on mortality
The probability of experiencing fractures increased for Myoung and Wyoung, plateauing around 8% and 11% respectively by the end of 15 years (Fig. 3). However, for Mold and Wold, the fracture risk peaked at approximately 10% after 6.4 years and at 23% after 6.4 years, respectively, before gradually decreasing to 1% and 6%, respectively, by the end of 15 years (Fig. 3). The probability of mortality both due to other causes and due to fracture increased over time for the young-old subjects (Myoung and Wyoung). However, for older subjects, the increase in probability of mortality slowed down after 10 years towards the end of follow-up. The survival of Myoung and Mold were relatively poorer than the respective female counterparts, with a greater probability of overall mortality over the 15 years. Additionally, older subjects (Mold and Wold) had a worse survival than younger subjects (Myoung and Wyoung), such that the probability of being alive at 15 years was approximately 5–10% (Fig. 3). The probability of mortality due to fracture remained relatively lower than the mortality due to other causes for all four reference subjects.
Model 2: Impact of index fracture on refracture and mortality
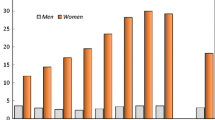
Myoung generally exhibited a higher risk of refracture than Mold except in the first two years (Fig. 4A). The risk of refracture for Myoung consistently increased for three years, until it plateaued for the next 4 years (15–16%) before declining over the remaining period (Fig. 4A). For Mold, the risk peaked at two years (15%) before declining steadily (Fig. 4A). The imminent risk of refracture was 3 and 2 years for Myoung and Mold respectively. Despite the declining risk over time, Myoung was at a 9% higher risk of refracture than Mold at 10 years. Like Myoung and Mold, Wold was also at highest risk of refracture for the first 2 years after index fracture at 19%, plateaued for the next 2 years and lastly decreased to 7% at 10 years (Fig. 4B). Wold faced a higher risk of refracture than Wyoung in the first 5 years and a reversal of trend occurred in the remaining 5 years (Fig. 4B). In contrast, Wyoung showed an increasing refracture profile for 6 years before plateauing at an elevated risk of approximately 20% at 10 years (Fig. 4B) The imminent risk of refracture for Wyoung and Wold was 6 and 2 years respectively.
The risk of mortality after both index fracture and refracture monotonically increased with time and was higher for the older counterparts (Mold and Wold) (Fig. 4C-F). The risk of mortality in the first-year post-index fracture was close to twice as high between Myoung (13%) and Mold (25%) (Fig. 4C), while it was almost three times higher for Wold (16%) than Wyoung (6%) (Fig. 4D). A similar trend was observed for the first year post-refracture mortality between Mold (35%) and Myoung (16%) (Fig. 4E) as well as Wold (26%) and Wyoung (9%) (Fig. 4F). In addition, males were also at a higher risk of mortality than their respective female counterparts. Following refracture, the 5-year mortality was 54% in Myoung and 35% in Wyoung (Fig. 4E-F) and was much higher in their older counterparts respectively (Mold: 86% and Wold: 74%) (Fig. 4E-F). This trend persisted consistently through the tenth year, where mortality following refracture became remarkably pronounced at 98% and 94% for Mold and Wold respectively (Fig. 4E-F).
Model 3: Impact of index fracture location on refracture and mortality
In Myoung, the risk of refracture after a lower leg fracture was highest, compared to other fracture locations over the observed 10-year period (Fig. 5A). The imminent risk of refracture persisted up to 2 years following hip fractures (14%), up to 3 years following vertebral fractures (18%), up to 4 years following lower leg fractures (24%) and up to 6 years following forearm fractures (19%) (Fig. 5A). Following this imminent risk, refracture risks decreased for all fracture locations, except for forearm fractures. Conversely, in the case of Wyoung, the risk profiles for refracture exhibited a persistent heightened risk throughout the entire 10-year period for all fracture locations. There were minimal declines in the risks of refracture, resulting in a plateau of risk by the end of 10 years. The highest risks of refracture before plateauing for Wyoung occurred at 7 years for hip (27%), at 6 years for vertebral (29%), at 4 years for lower leg (25%) and at 8 years for forearm fractures (18%) (Fig. 5B). The 5-year risks of refracture were 14%, 17%, 21% and 17% for hip, vertebral, lower leg, and forearm fractures for Myoung (Fig. 5A) while those for Wyoung were 22%, 25%, 24% and 14% (Fig. 5B) respectively. While forearm fractures had the lowest likelihood of refracture, all other fracture types had the highest likelihood in Wyoung (Fig. 5B).
In Mold, the imminent risk of refracture persisted up to 2 years following hip (15%), up to 3 years for vertebral (13%) and forearm (19%) fractures, and at 1 year for lower leg fractures (19%) (Fig. 5C). Compared to Myoung, the highest risks of refracture occurred earlier in Mold for hip and vertebral fractures. The 5-year risks of refracture were generally lower in Mold compared to Myoung for all fracture locations (8% vs 14% for hip, 9% vs 17% for vertebral, 10% vs 21% for lower leg, and 14% vs 17% for forearm fractures) and these risks continued to steadily decline over the course of 10 years (Fig. 5C). In Wold, the imminent risk of refracture persisted up to 2 years following hip fractures (19%), up to 3 years following vertebral (18%) and forearm (26%) fractures, and up to 4 years following lower leg fractures (25%) (Fig. 5D). A similar trend was exhibited by Wold, as observed in Mold, whereby the refracture risks steadily declined over the remaining period. The 5-year risks of refracture in Wold were 16%, 16%, 20% and 25% for hip, vertebral, lower leg, and forearm fractures respectively (Fig. 5D), which were substantially higher than the 5-year risks of refracture in Mold.
The risk of mortality following a fracture increased over time for all subjects. In Myoung, the 5-year mortality risks after hip, vertebral, lower leg, and forearm fractures were 48%, 46%, 18% and 20% respectively (Fig. 5E). In Wyoung, the highest 5-year mortality risk was associated with hip fractures (30%), followed by vertebral (24%), lower leg (19%), and forearm (11%) fractures (Fig. 5F). In Mold, the risks increased significantly after hip, vertebral, lower leg, and forearm fractures, resulting in 5-year mortality rates of 63%, 55%, 46%, and 30% respectively (Fig. 5G). In Wold, the 5-year mortality risks after the same fractures were 48%, 39%, 14%, and 14% respectively (Fig. 5H). Wyoung experiences the least mortality burden (< 41%) regardless of the fracture location. While hip and vertebral fractures posed the highest mortality burden for all subjects, mortality risk associated with lower leg fractures was notably high in Mold. In general, men (Myoung and Mold) have a greater risk of mortality compared to women (Wyoung and Wold).
Discussion
This study is the first to evaluate three models exploring fractures, refractures, and associated mortality in the elderly. Based on the baseline characteristics of the AGES cohort, it was found that 43% of women and 34% of men, who experienced an incident fracture, suffered a refracture, while 35% of women and 49% of men died during the follow-up period of 17 years. For those who had a refracture, approximately 42% of women and 33% of men experienced more than two fractures, and 77% of women and 88% of men died thereafter. The mortality rate associated with refractures was significantly higher than that of incident fractures, highlighting the elevated mortality risk with refractures. [14]
Model 1: Impact of fracture on mortality
Expectedly, elderly individuals aged 80 and older exhibit notably poorer survival prospects compared to their relatively younger counterparts, emphasizing the influence of age on mortality outcomes. Elderly men experience substantially elevated mortality risk over time, even after a decline in fracture risk. This emphasizes the negative impact of fractures on men's survival. Meanwhile, elevated fracture risk persists in elderly individuals below 75 years of age and is particularly pronounced among elderly women aged 80 and above. The findings from this model highlight the importance of regularly monitoring elderly men and women for at least 10 years, who are particularly susceptible to long-term elevated mortality and fracture risk respectively [9, 15].
Model 2: Impact of index fracture on refracture and mortality
Model 2 demonstrates that the risk associated with refracture and mortality post-index fracture is not linear [10]. The imminent risk of refracture following an incident fracture was found to be 2–6 years, but it remained elevated over follow-up in this study. Imminent risk has been typically reported to last for 1–2 years [11, 16, 17], but some of these studies had short follow-up times [18]. A study demonstrated that the elevated refracture risk did not change from the first 2 years to 5 years for both men and women [17], which suggests that imminent risk may last longer. Furthermore, that study also found that the risk did not change for women for up to 10 years but decreased for men [17]. This is in line with our finding that elderly women under 75 years old have a persistently elevated risk of refracture for up to ten years. This model emphasizes the urgent need for targeted interventions in all post-fracture patients, regardless of age for at least six years following the initial fracture and a need for ongoing post-fracture management in younger elderly women. Furthermore, it is important to note that there is a substantial increase in mortality rates following refracture with increasing age. The progressively escalating trend in mortality rates, especially after refracture, demonstrates not only the immediate consequences of fracture itself, but the compounding effects of age-related comorbidities. The interplay between fracture or refracture events and age-related comorbidities contribute to the overall mortality in the elderly and this should be taken into consideration to effectively mitigate mortality risk.
Model 3: Impact of index fracture location on refracture and mortality
The risk of refracture and mortality after an index fracture varies with age, gender, and fracture location. Among elderly women below the age of 75, refracture risk generally remained elevated, whereas elderly men and elderly women aged above 80 exhibited a distinct imminent risk of refracture. The refracture risk after sustaining lower leg fractures was relatively high in elderly men below the age of 75, with an imminent risk of up to 4 years. In addition, there was a relatively high mortality risk observed in elderly men aged over 80 who experienced lower leg fractures. It is important to note that lower leg fractures can lead to severe functional impairment in the elderly population [19]. Studies have shown that changes in functional ability are closely linked to the probability of refracture [20]. Given the heightened imminent risk and potential functional impairment associated with lower leg fractures, there is a clear need to prioritize monitoring and treatment in elderly men who have sustained lower leg fractures.
Despite forearm fractures showing the lowest refracture burden among elderly women below 75 years of age, it is essential to note that the risk remained elevated throughout the entire 10-year period. In addition, elderly women over 80 years old had the highest refracture burden following forearm fracture, with an imminent risk that lasted up to 3 years. A US-based population study involving patients with forearm fractures revealed that women aged 70 and above had a higher risk of hip fracture compared to younger women [21]. Since elderly men also exhibited relatively high refracture risk following forearm fractures, it becomes crucial to identify and provide treatment for elderly individuals with forearm fractures, particularly those aged over 80, in order to reduce refracture risk. Our study indicates that forearm fractures carry the lowest mortality risk, compared to other fracture locations. While some studies have reported an association between distal radial fractures and increased mortality [22], the relationship between forearm fractures and excess mortality is still not fully understood and further research is needed.
Furthermore, refracture risk after vertebral fracture was relatively high in elderly women under 75 years old, compared to elderly men, and elderly women above 80 years of age. Similarly, although hip fractures exhibited a relatively lower refracture burden than lower leg and vertebral fractures, the associated elevated refracture risk persisted, with minimal decline over the 10 years. These findings suggest that preventive strategies should focus on elderly women who sustain hip and vertebral fractures early as they may be plagued by a long-term elevated refracture burden. In line with previous studies, hip and vertebral fractures carried the highest mortality burden, particularly in elderly men, in our study [23,24,25,26]. The 1-year post-hip fracture mortality, ranging from 12–36% aligned with findings from previous studies [27,28,29]. The 10-year mortality after hip and vertebral fractures were 60–69% and 60–67% in men, and 41–57% and 39–54% in women respectively, indicating a higher risk of mortality among elderly men as observed in other studies.[15, 22], which emphasizes the need for early diagnosis of poor bone health in this demographic.
This study had several notable strengths. Firstly, it had a representative sample of the community-dwelling general elderly population in Iceland, which increases the generalizability of the findings. Moreover, the fracture records were obtained from electronic health records, ensuring their reliability and accuracy. The study also had a long follow-up period of 20 years with no loss to follow-up, which increases the validity of the results. However, the study also had some limitations. One major limitation was the lack of statistical power to determine the association between prior fracture occurrences and fracture, refracture, and mortality. Additionally, the low number of refractures made it difficult to determine the impact of the index fracture location on refracture location.
In conclusion, our study reveals two distinct phases in refracture risk following an initial fracture. The first phase entails an imminent risk spanning up to six years, followed by a phase marked by diminishing risk. Despite this decline, the refracture risk persists at an elevated level for a substantial span of a decade. The progression of mortality risk, following fracture or refracture, with age emphasizes the intricate interplay between aging and fracture consequences. Older women, who sustain fractures relatively early and live long enough to undergo the consequences of fracture and refracture events, are subjected to a vicious cycle of refracture vulnerability. Elderly men regardless of age, particularly those with hip and vertebral fractures carry the highest mortality burden. Further research should focus on defining imminent risk in the elderly for effective resource allocation. This study emphasizes the pressing need for targeted strategies to identify refracture and mortality risk in different fracture scenarios in the elderly. Such strategies can include regular monitoring and targeted interventions, such as fall prevention programs, fracture liaison service and pharmacological treatments. By focusing these targeted preventative strategies within the first six years following the initial fracture or towards more vulnerable elderly populations, cost-effective management strategies that improve the quality of life among the elderly population in Iceland can be developed.
Data availability
Data are available on request from the authors.
References
Hernlund E, Svedbom A, Ivergård M et al (2013) Osteoporosis in the European Union: medical management, epidemiology and economic burden: A report prepared in collaboration with the International Osteoporosis Foundation (IOF) and the European Federation of Pharmaceutical Industry Associations (EFPIA). Arch Osteoporos 8:136. https://doi.org/10.1007/s11657-013-0136-1
Willers C, Norton N, Harvey NC et al (2022) Osteoporosis in Europe: a compendium of country-specific reports. Arch Osteoporos 17:23. https://doi.org/10.1007/s11657-021-00969-8
OECD (2015) Labour market statistics. https://www.oecd-ilibrary.org/content/data/data-00046-en
Balasubramanian A, Zhang J, Chen L et al (2019) Risk of subsequent fracture after prior fracture among older women. Osteoporos Int 30:79–92. https://doi.org/10.1007/s00198-018-4732-1
Morin SN, Yan L, Lix LM, Leslie WD (2021) Long-term risk of subsequent major osteoporotic fracture and hip fracture in men and women: a population-based observational study with a 25-year follow-up. Osteoporos Int 32:2525–2532. https://doi.org/10.1007/s00198-021-06028-9
Colón-Emeric C, Kuchibhatla M, Pieper C et al (2003) The contribution of hip fracture to risk of subsequent fractures: data from two longitudinal studies. Osteoporos Int 14:879–883. https://doi.org/10.1007/s00198-003-1460-x
Klotzbuecher CM, Ross PD, Landsman PB et al (2010) Patients with Prior Fractures Have an Increased Risk of Future Fractures: A Summary of the Literature and Statistical Synthesis. J Bone Miner Res 15:721–739. https://doi.org/10.1359/jbmr.2000.15.4.721
Söreskog E, Ström O, Spångéus A et al (2020) Risk of major osteoporotic fracture after first, second and third fracture in Swedish women aged 50 years and older. Bone 134:115286. https://doi.org/10.1016/j.bone.2020.115286
Bliuc D, Nguyen ND, Nguyen TV et al (2013) Compound risk of high mortality following osteoporotic fracture and refracture in elderly women and men: MORTALITY RISK AFTER OSTEOPOROTIC FRACTURE/REFRACTURE IN THE ELDERLY. J Bone Miner Res 28:2317–2324. https://doi.org/10.1002/jbmr.1968
Roux C, Briot K (2017) Imminent fracture risk. Osteoporos Int 28:1765–1769. https://doi.org/10.1007/s00198-017-3976-5
van Geel TACM, van Helden S, Geusens PP et al (2009) Clinical subsequent fractures cluster in time after first fractures. Ann Rheum Dis 68:99–102. https://doi.org/10.1136/ard.2008.092775
Wong RMY, Wong PY, Liu C et al (2022) The imminent risk of a fracture—existing worldwide data: a systematic review and meta-analysis. Osteoporos Int 33:2453–2466. https://doi.org/10.1007/s00198-022-06473-0
Putter H, Fiocco M, Geskus RB (2007) Tutorial in biostatistics: competing risks and multi-state models. Statist Med 26:2389–2430. https://doi.org/10.1002/sim.2712
Bliuc D, Nguyen ND, Milch VE et al (2009) Mortality Risk Associated With Low-Trauma Osteoporotic Fracture and Subsequent Fracture in Men and Women. JAMA 301:513. https://doi.org/10.1001/jama.2009.50
Ravindrarajah R, Hazra NC, Charlton J et al (2018) Incidence and mortality of fractures by frailty level over 80 years of age: cohort study using UK electronic health records. BMJ Open 8:e018836. https://doi.org/10.1136/bmjopen-2017-018836
Johansson H, Siggeirsdóttir K, Harvey NC et al (2017) Imminent risk of fracture after fracture. Osteoporos Int 28:775–780. https://doi.org/10.1007/s00198-016-3868-0
Center JR, Bliuc D, Nguyen TV, Eisman JA (2007) Risk of Subsequent Fracture After Low-Trauma Fracture in Men and Women. JAMA 297:387. https://doi.org/10.1001/jama.297.4.387
Hannan MT, Weycker D, McLean RR, et al (2019) Predictors of Imminent Risk of Nonvertebral Fracture in Older, High‐Risk Women: The Framingham Osteoporosis Study. JBMR Plus 3:. https://doi.org/10.1002/jbm4.10129
Hsu C-Y, Tsai Y-S, Yau C-S et al (2019) Differences in gait and trunk movement between patients after ankle fracture and healthy subjects. BioMed Eng OnLine 18:26. https://doi.org/10.1186/s12938-019-0644-3
Osipov B, Christiansen BA (2021) Mechanisms for increased systemic fracture risk after index fracture. Medicine in Novel Technology and Devices 11:100072. https://doi.org/10.1016/j.medntd.2021.100072
Cuddihy M-T, Gabriel SE, Crowson CS et al (1999) Forearm Fractures as Predictors of Subsequent Osteoporotic Fractures. Osteoporos Int 9:469–475. https://doi.org/10.1007/s001980050172
Johnell O, Kanis JA, Odén A et al (2004) Mortality after osteoporotic fractures. Osteoporos Int 15:38–42. https://doi.org/10.1007/s00198-003-1490-4
Haentjens P (2010) Meta-analysis: Excess Mortality After Hip Fracture Among Older Women and Men. Ann Intern Med 152:380. https://doi.org/10.7326/0003-4819-152-6-201003160-00008
Cauley JA, Thompson DE, Ensrud KC et al (2000) Risk of Mortality Following Clinical Fractures. Osteoporos Int 11:556–561. https://doi.org/10.1007/s001980070075
Tran T, Bliuc D, van Geel T et al (2017) Population-Wide Impact of Non-Hip Non-Vertebral Fractures on Mortality: POPULATION-WIDE IMPACT OF NHNV FRACTURES ON MORTALITY. J Bone Miner Res 32:1802–1810. https://doi.org/10.1002/jbmr.3118
Adams AL, Ryan DS, Li BH et al (2022) Outcomes post fragility fracture among members of an integrated healthcare organization. Osteoporos Int 33:783–790. https://doi.org/10.1007/s00198-021-06205-w
Teng GG, Curtis JR, Saag KG (2008) Mortality and osteoporotic fractures: is the link causal, and is it modifiable? Clin Exp Rheumatol 26:S125-137
Roux C, Thomas T, Paccou J, et al (2021) Refracture and mortality following hospitalization for severe osteoporotic fractures: The Fractos Study. JBMR Plus 5:. https://doi.org/10.1002/jbm4.10507
Center JR (2017) Fracture Burden: What Two and a Half Decades of Dubbo Osteoporosis Epidemiology Study Data Reveal About Clinical Outcomes of Osteoporosis. Curr Osteoporos Rep 15:88–95. https://doi.org/10.1007/s11914-017-0352-5
Acknowledgements
The research was conducted at the Future Health Technologies at the Singapore-ETH Centre, which was established collaboratively between ETH Zurich and the National Research Foundation Singapore. This research is supported by the National Research Foundation Singapore (NRF) under its Campus for Research Excellence and Technological Enterprise (CREATE) programme.
Funding
This research is supported by the National Research Foundation Singapore (NRF) under its Campus for Research Excellence and Technological Enterprise (CREATE) programme.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Anitha D. Praveen, Thor Aspelund, Stephen J. Ferguson, Sigurður Sigurðsson, Vilmundur Guðnason, Halldór Pálsson, David Matchar, and Benedikt Helgason declare that they have no conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Praveen, A.D., Aspelund, T., Ferguson, S.J. et al. Refracture and mortality risk in the elderly with osteoporotic fractures: the AGES-Reykjavik study. Osteoporos Int 35, 1231–1241 (2024). https://doi.org/10.1007/s00198-024-07096-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00198-024-07096-3