Abstract
Purpose
Assessment of the conventional mechanical axis (MA) (hip-to-talus axis) is reported to result in constitutional varus in the native knee. However, the ground MA (hip-to-calcaneus axis), which is the line from the hip center to the bottom of the calcaneus, passes through the center of the knee joint in the native knee and is a possible alternative target for total knee arthroplasty (TKA) assessments. Therefore, this study aimed to present a “ground kinematically aligned (KA)-TKA.” In this technique, the femoral component is placed on the cylindrical axis using the calipered technique and the tibial component is placed to give a neutral ground MA. Radiographical investigation was used to determine whether physiological alignment can be individually achieved with ground KA-TKA; this was compared with that of a tibia-restricted modified KA-TKA, referring to conventional MA (hip-to-talus axis) results.
Methods
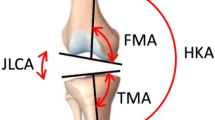
As the primary endpoint, this prospective cohort study compared the ground MA ratios of the knee joints in 40 ground KA-TKAs (G group: Coronal Plain Alignment of the Knee (CPAK) 28 type I, 7 II, 1 IV, and 4 V) with those of the preceding 60 modified KA-TKAs (M group: CPAK 46 type I, 12 II, and 2 V) performed for patients with varus osteoarthritis (OA). The number of outliers differing over ± 5% from the neutral were compared between groups using the χ2-test. The Hip–knee–ankle (HKA) angle, coronal femoral/tibial component alignment (FCA/TCA), and joint line orientation angle (JLOA) were compared between the groups using non-paired t-tests. Statistical significance was set at p < 0.05.
Results
The G group had a higher ratio of the ground MA passing through the knee center than the M group did; outliers differing over ± 5% from the neutral of the ground MA were 2/40 cases in the G group and 20/60 cases in the M group, which was a significant difference (p = 0.001). The HKA angle, FCA/TCA, and JLOA were not significantly different between the groups.
Conclusions
Targeting the ground MA in KA-TKA for patients with varus OA was feasible and has the potential to provide a physiological alignment more similar to the native knee in TKA than other kinematic alignment techniques.
Level of evidence
Level III.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Recently, the alignment philosophy underpinning the study of total knee arthroplasty (TKA) has tended to shift from mechanically aligned TKA as the gold standard to personalized alignment instead [10]. Hirschmann et al. created a new classification for functional knee phenotypes using a coronal lower limb alignment based on the native alignment in young individuals without osteoarthritis (OA) [12]. Based on 125 possible functional knee phenotypes, they indicated the eight most common functional phenotypes which covered two-thirds of the total population and represented which phenotypes were suitable for mechanical, anatomical, and restricted kinematic alignment. The group also confirmed the great variability of joint line orientation in osteoarthritic and non-osteoarthritic knees by assessing the femoral mechanical angle (FMA) and tibial mechanical angle (TMA), indicating the necessity of a more individualized approach in TKA [9, 11]. More recently, MacDessi et al. introduced the Coronal Plane Alignment of the Knee (CPAK) classification system which classified knee phenotypes based on constitutional limb alignment and joint line obliquity [21]. The classification system also indicated that the kinematic approach was suitable for Type I (varus, apex distal joint line) and type IV (varus, neutral joint line) out of nine classification categories. Anatomical and restricted kinematically aligned (KA)-TKA [14, 16] have gained popularity for reproducing physiological joint lines and kinematics with minimal soft tissue release, and achieve better clinical outcomes than mechanically aligned TKA. However, recent meta-analyses have shown that the advantage of KA-TKA is still controversial compared with mechanically aligned TKA; one showed better early clinical outcomes and another did not [4, 12] and MacDessi’s [21] classifications for ground KA-TKA should be investigated by widening the patient population. The radiological two-dimensional simulation of the surgery was another limitation of this study. The influence of limb rotational position on parameter changes should be validated by three-dimensional analysis. Most importantly, the clinical outcomes were not assessed. Reduced alignment outliers in ground KA-TKA may lead to good clinical outcomes without any catastrophic failures; however, its clinical relevance should be investigated further in the future.
Conclusions
In conclusion, the ground KA-TKA technique with radiological preoperative planning was easily feasible for mild-to-moderate varus OA patients. This new KA-TKA procedure, as a personalized alignment technique, may provide greater physiological alignment which is more comparable to the native knee than other alignment techniques in TKA.
Data availability
The data that support the findings of this study are available on request from the corresponding author.
References
Bellemans J, Colyn W, Vandenneucker H, Victor J (2012) The Chitranjan Ranawat award: is neutral mechanical alignment normal for all patients? The concept of constitutional varus. Clin Orthop Relat Res 470:45–53
Chandler JT, Moskal JT (2004) Evaluation of knee and hindfoot alignment before and after total knee arthroplasty: a prospective analysis. J Arthroplast 19:211–216
Cho WS, Cho HS, Byun SE (2017) Changes in hindfoot alignment after total knee arthroplasty in knee osteoarthritic patients with varus deformity. Knee Surg Sports Traumatol Arthrosc 25:3596–3604
Courtney PM, Lee GC (2017) Early outcomes of kinematic alignment in primary total knee arthroplasty: a meta-analysis of the literature. J Arthroplast 32(2028–2032):e2021
Desai SS, Shetty GM, Song HR, Lee SH, Kim TY, Hur CY (2007) Effect of foot deformity on conventional mechanical axis deviation and ground mechanical axis deviation during single leg stance and two leg stance in genu varum. Knee 14:452–457
Faul F, Erdfelder E, Lang AG, Buchner A (2007) G*Power 3: a flexible statistical power analysis program for the social, behavioral, and biomedical sciences. Behav Res Methods 39:175–191
Gao ZX, Long NJ, Zhang SY, Yu W, Dai YX, **ao C (2020) Comparison of kinematic alignment and mechanical alignment in total knee arthroplasty: a meta-analysis of randomized controlled clinical trials. Orthop Surg 12:1567–1578
Haraguchi N, Ota K, Tsunoda N, Seike K, Kanetake Y, Tsutaya A (2015) Weight-bearing-line analysis in supramalleolar osteotomy for varus-type osteoarthritis of the ankle. J Bone Joint Surg Am 97:333–339
Hess S, Moser LB, Robertson EL, Behrend H, Amsler F, Iordache E et al (2022) Osteoarthritic and non-osteoarthritic patients show comparable coronal knee joint line orientations in a cross-sectional study based on 3D reconstructed CT images. Knee Surg Sports Traumatol Arthrosc 30:407–418
Hirschmann MT, Karlsson J, Becker R (2018) Hot topic: alignment in total knee arthroplasty-systematic versus more individualised alignment strategies. Knee Surg Sports Traumatol Arthrosc 26:1587–1588
Hirschmann MT, Moser LB, Amsler F, Behrend H, Leclercq V, Hess S (2019) Phenoty** the knee in young non-osteoarthritic knees shows a wide distribution of femoral and tibial coronal alignment. Knee Surg Sports Traumatol Arthrosc 27:1385–1393
Hirschmann MT, Moser LB, Amsler F, Behrend H, Leclerq V, Hess S (2019) Functional knee phenotypes: a novel classification for phenoty** the coronal lower limb alignment based on the native alignment in young non-osteoarthritic patients. Knee Surg Sports Traumatol Arthrosc 27:1394–1402
Hiyama S, Takahashi T, Takeshita K (2022) Kinematically aligned total knee arthroplasty did not show superior patient-reported outcome measures: an updated meta-analysis of randomized controlled trials with at least 2-year follow-up. J Knee Surg 35:634–639
Howell SM, Howell SJ, Kuznik KT, Cohen J, Hull ML (2013) Does a kinematically aligned total knee arthroplasty restore function without failure regardless of alignment category? Clin Orthop Relat Res 471:1000–1007
Howell SM, Papadopoulos S, Kuznik KT, Hull ML (2013) Accurate alignment and high function after kinematically aligned TKA performed with generic instruments. Knee Surg Sports Traumatol Arthrosc 21:2271–2280
Hutt JR, LeBlanc MA, Masse V, Lavigne M, Vendittoli PA (2016) Kinematic TKA using navigation: surgical technique and initial results. Orthop Traumatol Surg Res 102:99–104
Ishii Y, Noguchi H, Sato J, Takahashi I, Ishii H, Ishii R et al (2021) Alignment evaluation using different distal reference points after total knee arthroplasty. J Orthop 25:186–190
Kamenaga T, Nakano N, Takayama K, Tsubosaka M, Takashima Y, Kikuchi K et al (2021) Comparison of plantar pressure distribution during walking and lower limb alignment between modified kinematically and mechanically aligned total knee arthroplasty. J Biomech 120:110379
Kikuchi N, Kanamori A, Kadone H, Okuno K, Hyodo K, Yamazaki M (2022) Radiographic analysis using the hip-to-calcaneus line and its association with lower limb joint kinetics in varus knee osteoarthritis. Knee 35:142–148
Kim JG, Suh DH, Choi GW, Koo BM, Kim SG (2021) Change in the weight-bearing line ratio of the ankle joint and ankle joint line orientation after knee arthroplasty and high tibial osteotomy in patients with genu varum deformity. Int Orthop 45:117–124
MacDessi SJ, Griffiths-Jones W, Harris IA, Bellemans J, Chen DB (2021) Coronal plane alignment of the knee (CPAK) classification. Bone Joint J 103-B:329–337
Matsumoto T, Hashimura M, Takayama K, Ishida K, Kawakami Y, Matsuzaki T et al (2015) A radiographic analysis of alignment of the lower extremities–initiation and progression of varus-type knee osteoarthritis. Osteoarthritis Cartilage 23:217–223
Matsumoto T, Takayama K, Ishida K, Hayashi S, Hashimoto S, Kuroda R (2017) Radiological and clinical comparison of kinematically versus mechanically aligned total knee arthroplasty. Bone Joint J 99-B:640–646
Matsumoto T, Takayama K, Ishida K, Kuroda Y, Tsubosaka M, Muratsu H et al (2020) Intraoperative soft tissue balance/kinematics and clinical evaluation of modified kinematically versus mechanically aligned total knee arthroplasty. J Knee Surg 33:777–784
Matsumoto T, Takayama K, Muratsu H, Matsushita T, Kuroda R, Kurosaka M (2015) Semimembranosus release reduces tibial internal rotation and flexion angle in cruciate-retaining total knee arthroplasty. J Arthroplasty 30:1537–1541
Mullaji A, Shetty GM (2011) Persistent hindfoot valgus causes lateral deviation of weightbearing axis after total knee arthroplasty. Clin Orthop Relat Res 469:1154–1160
Naylor BH, Seidman D, Scuderi GR (2021) Bridging the gap: the influence of foot and ankle pathomechanics in total knee arthroplasty. J Am Acad Orthop Surg 29:e693–e701
Norton AA, Callaghan JJ, Amendola A, Phisitkul P, Wongsak S, Liu SS et al (2015) Correlation of knee and hindfoot deformities in advanced knee OA: compensatory hindfoot alignment and where it occurs. Clin Orthop Relat Res 473:166–174
Reilingh ML, Beimers L, Tuijthof GJ, Stufkens SA, Maas M, van Dijk CN (2010) Measuring hindfoot alignment radiographically: the long axial view is more reliable than the hindfoot alignment view. Skeletal Radiol 39:1103–1108
Schelker BL, Nowakowski AM, Hirschmann MT (2022) What is the “safe zone” for transition of coronal alignment from systematic to a more personalised one in total knee arthroplasty? A systematic review. Knee Surg Sports Traumatol Arthrosc 30:419–427
Tanaka T, Takayama K, Hashimoto S, Kanzaki N, Hayashi S, Kuroda R et al (2017) Radiographic analysis of the lower limbs using the hip-calcaneus line in healthy individuals and in patients with varus knee osteoarthritis. Knee 24:1146–1152
Acknowledgements
The authors thank Editage, a division of Cactus Communications, for their assistance with the preparation of this manuscript.
Funding
Open access funding provided by Kobe University. The authors received no funding to support this study.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
None of the authors have any potential conflicts of interest, including financial interests, activities, relationships, and affiliations, to disclose.
Ethical approval
The hospital’s ethics committee approved the study protocol (Kobe University, No. 290038).
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Matsumoto, T., Nakano, N., Ishida, K. et al. Targeting the neutral hip-to-calcaneus axis in kinematically aligned total knee arthroplasty is feasible with fewer alignment outliers for varus osteoarthritic patients. Knee Surg Sports Traumatol Arthrosc 31, 3880–3888 (2023). https://doi.org/10.1007/s00167-023-07306-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00167-023-07306-1