Abstract
Objective
Increased O-linked β-N-acetylglucosamine (O-GlcNAc) stimulation has been reported to protect against sepsis associated mortality and cardiovascular derangement. Previous studies, including our own research, have indicated that gasdermin-D(GSDMD)-mediated endothelial cells pyroptosis contributes to sepsis-associated endothelial injury. This study explored the functions and mechanisms of O-GlcNAc modification on lipopolysaccharide (LPS)-induced pyroptosis and its effects on the function of GSDMD.
Methods
A LPS-induced septic mouse model administrated with O-GlcNAcase (OGA) inhibitor thiamet-G (TMG) was used to assess the effects of O-GlcNAcylation on sepsis-associated vascular dysfunction and pyroptosis. We conducted experiments on human umbilical vein endothelial cells (HUVECs) by challenging them with LPS and TMG to investigate the impact of O-GlcNAcylation on endothelial cell pyroptosis and implications of GSDMD. Additionally, we identified potential O-GlcNAcylation sites in GSDMD by utilizing four public O-GlcNAcylation site prediction database, and these sites were ultimately established through gene mutation.
Results
Septic mice with increased O-GlcNAc stimulation exhibited reduced endothelial injury, GSDMD cleavage (a marker of pyroptosis). O-GlcNAc modification of GSDMD mitigates LPS-induced pyroptosis in endothelial cells by preventing its interaction with caspase-11 (a human homologous of caspases-4/5). We also identified GSDMD Serine 338 (S338) as a novel site of O-GlcNAc modification, leading to decreased association with caspases-4 in HEK293T cells.
Conclusions
Our findings identified a novel post-translational modification of GSDMD and elucidated the O-GlcNAcylation of GSDMD inhibits LPS-induced endothelial injury, suggesting that O-GlcNAc modification-based treatments could serve as potential interventions for sepsis-associated vascular endothelial injury.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Vascular endothelial injury is a critical factor in the pathogenesis and progression of sepsis [1,2,3,4]. This injury is characterized by the disruption of the endothelial barrier, increased vascular permeability, and leakage, which ultimately results in reduced blood flow perfusion in the microcirculation [2]. Existing literature has reported a close association between sepsis and vascular inflammation, thrombosis, and decreased blood perfusion, all of which contribute to increased mortality in septic patients. Evidence from evidence-based medicine shows that anti-inflammatory and anti-thrombotic therapies alone do not improve the ultimate outcomes of septic patients [5, 6]. Therefore, in our study, the focus has been on elucidating the potential mechanisms underlying the decrease in blood perfusion in sepsis. Previous research, including studies conducted by others and our own, has demonstrated that endothelial cell pyroptosis contributes to sepsis-associated endothelial injury and hypoperfusion in sepsis [7,8,9,36], GPP prediction server (https://comp.chem.nottingham.ac.uk/cgi-bin/glyco/bin/getparams.cgi) [37], and GlycoMine (https://glycomine.erc.monash.edu/Lab/GlycoMine/#webserver) [38]. The raw data obtained from these four prediction sites underwent statistical analysis. A Venn diagram was created to determine the predicted set of sites that were identified as the most likely potential O-GlcNAcylation sites for GSDMD. This analysis allowed for a comprehensive evaluation of the predictions made by each site and the identification of common sites predicted by multiple prediction methods.
Plasmid and molecular cloning
The pCMV vector expressing Myc-tagged human OGT (PPL00887-2a) was purchased from PPL. To generate the GSDMD constructs, the gene sequence of GSDMD was obtained from the GenBank database. The template for cloning and construction experiments was obtained, and the necessary modifications were made. The FLAG-tagged GSDMD, FLAG-tagged human GSDMD-NT, FLAG-tagged human GSDMD (S338A) and human GSDMD (S480A) constructs were generated by GENECHEM. The cloning and construction experiments allowed for the creation of the desired mutant plasmids.
Cell transfection
HEK293T and HUVECs were cultured in DMEM or F-12 medium supplemented with 10% FBS, 100 U/ml penicillin, and 100 µg/ml streptomycin, respectively. The cells were incubated in a humidified atmosphere containing 5% CO2. For transfection, cells were grown in 6-well plates until they reached 90% confluence. Plasmid DNA was added to 500 µl of medium, while Lipofectamine 2000 transfection reagent (Invitrogen) was added to another 500 µl of medium. After incubating for 5 min at room temperature, the two media were mixed and incubated for an additional 20 min. The cell culture medium was then replaced with the mixture of media containing the plasmid and Lipofectamine 2000.
Immunoblotting
Cultured HUVECs were collected and lysed with lysis buffer containing 98% RIPA lysis buffer, 1% protease inhibitor, and 1% phosphatase inhibitor. The cells were incubated with the lysis buffer on ice for 30 min. The total protein concentration in the lysate was measured using the BCA protein assay kit from Beyotime Biotechnology, Shanghai, China. Equal amounts of protein from each sample were loaded onto SDS-PAGE gels and separated by electrophoresis. The proteins were then transferred onto polyvinylidene fluoride (PVDF) membranes and blocked with PBST containing 5% skim milk blocking buffer at room temperature for 2 h.
Primary antibodies, including O-GlcNAc (Cell Signaling Technology, #9875), GSDMD (Santa Cruz Biotechnology, sc-393581), GSDMD (Abcam, ab209845), β-actin (SAB, #21338), GAPDH (Proteintech), OGT (Santa Cruz Biotechnology, sc-74546), Myc Tag (Invitrogen, # R951-25), OGA (Proteintech, 14711-1-AP), were incubated with the membranes followed by incubation with HRP-conjugated secondary antibodies (anti-rabbit IgG from Bioword, and anti-mouse IgG from Bioword). Protein bands were detected using an Enhanced Chemiluminescent (ECL) reagent from Thermo Scientific, and the images were acquired with a ChemiDoc MP System from Bio-Rad. Densitometric analysis was performed using ImageJ Software to quantify the protein bands.
Statistics
All experiments were conducted with a minimum of three independent replicates to ensure robustness and reliability of the results. Statistical analysis was performed using GraphPad Prism 8 software. The data are presented as mean ± standard deviation (SD). To compare the mean values of biochemical data between different groups, a two-tailed Student’s t test was employed. For comparisons involving multiple time points, repeated-measures analysis of variance (ANOVA) was used, followed by Bonferroni post-tests. A significance level of P < 0.05 was considered statistically significant for all analyses.
Results
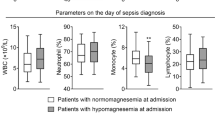
O-GlcNAc modification ameliorated vascular endothelial injury in septic mice
Following the methods described in the literature [26], we administered the OGA inhibitor TMG for 12 h, followed by intraperitoneal injection of LPS for an additional 12 h. We then assessed the blood flow perfusion in the liver, mesentery, and lower limbs of the mice using Laser Doppler imaging (Fig. 1A). After LPS administration, a significant decrease in blood flow perfusion was observed in the liver, mesentery, and lower limbs (P < 0.0001). In contrast, the septic mice treated with TMG showed a significant increase in blood perfusion in these regions compared to the sepsis group (LPS) (P < 0.005) (Fig. 1B–D). To investigate the impact of O-GlcNAc modification on the inhibition of vascular endothelial injury, we examined the expression of the vascular endothelial marker CD31 in the mice aorta. The results revealed a reduction in the fluorescence expression of CD31 in the vascular endothelial of septic mice compared to control mice. However, treatment with TMG effectively mitigated the LPS-induced reduction in the endothelial marker CD31 (Fig. 1E). These findings suggest that TMG has the potential to alleviate vascular endothelial injury induced by LPS.
O-GlcNAc modification ameliorated vascular endothelial injury in septic mice. A Experimental design for assessing the effect of Thiamet-G(TMG) on LPS-induced blood flow perfusion. 600 μg/kg TMG were injected intravenously 12 h before injection of LPS (20 mg/kg) was applied 10–12 h. B–D Analysis of blood flow perfusion of the liver, mesentery, and lower limbs by laser Doppler imaging in different treatment mice at 12 h after induction of endotoxemia (20 mg/kg i.p.). E Immunofluorescence analysis of endothelial marker CD31 in the aorta of different treatment mice at 12 h after induction of endotoxemia (20 mg/kg i.p.). Scale bar: 100 μm, n = 5, Data are expressed as means ± SD of six animals per treatment, **p < 0.005, ***p < 0.0005, ****p < 0.0001
Increased O-GlcNAc levels inhibited GSDMD cleavage in the aorta of septic mice
To elucidate the dose-dependent effect of TMG on increasing total vascular protein O-GlcNAcylation levels, we initially administered different doses of TMG via tail vein injection. Subsequently, 12 h post-injection, Western blot analysis was conducted to assess vascular total protein O-GlcNAc expression. The results indicated that a dose of 600 µg/kg TMG exhibited a consistently stable increase in vascular O-GlcNAc levels (Fig. 2A, B). Subsequent experiments were performed using this dosage condition. To assess the impact of TMG treatment on GSDMD protein cleavage, we examined the levels of global O-GlcNAc and GSDMD in the mice aorta. In an experimental sepsis model induced by LPS, aorta samples exhibited a decrease in global O-GlcNAc levels, accompanied by a significant increase in GSDMD-N production. However, upon treatment with TMG, the aorta showed increased global O-GlcNAc levels and decreased levels of GSDMD-N, as demonstrated by Western blot analysis (Fig. 2C, D). These findings demonstrate that increased O-GlcNAc levels contribute to the reduction of endothelial cell pyroptosis in septic mice.
Increased O-GlcNAc levels inhibited GSDMD cleavage. A, B Western Blot analysis of different doses of TMG were injected intravenously 12 h to detect the global O-GLcNAc level. Data are expressed as means ± SD of three animals per treatment, *p < 0.05, n = 3. C, D Western Blot analysis of TMG (600 μg/kg) were injected intravenously 12 h following injection of LPS (20 mg/kg) for 12 h to detect the global O-GlcNAc level and GSDMD-N production. Data are expressed as means ± SD of six animals per treatment, *p < 0.05, n = 6
Increased O-GlcNAc modification inhibited LPS-induced endothelial cells pyroptosis
To further investigate the role of O-GlcNAc modification in regulating LPS-induced endothelial cell pyroptosis in vitro, we treated HUVECs with different concentrations of LPS and examined the global O-GlcNAc levels. As shown in Fig. 3A, B, the global O-GlcNAc levels decreased with increasing LPS stimulation concentration. However, administration of TMG increased the global O-GlcNAc levels in HUVECs (Fig. 3C, D). Furthermore, we evaluated the effects of O-GlcNAc modification on LPS-induced pyroptosis. HUVECs treated with LPS exhibited rapid morphological changes and LDH release, indicating the occurrence of pyroptosis. However, these effects were inhibited by TMG treatment (Fig. 3E, H). Additionally, TMG pretreatment reduced the levels of GSDMD-N protein, as shown in Fig. 3F, G, suggesting that TMG may exert its effects by inhibiting GSDMD cleavage. In summary, these findings collectively demonstrate that O-GlcNAc modification inhibits LPS-induced endothelial cell pyroptosis, providing further evidence for the role of O-GlcNAc in regulating inflammatory processes in endothelial cells.
O-GlcNAc modification inhibits LPS-induced endothelial cells pyroptosis. A, B HUVECs transfected with LPS induced marked O-GLcNAc protein level in a concentration-dependent manner and statistics analysis of O-GLcNAc level, n = 3. C, D Western Blott showing global O-GlcNAc levels under TMG and LPS treatment, statistics analysis of O-GLcNAc level, n = 3. E Total cell lysates of HUVECs untreated or stimulated with LPS (1 μg/ml) alone with or without TMG (1 μM) pretreatment marked cell swell and lysis, n = 3. Scale bar: 50 μm, n = 3. F, G TMG (1 μM) treated HUVECs transfected with LPS induced marked GSDMD cleavage decreased as compared with that in HUVECs transfected with LPS, Statistics analysis of GSDMD-F and GSDMD-N level, n = 6. H TMG (1 μM) treated HUVECs transfected with LPS induced marked LDH release decreased as compared with that in HUVECs transfected with LPS, n = 3. Data are expressed as means ± SD of three independent experiments, *p < 0.05
GSDMD O-GlcNAcylation involvement in LPS-induced endothelial cell pyroptosis
To investigate the O-GlcNAcylation level of GSDMD and the effect of O-GlcNAc modification on the interaction between Caspase-4 and GSDMD under LPS stimulation in HUVECs, we conducted a co-immunoprecipitation (Co-IP) experiment. Firstly, we performed a Co-IP experiment between O-GlcNAc and GSDMD to observe the impact of LPS on GSDMD O-GlcNAcylation. (Fig. 4A–C). And then, when TMG was administered under LPS treatment, a Co-IP experiment between O-GlcNAc and GSDMD to observe the impact of LPS and TMG on GSDMD O-GlcNAcylation, it increased the O-GlcNAcylation of GSDMD and decreased the expression of GSDMD-N (Fig. 4D–F). The results suggest that O-GlcNAcylation of GSDMD may be involved in the regulation of pyroptosis effector molecule GSDMD-N expression by LPS and TMG. Furthermore, we used Caspase-4 antibodies for Co-IP and found that the interaction between Caspase-4 and GSDMD increased under LPS stimulation. However, this interaction was inhibited by TMG administration (Fig. 4G–H). These findings suggest that O-GlcNAcylation of GSDMD involvement in LPS-induced endothelial cell pyroptosis.
GSDMD O-GlcNAcylation involvement in LPS-induced endothelial cell pyroptosis. A Total cell lysates of HUVECs untreated or stimulated with LPS. Immunoprecipitation with anti-GSDMD antibody to pull down O-GlcNAcylated proteins, n = 3. B Total cell lysates of HUVECs untreated or stimulated with LPS alone with or without TMG pretreatment. Immunoprecipitation with anti-GSDMD antibody to pull down O-GlcNAcylated proteins, n = 3. C Total cell lysates of HUVECs untreated or stimulated with LPS alone with or without TMG pretreatment was immunoprecipitated with anti-Caspase-4 antibody, followed by immunoblotting with anti-GSDMD antibody, n = 3. D Statistics analysis of GSDMD level precipitated by Caspase-4. E Statistics analysis of O-GlcNAc level precipitated by GSDMD under untreated or stimulated with LPS. F Statistics analysis of GSDMD-F and GSDMD-N level of input group under untreated or stimulated with LPS. G Statistics analysis of O-GlcNAc level precipitated by GSDMD under untreated or stimulated with LPS alone with or without TMG pretreatment. H Statistics analysis of GSDMD-F and GSDMD-N level of input group under untreated or stimulated with LPS alone with or without TMG pretreatment. Data are expressed as means ± SD of three independent experiments, *p < 0.05
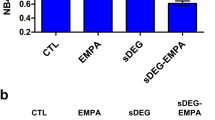
Increased O-GlcNAc modification of GSDMD Ser-338 lead to a reduction in interaction of GSDMD and Caspase-4
To identify potential O-GlcNAc modification sites on GSDMD, multiple prediction websites including DictyOGlyc 1.1 server, NetOGlyc 4.0 server, GPP prediction server, and GlycoMine were employed. Bioinformatic analysis suggests that Ser-338 may be a specific site for GSDMD O-GlcNAc modification (Fig. 5A). To confirm the importance of this site, site-directed mutagenesis was performed to generate a single mutant (S338A) within the C-terminal domain of GSDMD (Fig. 5B, C). In HEK293T cells, Flag-GSDMD-WT, Flag-GSDMD-S338A, and Flag-GSDMD-S480A (another potential O-GlcNAc modification site) were co-expressed with OGT. Western blot analysis revealed that GSDMD-WT and GSDMD-S480A were modified by O-GlcNAc, while GSDMD-S338A showed significantly reduced O-GlcNAc modification (Fig. 5D). These results indicated that Ser-338 might be the key site for O-GlcNAc modification of GSDMD. Furthermore, it was observed that TMG treatment reversed LPS-induced cell death in HEK293T cells transfected with GSDMD-WT plasmid. However, when GSDMD-S338A was transfected, TMG treatment had no effect on LPS-induced cell death (Fig. 5E). To further investigate the effect of GSDMD O-GlcNAcylation on GSDMD-N generation and the interaction between Caspase-4 and GSDMD. We employed the S338A mutant plasmid to perform a Co-IP experiment between Caspase-4 and GSDMD, the results indicate that when GSDMD is able to be O-GlcNAc-modified normally (GD-WT), TMG can increase GSDMD O-GlcNAcylation, thereby reducing the binding between caspase-4 and GSDMD as well as GSDMD cleavage (Lane 2 vs. Lane 1); GSDMD S338A cannot be O-GlcNAcylated (GD-S338A), and the effect of TMG in increasing GSDMD O-GlcNAcylation is abolished, resulting in the binding between Caspase-4 and GSDMD as well as GSDMD cleavage (Lane 3 vs. Lane 2) (Fig. 5F–H). Moreover, TMG reduced LDH release under LPS stimulation, while the GSDMD-S338A mutant exhibited defects in LDH release (Fig. 5I). These results suggest that reduced O-GlcNAcylation of GSDMD under LPS stimulation conditions promotes pyroptosis.
Increased O-GlcNAc modification of GSDMD Ser338 lead to a reduction in interaction of GSDMD and caspase-4. A Venn analysis diagram of O-GlcNAcylation prediction websites. B, C A view of the GSDMD mutant site. D O-GlcNAcylation of GSDMD-WT, GSDMD-S338A and GSDMD-S480A overexpressed in 293T cells in the presence of OGT, n = 3. E Cell morphology change of HUVECs untreated or stimulated with LPS alone with or without TMG pretreatment. Scale bar: 50 μm, n = 3. F GSDMD and GSDMD S338A mutant overexpressed in 293T cells untreated or stimulated with LPS alone with or without TMG was immunoprecipitated with anti-Caspase-4 antibody, followed by immunoblotting with anti-GSDMD antibody, n = 3. G Statistics Analysis of GSDMD level of immunoprecipitated with Caspase-4. H Statistics Analysis of GSDMD-F and GSDMD-N level of Input group. I LDH release of HUVECs untreated or stimulated with LPS alone with or without TMG pretreatment, n = 3. Data are expressed as means ± SD of three independent experiments, *p < 0.05
Discussion
In this study, we uncovered a novel post-translational modification of GSDMD and its functional implications. We provided evidence for the beneficial effects of enhancing O-GlcNAc modification on organ blood flow perfusion in sepsis. Our findings indicated that O-GlcNAcylation of GSDMD played a crucial role in the regulation of vascular endothelial function. Specifically, O-GlcNAcylation of GSDMD suppressed its interaction with caspase-4, leading to a decrease in LPS-induced GSDMD-N formation in HUVECs. The authors further identified Ser-338 as an important O-GlcNAcylation site on GSDMD during the process of pyroptosis (Fig. 6). These findings provide new evidence and insights into the mechanisms by which O-GlcNAc inhibits pyroptosis.
Schema of hypothesis that O-GlcNAc modification of GSDMD attenuates LPS-induced endothelial cells pyroptosis. Intracellular LPS directly activates caspase-4/11, and activated caspase-4/11 can cleave GSDMD and induce pyroptosis, which promotes the release of inflammatory factors and the entry of extracellular water into the cell, leading to cell swelling and lysis. While GSDMD can be modified by O-GlcNAc under the action of TMG, so that caspase-4/11 cannot bind to GSDMD, thus to prevent the cleavage of GSDMD, and finally inhibit the occurrence of pyroptosis. O–G O-GlcNAc
Our previous study discovered that GSDMD significantly exacerbated multiple-organ perfusion disturbances in endotoxemia models, which paralleled endotoxin death in mice [8]. Recent studies have also reported that acute increase in O-GlcNAc levels improves survival in mice with LPS-induced sepsis. In this study, they investigated the protective effect of O-GLcNAc on vascular injury in septic mice by constructing a sepsis model using intraperitoneal injection of 20 mg/kg LPS [26]. Thus, our study utilized this modeling approach to investigate the relationship between O-GlcNAc levels and vascular injury. We demonstrated that elevated O-GlcNAc levels promoted the blood flow perfusion in the liver, mesentery, and lower limbs of the LPS induced septic mice, increased the expression of the vascular endothelial marker CD31 in the LPS induced septic mice aorta, indicating that O-GlcNAcylation might improve the prognosis of sepsis by influencing blood flow perfusion and vascular endothelial integrity. Additionally, our findings indicated that TMG treatment inhibited the cleavage of vascular GSDMD in the septic mouse model, suggesting that O-GlcNAcylation regulates the process of pyroptosis.
This study, along with others, has demonstrated that increasing O-GLcNAc levels can mitigate endothelial injury induced by LPS, TNF-α and other factors [27]. Building upon this knowledge, we conducted further investigations and discovered that O-GlcNAcylation of GSDMD plays a crucial role in LPS-induced pyroptosis. The study supports the notion that O-GlcNAc modification of GSDMD inhibits LPS-induced endothelial cell pyroptosis by interfering with its interaction with Caspases, thereby preventing its cleavage and subsequent cell death. Other studies have also reported the inhibitory effects of GSDMD succination, another post-translational modification, on LPS-induced pyroptosis [19]. Based on these experimental findings, it is suggested that post-translational modifications of proteins play a protective role in vascular endothelial injury caused by LPS or other injurious factors.
Glycosylation, including O-GlcNAcylation, is known to regulate protein–protein interactions [23, 30, 39]. Previous studies have demonstrated that O-GlcNAcylation of RIPK3 blocks the interaction between RIPK3 and RIPK1 or RIPK3 and itself, thereby inhibiting downstream signaling activation [21]. Similarly, increased O-GlcNAcylation of A20 enhances its binding to TAX1BP1, a regulatory protein for A20 activity [27]. In our study, we found that O-GlcNAcylation of GSDMD on Ser-338 inhibits its interaction with Caspase-4. O-GlcNAc modification of proteins may induce conformational changes that affect the exposure of specific protein sequences, potentially altering the intermediate junction region of GSDMD or the binding site for Caspases in its C-terminal region. The specific mechanism by which Ser-338 sites of GSDMD affect Caspases-GSDMD interaction will be further investigated in future studies. It's important to note that besides glycosylation, other post-translational modifications such as phosphorylation, acetylation, and ubiquitination can also regulate protein function [40, 41]. Whether these modifications occur in GSDMD and contribute to its functional changes will require further experimental validation.
Although we have identified the role and mechanism of O-GlcNAc modification of GSDMD in LPS-induced pyroptosis, a comprehensive review is still needed to fully understand the effects of O-GlcNAcylation on pyroptosis. It is important to acknowledge that our study does not exclude the possibility of O-GlcNAc modification on GSDME, another protein involved in pyroptosis, and its potential role in regulating cell pyroptosis. GSDMD has been recognized as the primary substrate for Caspases in pyroptosis, particularly in sepsis, while GSDME mediates pyroptosis in other diseases [11]. In a study utilizing mice lacking only Caspase-1, where a Caspase-11 bacterial artificial chromosome transgene was microinjected into Caspase-1/11 double-knockout embryos, the authors demonstrated that Caspase-1-independent noncanonical pathways mediated by Caspase-11 promoted lethal septic shock following LPS challenge. They found that cytosolic LPS-mediated pyroptosis was the main driver for septic shock, highlighting the crucial role of Caspase-4/5/11 as LPS receptors [12].
In conclusion, our study revealed that GSDMD undergoes O-GlcNAc modification, and this modification plays a crucial role in suppressing pyroptosis by preventing the interaction between Caspases and GSDMD. Moreover, increasing O-GlcNAcylation promoted organ blood flow perfusion and protected against vascular endothelial dysfunction in a mouse sepsis model. These findings provide novel insights into the regulatory role of O-GlcNAcylation in pyroptosis during bacterial infections. Targeting GSDMD O-GlcNAcylation could be a potential therapeutic approach for the treatment of sepsis.
Data availability
The datasets used during the present study are available upon reasonable request.
Abbreviations
- O-GlcNAc:
-
O-Linked β-N-acetylglucosamine
- GSDMD:
-
Gasdermin-D
- LPS:
-
Lipopolysaccharide
- HUVECs:
-
Human umbilical vein endothelial cells
- OGT:
-
O-GlcNAc transferase
- OGA:
-
O-GlcNAcase
- TMG:
-
Thiamet-G
- LDH:
-
Lactate dehydrogenase
References
Darwish I, Liles WC. Emerging therapeutic strategies to prevent infection-related microvascular endothelial activation and dysfunction. Virulence. 2013;4:572–82. https://doi.org/10.4161/viru.25740.
Joffre J, Hellman J, Ince C, Ait-Oufella H. Endothelial responses in sepsis. Am J Respir Crit Care Med. 2020;202(3):361–70. https://doi.org/10.1164/rccm.201910-1911TR.
Opal SM, van der Poll T. Endothelial barrier dysfunction in septic shock. J Intern Med. 2015;277:277–93. https://doi.org/10.1111/joim.12331.
Lee WL, Slutsky AS. Sepsis and endothelial permeability. N Engl J Med. 2010. https://doi.org/10.1056/NEJMcibr1007320.
Dinarello CA. Proinflammatory cytokines. Chest. 2000;118:503–8. https://doi.org/10.1378/chest.118.2.503.
Warren BL, Eid A, Singer P, Pillay SS, Carl P, Novak I, Chalupa P, Atherstone A, Penzes I, Kubler A, Knaub S, Keinecke HO, Schindel F, Heinrichs H, Juers M, Bone RC, Opal SM, KyberSept Trial Study Group. Caring for the critically ill patient. High-dose antithrombin III in severe sepsis: a randomized controlled trial. JAMA. 2001;286:1869–78. https://doi.org/10.1001/jama.286.15.1869.
Chen Q, Yang Y, Hou J, Shu Q, Yin Y, Fu W, et al. Increased gene copy number of DEFA1/DEFA3 worsens sepsis by inducing endothelial pyroptosis. Proc Natl Acad Sci USA. 2019;116:3161–70. https://doi.org/10.1073/pnas.1812947116.
Liu H, Tang D, Zhou X, Yang X, Lu B, Chen AF. PhospholipaseCγ1/calcium-dependent membranous localization of Gsdmd-N drives endothelial pyroptosis, contributing to lipopolysaccharide-induced fatal outcome. Am J Physiol Heart Circ Physiol. 2020;319(6):H1482–95. https://doi.org/10.1152/ajpheart.00731.2019.
Cheng KT, Rehman J, Malik AB. Caspase-11–mediated endothelial pyroptosis underlies endotoxemia-induced lung injury. J Clin Invest. 2017;127(11):4124–35. https://doi.org/10.1172/jci94495.
Peng F, Chang W, Sun Q, Xu X, **e J, Qiu H, et al. HGF alleviates septic endothelial injury by inhibiting pyroptosis via the mTOR signalling pathway. Respir Res. 2020;21:215. https://doi.org/10.1186/s12931-020-01480-3.
Shi J, Gao W, Shao F. Pyroptosis: gasdermin-mediated programmed necrotic cell death. Trends Biochem Sci. 2017;42:245–54. https://doi.org/10.1016/j.tibs.2016.10.004.
Kayagaki N, Stowe IB, Lee BL, O’Rourke K, Anderson K, Warming S, et al. Caspase-11 cleaves gasdermin D for non-canonical inflammasome signalling. Nature. 2015;526:666–71. https://doi.org/10.1038/nature15541.
Yang J, Zhao Y, Shao F. Non-canonical activation of inflammatory caspases by cytosolic LPS in innate immunity. Curr Opin Immunol. 2015;32:78–83. https://doi.org/10.1016/j.coi.2015.01.007.
Hu JJ, Liu X, **a S, Zhang Z, Zhang Y, Zhao J, et al. FDA-approved disulfiram inhibits pyroptosis by blocking gasdermin D pore formation. Nat Immunol. 2020;21:736–45. https://doi.org/10.1038/s41590-020-0669-6.
Rathkey JK, Zhao J, Liu Z, Chen Y, Yang J, Kondolf HC, et al. Chemical disruption of the pyroptotic pore-forming protein gasdermin D inhibits inflammatory cell death and sepsis. Sci Immunol. 2018. https://doi.org/10.1126/sciimmunol.aat2738.
Liu Z, Wang C, Yang J, Chen Y, Zhou B, Abbott DW, et al. Caspase-1 engages full-length gasdermin d through two distinct interfaces that mediate caspase recruitment and substrate cleavage. Immunity. 2020;53:106–14. https://doi.org/10.1016/j.immuni.2020.06.007.
Aglietti RA, Dueber EC. Recent insights into the molecular mechanisms underlying pyroptosis and gasdermin family functions. Trends Immunol. 2017;38:261–71. https://doi.org/10.1016/j.it.2017.01.003.
Wang K, Sun Q, Zhong X, Zeng M, Zeng H, Shi X, et al. Structural mechanism for GSDMD targeting by autoprocessed caspases in pyroptosis. Cell. 2020;180:941-55e20. https://doi.org/10.1016/j.cell.2020.02.002.
Humphries F, Shmuel-Galia L, Ketelut-Carneiro N, Li S, Wang B, Nemmara VV, et al. Succination inactivates gasdermin D and blocks pyroptosis. Science. 2020;369:1633–7. https://doi.org/10.1126/science.abb9818.
Zachara NE. The roles of O-linked β-N-acetylglucosamine in cardiovascular physiology and disease. Am J Physiol Heart Circ Physiol. 2012;302:H1905–18. https://doi.org/10.1152/ajpheart.00445.2011.
Li X, Gong W, Wang H, Green DR, Singh PK, Wen H. O-GlcNAc transferase suppresses inflammation and necroptosis by targeting receptor-interacting serine_threonine-protein kinase 3. Immunity. 2019;50:1–15. https://doi.org/10.1016/j.immuni.2019.01.007.
Park J, Ha HJ, Chung ES, Baek SH, Cho Y, Kim HK, Han J, Sul JH, Lee J, Kim E, Kim J, Yang YR. O-GlcNAcylation ameliorates the pathological manifestations of Alzheimer’s disease by inhibiting necroptosis. Sci Adv. 2021;7:3. https://doi.org/10.1126/sciadv.abd3207.
Zhang J, Yu P, Hua F, Hu Y, **ao F, Liu Q, Huang D, Deng F, Wei G, Deng W, Ma J, Zhu W, Zhang J, Yu S. Sevoflurane postconditioning reduces myocardial ischemia reperfusion injury-induced necroptosis by up-regulation of OGT-mediated O-GlcNAcylated RIPK3. Aging. 2020. https://doi.org/10.18632/aging.104146.
Hilgers RH, **ng D, Gong K, Chen YF, Chatham JC, Oparil S. Acute O-GlcNAcylation prevents inflammation-induced vascular dysfunction. Am J Physiol Heart Circ Physiol. 2012;303:H513–22. https://doi.org/10.1152/ajpheart.01175.2011.
Jensen RV, Andreadou I, Hausenloy DJ, Bøtker HE. The role of O-GlcNAcylation for protection against ischemia-reperfusion injury. Int J Mol Sci. 2019. https://doi.org/10.3390/ijms20020404.
Silva JF, Olivon VC, Mestriner F, Zanotto CZ, Ferreira RG, Ferreira NS, et al. Acute increase in O-GlcNAc improves survival in mice with LPS-induced systemic inflammatory response syndrome. Front Physiol. 2019;10:1614. https://doi.org/10.3389/fphys.2019.01614.
Yao D, Xu L, Xu O, Li R, Chen M, Shen H, et al. O-Linked β-N-Acetylglucosamine modification of A20 enhances the inhibition of NF-κB (Nuclear Factor-κB) activation and elicits vascular protection after acute endoluminal arterial injury. Arterioscler Thromb Vasc Biol. 2018;38:1309–20. https://doi.org/10.1161/atvbaha.117.310468.
Zhong M, Wu W, Wang Y. Inhibition of sphingosine kinase 1 attenuates sepsis-induced microvascular leakage via inhibiting macrophage NLRP3 inflammasome activation in mice. Anesthesiology. 2020;132:1503–15. https://doi.org/10.1097/aln.0000000000003192.
Chatham JC, Young ME, Zhang J. Role of O-linked N-acetylglucosamine (O-GlcNAc) modification of proteins in diabetic cardiovascular complications. Curr Opin Pharmacol. 2020;57:1–12. https://doi.org/10.1016/j.coph.2020.08.005.
Chatham JC, Zhang J, Wende AR. Role of O-linked N-acetylglucosamine protein modification in cellular (patho)physiology. Physiol Rev. 2020. https://doi.org/10.1152/physrev.00043.2019.
Ju KE. O-GlcNAc transferase: structural characteristics, catalytic mechanism and small-molecule inhibitors. ChemBioChem. 2020;21:3026–35. https://doi.org/10.1002/cbic.202000194.
Elbatrawy AA, Kim EJ, Nam G. O-GlcNAcase: emerging mechanism, substrate recognition and small molecule inhibitors. ChemMedChem. 2020;15:1244–57. https://doi.org/10.1002/cmdc.202000077.
Zachara NE, Hart GW. The emerging significance of O-GlcNAc in cellular regulation. Chem Rev. 2002;102:431–8. https://doi.org/10.1021/cr000406u.
Fulop N, Marchase R, Chatham J. Role of protein O-linked N-acetyl-glucosamine in mediating cell function and survival in the cardiovascular system. Cardiovasc Res. 2007;73:288–97. https://doi.org/10.1016/j.cardiores.2006.07.018.
Gupta R, Jung E, Gooley AA, Williams KL, Brunak S, Hansen J. Scanning the available Dictyostelium discoideum proteome for O-linked GlcNAc glycosylation sites using neural networks. Glycobiology. 1999;9:1009–22. https://doi.org/10.1093/glycob/9.10.1009.
Steentoft C, Vakhrushev SY, Joshi HJ, Kong Y, Vester-Christensen MB, Schjoldager KT, et al. Precision map** of the human O-GalNAc glycoproteome through SimpleCell technology. EMBO J. 2013;32:1478–88. https://doi.org/10.1038/emboj.2013.79.
Hamby SE, Hirst JD. Prediction of glycosylation sites using random forests. BMC Bioinform. 2008;9:500. https://doi.org/10.1186/1471-2105-9-500.
Li F, Li C, Wang M, Webb GI, Zhang Y, Whisstock JC, et al. GlycoMine: a machine learning-based approach for predicting N-, C- and O-linked glycosylation in the human proteome. Bioinformatics (Oxford, England). 2015;31:1411–9. https://doi.org/10.1093/bioinformatics/btu852.
Zhang B, Li M-D, Yin R, Liu Y, Yang Y, Mitchell-Richards KA, et al. O-GlcNAc transferase suppresses necroptosis and liver fibrosis. JCI Insight. 2019. https://doi.org/10.1172/jci.insight.127709.
Bolanle IO, Riches-Suman K, Williamson R, Palmer TM. Emerging roles of protein O-GlcNAcylation in cardiovascular diseases: insights and novel therapeutic targets. Pharmacol Res. 2021;165: 105467. https://doi.org/10.1016/j.phrs.2021.105467.
Jensen ON. Modification-specific proteomics characterization of posttranslational modifications by mass spectrometry. Curr Opin Chem Biol. 2004. https://doi.org/10.1016/j.cbpa.2003.12.009.
Acknowledgements
We thank Dr. ** Leng
Contributions
FY designed the work, performed the experiments and wrote the manuscript. YL performed data analysis and provided technical support. ZZ and AC contributed to the conceptualization and reviewed the manuscript. All authors reviewed the manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Ethics statement
The animal studies were performed with the approval and supervision of the Animal Welfare and Ethics Committee of The Third **angya Hospital of Central South University.
Additional information
Responsible Editor: John Di Battista.
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Yu, F., Zhang, Z., Leng, Y. et al. O-GlcNAc modification of GSDMD attenuates LPS-induced endothelial cells pyroptosis. Inflamm. Res. 73, 5–17 (2024). https://doi.org/10.1007/s00011-023-01812-1
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00011-023-01812-1