Abstract
Objectives
To compare the performance of ultra-low-dose computed tomography (ULD-CT) with standard-dose computed tomography (SD-CT) for the diagnosis of non-displaced fractures of the shoulder, knee, ankle, and wrist.
Methods
This prospective study enrolled 92 patients receiving conservative treatment for limb joint fractures who underwent SD-CT followed by ULD-CT at a mean interval of 8.85 ± 1.98 days. Fractures were characterized as displaced or non-displaced. Objective (signal-to-noise ratio, contrast-to-noise ratio) and subjective CT image quality were evaluated. Observer performance for ULD-CT and SD-CT detecting non-displaced fractures was estimated by calculating the area under the receiver operating characteristic (ROC) curve (Az).
Results
The effective dose (ED) for the ULD-CT protocol was significantly lower than the ED for the SD-CT protocol (F = 422.21~2112.25, p < 0.0001); 56 patients (65 fractured bones) had displaced fractures, and 36 patients (43 fractured bones) had non-displaced fractures. Two non-displaced fractures were missed by SD-CT. Four non-displaced fractures were missed by ULD-CT. Objective and subjective CT image quality was significantly improved for SD-CT compared to ULD-CT. The sensitivity, specificity, PPV, NPV, and diagnostic accuracy of SD-CT and ULD-CT for non-displaced fractures of the shoulder, knee, ankle and wrist were similar: 95.35% and 90.70%; 100% and 100%; 100% and 100%; 99.72% and 99.44%; and 99.74% and 99.47%, respectively. The Az was 0.98 for SD-CT and 0.95 for ULD-CT (p = 0.32).
Conclusion
ULD-CT has utility for the diagnosis of non-displaced fractures of the shoulder, knee, ankle, and wrist and can support clinical decision-making.
Key points
-
1.
ULD-CT qualified the requirements for diagnosis of non-displaced fractures.
-
2.
ULD-CT for limb joint fractures is a useful alternative to digital radiography.
-
3.
ULD-CT protocol for limb joint imaging effectively reduces the dose of radiation.
Similar content being viewed by others
Background
Fracture of the bones that make up the joints of an upper or lower extremity is a common acute health issue. Computed tomography (CT) is the gold-standard imaging modality for the diagnosis and evaluation of limb joint fractures [1] and is used for clinical decision-making [2,3,4]. In 2019, in the USA, an estimated 90 million CT scans were performed [5].
Standard-dose CT (SD-CT) is associated with 70–100 times the radiation exposure of conventional X-rays, and medical radiation from CT scans is responsible for approximately 0.4% of all malignant tumors [6]. Increasingly, CT scans for fractures are optimized to reduce radiation doses to “as low as reasonably achievable” while maintaining diagnostic accuracy [8,9,10].
Although low-dose (LD-CT) and ultra-low-dose CT (ULD-CT) (effective dose [ED] 0.53–900 μSv) have been used to diagnose selected limb fractures [7, 9, 11, 12], reports on the use of ULD-CT for the diagnosis of non-displaced limb fractures are scarce. The objective of this study was to compare the performance of ULD-CT with SD-CT for the diagnosis of non-displaced fractures of the shoulder, knee, ankle, and wrist.
Methods
Study population
This prospective study enrolled patients receiving conservative treatment for musculoskeletal complaints between November 30, 2019, and April 25, 2021. Inclusion criteria were (1) age ≥ 18 years; (2) recent history of trauma; (3) diagnosis of fracture on digital radiography (DR) or suspected fracture; and (4) clinical indication for SD-CT. Exclusion criteria were (1) metal implant; (2) history of tumors; or (3) history of arthritis or bone metabolic disease.
Included patients underwent clinically indicated SD-CT followed by an ULD-CT at an interval of 1–2 weeks. CT re-examination was required for non-operated fracture patients within 2 weeks to evaluate any increase in the degree of fracture displacement necessitating surgery [13].
The protocol for this study was approved by the Ethics Committee of Guangdong Provincal Hospital of Traditional Chinese Medicine (BF2019-030-01). All patients provided written informed consent for the acquisition of a ULD-CT after a SD-CT.
Scan protocols
Scans were performed using a Canon 320-detector-row CT scanner (Aquilion One Vision; Canon Medical Systems, Otawara, Japan). For the shoulder, knee, ankle, and wrist, SD-CT scanning parameters were 120 kV tube voltage and 150, 120, 120, and 50 mA tube current, respectively; ULD-CT scanning parameters were 80 kV tube voltage and 52, 11, 11, and 4 mA tube current, respectively; scan range was 160 mm, 140 mm, 140 mm, and 100 mm, respectively. Scan slice thickness was 0.5–1 mm. CTDIvol (mGy) and DLP (mGy*cm) were automatically implemented for all CT-protocols by the scanner software.
Effective dose (ED = DLP*k) for each patient was calculated by multiplying DLP by k (a conversion coefficient): shoulder k = 0.0113 (SD-CT) k = 0.0091 (ULD-CT); knee k = 0.0004 (SD-CT and ULD-CT); ankle and wrist k = 0.0002 (SD-CT and ULD-CT) [12]
Post-processing was performed on a dedicated workstation (VitreaFX3.0). Image reconstruction involved multiplanar reformatting (MPR), volume rendering (VR), and maximum intensity projection (MIP).
Image evaluation
Two senior clinicians with 10–13 years of experience in musculoskeletal diseases independently reviewed each image to characterize each fracture as displaced or non-displaced. Displaced fractures were defined as having a fracture line > 2 mm wide and/or > 1 mm displacement of the bone cortex. Non-displaced fractures were defined as having no angulation or shortening, a fracture line < 2 mm wide, and/or < 1 mm displacement of the bone cortex [14,15,16]. Avulsion fractures caused by a sudden and violent pull of a muscle or ligament were characterized as displaced or non-displaced fractures when bone fragment displacement was > 5 mm or < 5 mm, respectively [16]. Each clinician reviewed each image twice at an interval of > 6 weeks. Disagreements about image interpretation were resolved through discussion and consensus.
A final diagnosis was made based on the CT/DR review within 1–3 months based on the presence of a callus at the fracture end, dysplasia, and an old fracture without a callus [8, 16].
One experienced radiologist evaluated objective CT image quality metrics. A region of interest (ROI) (70 mm2) was placed within the muscles around the joints. Mean/standard deviation CT values of muscle (CTm) were determined from three measurements. A ROI (8 mm2) was placed on the thickest region of the cross section of the cortical shell of the bones of the joint. Mean/standard deviation CT values of bone (CTb) were determined from three measurements. CT values of joint cortical bone (CTc) were calculated as: CTb-CTm. Noise was calculated as mean CTm standard deviation. Signal-to-noise ratio (SNR) was calculated as: mean CTm/mean CTm standard deviation. Contrast-to-noise ratio (CNR) was calculated as (mean CTc–mean CTm) /mean CTm standard deviation [16].
Two experienced radiologists and two orthopedic physicians evaluated subjective CT image quality and the impact of subjective CT image quality on clinical decision-making on a 5-point Likert-type scale (Table 1).
Statistical analysis
Statistical analyses were conducted using IBM SPSS Statistics, v26.0 (IBM Corp., Armonk, NY, USA). CTDIvol, DLP, ED, CTc, SNR, and CNR for SD-CT and ULD-CT were compared using analysis of variance (ANOVA), or Tamhane's T2 test for data with unequal variances. Subjective CT image quality and the impact of subjective CT image quality on clinical decision-making for SD-CT and ULD-CT were compared with the rank sum test. The consistency of the two radiologists on the 5-point Likert-type scale evaluating subjective CT image quality and the impact of subjective CT image quality on clinical decision-making was assessed using the intraclass correlation coefficient (ICC), where < 0.40 = poor consistency; 0.41–0.60 = moderately consistent; 0.61–0.80 = good consistency; 0.81–1.00 = perfect consistency. The sensitivity, specificity, positive predictive value (PPV), negative predictive value (NPV), and accuracy of SD-CT and ULD-CT for the diagnosis of non-displaced fractures of the shoulder, knee, ankle, and wrist were calculated. Observer performance for ULD-CT and SD-CT was estimated by calculating the area under the Receiver Operating Characteristic (ROC) curve (Az).
Results
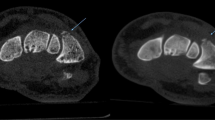
This study included 92 patients receiving conservative treatment for fractures of the shoulder, knee, ankle, or wrist who underwent SD-CT and ULD-CT at an interval of 1–2 weeks (mean, 8.85 ± 1.98 days); 24 patients (72 bones) had shoulder fractures, 17 patients (68 bones) had knee fractures, 25 patients (225 bones) had ankle fractures, and 26 patients (390 bones) had wrist fractures. Of these, 56 patients (65 fractured bones; 17 fractured shoulders, 14 fractured knees, 10 fractured ankles and 6 fractured wrists, with 1 bone fracture per joint; 1 fractured ankle and 8 fractured wrists, with 2 bone fractures per joint) had displaced fractures, and 36 patients (43 fractured bones; 7 fractured shoulders (Fig. 1a, b), 3 fractured knees (Fig. 1c, d), 12 fractured ankles and 7 fractured wrists, with 1 bone fracture per joint; 2 fractured ankles and 5 fractured wrists, with 2 bone fractures per joint (Figs. 2 , 3) had non-displaced fractures. Four non-displaced fractures were missed by ULD-CT (Fig. 2).
Diagnosis of non-displaced fracture of the shoulder (a, b) or knee (c, d) (red arrow). a and c: SD-CT images (subjective CT image quality and impact of subjective CT image quality on clinical decision-making, 5 points); b and d ULD-CT images (subjective CT image quality and impact of subjective CT image quality on clinical decision-making, 3 points)
Missed diagnosis of non-displaced fracture of the ankle on SD-CT and ULD-CT (the fracture line can be seen as the red arrow). a SD-CT image (subjective CT image quality and impact of subjective CT image quality on clinical decision-making, 5 points); b SD-CT three-dimensional reconstruction; c ULD-CT image (subjective CT image quality, 4 points, impact of subjective CT image quality on clinical decision-making, 5 points); d ULD-CT three-dimensional reconstruction
The ED for the ULD-CT protocol was significantly lower (shoulder, knee, ankle, wrist: 23.21 ± 2.24 μSv, 2.10 ± 0.25 μSv, 1.02 ± 0.11, 0.29 ± 0.06 μSv, respectively) than the ED for the SD-CT protocol (shoulder, knee, ankle, wrist: 2513.49 ± 345.13 μSv, 71.05 ± 8.57μSv, 34.60 ± 3.65 μSv, 9.40 ± 2.26 μSv, respectively) (F = 422.21~2112.25, p < 0.0001; Table 2).
Objective CT image quality (noise, SNR, CNR) was significantly improved for SD-CT compared to ULD-CT (F = 16.42~1808.07, p < 0.0001). CTc was significantly higher for ULD-CT compared to SD-CT (F = 23.97~136.48, p < 0.0001; Table 3) Scores for subjective CT image quality and the impact of subjective CT image quality on clinical decision-making were ≥ 3 points for SD-CT and ULD-CT, but were significantly improved for SD-CT compared to ULD-CT (Z = − (3.76–4.46), p < 0.0001) (Figs. 1, 2, 3, Table 4). ICC values for subjective CT image quality and the impact of subjective CT image quality on clinical decision-making for SD-CT and ULD-CT indicated good consistency (ICC = 0.65–0.99, Table 4).
The sensitivity, specificity, PPV, NPV, and diagnostic accuracy of SD-CT and ULD-CT for non-displaced fractures of the shoulder, knee, ankle, and wrist were similar: 95.35% and 90.70%; 100% and 100%; 100% and 100%; 99.72% and 99.44%; and 99.74% and 99.47%, respectively.
The Az value for detecting non-displaced fractures using SD-CT was 0.98 (95%CI: 0.96–0.99), which was slightly higher than ULD-CT (0.95, [95%CI: 0.94–0.97], p = 0.32).
Discussion
This study compared the performance of ULD-CT with SD-CT for the diagnosis of non-displaced fractures of the shoulder, knee, ankle, and wrist. Findings showed the ED for the ULD-CT protocol was significantly lower than the ED for the SD-CT protocol and lower than that for DR [17]. ULD-CT image quality was inferior to SD-CT, but the sensitivity, specificity, PPV, NPV, and diagnostic accuracy of SD-CT and ULD-CT for non-displaced fractures of the shoulder, knee, ankle, and wrist were similar. To the author’s knowledge, this is the first study to show that ULD-CT is a feasible alternative to SD-CT for imaging these types of fracture.
Non-displaced fractures are challenging to detect by physical examination and DR [18]. Missed or misdiagnosis of a non-displaced fracture can delay treatment and have a negative impact on patients' functional recovery [18]. Reports on the diagnostic performance of CT for assessment of non-displaced fractures are scarce [19, 20], potentially due to the lack of a clear definition of displaced versus non-displaced fractures [14,15,16]. A fracture is considered non-displaced if the fragments remain aligned. Displaced fragments are defined as the abnormal position of the distal fracture fragment in relation to the proximal bone and may be minimal, moderate, or severe. Non-displaced or minimally displaced fractures can be difficult to differentiate, but it is important to distinguish between these as treatment and outcome can vary [21].
Previous studies have assessed the clinical utility of ULD-CT for evaluating select limb fractures [7, 9, 11,12,13, 16]. Two studies showed ULD-CT (tube voltage, 80–120 kV; tube current, 10 mA) was a useful alternative to DR in the evaluation of acute wrist and ankle fractures [9, 22]. In another study, a ULD-CT protocol (tube voltage, 120 kV; tube current, 15–19 mA) that decreased the ED by a factor of 14 compared to SD-CT provided high-quality images for reliable detection of various types of limb fracture identifiable on screening plain radiographs of an injured body part [20]. In the present study, scanning parameters were designed to reduce ED according to the size and thickness of limb joints. The highest ED was used for the shoulder (80 kv, 52 mAs). The lowest ED (80 kV, 5 mAs) was used for the wrist. In a previous study that used a similar protocol for wrist traumas in an emergency department, ULD-CT (80 kV, 5 mAs) provided high-quality images with no changes in diagnostic accuracy while reducing the radiation dose by approximately 98% compared to SD-CT [7, 23].
The present study was associated with several limitations. First, the sample size was small. Second, SD-CT and ULD-CT were performed at an interval of 1–2 weeks; during this time, fractures may have changed. Third, the ULD-CT protocol was not compared to DR or magnetic resonance imaging (MRI). Finally, the impact of SD-CT and ULD-CT on perioperative outcomes was not evaluated.
Conclusion
The sensitivity, specificity, and diagnostic accuracy of SD-CT and ULD-CT for non-displaced fractures of the shoulder, knee, ankle, and wrist were similar. These data imply that ULD-CT has utility for the diagnosis of non-displaced fractures of the shoulder, knee, ankle and wrist, and can support clinical decision-making.
Availability of data and materials
The datasets used or analyzed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- CNR:
-
Contrast-to-noise ratio.
- CTb:
-
CT values of bone
- CTm:
-
CT values of muscle
- DR:
-
Digital radiography
- ED:
-
Effective dose
- MIP:
-
Maximum intensity projection
- MPR:
-
Multiplanar reformatting
- ROC:
-
Receiver operating characteristic
- ROI:
-
Region of interest
- SD-CT:
-
Standard-dose computed tomography
- SNR:
-
Signal-to-noise ratio
- ULD-CT:
-
Ultra-low-dose computed tomography
- VR:
-
Volume rendering
References
Cuddy K, Khatib B, Bell RB et al (2018) Use of intraoperative computed tomography in craniomaxillofacial trauma surgery. J Oral Maxillofac Surg 76(5):1016–1025
Matsuoka S, Eguchi T, Takeda T, Miura K, Hamanaka K, Shimizu K (2021) Three-dimensional computed tomography and indocyanine green-guided technique for pulmonary sequestration surgery. General Thorac Cardiovasc Surg 69(3):621–624
**a H, Sun Z, Wang J et al (2020) Application of rib surface positioning ruler combined with volumetric CT measurement technique in endoscopic minimally invasive thoracic wall fixation surgery. Exp Ther Med 20(2):1616–1620
Halvachizadeh S, Berk T, Pieringer A et al (2020) Is the additional effort for an intraoperative CT scan justified for distal radius fracture fixations? A comparative clinical feasibility study. J Clin Med 9(7):2254
Garg M, Karami V, Moazen J et al (2022) Radiation exposure and lifetime attributable risk of cancer incidence and mortality from low-and standard-dose CT chest: implications for COVID-19 pneumonia subjects. Diagonstics (Basel) 12(12):3043
Azman RR, Shah MNM, Ng KH (2019) Radiation safety in emergency medicine: balancing the benefits and risks. Korean J Radiol 20(3):399–404
**ao M, Zhang M, Lei M et al (2021) Application of ultra-low-dose CT in 3D printing of distal radial fractures. Eur J Radiol 135:109488
Elegbede A, Diaconu S, Dreizin D et al (2020) Low-dose computed tomographic scans for postoperative evaluation of craniomaxillofacial fractures: a pilot clinical study. Plast Reconstr Surg 146(2):366–370
Alagic Z, Bujila R, Enocson A, Srivastava S, Koskinen SK (2020) Ultra-low-dose CT for extremities in an acute setting: initial experience with 203 subjects. Skeletal Radiol 49(4):531–539
Eriksson T, Berg P, Olerud C, Shalabi A, Hänni M (2019) Low-dose CT of postoperative pelvic fractures: a comparison with radiography. Acta Radiol 60(1):85–91
Hamard A, Greffier J, Bastide S et al (2021) Ultra-low-dose CT versus radiographs for minor spine and pelvis trauma: a Bayesian analysis of accuracy. Eur Radiol 31:2621–2633
Lei M, Zhang M, Li H et al (2022) The diagnostic performance of ultra-low-dose 320-row detector CT with different reconstruction algorithms on limb joint fractures in the emergency department. Jpn J Radiol 40:1079–1086
Zhang M, Lei M, Zhang J et al (2022) Feasibility study of three-dimensional printing knee model using the ultra-low-dose CT scan for preoperative planning and simulated surgery. Insights Imaging 13(1):1–9
Jensen MR, Andersen KH, Jensen CH (1997) Management of undisplaced or minimally displaced Colles’ fracture: one or three weeks of immobilization. J Orthop Sci 2(6):424–427
Prins JTH, Van Lieshout EMM, Reijnders MRL, Verhofstad MHJ, Wijffels MME (2020) Rib fractures after blunt thoracic trauma in patients with normal versus diminished bone mineral density: a retrospective cohort study. Osteoporos Int 31(2):225–231
Lei M, Zhang M, Luo N et al (2022) The clinical performance of ultra-low-dose shoulder CT scans: the assessment on image and physical 3D printing models[J]. PLoS One 17(9):e0275297
Wall BF, Kendall GM, Edwards AA, Bouffler S, Muirhead CR, Meara JR (2014) What are the risks from medical X-rays and other low dose radiation? Br J Radiol 79(940):285–294. https://doi.org/10.1259/bjr/55733882
Cho SH, Sung YM, Kim MS (2012) Missed rib fractures on evaluation of initial chest CT for trauma patients: pattern analysis and diagnostic value of coronal multiplanar reconstruction images with multidetector row CT. Br J Radiol 85(1018):e845
Jang SW, Chung BM, Kim WT, Gil JR (2019) Nondisplaced fractures on hip CT: added value of dual-energy CT virtual non-calcium imaging for detection of bone marrow edema using visual and quantitative analyses. Acta Radiol 60(11):1465–1473
Wu S, Wang W, Zhang B et al (2021) A three-dimensional measurement based on CT for the posterior tilt with ideal inter-and intra-observer reliability in non-displaced femoral neck fractures. Comput Methods Biomech Biomed Eng 24(16):1854–1861
Johnson N, Leighton P; Distal Radius Fracture Delphi Study Group; Pailthorpe C, Dias J (2019) Defining displacement thresholds for surgical intervention for distal radius fractures–a Delphi study. PLoS One 14(1):e0210462
Konda SR, Goch AM, Leucht P et al (2016) The use of ultra-low-dose CT scans for the evaluation of limb fractures: is the reduced effective dose using ct in orthopaedic injury (REDUCTION) protocol effective? Bone Joint J 98(B-12):1668
Tekin E, Tuncer K, Ozlu I, Sade R, Pirimoglu RB, Polat G (2022) Ultra-low-dose computed tomography and its utility in wrist trauma in the emergency department. Acta Radiol 63(2):192–199
Acknowledgements
Grateful acknowledgement is made to Dr Rulin Xu (Cannon Medical Systems (China) Co., LTD) who gave me considerable help by means of suggestion.
Funding
This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
Author information
Authors and Affiliations
Contributions
JZY and MZ were involved in drafting the manuscript. ML, FHL, YXC were involved in acquisition of data and preparing the figures. JFL and JC designed the manuscript. MQX was involved in analysis and interpretation of data. MQX and JZY were involved in review and revise the manuscript. All authors have read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This study was approved by the institutional review board of Guangdong Provincial Hospital of Traditional Chinese Medicine (BF2019-030-01), and all patients provided written informed consent., and written informed consent was obtained from each patient or the patient’s family before performing the CT scan. This study was conducted in accordance with the Declaration of Helsinki.
Consent for publication
Written informed consent for publication was obtained from all participants.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
**ao, M., Zhang, M., Lei, M. et al. Diagnostic accuracy of ultra-low-dose CT compared to standard-dose CT for identification of non-displaced fractures of the shoulder, knee, ankle, and wrist. Insights Imaging 14, 40 (2023). https://doi.org/10.1186/s13244-023-01389-7
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13244-023-01389-7