Abstract
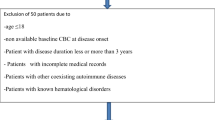
Multiple sclerosis (MS) is a prevalent chronic inflammatory disease of the CNS. There is a growing need for a reliable marker for MS diagnosis and disease monitoring. We aimed to assess the potential of the neutrophil-to-lymphocyte ratio (NLR) as a biomarker for MS diagnosis as well as the prediction of relapses and disability. We searched MEDLINE, Scopus, Web of Science, and Embase for relevant studies. The main outcome was the mean difference in NLR between MS patients and healthy controls and different subtypes of MS. We also calculated the sensitivity, specificity, positive likelihood ratio, negative likelihood ratio, and diagnostic odds ratio for NLR for diagnosis of MS and MS activity and disability. NLR was significantly higher in MS patients than in healthy controls (MD = 0.69; 95% CI, 0.48–0.9). Also, NLR was significantly higher during relapse than remission (MD = 1.26; 95% CI, 0.37–2.16). Regarding the performance of NLR as a marker for MS activity, its pooled sensitivity and specificity were 0.56 (95% CI 0.52–0.76) and 0.92 (95% CI 0.86–0.95), respectively; also, positive likelihood ration and negative likelihood ratio were 9.85 (95% CI 1.87–51.94) and 0.39 (95% CI 0.28–0.54) respectively. NLR can serve as an adjunctive biomarker for diagnosing MS and identifying relapse periods. However, the clinical utility of NLR in MS is yet to be confirmed by future large, prospective studies with longer follow-ups.



Similar content being viewed by others
Data Availability
Data available on request.
Code Availability
Available upon request.
Change history
09 March 2023
A Correction to this paper has been published: https://doi.org/10.1007/s42399-023-01440-0
References
Reich DS, Lucchinetti CF, Calabresi PA. Multiple sclerosis. N Engl J Med. 2018;378(2):169–80. https://doi.org/10.1056/NEJMra1401483.
Dobson R, Giovannoni G. Multiple sclerosis - a review. Eur J Neurol. 2019;26(1):27–40. https://doi.org/10.1111/ene.13819.
Vladić A, Horvat G, Vukadin S, Sucić Z, Simaga S. Cerebrospinal fluid and serum protein levels of tumour necrosis factor-alpha (TNF-alpha) interleukin-6 (IL-6) and soluble interleukin-6 receptor (sIL-6R gp80) in multiple sclerosis patients. Cytokine. 2002;20(2):86–9. https://doi.org/10.1006/cyto.2002.1984.
Ragab SM, Sarhan A, El Sayed D, Lotfy S, Zidan A. Serum lactate as a biomarker in multiple sclerosis. Zagazig Univ Med J. 2021;27(5):832–8. https://doi.org/10.21608/zumj.2019.14966.1352.
Abdel Naseer M, Rabah AM, Rashed LA, Hassan A, Fouad AM. Glutamate and nitric oxide as biomarkers for disease activity in patients with multiple sclerosis. Mult Scler Relat Disord. 2020;38:101873. https://doi.org/10.1016/j.msard.2019.101873.
Perry VH, Cunningham C, Holmes C. Systemic infections and inflammation affect chronic neurodegeneration. Nat Rev Immunol. 2007;7(2):161–7. https://doi.org/10.1038/nri2015.
Kamal A, Hosny M, AbdElwahab A, Shawki Kamal Y, Shehata HS, Hassan A. FOXP3rs3761548 gene variant and interleukin-35 serum levels as biomarkers in patients with multiple sclerosis. Rev Neurol (Paris). 2021;177(6):647–54. https://doi.org/10.1016/j.neurol.2020.07.010.
Imtiaz F, Shafique K, Mirza SS, Ayoob Z, Vart P, Rao S. Neutrophil lymphocyte ratio as a measure of systemic inflammation in prevalent chronic diseases in Asian population. Int Arch Med. 2012;5(1):2. https://doi.org/10.1186/1755-7682-5-2.
Brownlee WJ, Hardy TA, Fazekas F, Miller DH. Diagnosis of multiple sclerosis: progress and challenges. Lancet (London, England). 2017;389(10076):1336–46. https://doi.org/10.1016/S0140-6736(16)30959-X.
Gelibter S, et al. Neutrophil-to-lymphocyte ratio: a marker of neuro-inflammation in multiple sclerosis? J Neurol. 2021;268(2):717–23. https://doi.org/10.1007/s00415-020-10322-7.
Bisgaard AK, Pihl-Jensen G, Frederiksen JL. The neutrophil-to-lymphocyte ratio as disease actvity marker in multiple sclerosis and optic neuritis. Mult Scler Relat Disord. 2017;18:213–7. https://doi.org/10.1016/j.msard.2017.10.009.
Guzel I, Mungan S, Oztekin ZN, Ak F. Is there an association between the expanded disability status scale and inflammatory markers in multiple sclerosis? J Chin Med Assoc. 2016;79(2):54–7. https://doi.org/10.1016/j.jcma.2015.08.010.
Hasselbalch IC, et al. The neutrophil-to-lymphocyte ratio is associated with multiple sclerosis. Mult Scler J - Exp Transl Clin. 2018;4(4):2055217318813183. https://doi.org/10.1177/2055217318813183.
Fahmi RM, Ramadan BM, Salah H, Elsaid AF, Shehta N. Neutrophil-lymphocyte ratio as a marker for disability and activity in multiple sclerosis. Mult Scler Relat Disord. 2021;51: 102921. https://doi.org/10.1016/j.msard.2021.102921.
Page MJ, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ. 2021;372:n71. https://doi.org/10.1136/bmj.n71.
Lo CK-L, Mertz D, Loeb M. Newcastle-Ottawa Scale: comparing reviewers’ to authors’ assessments. BMC Med Res Methodol. 2014;14(1):45. https://doi.org/10.1186/1471-2288-14-45.
Ma L-L, Wang Y-Y, Yang Z-H, Huang D, Weng H, Zeng X-T. Methodological quality (risk of bias) assessment tools for primary and secondary medical studies: what are they and which is better? Mil Med Res. 2020;7(1):7. https://doi.org/10.1186/s40779-020-00238-8.
Yetkin MF, Mirza M. Neutrophil to-lymphocyte ratio as a possible predictor of prognosis in recently diagnosed multiple sclerosis patients. J Neuroimmunol. 2020;346: 577307. https://doi.org/10.1016/j.jneuroim.2020.577307.
D’Amico E, Zanghì A, Romano A, Sciandra M, Palumbo GAM, Patti F. The neutrophil-to-lymphocyte ratio is related to disease activity in relapsing remitting multiple sclerosis. Cells. 2019;8(10):1114. https://doi.org/10.3390/cells8101114.
Joisten N, et al. High-intensity interval training reduces neutrophil-to-lymphocyte ratio in persons with multiple sclerosis during inpatient rehabilitation. Mult Scler. 2021;27(7):1136–9. https://doi.org/10.1177/1352458520951382.
Saçmacı H, Aktürk T, Tanık N. The predictive value of the systemic immune-inflammation index as a new prognostic marker for disability in patients with multiple sclerosis. Turk J Neurol. 2021;27(2):133–9. https://doi.org/10.4274/tnd.2021.50329.
Goldman MD, Dwyer L, Coleman R, Sohn M-W, Stuve O (2020) Patient-specific factors modulate leukocyte response in dimethyl fumarate treated MS patients. PLoS One 15(2):e0228617. [Online]. Available: https://doi.org/10.1371/journal.pone.0228617
Akil E, Alp R, Aluclu MU, Acar A, Kaplan I. Serum endocan levels in multiple sclerosis relapse and remission. Eur Rev Med Pharmacol Sci. 2021;25(11):4091–8. https://doi.org/10.26355/eurrev_202106_26051.
Akaishi T, et al. White blood cell count profiles in multiple sclerosis during attacks before the initiation of acute and chronic treatments. Sci Rep. 2021;11(1):22357. https://doi.org/10.1038/s41598-021-01942-8.
Hemond CC, Glanz BI, Bakshi R, Chitnis T, Healy BC. The neutrophil-to-lymphocyte and monocyte-to-lymphocyte ratios are independently associated with neurological disability and brain atrophy in multiple sclerosis. BMC Neurol. 2019;19(1):23. https://doi.org/10.1186/s12883-019-1245-2.
Al-Hussain F, et al. Relationship between neutrophil-to-lymphocyte ratio and stress in multiple sclerosis patients. J Clin Diagn Res. 2017;11(5):CC01–4. https://doi.org/10.7860/JCDR/2017/24388.9764.
Benetou C, Berti F, Hemingway C, Hacohen Y, Lim M. Neutrophil-to-lymphocyte ratio correlates with disease activity in myelin oligodendrocyte glycoprotein antibody associated disease (MOGAD) in children. Mult Scler Relat Disord. 2020;45: 102345. https://doi.org/10.1016/j.msard.2020.102345.
Bolayir A, Cigdem B, Gokce SF, Yilmaz D. The relationship between neutrophil/lymphocyte ratio and uric acid levels in multiple sclerosis patients. Bratisl Lek Listy. 2021;122(5):357–61. https://doi.org/10.4149/BLL_2021_060.
CarneroContentti E, et al. Platelet-to-lymphocyte ratio differs between MS and NMOSD at disease onset and predict disability. Mult Scler Relat Disord. 2022;58:103507. https://doi.org/10.1016/j.msard.2022.103507.
Demirci S, Demirci S, Kutluhan S, Koyuncuoglu HR, Yurekli VA. The clinical significance of the neutrophil-to-lymphocyte ratio in multiple sclerosis. Int J Neurosci. 2016;126(8):700–6. https://doi.org/10.3109/00207454.2015.1050492.
Huang W-C, et al. Neutrophil-to-lymphocyte ratio and monocyte-to-lymphocyte ratio are associated with a 2-year relapse in patients with multiple sclerosis. Mult Scler Relat Disord. 2022;58: 103514. https://doi.org/10.1016/j.msard.2022.103514.
Hasselbalch IC, et al. The neutrophil-to-lymphocyte ratio is associated with multiple sclerosis. Mult Scler J. 2017;23(3):306–7. https://doi.org/10.1177/1352458517731404.
Gursoy AE, Renk ZC, Asil T (2017) Evaluation of neutrophil lymphocyte ratio in multiple sclerosis. Mult Scler J 23 MA-E, no. 7th Joint European-Committee-for-Treatment-and-Research-in-Multiple-Sclerosis (ECTRIMS)-Americas-Committee-for-Treatment-and-Research-in-Multiple-Sclerosis (ACTRIMS):778
Ekmekyapar Firat Y, Neyal AM, GünelKaradeniz P. Association between hematological inflammatory markers and attack period in multiple sclerosis: retrospective study. Turkiye Klin J Med Sci. 2021;41(4):431–7. https://doi.org/10.5336/medsci.2021-84574.
Berti FB, Benetou CB, Hemingway CH, Hacohen YH, Lim ML. Neutrophil-to-lymphocyte ratio as a biomarker to differentiate paediatric MOG+ recurrent demyelinating syndrome from multiple sclerosis. Dev Med Child Neurol. 2019;61:9. https://doi.org/10.1111/dmcn.14119.
Olsson A, et al. Neutrophil-to-lymphocyte ratio and CRP as biomarkers in multiple sclerosis: a systematic review. Acta Neurol Scand. 2021;143(6):577–86. https://doi.org/10.1111/ane.13401.
Dirican N, Anar C, Kaya S, Bircan HA, Colar HH, Cakir M. The clinical significance of hematologic parameters in patients with sarcoidosis. Clin Respir J. 2016;10(1):32–9. https://doi.org/10.1111/crj.12178.
Celikbilek M, et al. Neutrophil-lymphocyte ratio as a predictor of disease severity in ulcerative colitis. J Clin Lab Anal. 2013;27(1):72–6. https://doi.org/10.1002/jcla.21564.
Zengin O, et al. New inflammatory markers in early rheumatoid arthritis. Z Rheumatol. 2018;77(2):144–50. https://doi.org/10.1007/s00393-016-0187-y.
Akıl E, Bulut A, Kaplan İ, Özdemir HH, Arslan D, Aluçlu MU. The increase of carcinoembryonic antigen (CEA), high-sensitivity C-reactive protein, and neutrophil/lymphocyte ratio in Parkinson’s disease. Neurol Sci Off J Ital Neurol Soc Ital Soc Clin Neurophysiol. 2015;36(3):423–8. https://doi.org/10.1007/s10072-014-1976-1.
Kuyumcu ME, et al. The evaluation of neutrophil-lymphocyte ratio in Alzheimer’s disease. Dement Geriatr Cogn Disord. 2012;34(2):69–74. https://doi.org/10.1159/000341583.
De Bondt M, Hellings N, Opdenakker G, Struyf S. Neutrophils: underestimated players in the pathogenesis of multiple sclerosis (MS). Int J Mol Sci. 2020;21(12):4558. https://doi.org/10.3390/ijms21124558.
Steinbach K, Piedavent M, Bauer S, Neumann JT, Friese MA. Neutrophils amplify autoimmune central nervous system infiltrates by maturing local APCs. J Immunol. 2013;191(9):4531–9. https://doi.org/10.4049/jimmunol.1202613.
Woodberry T, Bouffler SE, Wilson AS, Buckland RL, Brüstle A. The emerging role of neutrophil granulocytes in multiple sclerosis. J Clin Med. 2018;7(12):511. https://doi.org/10.3390/jcm7120511.
Tillack K, et al. Gender differences in circulating levels of neutrophil extracellular traps in serum of multiple sclerosis patients. J Neuroimmunol. 2013;261(1–2):108–19. https://doi.org/10.1016/j.jneuroim.2013.05.004.
Pierson ER, Wagner CA, Goverman JM. The contribution of neutrophils to CNS autoimmunity. Clin Immunol. 2018;189:23–8. https://doi.org/10.1016/j.clim.2016.06.017.
Naegele M, Tillack K, Reinhardt S, Schippling S, Martin R, Sospedra M. Neutrophils in multiple sclerosis are characterized by a primed phenotype. J Neuroimmunol. 2012;242(1–2):60–71. https://doi.org/10.1016/j.jneuroim.2011.11.009.
Ziaber J, PaSnik J, Baj Z, Pokoca L, Chmielewski H, Tchórzewski H. The immunoregulatory abilities of polymorphonuclear neutrophils in the course of multiple sclerosis. Mediators Inflamm. 1998;7: 592917. https://doi.org/10.1080/09629359890857.
Musubire AK, et al. Epidemiology of non-traumatic spinal cord injury in Uganda: a single center, prospective study with MRI evaluation. BMC Neurol. 2019;19(1):10. https://doi.org/10.1186/s12883-019-1236-3.
Author information
Authors and Affiliations
Contributions
• Anas Elgenidy: data collection, analysis, screening, and scientific writing.
• Mostafa Atef, Abdelrahman Nasar, and Huzaifa: screening, data collection, and scientific writing.
• Abdullah Emad, and Islam salah: data collection, and scientific writing.
• Yousef Sonbol, Ahmed M. Afifi, Sherief Ghozy, and Amr Hassan: scientific writing, revision, and drafting of the manuscript.
Corresponding authors
Ethics declarations
Ethics Approval
NA.
Consent to Participate
Not applicable.
Consent for Publication
Not applicable.
Conflict of Interest
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on Medicine.
The original online version of this article was revised to correct the third author's family name.
Supplementary Information
Below is the link to the electronic supplementary material.
Appendix 1.
Search strategy (DOCX 16 kb)
Appendix 2.
Quality assessment of cohort studies (NIH Quality Assessment tool). Appendix 3. Risk of bias assessment for Case control studies (Newcastle–Ottawa Quality Assessment Scale criteria). Appendix 4. Quality assessment of Randomized controlled trials (NIH Quality Assessment tool) (DOCX 29 kb)

Appendix 5.
DTA for diagnosis MS (PNG 78 kb)

Appendix 6.
DTA for MS activity (PNG 53 kb)

Appendix 7.
DTA for MS disability (PNG 67 kb)

Appendix 8.
Leave-one-out for analysis comparing MS VS HC (PNG 235 kb)

Appendix 9.
Sensitivity analysis (PNG 59 kb)

Appendix 10.
Leave-one-out for analysis comparing Relapes VS Remission (PNG 81 kb)

Appendix 11.
funnel plot for MS VS HC. (PNG 86 kb)
Appendix 12.
References for the included studies (DOCX 17 kb)
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Elgenidy, A., Atef, M., Nassar, A. et al. Neutrophil-to-Lymphocyte Ratio: a Marker of Neuro-inflammation in Multiple Sclerosis Patients: a Meta-analysis and Systematic Review. SN Compr. Clin. Med. 5, 68 (2023). https://doi.org/10.1007/s42399-022-01383-y
Accepted:
Published:
DOI: https://doi.org/10.1007/s42399-022-01383-y