Abstract
Purpose
This study aimed to examine the modifiable predictors of T2DM and the roles of insulin resistance (IR) and β-cell function over a 6-year study and 30-year follow-up.
Methods
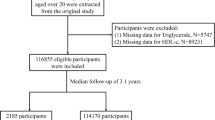
A total of 462 non-diabetic participants, 282 with impaired glucose tolerance (IGT), and 180 with normal glucose tolerance (NGT) were enrolled in this analysis. The Matsuda IR index and area under the curve of insulin-to-glucose ratio (AUCI/G-R) were used as IR and β-cell function indices in the analysis.
Results
In all participants, multivariable analysis showed that BMI, glucose status, Matsuda IR index and systolic blood pressure (SBP) at baseline were independently associated with an increased risk of T2DM over 30 years, whereas lifestyle intervention and AUCI/G-R were inversely associated with this risk. The predictive effect of the Matsuda IR index and AUCI/G-R in participants with IGT was consistent with the results of all participants, whereas in those with NGT, only the Matsuda IR index, not the AUCI/G-R, predicted the development of T2DM (HR = 1.42, 95% CI 1.07–1.89 vs HR = 1.09, 95% CI 0.76–1.56). The predictive effect of the Matsuda IR index on T2DM existed even in participants with BMI < 25 (p = 0.049).
Conclusion
The modifiable predictors of T2DM in Chinese adults were high BMI, hypertension, mild hyperglycaemia, IR, and β-cell dysfunction. Both IR and β-cell function contributed to the development of T2DM in the long term; however, IR remains the initial and long-standing key risk factor for T2DM.

Similar content being viewed by others
Data availability
All data used to support the findings of this research are available on request from the corresponding author.
References
Saeedi P, Petersohn I, Salpea P et al (2019) Global and regional diabetes prevalence estimates for 2019 and projections for 2030 and 2045: results from the international diabetes federation diabetes atlas, 9th edition. Diabetes Res Clin Pract 157:107843. https://doi.org/10.1016/j.diabres.2019.107843
Yudkin JS, Montori VM (2014) The epidemic of pre-diabetes: the medicine and the politics. BMJ 349:g4485. https://doi.org/10.1136/bmj.g4485
Souza CF, Gross JL, Gerchman F, Leitão CB (2012) Pre-diabetes: diagnosis, evaluation and treatment of chronic complications. Arq Bras Endocrinol Metabol 56(5):275–284. https://doi.org/10.1590/s0004-27302012000500001
Gerstein HC, Miller ME, Action to Control Cardiovascular Risk in Diabetes Study Group et al (2008) Effects of intensive glucose lowering in type 2 diabetes. N Engl J Med 358(24):2545–2559. https://doi.org/10.1056/NEJMoa0802743
Tuomilehto J, Lindström J, Eriksson JG et al (2001) Prevention of type 2 diabetes mellitus by changes in lifestyle among subjects with impaired glucose tolerance. N Engl J Med 344(18):1343–1350. https://doi.org/10.1056/NEJM200105033441801
Diabetes Prevention Program Research Group (2002) Reduction in the incidence of type 2 diabetes with lifestyle intervention or metformin. N Engl J Med 346(6):393–403. https://doi.org/10.1056/NEJMoa012512
Pan XR, Li GW, Hu YH et al (1997) Effects of diet and exercise in preventing NIDDM in people with impaired glucose tolerance: the Da Qing IGT and diabetes study. Diabetes Care 20(4):537–544. https://doi.org/10.2337/diacare.20.4.537
Lorenzo C, Hazuda HP, Haffner SM (2012) Insulin resistance and excess risk of diabetes in Mexican-Americans: the San Antonio heart study. J Clin Endocrinol Metab 97(3):793–799. https://doi.org/10.1210/jc.2011-2272
Weyer C, Tataranni PA, Bogardus C, Pratley RE (2001) Insulin resistance and insulin secretory dysfunction are independent predictors of worsening of glucose tolerance during each stage of type 2 diabetes development. Diabetes Care 24(1):89–94. https://doi.org/10.2337/diacare.24.1
Kodama K, Tojjar D, Yamada S et al (2013) Ethnic differences in the relationship between insulin sensitivity and insulin response: a systematic review and meta-analysis. Diabetes Care 36(6):1789–1796. https://doi.org/10.2337/dc12-1235
Torréns JI, Skurnick J, Davidow AL et al (2004) Ethnic differences in insulin sensitivity and beta-cell function in premenopausal or early perimenopausal women without diabetes: the study of women’s health across the nation (SWAN). Diabetes Care 27(2):354–361. https://doi.org/10.2337/diacare.27.2.354
Møller JB, Pedersen M, Tanaka H et al (2014) Body composition is the main determinant for the difference in type 2 diabetes pathophysiology between Japanese and Caucasians. Diabetes Care 37(3):796–804. https://doi.org/10.2337/dc13-0598
Ahuja V, Kadowaki T, Evans RW et al (2015) Comparison of HOMA-IR, HOMA-β% and disposition index between US white men and Japanese men in Japan: the ERA JUMP study. Diabetologia 58(7):265–271. https://doi.org/10.1007/s00125-015-3612-x
Møller JB, Dalla Man C, Overgaard RV et al (2014) Ethnic differences in insulin sensitivity, β-cell function, and hepatic extraction between Japanese and Caucasians: a minimal model analysis. J Clin Endocrinol Metab 99(11):4273–4280. https://doi.org/10.1210/jc.2014-1724
PrayGod G, Filteau S, Range N et al (2021) β-cell dysfunction and insulin resistance in relation to pre-diabetes and diabetes among adults in north-western Tanzania: a cross-sectional study. Trop Med Int Health 26(4):435–443. https://doi.org/10.1111/tmi.13545
Yoshinari M, Hirakawa Y, Hata J et al (2021) Comparison of the contributions of impaired beta cell function and insulin resistance to the development of type 2 diabetes in a Japanese community: the Hisayama Study. Diabetologia 64(8):1775–1784. https://doi.org/10.1007/s00125-021-05459-7
Narayan KMV, Kondal D, Daya N et al (2021) Incidence and pathophysiology of diabetes in South Asian adults living in India and Pakistan compared with US blacks and whites. BMJ Open Diabetes Res Care 9(1):e001927. https://doi.org/10.1136/bmjdrc-2020-001927
Wang L, Gao P, Zhang M et al (2017) Prevalence and ethnic pattern of diabetes and prediabetes in China in 2013. JAMA 317(24):2515–2523. https://doi.org/10.1001/jama.2017.7596
Li G, Zhang P, Wang J et al (2008) The long-term effect of lifestyle interventions to prevent diabetes in the China Da Qing Diabetes prevention study: a 20-year follow-up study. Lancet 371(9626):1783–1789. https://doi.org/10.1016/S0140-6736(08)60766-7
Gong Q, Zhang P, Wang J et al (2019) Morbidity and mortality after lifestyle intervention for people with impaired glucose tolerance: 30-year results of the Da Qing diabetes prevention outcome study. Lancet Diabetes Endocrinol 7(6):452–461. https://doi.org/10.1016/S2213-8587(19)300
An Y, Zhang P, Wang J et al (2015) Cardiovascular and all-cause mortality over a 23-year period among Chinese with newly diagnosed diabetes in the Da Qing IGT and diabetes study. Diabetes Care 38(7):1365–1371. https://doi.org/10.2337/dc14-2498
World Health Organization (1985) Diabetes mellitus: report of a WHO study group—technical report no 727. World Health Organization, Geneva
World Health Organization (1999) Definition and classification of diabetes mellitus and its complications. In: Report of a who consultation. Part 1: diagnosis and classification of diabetes mellitus. WHO, Department of noncommunicable disease surveillance, Geneva
Gong Q, Zhang P, Wang J et al (2016) Changes in mortality in people with IGT before and after the onset of diabetes during the 23-year follow-up of the Da Qing diabetes prevention study. Diabetes Care 39(9):1550–1555. https://doi.org/10.2337/dc16-0429
Matsuda M, DeFronzo RA (1999) Insulin sensitivity indices obtained from oral glucose tolerance testing: comparison with the euglycemic insulin clamp. Diabetes Care 22(9):1462–1470. https://doi.org/10.2337/diacare.22.9.1462
Santos JL, Yévenes I, Cataldo LR et al (2016) Development and assessment of the disposition index based on the oral glucose tolerance test in subjects with different glycaemic status. J Physiol Biochem 72(2):121–131. https://doi.org/10.1007/s13105-015-0458-0
Oka R, Yagi K, Hayashi K et al (2014) The evolution of non-diabetic hyperglycemia: a longitudinal study. Endocr J 61(1):91–99. https://doi.org/10.1507/endocrj.ej13-0359
Hanley AJ, Wagenknecht LE, Norris JM et al (2009) Insulin resistance, beta cell dysfunction and visceral adiposity as predictors of incident diabetes: the insulin resistance atherosclerosis study (IRAS) family study. Diabetologia 52(10):2079–2086. https://doi.org/10.1007/s00125-009-1464-y
Welsh P, Preiss D, Lloyd SM et al (2014) Contrasting associations of insulin resistance with diabetes, cardiovascular disease and all-cause mortality in the elderly: PROSPER long-term follow-up. Diabetologia 57(12):2513–2520. https://doi.org/10.1007/s00125-014-3383-9
Morimoto A, Tatsumi Y, Deura K et al (2013) Impact of impaired insulin secretion and insulin resistance on the incidence of type 2 diabetes mellitus in a Japanese population: the Saku study. Diabetologia 56(8):1671–1679. https://doi.org/10.1007/s00125-013-2932-y
Derakhshan A, Tohidi M, Arshi B et al (2015) Relationship of hyperinsulinaemia, insulin resistance and beta-cell dysfunction with incident diabetes and pre-diabetes: the Tehran lipid and glucose study. Diabet Med 32(1):24–32
Wu WC, Wei JN, Chen SC et al (2020) Progression of insulin resistance: a link between risk factors and the incidence of diabetes. Diabetes Res Clin Pract 161:108050. https://doi.org/10.1016/j.diabres.2020
Li CL, Tsai ST, Chou P (2003) Relative role of insulin resistance and beta-cell dysfunction in the progression to type 2 diabetes-The Kinmen Study. Diabetes Res Clin Pract 59(3):225–232. https://doi.org/10.1016/s0168-8227(02)00249-8
Trial Investigators DREAM, Gerstein HC, Yusuf S et al (2006) Effect of rosiglitazone on the frequency of diabetes in patients with impaired glucose tolerance or impaired fasting glucose: a randomized controlled trial. Lancet 368(9541):1096–1105. https://doi.org/10.1016/S0140-6736(06)
Defronzo RA, Banerji M, Bray GA et al (2009) Actos now for the prevention of diabetes (ACT NOW) study. BMC Endocr Disord 9:17. https://doi.org/10.1186/1472-6823-9-17
Holman RR, Haffner SM, NAVIGATOR Study Group et al (2010) Effect of nateglinide on the incidence of diabetes and cardiovascular events. N Engl J Med 362(16):1463–1514. https://doi.org/10.1056/NEJMoa1001122
Acknowledgements
The authors thank all the participants who took part in the original Da Qing IGT and Diabetes Study, the Da Qing Diabetes Prevention Study, and the Da Qing Diabetes Prevention Follow-up Study. The authors thank Peter H. Bennett who provided advice about the manuscript. We also thank late Professor **aoren Pan, as this study would not have been possible without his leadership in the design and implementation of the original DQDPS.
Funding
The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: the National Center for Chronic Disease Prevention and Health Promotion through CDC/WHO Cooperative Agreement No. U58/CCU424123-01–02 and the China-Japan Friendship Hospital.
Author information
Authors and Affiliations
Contributions
GL and HG: contributed to the conception and design of the work; data analysis, and revising of the paper. XS: involved in data analysis and drafted the article; SH and JW: involved data management, XQ, HW, BZ, YC, and LA: participated in data acquisition; HL: designed and supervised the study. All authors gave the final approval of the version published.
Corresponding authors
Ethics declarations
Conflict of interest
The authors declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Ethical approval and consent to participate
The Human Ethics Committee of China-Japan Friendship Hospital and Fuwai Hospital approved the study, and written informed consent was obtained from all participants
Informed consent
Informed consent was obtained from all individual participants included in the study.
Consent for publication
Not applicable.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Shen, X., He, S., Wang, J. et al. Modifiable predictors of type 2 diabetes mellitus and roles of insulin resistance and β-cell function over a 6-year study and 30-year follow-up. J Endocrinol Invest 46, 883–891 (2023). https://doi.org/10.1007/s40618-022-01932-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40618-022-01932-1