Abstract
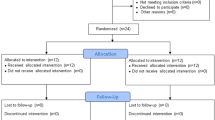
This study was conducted to investigate the effectiveness of Matrix rhythm therapy (MRT) on muscle tone, balance and gait parameters in stroke survivors. Thirty stroke individuals randomly assigned to study and control group received combining BT&MRT, and BT, respectively. This study was a single-blinded (assessor-blind), randomized controlled trial. A total of 30 stroke individuals with spastic hemiparesis (n = 30) aged between 20–65 years were included. The study group received combining BT and MRT on trunk and the affected lower limb. The control group received only BT. Participants in both groups were received therapy for 4 weeks, 3 days/week. The outcome measures were Modified Ashworth Scale (MAS), goniometric measurements (ROM), Single Leg Stance Test of the BESTest Balance Evaluation System, Timed “Get Up & Go” Test of the BESTest and BTS G-Walk Gait-Analysis System. Spasticity intensity, ROM, static/dynamic balance tests’ scores, gait velocity, cadence, and pelvic movement symmetries improved in study group (p < 0.05).In the control group, only dynamic balance improved after the treatment program(p < 0.05). Significant improvements were found in terms of spasticity intensity, ROM of knee and ankle joints, static/dynamic balance, gait velocity and cadence in favor of the study group (p < 0.05). This study gives preliminary evidence that adding MRT to BT may be beneficial in improving balance and gait by regulating muscle tone in the affected lower limb of stroke patients with spastic hemiparesis. The study was retrospectively registered at Clinical Trials.gov (ID: NCT04213417; URL: www.clinicaltrials.gov).


Similar content being viewed by others
References
Kulcu DG, Yanık B, Gılsen G (2009) The relationship betweeen balance disorders and upper extremity function in hemiplegic patients. J PMR Sci 12:1–6
Mauritz KH (2004) Gait training in hemiparetic stroke patients. Eura Medicophys 40:165–178
Duncan PW, Zorowitz R, Bates B, Choi JY, Glasberg JJ, Graham GD, Katz RC, Lamberty K, Reker D (2005) Management of adult stroke rehabilitation care: a clinical practice guideline. Stroke 36:100–143
Díaz-Arribas MJ, Martín-Casas P, Cano-de-la-Cuerda R, Plaza-Manzano G (2019) Effectiveness of the Bobath concept in the treatment of stroke: a systematic review. Disabil Rehabil 1–14
Kollen BJ, Lennon S, Lyons B et al (2009) The effectiveness of the Bobath concept in stroke rehabilitation: what is the evidence? Stroke 40:89–97
Prabhu RK, Swaminathan N, Harvey LA (2013) Passive movements for the treatment and prevention of contractures. Cochrane Database Syst Rev 12:1–31
Stein C, Fritsch CG, Robinson C et al (2015) Effects of electrical stimulation in spastic muscles after stroke: systematic review and metaanalysis of randomized controlled trials. Stroke 46:2197–2205
Cai Y, Zhang CS, Liu S et al (2017) (2017) Electro-acupuncture for post-stroke spasticity: a systematic review and meta-analysis. Arch Phys Med Rehabil 98:2578–2589
Randoll UG, Cutcheon R, Hennig FF (2006) Matrix-Rhythmus-Therapie und der Ostepatiche Ansatz. Osteopathische Medizin 7:28–34
Randoll UG (2015) How principles of Matrix rhythm therapy. Verlag Sistemiche Medizin, Germany
Jager PA, Chan D, Muderrisoglu HF (2008) Matriks ritm terapisinin sırt ve bel ağrılı hastalardaki etkisi. Fizyoterapi ve Rehabilitasyon 19:217
Naik V, Bhagwat S, Pathania T, Bootwala F (2018) Effectiveness of matrix rhythm therapy in frozen shoulder with respect to ROM and pain—an experimental study. Int J of Appl Res 4:73–76
Matriks Center Turkey Patient Reports (2018) https://matrixcenterturkiye.net/multi_icerik46cb.html?no=16. Accessed 14 November 2018
Taspinar F, Aslan UB, Sabir N, Cavlak U (2013) Implementation of matrix rhythm therapy and conventional massage in young females and comparison of their acute effects on circulation. J Altern Complement Med 19:826–832
Bhatikar K (2018) Effect of Matrix rhythm therapy in B/L adductor muscle tightness in pediatric cerebral palsy: a case report. J Palliat Care Med 9(1):1–3
Eser F, Aksel J, Karakus D (2004) Gait characteristics and role of gait analysis in hemiplegia after stroke. Fiziksel Tıp 7:39–42
Cavlak U, Altug F, Akman TC, Unal A, Duray M (2018) Inmeli hastalarda yuruyus ve yuruyus rehabilitasyonu. In: Erbahceci F, Bayramlar K (eds) Yuruyus. Hipokrat Publishing, Ankara, pp 247–293
van Swieten JC, Koudstaal PJ, Visser MC et al (1988) Interobserver agreement for the assessment of handicap in stroke patients. Stroke 19(5):604–607
Damiano DL, Quinlivan JM, Owen BF et al (2002) What does the Ashworth scale really measure and are instrumented measures more valid and precise? Dev Med Child Neurol 44:112–118
Bohannon RW, Smith MB (1987) Interrater reliability of a modified Ashworth scale of muscle spasticity. Phys Ther 67(2):206–207
Bravo-Esteban E, Taylor J, Aleixandre M et al (2014) Tibialis anterior muscle coherence during controlled voluntary activation in patients with spinal cord injury: diagnostic potential for muscle strength, gait and spasticity. J Neuroeng Rehabil 11:23. https://doi.org/10.1186/1743-0003-11-23
Barroso FO, Torricelli D, Bravo-Esteban E et al (2016) Muscle synergies in cycling after incomplete spinal cord injury: correlation with clinical measures of motor function and spasticity. Front Hum Neurosci 9:706
Reiter F, Danni M, Lagalla G et al (1998) Low-dose botulinum toxin with ankle ta** for the treatment of spastic equinovarus foot after stroke. Arch Phys Med Rehabil 79:532–535
Gouveia VHDO, Araújo AGDF, Maciel SDS et al (2014) Reliability of the measures inter and intra-evaluators with universal goniometer and fleximeter. Fisioterapia e Pesquisa 21(3):229–235
dos Santos CM, Ferreira G, Malacco PL et al (2012) Intra and inter examiner reliability and measurement error of goniometer and digital inclinometer use. Revista Brasileira de Medicina do Esporte 18(1):38–41
Rodrigues LC, Marques AP, Barros PB et al (2014) Reliability of the Balance Evaluation Systems Test (BESTest) and BESTest sections for adults with hemiparesis. Braz J Phys Ther 18(3):276–281
Chinsongkram B, Chaikeeree N, Saengsirisuwan V et al (2014) Reliability and validity of the balance evaluation systems test (BESTest) in people with subacute stroke. Phys Ther 94(11):1632–1643
Horak FB, Wrisley DM, Frank J (2009) The balance evaluation systems test (BESTest) to differentiate balance deficits. Phys Ther 89:484–498
Wren TA, Gorton GE, Ounpuu S et al (2011) Efficacy of clinical gait analysis: a systematic review. Gait and Posture 34:149–153
Sumbuloglu K, Sumbuloglu V (2004) Biyoistatistik. Hatiboglu Publishing, Ankara
Li S (2017) Spasticity, motor recovery, and neural plasticity after stroke. Front Neurol 8:1–8
Langhorne P, Coupar F, Pollock A (2009) Motor recovery after stroke: a systematic review. Lancet Neurol 8:741–754
Hara T, Abo M, Hara H et al (2018) (2018) Effects of botulinum toxin A therapy and multidisciplinary rehabilitation on lower limb spasticity classified by spastic muscle echo intensity in post-stroke patients. Int J Neurosci 128:412–420
Gupta AD, Chu WH, Howell S et al (2018) A systematic review: efficacy of botulinum toxin in walking and quality of life in post-stroke lower limb spasticity. Syst Rev 7:1
Sabut SK, Sikdar C, Kumar R et al (2011) Functional electrical stimulation of dorsiflexor muscle: effects on dorsiflexor strength, plantarflexor spasticity, and motor recovery in stroke patients. NeuroRehabilitation 29:393–400
Aslan SY (2018) The effect of extracorporeal shock wave therapy on the spasticity of ankle plantar flexor muscles in poststroke patients. Dissertation, Ankara University Faculty of Medicine
Celik D, Turkel N, Atalar AC (2016) Comparison of matrix rhythm therapy and stretching exercises on frozen shoulder: randomised controlled trial. Fiz Rehabil 27:81–88
Sánchez-Mila Z, Salom-Moreno J, Fernández-de-las-Peñas C (2018) Effects of dry needling on post-stroke spasticity, motor function and stability limits: a randomised clinical trial. Acupunct Med 36:358–366
Miyara K, Matsumoto S, Uema T et al (2014) Feasibility of using whole body vibration as a means for controlling spasticity in post-stroke patients: a pilot study. Complement Ther Clin Pract 20:70–73
Cekmece C. The effects of whole treatment on upper and lower limb functions with stroke. Dissertation, Kocaeli University Health Sciences Institute
Funding
This study was supported by the Pamukkale University Scientific Research Commission (Grant no. 2017SABE012, 2019KKP100).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
All the authors declare that they have no conflict of interest, and they have nothing to disclose.
Ethical approval
This study was performed in line with the principles of the Declaration of Helsinki. Approval was granted by Pamukkale University Medical Ethics Committee of Non-Interventional Clinical Researches (Ref. 27.12.2016/no: 81261). The study was retrospectively registered at Clinical Trials.gov (ID: NCT04213417; URL: www.clinicaltrials.gov).
Informed consent
Written informed consent was obtained from all subjects.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Unal, A., Altug, F., Tikac, G. et al. Effectiveness of matrix-rhythm therapy on increased muscle tone, balance and gait parameters in stroke survivors: a single-blinded, randomized, controlled clinical trial. Acta Neurol Belg 121, 689–699 (2021). https://doi.org/10.1007/s13760-020-01391-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13760-020-01391-6