Abstract
Stroke patients have gait dysfunctions that affect their activities of daily living. Stroke patients should be able to take multi-directional steps as it is necessary to achieve an independent gait. The study aimed to examine the effects of multi-directional step exercises (MSE) along with weight-shifting as an adjunct to conventional therapeutic exercises (CTE) on functional gait performance and balance in patients with stroke. Twenty-four stroke patients (mean age 56.75 years) participated in the study and were divided into experimental and control groups. The experimental group (EG) included MSE along with weight shifting and CTE. The control group (CG) included only CTE. Treatment intervention lasted for 4 weeks. Gait and balance were measured using the functional gait assessment (FGA) and the berg balance scale (BBS), respectively. EG showed a significant improvement (p = 0.000) in both the BBS and FGA scores. In CG, a significant improvement (p = 0.000) was observed only in FGA scores. EG showed a greater improvement in scores of BBS (p = 0.000) and FGA (p = 0.000) than CG. Four weeks of MSE in conjunction with CTE were more effective in improving balance and functional gait performance compared to CTE alone in the selected stroke population.
Similar content being viewed by others
Introduction
Stroke is one of the major causes of permanent disability1. Stroke can have many causes and occurs mainly in old age, although it can occur at any age2. Most stroke survivors can perform limited activities of daily living (ADL) due to motor, sensory, emotional, and cognitive impairments3. Stroke patients commonly exhibit symptoms of hemiplegia and thus, as a result, have defects in voluntary movements, asymmetrical weight-shifts, gait, and body balance4. Stroke patients have decreased balance ability due to their centre of gravity shifting towards the unaffected side4. In the standing posture, approximately 61% to 80% of their body weight is concentrated on the unaffected lower extremity5. Due to these asymmetric postures, stroke patients may have frequent falls, limited independent gait, and reduced gait velocity6. This asymmetric gait in hemiplegic patients may cause reduced bone density on the affected side and an overall increase in energy expenditure on walking7,8. In addition to normal walking, stroke survivors fall during transfers between beds and the wheelchair and during standing turns9,10. These gait dysfunctions after stroke are the main cause of impaired functional ambulation, which in turn causes decreased social participation and poor quality of life. Therefore, enhancing the tolerance and capability to bear weight on the affected lower extremity and achieving good body balance during various functional activities and symmetric gait patterns are the main goals of rehabilitation for stroke patients11,12,13.
Multi-directional steps are essential for ADL because, while walking indoors, 35–50% of all steps consist of those steps that change the direction of movement, i.e. non-straight steps14. Normal individuals and stroke patients should have the ability to take steps in multiple directions to perform ADL safely. In previous studies, step training in various directions has been reported to improve balance and gait in older people and patients with Parkinson’s disease15,16. The stroke patients also have impaired ability to bear weight on the paretic side in all three directions of a step, i.e. forward, backward and lateral17. Therefore, a rehabilitation program for stroke survivors should include multi-directional step exercises (MSE) and weight shifting training. One previous study by Park et al.4 compared the multi-directional step** training versus general physical therapy in stroke patients. Park et al. used two stair-shaped footholds (10 cm) and a weight rod for multi-directional step** training. They reported improvement in the berg balance scale (BBS), timed up and go (TUG) test, 10-m walk test, and fall efficacy scores after performing multi-directional step** training compared to general physical therapy. In their study, participants performed step** exercises over stair-shaped footholds and across the weight rod by the non-paretic side while kee** the paretic side fixed over the ground.
It will be interesting to examine the effects of MSE along with weight-shifting when performed by the paretic side of the participants while kee** the non-paretic side fixed over the ground. To the best of our knowledge, no study has examined these effects in stroke patients. Since it will be difficult for participants to take steps over a foothold by their paretic side, therefore, in the present study these exercises will be performed on the flat surface. Thus, this study was conceptualized to examine the effects of MSE along with weight-shifting when performed as an adjunct to conventional therapeutic exercises (CTE), on balance and functional gait performance in patients with stroke. We hypothesized that the addition of MSE along with weight-shifting to a 4-week program of CTE improves balance and functional gait performance in comparison to CTE alone in stroke patients.
Materials and methods
Participants' eligibility and ethical clearance
The study's sample size was calculated using the software G*Power18, version 3.1.9.4 (https://www.psychologie.hhu.de/arbeitsgruppen/allgemeine-psychologie-und-arbeitspsychologie/gpower). Mean difference, standard deviation, and effect size values were taken for variable BBS scores from the study of Park et al.4. Power was set at 0.95, and using the option of a two-tailed test, this calculation was done, which revealed 12 as the minimum total sample size. Therefore, 12 participants in each group were decided for recruitment, which made the total sample size 24.
Twenty-four patients with stroke were selected from the inpatient department of the Alva’s Health Centre hospital, Moodbidri, the Alva’s Ayurveda hospital, Vidhyagiri, and the outpatient department of the Alva’s College of Physiotherapy. The stroke was diagnosed by CT or magnetic resonance imaging. The recruited participants also had to have Mini-Mental status examination score greater than 21, the ability to maintain an independent standing posture for 30 s, should be able to walk independently without the use of an assistive device for at least 3 m, and could communicate and understand the therapist’s verbal commands. An expert physical therapist performed these examinations.
Participants who had a history of neurological pathologies (eg Alzheimer’s or Parkinson’s disease), visual deficits/disorders, concomitant medical disease (recent myocardial infarction, unstable angina, ventricular tachycardia), impaired balance, such as vertigo, dementia, impaired alertness, lower motor neuron lesion, severe orthopedic disease of the lower extremities, taking antispasmodic medications (eg Baclofen, Dantrolene sodium, etc.) or medications affecting balance were excluded from the study.
Ethics clearance was obtained from the ethics committee of Alva’s college of Physiotherapy (ACP/OP/2016/OL 06). All methods were performed in accordance with the relevant guidelines and regulations. The study was retrospectively registered on the public trial registry (ClinicalTrials.gov PRS; Registration No. NCT05285241 on 17/03/2022). Before the inclusion of participants in the study, the study details were explained to them, and written informed consent was obtained.
Study design, the protocol of the study, and randomization of participants
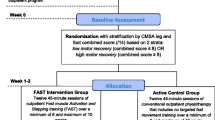
Two arms pretest–posttest experimental design was used. First, a detailed examination was performed that included the Mini-Mental State Examination (MMSE) to satisfy the inclusion and exclusion criteria. Two groups were formed: the experimental and the control group. The experimental group included MSE along with weight-shifting and CTE program while the control group included CTE program only. A physical therapy assistant, who did not measure the outcome measures, generated a random sequence and equally allotted the participants to two groups using the website randomization.com and lotteries. A total of 4 treatment sessions were given to each participant in both groups for a total of 4 weeks. The CTE sessions lasted approximately 45 min in both groups; however, in the experimental group, an additional 15 min was spent on MSE along with weight-shifting. Pre-test and post-test measurements of outcome measures were performed by the same physical therapist with 3 years of experience. The outcome assessor was kept blind to the allocation. Figure 1 includes the allocation and randomization of participants.
Materials required
-
20-foot walkway
-
Footstool or step
-
Two standard chairs, one with an armrest and the other without
-
Stairs with railing
-
Foot stepper
-
Stopwatch
-
Yardstick
-
Mirror
Outcome measures
-
Balance: measured by Berg Balance Scale (BBS)19.
-
Functional gait performance: measured by Functional Gait Assessment (FGA)20,21.
BBS consists of 14 items and can be used to quantitatively monitor the progression of balance in stroke patients19. It has high intra- and inter-rater reliability and validity22,23. For BBS measurement, the outcome assessor asked the participants to perform 14 predetermined tasks which were graded from 0 to 4 according to their performance. Therefore, in BBS, minimum and maximum possible scores are 0 and 56, respectively19. The lower the score, the more impaired the balance will be.
FGA assesses the patient’s ability to perform multiple tasks and postural stability while walking. This tool is a modified version of the dynamic gait index, consists of 10 items, and has good reliability and validity for assessing walking balance in stroke patients who can ambulate independently20,21. For FGA measurement, the outcome assessor asked the participants to perform 10 predetermined tasks, and according to their performance, these tasks were graded from 0 to 3. Therefore, in FGA, the minimum and maximum possible scores are 0 and 30, respectively, where the higher score indicates better functional gait performance and health-related quality of life24.
The outcome assessor measured outcome measures before the start of intervention for baseline values and after 4-weeks of intervention.
Interventions
Treatment intervention in both groups was performed for 4-weeks.
Experimental group
In this group, MSE and weight-shifting were performed along with CTE.
Conventional therapeutic exercises (CTE)
This included wall-supported gait training for around 10 min/session, functional mat exercises (supine to prone on the elbow, to prone on hand, to quadruped position, to kneeling, then at the end to standing, each position was maintained for 2 min) for around 10 min/session, stretching exercises (for hamstrings, quadriceps, gastrocnemius, glutei, elbow, and finger flexors, with 15–30 s hold for three repetitions for each muscle) for around 5 min/session, passive range of motion (ROM) exercises for the affected joints for about 10 min/session, active-assisted ROM exercises to progressive resistance exercises (PRE) with 10–15 s hold, 15 repetitions for affected muscles. Participants performed these exercises according to their abilities.
Multi-directional step exercises (MSE) along with weight-shifting
Participants were asked to stand barefoot with their hands on their sides. A mirror was placed in front of them for visual feedback. A physical therapy assistant stood beside them to support them in case of any balance disturbance. The first position is that stroke patients with hemiplegia have asymmetrical weight distribution between their lower extremities; therefore, they were asked to distribute their body weight between both lower extremities equally. In the second position, they had to take a sideway step with the affected lower extremity along with shifting their trunk towards the affected side, so that body weight passes through the affected foot. Then they had to return to the first position with an equal body weight distribution between both lower extremities. In the third position—they had to take a forward step with the affected lower extremity along with their trunk bending slightly forward so that the body weight passes through the forefoot of the affected side. Then they had to return to the first position. In the fourth position, they had to take a backward step along with shifting the trunk backwards so that body weight passed through the heel of the affected side. Then again, they had to return to the first position. Every position was to be maintained for 10 s each, and after completion of one set, a 2-min rest was given. This process had been repeated a total of three times.
Walking with wall support
Participants were asked to wear comfortable shoes and stand near the wall with the affected side towards it. A 3 cm wide and 10-m-long line was drawn parallel to the wall (20 cm away). The participants had to place their affected foot on the line while walking. Participants were instructed to touch the wall with their shoulders by shifting their trunks during the stance phase of the affected side. This way, the participants walked along the wall 10 times in one set. A total of 3 sets were performed with a 2-min rest between the sets.
Control group
Participants in this group performed CTE similar to the experimental group. In this group, participants also performed these exercises according to their abilities. These included wall-supported gait training for around 10 min/session, functional mat exercises for about 10 min/session, stretching exercises for about 5 min/session, passive range of motion (ROM) exercises for the affected joints for about 10 min/session, and active-assisted ROM exercises to progressive resistance exercises (PRE) with 10–15 s hold, 15 repetitions for affected muscles.
Data analysis
SPSS statistical software25, version 26 (SPSS Inc., Chicago, IL, USA), was used for statistical analysis (https://www.ibm.com/support/pages/downloading-ibm-spss-statistics-26). The distribution of baseline values of dependent variables was analyzed using the Shapiro–Wilk test of normality. The test showed a normal distribution for both groups' baseline values of BBS and FGA. Therefore, for further with-in and between-group analysis, parametric tests were used. With-in-group and between-group analyses were performed using the paired samples and independent samples test, respectively. The confidence interval was established at 95%, and p < 0.05 was considered significant.
Results
Demographic data and the p-values of the Shapiro–Wilk test of normality are presented in Table 1. This test revealed normal distribution for pre-intervention values of both variables; therefore, parametric tests were used for further with-in and between-group analyses.
With-in group analysis (paired samples test) (Table 2)
Experimental group
For BBS: a significant improvement in the BBS scores was observed in the experimental group from 41.91 to 50.83 (p = 0.000).
For FGA: a significant improvement in the FGA scores was observed in the experimental group from 10.58 to 20.66 (p = 0.000).
Control group
For BBS: no significant difference was observed in BBS scores in the control group (from 43.83 to 44.08) (p = 0.082).
For FGA scores: a significant improvement was observed in the FGA scores in the control group from 14.00 to 14.66 (p = 0.025).
Between-group analysis (independent samples test) (Table 3)
When both groups were compared, a significant difference was observed in the mean differences of both variables [BBS (p = 0.000) and FGA (p = 0.000)]. The experimental group (mean difference, BBS = 8.91; FGA = 10.08) showed a greater improvement in BBS and FGA scores than the control group (mean difference, BBS = 0.25; FGA = 0.66).
Discussion
The present study aimed to evaluate the effects of MSE along with weight-shifting on balance and functional gait performance in stroke patients when used as an adjunct to a 4-week CTE program. The results indicated that MSE along with weight-shifting, when performed in addition to a 4-week CTE program, was more effective in improving balance (BBS score) and gait performance (FGA score) than a CTE program alone in the selected stroke population. Significant improvement in FGA scores was also observed with the CTE program alone. However, a greater improvement was observed for both BBS and FGA scores after performing MSE along with weight-shifting in conjunction with the CTE program.
A combination of cognitive, emotional, sensory, and motor impairments occurs in patients after stroke26. These impairments limit the ability of stroke survivors to perform basic ADL3. 80% of patients with early-stage stroke lose their walking ability and begin to recover in 6 months. Stroke survivors commonly show hemiplegia symptoms leading to asymmetric weight-shifts, gait and body balance, and impaired voluntary movements. Their ability to bear weight on the paretic limb is impaired17. In stroke patients, the paretic limb has reduced ability of weight-shifting in three directions of a step, i.e. forward, backward and lateral and particularly greater loss in the forward direction17. Weight-bearing by the lower limbs is necessary for normal functional mobility in various directions and positions17. All these impairments, along with muscle weakness and loss of coordination, lead to gait dysfunction and reduced balance ability27. All these dysfunctions lead to decreased gait velocity, hampered independent gait, and may lead to falls6. Therefore, in patients with hemiplegic stroke, they must be confident that the lower limb of the affected side are ready and trained to bear the full body weight and generate the necessary muscle force to match the speed of the unaffected side28. Therefore, a few main goals of post-stroke rehabilitation are to enhance the weight-bearing capability and tolerance of the paretic limb during different tasks and to enhance the gait symmetry and independent gait thereby improving stroke patients' functions and social activities11,29.
Along with weight-shifting, multi-directional steps are also essential to gait during ADL. Stroke survivors should be able to take multi-directional steps to perform routine daily tasks. Therefore, to improve the ability of stroke patients to take multi-directional steps, i.e. steps in forward, lateral and backward directions and to enhance the weight-shifting ability, the MSE along with weight-shifting was added to the CTE program in the present study. The CTE program included AROM exercises, strengthening exercises, functional mat exercises, stretching exercises, and gait training.
The improvement observed in the present study in balance and functional gait performance is not surprising because an association between balance and weight-shifting has been reported previously. Eng and Chu17 suggested that poor balance in stroke patients may be due to the impairment in the weight-shifting ability of their hemiparetic side. The study by Jung et al.30 reported improved trunk control, trunk proprioception and balance by weight-shifting training on an unstable surface in chronic stroke patients. Learning to load and unload the paretic limb while standing is a crucial stage in the gait and balance training of stroke patients because the ability to start and control the voluntary weight-shifts toward either limb is a requirement for independent gait31. These previous studies already indicated an association between weight-shifting ability and balance in stroke patients; therefore, the improvements obtained in the present study were expected. BBS and FGA consist of different tasks which are related to each other. Improvement in one task may result in improvement in another task. For example, a study by Winstein et al.32 reported improved weight-bearing symmetry in standing after weight-shifting exercises. Similar findings supporting the association of tasks were also reported by Dean and Shephard33. Therefore, in the present study, MSE along with weight-shifting combined with the CTE program may have improved the ability of the hemiparetic side to take steps in different directions and bear more weight. Therefore, these improvements may have improved other tasks of BBS and FGA, resulting in an overall increment in scores.
One previous study by Park et al.4 reported similar results. They used multi-directional step** training for 6 weeks, using two footholds and a weight rod for the non-paretic side in stroke patients and used BBS, TUG, 10-m walk test, and falls efficacy scale scores as outcome measures. They reported improvement in all outcome measures in comparison to the control group. However, the practical applicability of Park et al.’s study is not similar to the present study as they used step** exercises by the non-paretic side of the patients however, in the present study step** exercises were performed by the paretic side of the patients.
Another recently performed study by Choi and Kim34 compared the combined effects of multi-directional step-up training along with rhythmic auditory stimulation versus the multi-directional step-up training alone in stroke patients. Their effects were assessed on gait and balance ability. They concluded that multi-directional step-up training alone or with rhythmic auditory stimulation could improve balance and gait in stroke patients. However, greater improvement can be achieved when multi-directional step-up training is accompanied by rhythmic auditory stimulation.
Most studies that have been conducted on the improvement of balance and functional gait performance in stroke population have used lavish equipment like force plate systems, gyroscopes etc. However, the exercises performed in the present study are extremely easy and convenient to follow up even in a community step-up without any use of appliances. Therefore, the physical therapist may consider adding MSE along with weight-shifting to the CTE program of stroke rehabilitation as it does not require sophisticated equipment and can easily be performed by stroke patients.
There is some scope for future studies and limitations in the present study. Firstly, stroke patients, irrespective of their disease duration, were recruited for the study. Acute stroke patients may respond differently to exercise protocol than chronic stroke patients. Also, depending upon the side, site and severity of the lesion in the brain, participants' responses to exercises may differ. Therefore, future studies may consider these factors while recruiting participants and designing their protocol. The sample size was not large, and no long-term follow-up was performed. Improvements gained with the addition of MSE and weight-shifting may be temporary and short-lived; therefore, future studies should include a long-term follow-up with large sample size. At the time of data collection, the PT examiner missed taking the participants' height, weight, and BMI values. These demographic data could have provided additional information on the association of height, weight, and BMI with stroke patients' recovery and functional progress. In the present study, balance and gait performance were measured without sophisticated equipment; future studies should use equipment such as force plates and gait analyzers to assess balance and gait performance more accurately and precisely. Future studies may explore the role of MSE in other neurological disorders where normal balance and gait are affected, e.g. cerebral palsy.
Conclusion
A 4-week program of MSE along with weight-shifting in conjunction with CTE is more effective than a program of CTE alone in improving balance and functional gait performance in the selected stroke population. However, further randomized controlled trials should confirm these findings with large sample sizes and participants with a specific disease states like acute, subacute and chronic.
Data availability
The data associated with the paper are not publicly available but are available from the corresponding author on reasonable request.
References
Geurts, A. C., De Haart, M., Van Nes, I. J. & Duysens, J. A review of standing balance recovery from stroke. Gait Posture 22(3), 267–281 (2005).
Warlow, C. P. et al. Stroke: practical Management (Wiley, 2011).
Hochstenbach, J., Donders, R., Mulder, T., Limbeek, J. & Schoonderwaldt, H. Long-term Outcome After Stroke: A Disability-Orientated Approach (1996).
Park, G.-D., Choi, J.-U. & Kim, Y.-M. The effects of multidirectional step** training on balance, gait ability, and falls efficacy following stroke. J. Phys. Ther. Sci. 28(1), 82–86 (2016).
Sackley, C. M. & Lincoln, N. B. Single blind randomized controlled trial of visual feedback after stroke: Effects on stance symmetry and function. Disabil. Rehabil. 19(12), 536–546 (1997).
Dodd, K. J. & Morris, M. E. Lateral pelvic displacement during gait: Abnormalities after stroke and changes during the first month of rehabilitation. Arch. Phys. Med. Rehabil. 84(8), 1200–1205 (2003).
Di Fabio, R. P., Kurszewski, W. M., Jorgenson, E. E. & Kunz, R. C. Footlift asymmetry during obstacle avoidance in high-risk elderly. J. Am. Geriatr. Soc. 52(12), 2088–2093 (2004).
Zamparo, P., Francescato, M., De Luca, G., Lovati, L. & di Prampera, P. The energy cost of level walking in patients with hemiplegia. Scand. J. Med. Sci. Sports 5(6), 348–352 (1995).
Harris, J. E., Eng, J. J., Marigold, D. S., Tokuno, C. D. & Louis, C. L. Relationship of balance and mobility to fall incidence in people with chronic stroke. Phys. Ther. 85(2), 150–158 (2005).
Simpson, L. A., Miller, W. C. & Eng, J. J. Effect of stroke on fall rate, location and predictors: A prospective comparison of older adults with and without stroke. PLoS ONE 6(4), e19431 (2011).
Chen, G., Patten, C., Kothari, D. H. & Zajac, F. E. Gait differences between individuals with post-stroke hemiparesis and non-disabled controls at matched speeds. Gait Posture 22(1), 51–56 (2005).
Carr, J. H. & Shepherd, R. B. Neurological Rehabilitation: Optimizing Motor Performance (Elsevier Health Sciences, 2010).
Umphred, D. A. & Lazaro, R. T. Neurological Rehabilitation (Elsevier Health Sciences, 2012).
Glaister, B. C., Bernatz, G. C., Klute, G. K. & Orendurff, M. S. Video task analysis of turning during activities of daily living. Gait Posture 25(2), 289–294 (2007).
Shigematsu, R. & Okura, T. A novel exercise for improving lower-extremity functional fitness in the elderly. Aging Clin. Exp. Res. 18(3), 242–248 (2006).
Protas, E. J. et al. Gait and step training to reduce falls in Parkinson’s disease. NeuroRehabilitation 20(3), 183–190 (2005).
Eng, J. J. & Chu, K. S. Reliability and comparison of weight-bearing ability during standing tasks for individuals with chronic stroke. Arch. Phys. Med. Rehabil. 83(8), 1138–1144 (2002).
Faul, F., Erdfelder, E., Lang, A.-G. & Buchner, A. G* Power 3: A flexible statistical power analysis program for the social, behavioral, and biomedical sciences. Behav. Res. Methods 39(2), 175–191 (2007).
Blum, L. & Korner-Bitensky, N. Usefulness of the Berg Balance Scale in stroke rehabilitation: A systematic review. Phys. Ther. 88(5), 559–566 (2008).
Weber, C. et al. Reliability and validity of the functional gait assessment: A systematic review. Phys. Occup. Ther. Geriatr. 34(1), 88–103 (2016).
Van Bloemendaal, M. et al. Validity and reproducibility of the Functional Gait Assessment in persons after stroke. Clin. Rehabil. 33(1), 94–103 (2019).
Downs, S., Marquez, J. & Chiarelli, P. The Berg Balance Scale has high intra-and inter-rater reliability but absolute reliability varies across the scale: A systematic review. J. Physiother. 59(2), 93–99 (2013).
Şahin, F., Büyükavci, R., Saǧ, S., Doǧu, B. & Kuran, B. Reliability and Validity of the Turkish Version of the Berg Balance Scale in Patients with Stroke (2013).
Price, R. & Choy, N. L. Investigating the relationship of the functional gait assessment to spatiotemporal parameters of gait and quality of life in individuals with stroke. J. Geriatr. Phys. Ther. 42(4), 256–264 (2019).
Abu-Bader, S. H. Using Statistical Methods in Social Science Research: With a Complete SPSS Guide (Oxford University Press, 2021).
Chandler, J. M., Duncan, P. W. & Studenski, S. A. Balance performance on the postural stress test: Comparison of young adults, healthy elderly, and fallers. Phys. Ther. 70(7), 410–415 (1990).
Dickstein, R., Nissan, M., Pillar, T. & Scheer, D. Foot-ground pressure pattern of standing hemiplegic patients: Major characteristics and patterns of improvement. Phys. Ther. 64(1), 19–23 (1984).
Mansfield, A. et al. Training rapid step** responses in an individual with stroke. Phys. Ther. 91(6), 958–969 (2011).
Maynard, V., Bakheit, A. M. & Shaw, S. Comparison of the impact of a single session of isokinetic or isotonic muscle stretch on gait in patients with spastic hemiparesis. Clin. Rehabil. 19(2), 146–154 (2005).
Jung, K., Kim, Y., Chung, Y. & Hwang, S. Weight-shift training improves trunk control, proprioception, and balance in patients with chronic hemiparetic stroke. Tohoku J. Exp. Med. 232(3), 195–199 (2014).
Brunnstrom, S. Walking preparation for adult patients with hemiplegia. Phys. Ther. 45(1), 17–29 (1965).
Winstein, C. J., Gardner, E. R., McNeal, D. R., Barto, P. S. & Nicholson, D. Standing balance training: Effect on balance and locomotion in hemiparetic adults. Arch. Phys. Med. Rehabil. 70(10), 755–762 (1989).
Dean, C. M. & Shepherd, R. B. Task-related training improves performance of seated reaching tasks after stroke: A randomized controlled trial. Stroke 28(4), 722–728 (1997).
Choi, J. & Kim, J. Effects of Multi-Directional Step-Up Training with Rhythmic Auditory Stimulation on Gait and Balance Ability in Stroke Patients, Graduate school of Daegu Catholic University, Republic of Korea, Master's thesis (2021).
Acknowledgements
The authors extend their appreciation to the Deanship of Scientific Research, King Saud University for funding through Vice Deanship of Scientific Research Chairs; Rehabilitation Research Chair.
Funding
This study was funded by King Saud University, Deanship of Scientific Research, Vice Deanship of Scientific Research Chairs; Rehabilitation Research Chair.
Author information
Authors and Affiliations
Contributions
R.S., T.S.S., Z.J., S.N., A.H.A., and M.K. conceptualized the study and its methodology. R.S., T.S.S., and Z.J. were involved in data collection and curation. R.S. and M.K. wrote the original draft and final version. R.S. and M.K. did data analysis and interpretation of the results. T.S.S., S.N., and A.H.A. did supervision and critically reviewed the final version. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Shrestha, R., Sandesh, T.S., Jalal, Z. et al. Effects of multi-directional step exercise with weight-shifting as an adjunct to conventional exercises on balance and gait in stroke patients. Sci Rep 12, 17053 (2022). https://doi.org/10.1038/s41598-022-21073-y
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-022-21073-y
- Springer Nature Limited