Abstract
Purpose of Review
This review aims to summarize and discuss the relationship between sodium homeostasis and hypertension, including emerging concepts of factors outside cardiovascular and renal systems influencing sodium homeostasis and hypertension.
Recent Findings
Recent studies support the dose–response association between higher sodium and lower potassium intakes and a higher cardiovascular risk in addition to the dose–response relationship between sodium restriction and blood pressure lowering. The growing body of evidence suggests the role of genetic determinants, immune system, and gut microbiota in sodium homeostasis and hypertension.
Summary
Although higher sodium and lower potassium intakes increase cardiovascular risk, salt restriction is beneficial only to a certain limit. The immune system contributes to hypertension through pro-inflammatory effects. Sodium can affect the gut microbiome and induce pro-inflammatory and immune responses that contribute to salt-sensitive hypertension.
Similar content being viewed by others
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Rucker AJ, Rudemiller NP, Crowley SD. Salt, hypertension, and immunity. Annu Rev Physiol. 2018;80:283–307. https://doi.org/10.1146/annurev-physiol-021317-121134.
Wynn TA, Chawla A, Pollard JW. Macrophage biology in development, homeostasis and disease. Nature. 2013;496(7446):445–55. https://doi.org/10.1038/nature12034.
•• He FJ, Tan M, Ma Y, MacGregor GA. Salt reduction to prevent hypertension and cardiovascular disease: JACC state-of-the-art review. J Am Coll Cardiol. 2020;75(6):632–47. https://doi.org/10.1016/j.jacc.2019.11.055. This recent review provides an update on the evidence relating salt to health, with a particular focus on blood pressure and cardiovascular disease as well as the potential mechanism.
Ellison DH, Welling P. Insights into salt handling and blood pressure. N Engl J Med. 2021;385(21):1981–93. https://doi.org/10.1056/NEJMra2030212.
•• Elijovich F, Laffer CL, Sahinoz M, Pitzer A, Ferguson JF, Kirabo A. The gut microbiome, inflammation, and salt-sensitive hypertension. Curr Hypertens Rep. 2020;22(10):79. https://doi.org/10.1007/s11906-020-01091-9. This recent review provides a discussion of the mechanisms of salt-induced cardiovascular disease as well as how the microbiome may play a role.
Denton D, Weisinger R, Mundy NI, Wickings EJ, Dixson A, Moisson P, et al. The effect of increased salt intake on blood pressure of chimpanzees. Nat Med. 1995;1(10):1009–16. https://doi.org/10.1038/nm1095-1009.
Intersalt Cooperative Research Group. Intersalt: an international study of electrolyte excretion and blood pressure. Results for 24 hour urinary sodium and potassium excretion. BMJ. 1988;297(6644):319–28. https://doi.org/10.1136/bmj.297.6644.319.
Mente A, O’Donnell MJ, Rangarajan S, McQueen MJ, Poirier P, Wielgosz A, et al. Association of urinary sodium and potassium excretion with blood pressure. N Engl J Med. 2014;371(7):601–11. https://doi.org/10.1056/NEJMoa1311989.
Weinberger MH. Salt sensitivity of blood pressure in humans. Hypertension. 1996;27(3 Pt 2):481–90. https://doi.org/10.1161/01.hyp.27.3.481.
•• Aliasgharzadeh S, Tabrizi JS, Nikniaz L, Ebrahimi-Mameghani M, Lofti Yagin N. Effect of salt reduction interventions in lowering blood pressure: a comprehensive systematic review and meta-analysis of controlled clinical trials. 2022;17(12):e0277929. https://doi.org/10.1371/journal.pone.0277929. This recent systematic review analyzes the effect of salt reduction interventions on blood pressures supporting salt substitution and education as effective strategies to lower blood pressure.
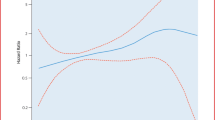
•• Filippini T, Malavolti M, Whelton PK, Naska A, Orsini N, Vinceti M. Blood pressure effects of sodium reduction: dose-response meta-analysis of experimental studies. Circulation. 2021;143(16):1542–67. https://doi.org/10.1161/CIRCULATIONAHA.120.050371. This recent meta-analysis of experimental studies describes and supports the linear dose-response analysis of sodium reduction on blood pressure.
• Huang L, Trieu K, Yoshimura S, Neal B, Woodward M, Campbell NRC, et al. Effect of dose and duration of reduction in dietary sodium on blood pressure levels: systematic review and meta-analysis of randomised trials. BMJ. 2020;368:m315. https://doi.org/10.1136/bmj.m315. This systematic review and meta-analysis examines and further supports the dose-response relationship between dietary sodium reduction and change in blood pressure.
•• Graudal NA, Hubeck-Graudal T, Jurgens G. Effects of low sodium diet versus high sodium diet on blood pressure, renin, aldosterone, catecholamines, cholesterol, and triglyceride. Cochrane Database Syst Rev. 2020;12(12):CD004022. https://doi.org/10.1002/14651858.CD004022.pub5. This recent article assesses the effects of sodium reduction on blood pressure providing quantitative mean arterial pressure reductions in normotensive compared to hypertensive study participants.
World Health Organization. Effect of reduced sodium intake on blood pressure, renal function, blood lipids and other potential adverse effects. World Health Organization. 2012. https://apps.who.int/iris/handle/10665/79325.
He FJ, Li J, Macgregor GA. Effect of longer term modest salt reduction on blood pressure: cochrane systematic review and meta-analysis of randomised trials. BMJ. 2013;346:f1325. https://doi.org/10.1136/bmj.f1325.
Appel LJ, Brands MW, Daniels SR, Karanja N, Elmer PJ, Sacks FM. Dietary approaches to prevent and treat hypertension: a scientific statement from the American Heart Association. Hypertension. 2006;47(2):296–308. https://doi.org/10.1161/01.HYP.0000202568.01167.B6.
Aburto NJ, Ziolkovska A, Hooper L, Elliott P, Cappuccio FP, Meerpohl JJ. Effect of lower sodium intake on health: systematic review and meta-analyses. BMJ. 2013;346:f1326. https://doi.org/10.1136/bmj.f1326.
Wang M, Moran AE, Liu J, Qi Y, **e W, Tzong K, et al. A meta-analysis of effect of dietary salt restriction on blood pressure in Chinese adults. Glob Heart. 2015;10(4):291-299.e6. https://doi.org/10.1016/j.gheart.2014.10.009.
Whelton PK, Carey RM, Aronow WS, Casey DE Jr, Collins KJ, Dennison Himmelfarb C, et al. 2017 ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA guideline for the prevention, detection, evaluation, and management of high blood pressure in adults: a report of the American College of Cardiology/American Heart Association Task Force on clinical practice guidelines. J Am Coll Cardiol. 2018;71(19):e127–248. https://doi.org/10.1016/j.jacc.2017.11.006.
• Williams B, Mancia G, Spiering W, Agabiti Rosei E, Azizi M, Burnier M, et al. 2018 ESC/ESH guidelines for the management of arterial hypertension. Eur Heart J. 2018;39(33):3021–104. https://doi.org/10.1093/eurheartj/ehy339. This article provides updated evidence-based guidelines for blood pressure management in Europe.
•• Rabi DM, McBrien KA, Sapir-Pichhadze R, Nakhla M, Ahmed SB, Dumanski SM, et al. Hypertension Canada’s 2020 comprehensive guidelines for the prevention, diagnosis, risk assessment, and treatment of hypertension in adults and Children. Can J Cardiol. 2020;36(5):596–624. https://doi.org/10.1016/j.cjca.2020.02.086. This recent article provides updated 2020 guidelines on blood pressure management in Canada based on evidence-based hypertension care.
Institute of Medicine. Dietary reference intakes for water, potassium, sodium, chloride, and sulfate. Washington, DC: The National Academies Press. 2005. https://doi.org/10.17226/10925.
World Health Organization. Guideline: sodium intake for adults and children. Geneva: World Health Organization. 2012. https://www.ncbi.nlm.nih.gov/books/NBK133292/.
Obarzanek E, Proschan MA, Vollmer WM, Moore TJ, Sacks FM, Appel LJ, et al. Individual blood pressure responses to changes in salt intake: results from the DASH-Sodium trial. Hypertension. 2003;42(4):459–67. https://doi.org/10.1161/01.HYP.0000091267.39066.72.
Sacks FM, Svetkey LP, Vollmer WM, Appel LJ, Bray GA, Harsha D, et al. Effects on blood pressure of reduced dietary sodium and the dietary approaches to stop hypertension (DASH) diet. N Engl J Med. 2001;344(1):3–10. https://doi.org/10.1056/NEJM200101043440101.
Whelton PK, Appel LJ, Espeland MA, Applegate WB, Ettinger WH Jr, Kostis JB, et al. Sodium reduction and weight loss in the treatment of hypertension in older persons: a randomized controlled trial of nonpharmacologic interventions in the elderly (TONE). JAMA. 1998;279(11):839–46. https://doi.org/10.1001/jama.279.11.839.
•• O’Donnell M, Mente A, Alderman MH, Brady AJB, Diaz R, Gupta R, et al. Salt and cardiovascular disease: insufficient evidence to recommend low sodium intake. Eur Heart J. 2020;41(35):3363–73. https://doi.org/10.1093/eurheartj/ehaa586. This recent review supports an increased risk of cardiovascular disease when sodium intakes exceed 5 grams per day.
Powles J, Fahimi S, Micha R, Khatibzadeh S, Shi P, Ezzati M, et al. Global, regional and national sodium intakes in 1990 and 2010: a systematic analysis of 24 h urinary sodium excretion and dietary surveys worldwide. BMJ Open. 2013;3(12):e003733. https://doi.org/10.1136/bmjopen-2013-003733.
Stolarz-Skrzypek K, Kuznetsova T, Thijs L, Tikhonoff V, Seidlerová J, Richart T, et al. Fatal and nonfatal outcomes, incidence of hypertension, and blood pressure changes in relation to urinary sodium excretion. JAMA. 2011;305(17):1777–85. https://doi.org/10.1001/jama.2011.574.
O’Donnell MJ, Yusuf S, Mente A, Gao P, Mann JF, Teo K, et al. Urinary sodium and potassium excretion and risk of cardiovascular events. JAMA. 2011;306(20):2229–38. https://doi.org/10.1001/jama.2011.1729.
O'Donnell M, Mente A, Rangarajan S, McQueen MJ, O'Leary N, Yin L, et al. Joint association of urinary sodium and potassium excretion with cardiovascular events and mortality: prospective cohort study. BMJ. 2019;364:l772. https://doi.org/10.1136/bmj.l772.
•• Groenland EH, Vendeville JP, Bots ML, de Borst GJ, Nathoe HM, Ruigrok YM, et al. The relation between urinary sodium and potassium excretion and risk of cardiovascular events and mortality in patients with cardiovascular disease. PLoS One. 2022;17(3):e0265429. https://doi.org/10.1371/journal.pone.0265429. This recent article supports the association between sodium intake and a higher risk of recurrent cardiovascular events in patients with established vascular disease.
•• Wuopio J, Ling YT, Orho-Melander M, Engström G, Ärnlöv J. The association between sodium intake and coronary and carotid atherosclerosis in the general Swedish population. Eur Heart J Open. 2023;3(2):oead024. https://doi.org/10.1093/ehjopen/oead024. This study suggests that blood pressure could mediate the interaction between salt intake and atherosclerosis even before the onset of hypertension.
Mente A, O’Donnell M, Rangarajan S, Dagenais G, Lear S, McQueen M, et al. Associations of urinary sodium excretion with cardiovascular events in individuals with and without hypertension: a pooled analysis of data from four studies. Lancet. 2016;388(10043):465–75. https://doi.org/10.1016/S0140-6736(16)30467-6.
Graudal N, Jürgens G, Baslund B, Alderman MH. Compared with usual sodium intake, low- and excessive-sodium diets are associated with increased mortality: a meta-analysis. Am J Hypertens. 2014;27(9):1129–37. https://doi.org/10.1093/ajh/hpu028.
Lerchl K, Rakova N, Dahlmann A, Rauh M, Goller U, Basner M, et al. Agreement between 24-hour salt ingestion and sodium excretion in a controlled environment. Hypertension. 2015;66(4):850–7. https://doi.org/10.1161/HYPERTENSIONAHA.115.05851.
•• Ma Y, He FJ, Sun Q, Yuan C, Kieneker LM, Curhan GC, et al. 24-hour urinary sodium and potassium excretion and cardiovascular risk. N Engl J Med. 2022;386(3):252–63. https://doi.org/10.1056/NEJMoa2109794. (This article’s findings support the dose-response association between higher sodium and lower potassium intakes and a higher cardiovascular risk.)
Kido M, Ando K, Onozato ML, Tojo A, Yoshikawa M, Ogita T, et al. Protective effect of dietary potassium against vascular injury in salt-sensitive hypertension. Hypertension. 2008;51(2):225–31. https://doi.org/10.1161/HYPERTENSIONAHA.107.098251.
•• Brand A, Visser ME, Schoonees A, Naude CE. Replacing salt with low-sodium salt substitutes (LSSS) for cardiovascular health in adults, children and pregnant women. Cochrane Database Syst Rev. 2022;8(8):CD015207. https://doi.org/10.1002/14651858.CD015207. This recent systematic review supports low sodium salt substitutes probably reduce blood pressure, non-fatal cardiovascular events, and cardiovascular mortality in adults with an increased risk of hyperkalemia.
•• Liu Y, Shi M, Dolan J, He J. Sodium sensitivity of blood pressure in Chinese populations. J Hum Hypertens. 2020;34(2):94–107. https://doi.org/10.1038/s41371-018-0152-0. This article describes the role genetic determinants likely play in salt-sensitive hypertension.
• Mary S, Boder P, Padmanabhan S, McBride MW, Graham D, Delles C, et al. Role of uromodulin in salt-sensitive hypertension. Hypertension. 2022;79(11):2419–29. https://doi.org/10.1161/HYPERTENSIONAHA.122.19888. This article provides example of genetic aberrations associated with the alteration of sodium homeostasis and salt-sensitive hypertension.
• Citterio L, Delli Carpini S, Lupoli S, Brioni E, Simonini M, Fontana S, et al. Klotho gene in human salt-sensitive hypertension. Clin J Am Soc Nephrol. 2020;15(3):375–83. https://doi.org/10.2215/CJN.08620719. This article provides an example of genetic aberrations associated with the alteration of sodium homeostasis and salt-sensitive hypertension.
Xu L, Li S, Liu Z, Jiang S, Wang J, Guo M, et al. The NLRP3 rs10754558 polymorphism is a risk factor for preeclampsia in a Chinese Han population. J Matern Fetal Neonatal Med. 2019;32(11):1792–9. https://doi.org/10.1080/14767058.2017.1418313.
• Zhu Q, Hu J, Wang L, Wang W, Wang Z, Li PL, et al. Overexpression of microRNA-429 transgene into the renal medulla attenuated salt-sensitive hypertension in Dahl S Rats. Am J Hypertens. 2021;34(10):1071–7. https://doi.org/10.1093/ajh/hpab089. This article provides an example of genetic aberrations associated with the alteration of sodium homeostasis and salt-sensitive hypertension.
•• Van Beusecum JP, Moreno H, Harrison DG. Innate immunity and clinical hypertension. J Hum Hypertens. 2022;36(6):503–9. https://doi.org/10.1038/s41371-021-00627-z. This review describes how the immune system plays a role in sodium homeostasis and the pathogenesis of hypertension.
Shah KH, Shi P, Giani JF, Janjulia T, Bernstein EA, Li Y, et al. Myeloid suppressor cells accumulate and regulate blood pressure in hypertension. Circ Res. 2015;117(10):858–69. https://doi.org/10.1161/CIRCRESAHA.115.306539.
Yoshida S, Takeuchi T, Kotani T, Yamamoto N, Hata K, Nagai K, et al. Infliximab, a TNF-α inhibitor, reduces 24-h ambulatory blood pressure in rheumatoid arthritis patients. J Hum Hypertens. 2014;28(3):165–9. https://doi.org/10.1038/jhh.2013.80.
• Makavos G, Ikonomidis I, Andreadou I, Varoudi M, Kapniari I, Loukeri E, et al. Effects of interleukin 17A inhibition on myocardial deformation and vascular function in psoriasis. Can J Cardiol. 2020;36(1):100–11. https://doi.org/10.1016/j.cjca.2019.06.021. This article supports a beneficial effect on overall cardiovascular function following autoimmune disease immunomodulatory therapies.
•• Zhang Z, Zhao L, Zhou X, Meng X, Zhou X. Role of inflammation, immunity, and oxidative stress in hypertension: new insights and potential therapeutic targets. Front Immunol. 2023;13:1098725. https://doi.org/10.3389/fimmu.2022.1098725. This recent review provides additional support for the protective role the immune system may play in hypertension.
Ferguson JF, Aden LA, Barbaro NR, Van Beusecum JP, **ao L, Simmons AJ, et al. High dietary salt-induced dendritic cell activation underlies microbial dysbiosis-associated hypertension. JCI Insight. 2019;5(13):e126241. https://doi.org/10.1172/jci.insight.126241.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare that they have no conflict of interest.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Aung, K., Ream-Winnick, S., Lane, M. et al. Sodium Homeostasis and Hypertension. Curr Cardiol Rep 25, 1123–1129 (2023). https://doi.org/10.1007/s11886-023-01931-5
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11886-023-01931-5