Abstract
Background
The benefit of ischemic postconditioning (IPostC) might be the throttled inflow following cold ischemia. The current study investigated advantage and mechanisms of IPostC in healthy and fatty rat livers.
Methods
Male SD rats received a high-fat diet to induce fatty livers. Isolated liver perfusion was performed after 24 h ischemia at 4 °C as well as in vivo experiments after 90 min warm ischemia. The so-called follow-up perfusions served to investigate the hypothesis that medium from IPostC experiments is less harmful. Lactate dehydrogenase (LDH), transaminases, different cytokines, and gene expressions, respectively, were measured.
Results
Fatty livers showed histologically mild inflammation and moderate to severe fat storage. IPostC reduced LDH and TXB2 in healthy and fatty livers and increased bile flow. LDH, TNF-α, and IL-6 levels in serum decreased after warm ischemia + IPostC. The gene expressions of Tnf, IL-6, Ccl2, and Ripk3 were downregulated in vivo after IPostC.
Conclusions
IPostC showed protective effects after ischemia in situ and in vivo in healthy and fatty livers. Restricted cyclic inflow was an important mechanism and further suggested involvement of necroptosis. IPostC represents a promising and easy intervention to improve outcomes after transplantation.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Ischemia reperfusion injury (IRI) is a major issue after liver transplantation. The interruption of oxygenation during ischemia leads to a narrowing of liver sinusoids with impaired microcirculation [1, 2] and triggers the release of reactive oxygen species (ROS) and inflammatory cytokines by activated Kupffer cells (KCs) as well as neutrophils [2, 3]. With the start of reperfusion, new oxygen is available for oxidative processes, and pH-dependent proteases and phosphatases are activated to continue and exacerbate liver damage [4]. Both ischemia and reperfusion impair organ function, which may cause organ failure and threaten patient survival after liver transplantation [5, 6].
One easy-to-apply surgical method to protect the liver against IRI consists of a procedure called ischemic postconditioning (IPostC). This strategy applies a series of brief periods of ischemia and reperfusion immediately after the ischemic period (in organ recipients), but prior to continuous reperfusion. Earlier experimental studies were performed in isolated perfused hearts and showed a protective effect on myocardium [7]. The first study testing IPostC in the liver in 2004 described a reduction in hepatocellular apoptosis through the downregulation of Bcl-2 and the inhibition of ROS by IPostC [8]. Further investigations into IPostC after ischemia showed a protective effect regarding liver regeneration [9] and gene expression profiles in liver tissue [10]. One human study showed a better tolerance to I/R injury on histological findings of grafts receiving IPostC [11].
A protective effect of IPostC was demonstrated in healthy livers [12, 13]. So far, there are no data on fatty livers. We investigated in the present study the influence of IPostC particularly on fatty livers to determine whether IPostC is able to protect healthy and fatty livers against IRI. Furthermore, we worked up a new method to investigate whether the dosed reperfusion is associated with reduced liver damage.
Materials and Methods
Animal Studies
Male Sprague–Dawley (SD) rats weighing 151–175 g from Charles River (Charles River Wiga GmbH, Sulzfeld) were used. The animals were treated according to the ethics criteria established by the National Academy of Sciences and published by the National Institutes of Health, in addition to the legal requirements of Germany. All animal experiments were approved by the local government (Regierung von Oberbayern, Munich) and were reported to the responsible authorities.
Diet-Induced Obesity
To induce fatty livers [14, 15], the animals received a control diet with 10% energy from fat (Altromin, Lage) for 10 days to prepare the gastrointestinal tract for the high–fat diet (HFD) with 70% energy from fat (Altromin, Lage) for 4 weeks ad libitum until perfusion.
Isolated Rat Liver Perfusion: Cold Ischemia and IPostC
SD rats were anesthetized with an intraperitoneal injection of pentobarbital (30–50 mg/kg of body weight) and intravenously received heparin (2000–5000 U/kg of body weight) via the femoral vein. After median laparotomy, a soft catheter was inserted into the portal vein and secured with two previously laid ligatures. The abdominal inferior vena cava was opened to flush out blood from the liver. After opening the thorax, a soft catheter was inserted into the right atrium and secured with two ligatures. A ligature around the abdominal inferior vena cava was drawn to derive the medium through the atrium and to collect it. Finally, the common bile duct was cannulated with a catheter to determine the bile flow (in ml/min × g liver) during perfusion. The portal perfusion pressure (in cmH2O) was continuously monitored.
After stabilization for 30 min, the liver was perfused with 30 ml of cold HTK solution (Dr. Franz Köhler Chemie GmbH, Bensheim) for 1 min. Storage of the liver outside of the animals for 24 h at 4 °C in HTK solution was followed with reperfusion lasting 2 h. In control group (n = 8), only reperfusion was performed. In the intervention groups (each n = 8), two different cycles of IPostC were tested immediately following ischemia: 8 × 20 s and 4 × 60 s (Fig. 1a). Perfusate and bile were collected at specific time points and stored at − 80 °C. Samples of the livers were taken at the end of each experiment for freezing at − 80 °C and fixing in formalin. During stabilization period and reperfusion, the livers were perfused with Krebs–Henseleit buffer (KH buffer, 37 °C, pH 7.4), which was previously gassed with carbogen (95% O2 and 5% CO2, Linde, Unterschleißheim) using an oxygenator.
Experimental protocols for animal studies. a Animals received a high-fat diet (HFD) over 4 weeks to induce fatty livers. For the implementation of cold ischemia, healthy and fatty livers of male SD rats were perfused for 30 min followed by storage for 24 h at 4 °C and reperfusion at 37 °C for 120 min. Intervention groups of IPostC 8 × 20 s and 4 × 60 s were performed after ischemia (control and interventions, each n = 7–8). b After the induction of fatty livers by HFD for 4 weeks, in vivo studies were performed in healthy and fatty livers in male SD rats. The left liver lobe was clamped for 90 min at 37 °C for partial warm ischemia followed by 90 min reperfusion at 37 °C. The intervention group with IPostC 4 × 60 s after ischemia was established, and a sham group underwent 90 + 90 min without clam** (sham, control, and intervention: n = 8)
Follow-Up Study
In this variation of the isolated rat liver perfusion, we induced cold liver ischemia in healthy livers of two groups of rats (24 h ischemia with or without IPostC 4 × 60 s, each n = 4) and collected their reperfusion perfusate, which we subsequently used to perfuse a second healthy rat liver (Supplementary Fig-1).
In Vivo Model: Warm Ischemia ± IPostC
Animals were anesthetized with an intraperitoneal injection of pentobarbital (1:3 diluted with 0.9% NaCl; 30–50 mg/kg of body weight) and received a subcutaneous injection of buprenorphin (0.05 mg/kg of body weight). The carotis artery was cannulated to continuously monitor arterial blood pressure with a pressure gage (Becton, Dickinson and Company, New Jersey). After median laparotomy, the left liver lobe (segment VIII) was clamped through the vena portae and arteria hepatica, and the abdominal wall was closed with 3–0 prolene (Ethicon, Somerville). For the control group (n = 8), the clamp was removed after 90 min of warm ischemia for 90 min of reperfusion. For the intervention group (n = 8), IPostC for 4 × 60 s was performed directly after ischemia with subsequent reperfusion. For the sham group, 90 + 90 min perfusion without clam** was executed (Fig. 1b). Samples of blood and liver were collected at the end of the experiments and stored at − 80 °C. Additional samples of the liver were fixed in formalin.
Histological Evaluation
Pieces of the livers were fixed in 4% buffered formalin, dehydrated in graded ethanol, and embedded in paraffin. The sections were stained with hematoxylin–eosin (HE) and Elastica van Gieson (EvG) and were evaluated regarding the following parameters (supplementary Table 1A and 1B): inflammation, fat deposition, group necrosis, and fibrosis. The graduation of parameters was carried out as follows: 0 = none, 1 = low, 2 = moderate, and 3 = severe. All steps were performed at the Department of Pathology of LMU Munich.
Lactate Dehydrogenase
The quantity of LDH in the perfusate was measured using an enzymatic test of the kinetic indicator reaction at 365 nm. LDH activity is thus proportional to a decrease in NADH. After a measurement in the linear range, the concentration of LDH (in mU/min x g liver) was calculated.
Enzyme-Linked Immunosorbent Assay (ELISA)
The efflux of thromboxane B2 into the perfusate was measured with an enzyme-linked immunosorbent assay (Cayman Chemical, Ann Arbor). Additionally, concentrations of TNF-α and IL-6 in the serum were quantified by enzyme-linked immunosorbent assays (Young In Frontier Co., Seoul).
Serum Enzyme Levels
Blood samples were collected after each in vivo experiment. After precipitation and centrifugation for 10 min at 3000 rpm, the serum was removed and stored at − 80 °C. LDH, AST, and ALT were measured in the serum at the Institute of Laboratory Medicine of LMU Munich using kinetic UV tests at 37 °C in AU 5800 and AU 680 analysis systems (Beckman Coulter GmbH, Krefeld).
RNA Extraction and RT-qPCR
Total RNA was isolated from rat livers using a miRNeasy® Mini Kit (Qiagen GmbH, Hilden) and quantified photometrically at 260 nm. cDNA synthesis was performed with a RT2 First Strand Kit (Qiagen, Hilden). RT-qPCR was executed using a Custom RT2 Profiler PCR Array (Qiagen, Hilden) and the RT2 SYBR Green ROX™ qPCR Master Mix (Qiagen, Hilden). Gene expression was evaluated relative to the housekee** genes Actb and B2m. Genes with reference sequences are listed in supplementary Table 2.
Statistical Analysis
All data are expressed as the mean ± standard error of the mean (SEM). Statistical analyses of the data were performed using GraphPad Prism 8.4.0., and a p value < 0.05 was considered to be statistically significant. Different parameter values and applied statistical tests of Figs. 3, 4, 5, and 6 and supplementary Fig. 2 are indicated in supplementary Tables 3–7.
Results
Histological Evaluation
Healthy livers showed low focal fat deposition after 24 h of cold ischemia. Fatty livers showed very low periportal and pericentral fibrosis and severe fat deposition. There was no inflammation in either liver model, but a granulocyte phagocytosis was noted near necrotic hepatocytes in both models. Furthermore, precursors of necrosis, single cell necrosis, and cytoplasm degeneration with core whitening, but only slight core loss were found in healthy and fatty livers. No effect of IPostC could be detected due to an inhomogeneous histological appearance (Fig. 2a, b).
Histological evaluation of healthy and fatty livers after cold ischemia in situ and warm ischemia in vivo. To induce fatty livers, male SD rats received a high-fat diet over the course of 4 weeks. For cold ischemia, healthy (a) and fatty (b) livers were perfused for 30 min and stored for 24 h at 4 °C followed by 120 min of reperfusion. Interventions with IPostC 8 × 20 s and 4 × 60 s were carried out after ischemia (each n = 7–8 for the control group and interventions). To perform in vivo studies, healthy (sham—c; ischemia—d) and fatty (sham—e; ischemia—f) livers underwent 90 min partial ischemia at 37 °C followed by 90 min reperfusion. An IPostC intervention group 4 × 60 s after ischemia and sham group with 90 + 90 min perfusion without clam** were established (sham, control, and intervention, each n = 8)
The experimental in vivo sham group showed low hepatocyte degeneration without core loss or necrosis. After 90 min, the histological appearance of warm ischemia in vivo with or without IPostC (Fig. 2c–f) was very heterogeneous with no clear evidence of an effect of IPostC. A low-fat deposition and low inflammation with focal periportal granulocyte infiltrates was detected. Additional confluent cytoplasm degeneration with core whitening, but no core loss, was observed.
Cell Damage, Organ Function and Portal Pressure
After ischemia and reperfusion, both groups of IPostC (8 × 20 s and 4 × 60 s) had reduced total LDH (Fig. 3a) in healthy livers without significant increase in the total bile flow (Fig. 3d). In the early phase of reperfusion (minute 0–60), there was no effect on LDH (Fig. 3b); however, bile flow was increased (Fig. 3e) by IPostC. In the late phase of reperfusion (minute 70–120), LDH (Fig. 3c) was significantly decreased and bile flow (Fig. 3f) was improved in both liver models and by both groups of IPostC. Portal perfusion pressure was reduced at the end of perfusion (Fig. 3g) by IPostC only in healthy livers.
Lactate dehydrogenase, bile flow, and portal perfusion pressure in healthy and fatty livers after cold ischemia in situ± IPostC. Fatty livers were induced by a high-fat diet for 4 weeks. After 30 min perfusion, healthy and fatty livers were stored for 24 h at 4 °C followed by 120 min reperfusion. IPostC 8 × 20 s and 4 × 60 s were performed after ischemia (control and interventions, each n = 7–8). Lactate dehydrogenase (LDH) was measured in the perfusate and is represented as total value (a) and during the early phase (minute 0–60; b) and the late phase (minute 60–120; c) of reperfusion. Bile was collected, and also, the bile flow is shown as total value (d) and at the early (e) and late (f) phase of reperfusion. For the portal perfusion pressure (g), which was monitored continuously, the value at the end of perfusion is displayed. All data are expressed as the mean ± SEM. Significances are specified as *p < 0.05, **p < 0.01, ***p < 0.001, and ****p < 0.0001
Production of Vasoconstrictor TXB2
Healthy and fatty livers have nearly the same basal values for TXB2 in the perfusate (no data shown). After cold ischemia ± IPostC, the total TXB2 (Fig. 4a) was unchanged in both liver models. The early phase of reperfusion (Fig. 4b) did not affect IPostC; however, in the late phase (Fig. 4c), TXB2 could be significantly decreased in healthy and fatty livers.
Thromboxane B2 in healthy and fatty livers after cold ischemia in situ ± IPostC. After the induction of fatty livers with a high-fat diet for 4 weeks, healthy and fatty livers were perfused for 30 min and stored for 24 h at 4 °C followed by 120 min of reperfusion. Interventions of IPostC for 8 × 20 s and 4 × 60 s were performed after ischemia (control and interventions, each n = 7–8). The perfusate was collected, and thromboxane B2 (TXB2) was measured using an enzyme-linked immunosorbent assay. The values for TXB2 are shown in total (a) and during the early phase (minute 0–60; b) and the late phase (minute 60–120; c) of reperfusion. All data are expressed as the mean ± SEM, and significances are specified as **p < 0.01 and ***p < 0.001
Serum Enzyme and Cytokine Levels
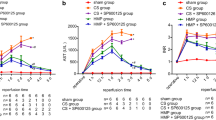
Transaminases showed strong increases in the serum of healthy and fatty livers after 90 min warm ischemia; the same result was noted with LDH (Fig. 5a–c). After IPostC 4 × 60 s, LDH was significantly reduced in healthy livers (Fig. 5a–c). TNF-α and IL-6 had very high levels in the serum of both liver models after warm ischemia compared with the sham group (Fig. 5d, e). After IPostC 4 × 60 s, levels significantly decreased, but remained higher than in the sham group (Fig. 5d, e).
Enzyme and cytokine levels in the serum of healthy and fatty livers after warm ischemia in vivo ± IPostC. In fatty livers, in vivo studies were performed. For the intervention group, IPostC 4 × 60 s was carried out after ischemia, and the sham group received 90 + 90 min without clam** (sham, control, and intervention, each n = 8). Serum was collected, and AST (a), ALT (b), and lactate dehydrogenase (LDH; c) were measured. Additionally, the cytokines tumor necrosis factor α (TNF-α; d) and interleukin 6 (IL-6; e) were determined. All data are expressed as the mean ± SEM. Significances are specified as **p < 0.01, ***p < 0.001, and ****p < 0.0001
Gene Expressions
Following warm ischemia in vivo, the genes of Ccl2, IL-10, IL-6, Tnf, and Ripk3 were upregulated in healthy and fatty (not Tnf) livers (Fig. 6a–d/g). Expressions of IL-6 and Tnf could be significantly reduced in healthy livers by IPostC 4 × 60 s (Fig. 6c, d). In fatty livers, only decreases in Ccl2 (Fig. 6a) and Ripk3 (Fig. 6g) were significant; however, all other genes as well were substantially downregulated with IPostC 4 × 60 s. Genes of Casp8 (Fig. 6e) and Ripk1 (Fig. 6f) had not changed in healthy or fatty livers after warm ischemia and IPostC.
Gene expressions in healthy and fatty livers after warm ischemia in vivo ± IPostC. The gene expressions of Ccl2 (a), interleukin 10 (IL-10; b), interleukin 6 (IL-6; c), tumor necrosis factor (Tnf; d), Caspase 8 (Casp8; e), receptor-interacting protein kinase (Ripk1; F), and receptor-interacting protein kinase 3 (Ripk3; g) were investigated using RT-qPCR. The gene expressions of intervention groups (control and 4 × 60 s) are represented as the fold change compared with the sham group (mean ± SEM; each n = 8). Significances are specified as *p < 0.05, **p < 0.01, ***p < 0.001, and ****p < 0.0001
Influence of Postconditioned Perfusate (“Follow-Up Study”)
We hypothesized that one of the major protective mechanisms of ischemic postconditioning is the restricted inflow following ischemia. To find out this is not only of major relevance for the system of ischemic postconditioning, but brings also new light into the mechanisms of ischemia reperfusion injury. To test this hypothesis, we collected the whole perfusate of rat liver perfusion number one with 24 h cold ischemia and reperfusion ± IPostC 4 × 60 s and used it to perform a second rat liver perfusion in additional healthy rat livers for 80 min (supplementary Fig. 1). The maximal and total values of LDH (supplementary Fig. 2A-B) were substantially lower after perfusions with postconditioned (4 × 60 s) perfusate; no significant effect could be shown on bile flow (supplementary Fig. 2C-D). The portal perfusion pressure (supplementary Fig. 2E) was significantly decreased in the postconditioned perfusate group compared to the non-postconditioned group.
Discussion
The so-called intervention of ischemic postconditioning (IPostC) was tested in this study and showed a protective effect in fatty livers for the first time. With an increasing number of fatty liver diseases in the near future [16], this might be of major importance. In addition, the experiments in the present study showed one important and novel aspect of ischemia reperfusion injury: The “dosed” reperfusion in the setting of IPostC has been shown to be less harmful to the livers.
For IPostC, different time courses (8 × 20 s and 4 × 60 s) have been tested in the present study. Organ function could be improved in both settings without any relevant differences regarding cell damage. So, both settings might be helpful in clinical use, but longer cycles could have the advantage of reduced damage of the vessels due to fewer clamp usages. A similar effect of IPostC has been observed in healthy livers [8,9,10, 17], but in the present study protective effects of IPostC were shown in fatty livers for the first time. The cold ischemia time of 24 h used in the present study has also been involved in earlier studies with fatty livers [18,19,20]. As stated above, to further investigate the mechanisms of IPostC we extended our perfusion model in the following way: We experimentally induced liver ischemia in two groups of rats (24 h cold ischemia with or without IPostC 4 × 60 s) and collected their reperfusion perfusate, which we subsequently used to perfuse a healthy rat liver. The perfusate derived from postconditioned group had substantially reduced damage potential compared with the perfusate derived from the non-postconditioned group. Therefore, we speculate that IPostC reduces the release of liver-damaging metabolites into the perfusate, thereby preventing cell damage by IRI. Reductions in damaging metabolites could be accomplished by previously described cumulative triggers following metabolites as well as end effectors due to IPostC.
Among NO and endothelin, an important mediator in disturbed microcirculation during ischemia is the vasoconstrictor TXA2 [1, 2]. Additionally, TXA2 promotes inflammatory processes by increasing the expression of adhesion molecules [21]. By IPostC TXB2, the inactive metabolite of TXA2 was reduced in the perfusate after ischemia and reperfusion. Thus, IPostC attenuates the production of the vasoconstrictor TXA2, thereby improving microcirculation in liver sinusoids required for the optimal supply of hepatocytes with oxygen and nutrients. This aspect is very important for fatty livers because fat depositions in the cytoplasm of hepatocytes cause an increased cell volume, which restricts the sinusoidal space prior to ischemia and reperfusion and worsens microcirculation [17].
To evaluate IPostC effect further, in vivo experiments were performed in healthy and fatty livers. Hepatic transaminases (ALT and AST) and LDH increased after 90 min of warm ischemia and were reduced by IPostC (LDH significantly in healthy livers), thereby confirming the protective effect of IPostC on healthy and fatty livers in vivo. Due to their clinical relevance, many experimental studies previously described a positive effect for IPostC on AST and ALT [9, 13, 22,23,24]. Additionally, two relevant cytokines in the genesis of IRI (TNF-α and IL-6) were measured in the serum. TNF-α was significantly decreased by IPostC in healthy as well as in fatty livers, IL-6 only in healthy livers. This is in accordance to previous studies which found reduced TNF-α in the serum [25] and liver tissue [17, 26]. IL-6 has been described in one study before on remote ischemic postconditioning (RIPostC) in an LPS-induced systemic inflammation model. A reduction in IL-6 and TNF-α in the serum due to RIPostC was found [27], which indicates a protective effect of IPostC even if performed indirectly.
To understand the underlying molecular mechanisms of IPostC in vivo after warm ischemia, we examined the expression of genes under the hypothesis to be involved in mediating the ischemia–reperfusion injury. We postulated a lower accumulation and activation of immune cells by IPostC. The first investigated chemokine Ccl2 is released from KCs. It is known to damage hepatocytes and activate hepatic stellate cells (HSCs) and interestingly was described as upregulated chemokine in fatty livers [28]. The reduced expression of Ccl2 in fatty livers by IPostC confirmed the inflammatory hypothesis and indicates an attenuated infiltration of immunologically active cells into the tissue as well as a reduction in cellular damage. Ccl2 has not been investigated regarding its role in inhibiting IRI in an IPostC scenario in the liver; however, ICAM 1, an adhesion molecule involved in recruiting neutrophils, was shown to be immunohistochemically reduced in liver tissue by IPostC [26].
In addition to ischemic postconditioning, also ischemic preconditioning and ischemic remote postconditioning have been investigated in experimental and human studies [29,30,31,32,33]. Possible mechanisms among others were related to adenosine, NO, or cytokines [34,35,36,37]. To compare the effects and mechanisms of all three variants was out of the scope of the present study, but might be focused on further studies in fatty livers. Overall ischemic postconditioning can be performed after the transplantation in the transplant center. This has the advantage of easier logistics, but the differences in effects are not yet known. Remote ischemic postconditioning could also be performed in the transplant center, but needs additional trauma. Therefore, ischemic postconditioning might be a simple and easy-to-perform procedure to improve outcome after liver transplantation, but studies in humans will be needed.
These novel findings might have impact on future surgical procedures in the setting of liver transplantation or liver resection as there is a wide range how to dose inflow into the liver following ischemia. One possibility is the additional off and on clam** of the portal vein as it is proposed here (IPostC). On the other hand, also a slowly opening of the clamp might be feasible, but has not been investigated in the present study.
In summary (see also Fig. 7), IPostC offers a very promising method to protect healthy and fatty livers from IRI. The idea of “dosed” reperfusion might have impact for future treatment. We could show in complex follow-up experiments that the medium of a postconditioned liver has lower potential to damage a second liver. From a clinical point of view, the intervention of ischemic postconditioning may help to improve graft function after ischemia reperfusion injury.
Abbreviations
- EvG:
-
Elastica van Gieson
- HE:
-
Hematoxylin/eosin
- HFD:
-
High-fat diet
- ICAM:
-
Intercellular adhesion molecule
- IL:
-
Interleukin
- IPC:
-
Ischemic preconditioning
- IPostC:
-
Ischemic postconditioning
- IRI:
-
Ischemia–reperfusion injury
- LDH:
-
Lactate dehydrogenase
- NO:
-
Nitric oxide
- RIPK:
-
Receptor-interacting protein kinase
- SOD:
-
Superoxide dismutase
- TNF:
-
Tumor necrosis factor
- TX:
-
Thromboxane
References
Peralta C, Closa D, Hotter G, Gelpi E, Prats N, Rosello-Catafau J. Liver ischemic preconditioning is mediated by the inhibitory action of nitric oxide on endothelin. Biochem Biophys Res Commun. 1996;229(1):264–270.
Peralta C, Jimenez-Castro MB, Gracia-Sancho J. Hepatic ischemia and reperfusion injury: effects on the liver sinusoidal milieu. J Hepatol. 2013;59(5):1094–1106. https://doi.org/10.1016/j.jhep.2013.06.017.
Karatzas T, Neri AA, Baibaki ME, Dontas IA. Rodent models of hepatic ischemia-reperfusion injury: time and percentage-related pathophysiological mechanisms. J Surg Res. 2014;191(2):399–412. https://doi.org/10.1016/j.jss.2014.06.024.
Guan LY, Fu PY, Li PD, et al. Mechanisms of hepatic ischemia-reperfusion injury and protective effects of nitric oxide. World J Gastrointest Surg. 2014;6(7):122–128. https://doi.org/10.4240/wjgs.v6.i7.122.
Ali JM, Davies SE, Brais RJ, et al. Analysis of ischemia/reperfusion injury in time-zero biopsies predicts liver allograft outcomes. Liver Transplant Off Publ Am Assoc Study Liver Dis the Int Liver Transplant Soc. 2015;21(4):487–499. https://doi.org/10.1002/lt.24072.
Pine JK, Aldouri A, Young AL, et al. Liver transplantation following donation after cardiac death: an analysis using matched pairs. Liver Transplant Off Publ Am Assoc Study Liver Dis the Int Liver Transplant Soc. 2009;15(9):1072–1082. https://doi.org/10.1002/lt.21853.
Tsang A, Hausenloy DJ, Mocanu MM, Yellon DM. Postconditioning: a form of “modified reperfusion” protects the myocardium by activating the phosphatidylinositol 3-kinase-Akt pathway. Circ Res. 2004;95(3):230–232. https://doi.org/10.1161/01.RES.0000138303.76488.fe.
Sun K, Liu ZS, Sun Q. Role of mitochondria in cell apoptosis during hepatic ischemia-reperfusion injury and protective effect of ischemic postconditioning. World J Gastroenterol. 2004;10(13):1934–1938.
Young SB, Pires AR, Boaventura GT, Ferreira AM, Martinho JM, Galhardo MA. Effect of ischemic preconditioning and postconditioning on liver regeneration in prepubertal rats. Transplant Proc. 2014;46(6):1867–1871. https://doi.org/10.1016/j.transproceed.2014.05.025.
Knudsen AR, Kannerup AS, Dich R, et al. Ischemic pre- and postconditioning has pronounced effects on gene expression profiles in the rat liver after ischemia/reperfusion. Am J Physiol Gastrointest Liver Physiol. 2012;303(4):G482–G489. https://doi.org/10.1152/ajpgi.00337.2011.
Ricca L, Lemoine A, Cauchy F, et al. Ischemic postconditioning of the liver graft in adult liver transplantation. Transplantation. 2015;99(8):1633–1643. https://doi.org/10.1097/TP.0000000000000685.
Tian YS, Rong TZ, Hong YL, Min L, Jian PG. Pharmacological postconditioning with diazoxide attenuates ischemia/reperfusion-induced injury in rat liver. Exp Ther Med. 2013;5(4):1169–1173. https://doi.org/10.3892/etm.2013.941.
Lin HC, Lee TK, Tsai CC, Lai IR, Lu KS. Ischemic postconditioning protects liver from ischemia-reperfusion injury by modulating mitochondrial permeability transition. Transplantation. 2012;93(3):265–271. https://doi.org/10.1097/TP.0b013e31823ef335.
Takahashi Y, Soejima Y, Fukusato T. Animal models of nonalcoholic fatty liver disease/nonalcoholic steatohepatitis. World J Gastroenterol. 2012;18(19):2300–2308. https://doi.org/10.3748/wjg.v18.i19.2300.
Schattenberg JM, Galle PR. Animal models of non-alcoholic steatohepatitis: of mice and man. Dig Dis. 2010;28(1):247–254. https://doi.org/10.1159/000282097.
Ahmed MH, Husain NE, Almobarak AO. Nonalcoholic Fatty liver disease and risk of diabetes and cardiovascular disease: what is important for primary care physicians? J Family Med Prim Care. 2015;4(1):45–52. https://doi.org/10.4103/2249-4863.152252.
Tashiro H, Kuroda S, Mikuriya Y, Ohdan H. Ischemia-reperfusion injury in patients with fatty liver and the clinical impact of steatotic liver on hepatic surgery. Surg Today. 2014;44(9):1611–1625. https://doi.org/10.1007/s00595-013-0736-9.
von Heesen M, Seibert K, Hulser M, et al. Multidrug donor preconditioning protects steatotic liver grafts against ischemia-reperfusion injury. Am J Surg. 2012;203(2):168–176. https://doi.org/10.1016/j.amjsurg.2011.01.026.
Baskin-Bey ES, Canbay A, Bronk SF, et al. Cathepsin B inactivation attenuates hepatocyte apoptosis and liver damage in steatotic livers after cold ischemia-warm reperfusion injury. Am J Physiol Gastrointest Liver Physiol. 2005;288(2):G396–G402. https://doi.org/10.1152/ajpgi.00316.2004.
Arnault I, Bao YM, Sebagh M, et al. Beneficial effect of pentoxifylline on microvesicular steatotic livers submitted to a prolonged cold ischemia. Transplantation. 2003;76(1):77–83. https://doi.org/10.1097/01.TP.0000071846.35825.B1.
Nakahata N. Thromboxane A2: physiology/pathophysiology, cellular signal transduction and pharmacology. Pharmacol Ther. 2008;118(1):18–35. https://doi.org/10.1016/j.pharmthera.2008.01.001.
Zeng Z, Huang HF, Chen MQ, Song F, Zhang YJ. Postconditioning prevents ischemia/reperfusion injury in rat liver transplantation. Hepato-Gastroenterol. 2010;57(101):875–881.
Zeng Z, Huang HF, Chen MQ, Song F, Zhang YJ. Contributions of heme oxygenase-1 in postconditioning-protected ischemia-reperfusion injury in rat liver transplantation. Transplant Proc. 2011;43(7):2517–2523. https://doi.org/10.1016/j.transproceed.2011.04.021.
Zhu YL, Yang H, Liu QN, Zhang XQ, Zhao G, Lu Y. Effects of ischemic postconditioning on liver regeneration and energy metabolism in rats. Zhonghua yi xue za zhi. 2012;92(37):2601–2606.
Song X, Zhang N, Xu H, Cao L, Zhang H. Combined preconditioning and postconditioning provides synergistic protection against liver ischemic reperfusion injury. Int J Biol Sci. 2012;8(5):707–718. https://doi.org/10.7150/ijbs.4231.
Guo JY, Yang T, Sun XG, et al. Ischemic postconditioning attenuates liver warm ischemia-reperfusion injury through Akt-eNOS-NO-HIF pathway. J Biomed Sci. 2011;18:79. https://doi.org/10.1186/1423-0127-18-79.
Kim YH, Yoon DW, Kim JH, Lee JH, Lim CH. Effect of remote ischemic post-conditioning on systemic inflammatory response and survival rate in lipopolysaccharide-induced systemic inflammation model. J Inflamm. 2014;11:16. https://doi.org/10.1186/1476-9255-11-16.
Marra F, Tacke F. Roles for chemokines in liver disease. Gastroenterology. 2014;147(3):577–594. https://doi.org/10.1053/j.gastro.2014.06.043.
Murry CE, Jennings RB, Reimer KA. Preconditioning with ischemia: a delay of lethal cell injury in ischemic myocardium. Circulation. 1986;74(5):1124–1136. https://doi.org/10.1161/01.cir.74.5.1124.
Takaoka A, Nakae I, Mitsunami K, et al. Renal ischemia/reperfusion remotely improves myocardial energy metabolism during myocardial ischemia via adenosine receptors in rabbits: effects of “remote preconditioning”. J Am Coll Cardiol. 1999;33(2):556–564. https://doi.org/10.1016/s0735-1097(98)00559-2.
Clavien PA, Selzner M, Rudiger HA, et al. A prospective randomized study in 100 consecutive patients undergoing major liver resection with versus without ischemic preconditioning. Ann Surg. 2003;238(6):843–850. https://doi.org/10.1097/01.sla.0000098620.27623.7d. discussion 51-2.
Desai KK, Dikdan GS, Shareef A, Koneru B. Ischemic preconditioning of the liver: a few perspectives from the bench to bedside translation. Liver Transplant Off Publ Am Assoc Study Liver Dis the Int Liver Transplant Soc. 2008;14(11):1569–1577. https://doi.org/10.1002/lt.21630.
Heizmann O, Loehe F, Volk A, Schauer RJ. Ischemic preconditioning improves postoperative outcome after liver resections: a randomized controlled study. Eur J Med Res. 2008;13(2):79–86.
Koti RS, Seifalian AM, Davidson BR. Protection of the liver by ischemic preconditioning: a review of mechanisms and clinical applications. Digest Surg. 2003;20(5):383–396. https://doi.org/10.1159/000072064.
Hausenloy DJ, Yellon DM. Remote ischaemic preconditioning: underlying mechanisms and clinical application. Cardiovasc Res. 2008;79(3):377–386. https://doi.org/10.1093/cvr/cvn114.
Banga NR, Homer-Vanniasinkam S, Graham A, Al-Mukhtar A, White SA, Prasad KR. Ischaemic preconditioning in transplantation and major resection of the liver. Br J Surg. 2005;92(5):528–538. https://doi.org/10.1002/bjs.5004.
Tapuria N, Kumar Y, Habib MM, Abu Amara M, Seifalian AM, Davidson BR. Remote ischemic preconditioning: a novel protective method from ischemia reperfusion injury–a review. J Surg Res. 2008;150(2):304–330. https://doi.org/10.1016/j.jss.2007.12.747.
Acknowledgments
Open Access funding provided by Projekt DEAL. The authors thank Natalie Leistner and Lisa Selzner for their excellent technical assistance. This study was supported by grants from the Deutsche Forschungsgemeinschaft (DFG STE 1022/2-3 and DFG STE 1022/4-1).
Funding
This study was supported by DFG STE 1022/2-3 and DFG STE 1022/4-1.
Author information
Authors and Affiliations
Contributions
JS and CJS took part in research design, performance of the research, data analysis and wrote the manuscript. MCM and JZ performed part of the research and analyzed data. AK took part in research design and performance of the research. DM took part in research design and analyzed data. SR and ALG took part in research design and contributed writing the manuscript. MS took part in research design, data analysis, and contributed writing the manuscript.
Corresponding author
Ethics declarations
Conflicts of interest
The authors declare no conflicts of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Schewe, J., Makeschin, MC., Khandoga, A. et al. To Protect Fatty Livers from Ischemia Reperfusion Injury: Role of Ischemic Postconditioning. Dig Dis Sci 66, 1349–1359 (2021). https://doi.org/10.1007/s10620-020-06328-w
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10620-020-06328-w