Abstract
Background
An arteriovenous fistula (AVF) is the most frequently used dialysis access for haemodialysis. However, it can cause volume loading for the heart and may induce circulatory failure when performed in patients with low cardiac function. This study aimed to characterise patients with low cardiac function when initiating dialysis and determine how cardiac function changes after the dialysis access surgery.
Methods
We conducted a retrospective observational study at two centres incorporating 356 patients with end-stage kidney disease who underwent echocardiography before the dialysis access surgery.
Results
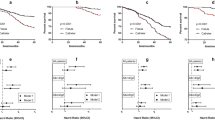
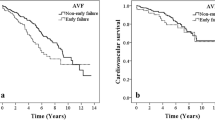
An AVF and a subcutaneously fixed superficial artery were selected in 70.4% and 23.5% of 81 patients with reduced/mildly reduced (< 50%) left ventricular ejection fraction (LVEF), respectively, and in 94.2% and 1.1% of 275 patients with preserved (≥ 50%) LVEF (p < 0.001), respectively. Follow-up echocardiography was performed in 70.4% and 38.2% of patients with reduced/mildly reduced and preserved LVEF, respectively, which showed a significant increase in LVEF (41 ± 9–44 ± 12%, p = 0.038) in patients with reduced/mildly reduced LVEF. LVEF remained unchanged in 12 patients with reduced/mildly reduced LVEF who underwent subcutaneously fixed superficial artery (30 ± 10–32 ± 15%, p = 0.527). Patients with reduced/mildly reduced LVEF had lower survival rates after surgery than those with preserved LVEF (p = 0.021 for log-rank).
Conclusion
The LVEF subcategory was associated with dialysis access selection. After the dialysis access surgery, LVEF was increased in patients with reduced/mildly reduced LVEF. These results may help select dialysis access for patients initiating dialysis.

Similar content being viewed by others
Data availability
The datasets generated and/or analyzed during the current study are available from the corresponding author on reasonable request.
References
Thomas B, Wulf S, Bikbov B, Perico N, Cortinovis M, de Vaccaro KC, et al. Maintenance dialysis throughout the World in years 1990 and 2010. J Am Soc Nephrol. 2015;26(11):2621–33.
Tang SCW, Yu X, Chen HC, Kashihara N, Park HC, Liew A, et al. Dialysis care and dialysis funding in Asia. Am J Kidney Dis. 2020;75(5):772–81.
Lai AC, Bienstock SW, Sharma R, Skorecki K, Beerkens F, Samtani R, et al. A personalized approach to chronic kidney disease and cardiovascular disease: JACC review topic of the week. J Am Coll Cardiol. 2021;77(11):1470–9.
House AA, Wanner C, Sarnak MJ, Piña IL, McIntyre CW, Komenda P, et al. Heart failure in chronic kidney disease: conclusions from a Kidney Disease: Improving Global Outcomes (KDIGO) Controversies Conference. Kidney Int. 2019;95(6):1304–17.
Roca-Tey R. Permanent arteriovenous fistula or catheter dialysis for heart failure patients. J Vasc Access. 2016;17(Suppl 1):S23–9.
Malik J. Heart disease in chronic kidney disease - review of the mechanisms and the role of dialysis access. J Vasc Access. 2018;19(1):3–11.
Postorino M, Marino C, Tripepi G, Zoccali C, Dialysis obotCRo, Transplantation. Prognostic value of the New York Heart Association classification in end-stage renal disease. Nephrol Dial Transplant. 2007;22(5):1377–82.
Kukita K, Ohira S, Amano I, Naito H, Azuma N, Ikeda K, et al. 2011 update Japanese Society for Dialysis Therapy Guidelines of vascular access construction and repair for chronic hemodialysis. Ther Apher Dial. 2015;19(Suppl 1):1–39.
Horio M, Imai E, Yasuda Y, Watanabe T, Matsuo S. Modification of the CKD epidemiology collaboration (CKD-EPI) equation for Japanese: accuracy and use for population estimates. Am J Kidney Dis. 2010;56(1):32–8.
Devereux RB, Alonso DR, Lutas EM, Gottlieb GJ, Campo E, Sachs I, et al. Echocardiographic assessment of left ventricular hypertrophy: comparison to necropsy findings. Am J Cardiol. 1986;57(6):450–8.
Teichholz LE, Kreulen T, Herman MV, Gorlin R. Problems in echocardiographic volume determinations: Echocardiographic-angiographic correlations in the presence or absence of asynergy. Am J Cardiol. 1976;37(1):7–11.
McDonagh TA, Metra M, Adamo M, Gardner RS, Baumbach A, Böhm M, et al. 2021 ESC Guidelines for the diagnosis and treatment of acute and chronic heart failure. Eur Heart J. 2021;42(36):3599–726.
Heidenreich PA, Bozkurt B, Aguilar D, Allen LA, Byun JJ, Colvin MM, et al. 2022 AHA/ACC/HFSA Guideline for the Management of Heart Failure: A Report of the American College of Cardiology/American Heart Association Joint Committee on Clinical Practice Guidelines. Circulation. 2022;145(18):e895–1032.
Nagueh SF, Smiseth OA, Appleton CP, Byrd BF, Dokainish H, Edvardsen T, et al. Recommendations for the evaluation of left ventricular diastolic function by echocardiography: an update from the American Society of Echocardiography and the European Association of Cardiovascular Imaging. J Am Soc Echocardiogr. 2016;29(4):277–314.
Bansal N, Roy J, Chen H-Y, Deo R, Dobre M, Fischer MJ, et al. Evolution of echocardiographic measures of cardiac disease from CKD to ESRD and Risk of all-cause mortality: findings from the CRIC study. Am J Kidney Dis. 2018;72(3):390–9.
Hase H, Tsunoda T, Tanaka Y, Takahashi Y, Imamura Y, Ishikawa H, et al. Risk factors for de novo acute cardiac events in patients initiating hemodialysis with no previous cardiac symptom. Kidney Int. 2006;70(6):1142–8.
Sood MM, Pauly RP, Rigatto C, Komenda P. Left ventricular dysfunction in the haemodialysis population. NDT Plus. 2008;1(4):199–205.
Aizawa N, Konishi M, Kitai T, Tsujisaka Y, Kawase Y, Shimada N, et al. Infrequent use of nighttime dialysis for emergency admission due to worsening heart failure in patients on maintenance hemodialysis. Ther Apheresis Dial. 2022;26(1):85–93.
Makar MS, Pun PH. Sudden cardiac death among hemodialysis patients. Am J Kidney Dis. 2017;69(5):684–95.
Acknowledgements
We would like to thank Editage (www.editage.com) for English language editing.
Funding
This work is funded by The Ministry of Education, Science, and Culture in Japan, 19K16986 (Masaaki Konishi).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
All authors have declared no conflict of interest.
Ethical approval
This study was approved by the Ethics Committee of Yokohama City University Hospital (approval number: B200700019) and the Ethics Committee of Yokohama City University Medical Centre (approval number: B20070041).
Informed consent
The requirement for written informed consent was waived due to the retrospective study design, and informed consent was obtained using the opt-out method.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
About this article
Cite this article
Saka, S., Konishi, M., Kamimura, D. et al. Clinical impact of left ventricular systolic dysfunction in patients undergoing dialysis access surgery. Clin Exp Nephrol 27, 374–381 (2023). https://doi.org/10.1007/s10157-023-02323-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10157-023-02323-3