Abstract
Lung ultrasound (LUS) has become as essential a tool as the stethoscope in the management of patients with respiratory disease. Other than its usual application in guiding thoracentesis, intercostal catheter placement, and medical thoracoscopy, currently, LUS is valued as an extension of clinical examination in the evaluation of chest pathologies involving pleural diseases, parenchymal infections and in the emergent evaluation of a hypoxic patient. A comprehensive understanding of the sound properties of tissue, air and fluid and their interaction, to evaluate both normal tissue, pathologies and artifacts is essential for image interpretation. Similarly, sufficient bedside experience in applying point-of-care ultrasound to extend the clinical assessment of pleural and parenchymal disease is needed, and the current generation of clinicians needs to be trained early in these methods. A growing body of evidence attests to fewer procedure-related complications in addition to cost savings associated with ultrasound use. Various management protocols have been suggested to guide diagnosis and management strategies after incorporating clinical signs along with ultrasound examination. The expanding scope of reliable literature indicates an increase in the possibility of using lung ultrasound at the patient’s bedside, especially with the advent of handheld devices.
Access this chapter
Tax calculation will be finalised at checkout
Purchases are for personal use only
Similar content being viewed by others
References
Ross AM, Genton E, Holmes JH. Ultrasonic examination of the lung. J Lab Clin Med. 1968;72(4):556–64.
Volpicelli G, Elbarbary M, Blaivas M, Lichtenstein DA, Mathis G, Kirkpatrick AW, International Liaison Committee on Lung Ultrasound (ILC-LUS) for International Consensus Conference on Lung Ultrasound (ICC-LUS), et al. International evidence-based recommendations for point-of-care lung ultrasound. Intensive Care Med. 2012;38(4):577–91.
Mojoli F, Bouhemad B, Mongodi S, Lichtenstein D. Lung ultrasound for critically ill patients. Am J Respir Crit Care Med. 2019;199(6):701–14.
Gargani L, Volpicelli G. How I do it: lung ultrasound. Cardiovasc Ultrasound. 2014 Jul;4(12):25. https://doi.org/10.1186/1476-7120-12-25.
Singh Y, Tissot C, Fraga MV, Yousef N, Cortes RG, Lopez J, et al. International evidence-based guidelines on point of care ultrasound (POCUS) for critically ill neonates and children issued by the POCUS Working Group of the European Society of Paediatric and Neonatal Intensive Care (ESPNIC). Crit Care. 2020;24(1):65.
Aldrich JE. Basic physics of ultrasound imaging. Crit Care Med. 2007;35(Suppl):S131–7.
Buessler A, Chouihed T, Duarte K, Bassand A, Huot-Marchand M, Gottwalles Y, et al. Accuracy of several lung ultrasound methods for the diagnosis of acute heart failure in the ED: a multicenter prospective study. Chest. 2020;157(1):99–110.
Lichtenstein D, Goldstein I, Mourgeon E, Cluzel P, Grenier P, Rouby JJ. Comparative diagnostic performances of auscultation, chest radiography, and lung ultrasonography in acute respiratory distress syndrome. Anesthesiology. 2004;100(1):9–15.
Pivetta E, Goffi A, Lupia E, Tizzani M, Porrino G, Ferreri E, SIMEU Group for Lung Ultrasound in the Emergency Department in Piedmont, et al. Lung ultrasound-implemented diagnosis of acute decompensated heart failure in the ED: a SIMEU multicenter study. Chest. 2015;148(1):202–10.
Volpicelli G, Mussa A, Garofalo G, Cardinale L, Casoli G, Perotto F, et al. Bedside lung ultrasound in the assessment of alveolar-interstitial syndrome. Am J Emerg Med. 2006;24(6):689–96.
Jambrik Z, Monti S, Coppola V, Agricola E, Mottola G, Miniati M, Picano E. Usefulness of ultrasound lung comets as a nonradiologic sign of extravascular lung water. Am J Cardiol. 2004;93(10):1265–70.
Lichtenstein DA, Menu Y. A bedside ultrasound sign ruling out pneumothorax in the critically ill. Lung sliding. Chest. 1995;108(5):1345–8.
Lichtenstein D, Mezière G, Biderman P, Gepner A. The lung point: an ultrasound sign specific to pneumothorax. Intensive Care Med. 2000;4:1434–40.
Lichtenstein D, Mezière G, Lascols N, Biderman P, Courret JP, Gepner A, Tenoudji-Cohen M. Ultrasound diagnosis of occult pneumothorax. Crit Care Med. 2005;4:1231–8.
Lichtenstein D, Lascols N, Prin S, Mezière G. The lung pulse: an early ultrasound sign of complete atelectasis. Intensive Care Med. 2003;4:2187–92.
Targhetta R, Bourgeois JM, Chavagneux R, Marty-Double C, Balmes P. Ultrasonographic approach to diagnosing hydropneumothorax. Chest. 1992;101:931–4.
Koh DM, Burke S, Davies N, Padley SP. Transthoracic US of the chest: clinical uses and applications. Radiographics. 2002;22(1):e1.
Volpicelli G. Sonographic diagnosis of pneumothorax. Intensive Care Med. 2011 Feb;37(2):224–32.
Alrajhi K, Woo MY, Vaillancourt C. Test characteristics of ultrasonography for the detection of pneumothorax: a systematic review and meta-analysis. Chest. 2012;141(3):703.
Copetti R, Soldati G, Copetti P. Chest sonography: a useful tool to differentiate acute cardiogenic pulmonary edema from acute respiratory distress syndrome. Cardiovasc Ultrasound. 2008;6:16.
Bouhemad B, Zhang M, Lu Q, Rouby JJ. Clinical review: bedside lung ultrasound in critical care practice. Crit Care. 2007;11:205.
Pneumatikos I, Bouros D. Pleural effusions in critically ill patients. Respiration. 2008;76:241–8.
Roch A, Bojan M, Michelet P, Romain F, Bregeon F, Papazian L, et al. Usefulness of ultrasonography in predicting pleural effusions>500 mL in patients receiving mechanical ventilation. Chest. 2005;127:224–32.
Via G, Storti E, Gulati G, Neri L, Mojoli F, Braschi A. Lung ultrasound in the ICU: from diagnostic instrument to respiratory monitoring tool. Minerva Anestesiol. 2012;78:1282–96.
Lichtenstein DA, Mezière GA. Relevance of lung ultrasound in the diagnosis of acute respiratory failure: the BLUE protocol. Chest. 2008;134:117–25.
Reissig A, Kroegel C. Transthoracic ultrasound of lung and pleura in the diagnosis of pulmonary embolism: a novel non-invasive bedside approach. Respiration. 2003;70:441–52.
Wang XT, Liu DW, Zhang HM, He HW, Liu Y, Chai WZ, et al. The value of bedside lung ultrasound in emergency-plus protocol for the assessment of lung consolidation and atelectasis in critical patients. Zhonghua Nei Ke Za Zhi. 2012;51:948–51.
Mongodi S, Via G, Girard M, Rouquette I, Misset B, Braschi A, Mojoli F, Bouhemad B. Lung ultrasound for early diagnosis of ventilator-associated pneumonia. Chest. 2016;149:969–80.
Ho MC, Ker CR, Hsu JH, Wu JR, Dai ZK, Chen IC. Usefulness of lung ultrasound in the diagnosis of community-acquired pneumonia in children. Pediatr Neonatol. 2015;56:40–5.
Alzahrani SA, Al-Salamah MA, Al-Madani W, Elbarbary MA. Systematic review and meta-analysis for the use of ultrasound versus radiology in diagnosing of pneumonia. Crit Ultrasound J. 2017;9:6.
Reissig A, Copetti R, Mathis G, Mempel C, Schuler A, Zechner P, et al. Lung ultrasound in the diagnosis and follow-up of community-acquired pneumonia: a prospective, multicenter, diagnostic accuracy study. Chest. 2012;142:965–72.
Testa A, Soldati G, Copetti R, Giannuzzi R, Portale G, Gentiloni-Silveri N. Early recognition of the 2009 pandemic influenza a (H1 N1) pneumonia by chest ultrasound. Crit Care. 2012;16:R30.
Lissaman C, Kanjanauptom P, Ong C, Tessaro M, Long E, O'Brien A. Prospective observational study of point-of-care ultrasound for diagnosing pneumonia. Arch Dis Child. 2019;104:12–8.
Tsai NW, Ngai CW, Mok KL, Tsung JW. Lung ultrasound imaging in avian influenza a (H7 N9) respiratory failure. Crit Ultrasound J. 2014;6:6.
Tsung JW, Kessler DO, Shah VP. Prospective application of clinician-performed lung ultrasonography during the 2009 H1 N1 influenza a pandemic: distinguishing viral from bacterial pneumonia. Crit Ultrasound J. 2012;4:16.
Shen MS, Yin T, Ji XL. Pathological diagnosis and differential diagnosis of severe acute respiratory syndrome. J Clin Exp Pathol. 2003;19:387–9.
Xu Z, Shi L, Wang Y, Zhang J, Huang L, Zhang C, et al. Pathological findings of COVID-19 associated with acute respiratory distress syndrome. Lancet Respir Med. 2020;8:420–2.
Zhu ZX, Lian XH, Zeng YM, Wu WJ, Xu ZR, Chen YJ, et al. Point-of-care ultrasound- a new option for early quantitative assessment of pulmonary edema. Ultrasound Med Biol. 2020;46:1–10.
Zeng LQ, Lyu GR, Lian XH, Zhu ZX, Chen YJ, Xu ZR, Guo YN. Study on the correlation between B line in ultrasound and severity of pulmonary edema. Chinese J Ultrasound Med. 2019;35:272–4.
Yang PC. Ultrasound-guided transthoracic biopsy of the chest. Radiol Clin N Am. 2000;38(2):323–43.
Sheth S, Hamper UM, Stanley DB, Wheeler JH, Smith PA. US guidance for thoracic biopsy: a valuable alternative to CT. Radiology. 1999;210:721–6.
Hendrikse K, Gramata J, ten Hove W, Rommes J, Schultz M, Spronk P. Low value of routine chest radiographs in a mixed medical-surgical ICU. Chest. 2007;4:823–8.
McGonigal MD, Schwab CW, Kauder DR, Miller WT, Grumbach K. Supplemented emergent chest CT in the management of blunt torso trauma. J Trauma. 1990;4:1431–5. https://doi.org/10.1097/00005373-199012000-00001.
Lauer MS. Elements of danger - the case of medical imaging. N Engl J Med. 2009;4:841–3. https://doi.org/10.1056/NEJMp0904735.
Lichtenstein D, Hulot JS, Rabiller A, Tostivint I, Mezière G. Feasibility and safety of ultrasound-aided thoracentesis in mechanically ventilated patients. Intensive Care Med. 1999;4:955–8.
Lichtenstein D, Mezière G, Seitz J. The dynamic air bronchogram. An ultrasound sign of alveolar consolidation ruling out atelectasis. Chest. 2009;4:1421–5.
Lerolle N, Guérot E, Dimassi S, Zegdi R, Faisy C, Fagon JY, Diehl JL. Ultrasonographic diagnosis criterion for severe diaphragmatic dysfunction after cardiac surgery. Chest. 2009;4:401–7.
Vignon P, Chastagner C, Berkane V, Chardac E, Francois B, Normand S, et al. Quantitative assessment of pleural effusion in critically ill patients by means of ultrasonography. Crit Care Med. 2005;4:1757–63.
Bouhemad B, Brisson H, Le-Guen M, Arbelot C, Lu Q, Rouby JJ. Ultrasound assessment of positive end-expiratory pressure-induced lung recruitment. Am J Respir Crit Care Med. 2011;4:341–7.
Oveland NP, Lossius HM, Wemmelund K, Stokkeland PJ, Knudsen L, Sloth E. Using thoracic ultrasonography to accurately assess pneumothorax progression during positive pressure ventilation. A comparison with CT scanning. Chest. 2013;4(2):415–22.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
4.1 Electronic Supplementary Material
Right upper anterior point using phased array probe (MP4 21617 kb)
Right lower anterior point uisng transverse probe (MP4 9485 kb)
Right posterior-lateral alveolar plueral point (MP4 14008 kb)
Right costophrenic view (MP4 20839 kb)
Self-Assessment Questions: Select the Best Answer
Self-Assessment Questions: Select the Best Answer
-
1.
The maximum reflection of ultrasound signals during thoracic ultrasound happens at
-
A.
Skin and subcutaneous
-
B.
Subcutaneous and muscle layer
-
C.
Soft tissue and pleura
-
D.
Pleura and lung parenchyma
-
A.
-
2.
Following are the features of using a linear ultrasound probe in LUS except
-
A.
Deeper penetration
-
B.
Has narrow sector width
-
C.
Large footprint
-
D.
Not recommended for rapidly moving structures
-
A.
-
3.
For better image quality using color Doppler all are recommended except
-
A.
Using wall filter for rapidly moving structures
-
B.
High scale velocity
-
C.
Adjust color gain to get “snowstorm” appearance
-
D.
Doppler angle must be less than 60°
-
A.
-
4.
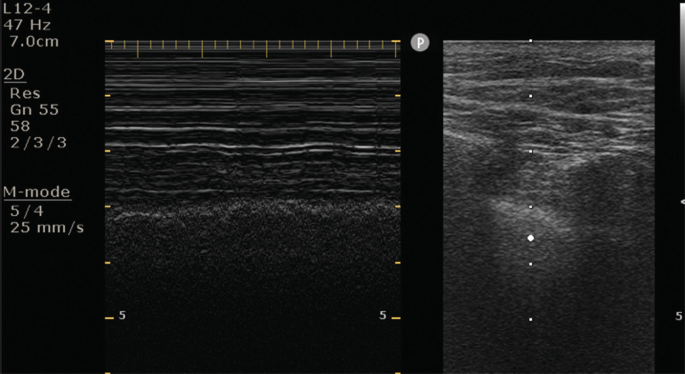
The structure highlighted in the following image represents

-
A.
Pleural line
-
B.
B-line
-
C.
A-line
-
D.
Z-line
-
A.
-
5.
The most appropriate technique to avoid acoustic shadowing from ribs is
-
A.
Using curvilinear probe
-
B.
Scanning in sagittal plane
-
C.
Phased array probe parallel to rib
-
D.
Using linear probe
-
A.
-
6.
A-lines are one of the common artifacts observed in LUS. The true statement about A-line is
-
A.
Reflection from bony surface
-
B.
Refraction from pleural surface
-
C.
Reverberation from pleural line
-
D.
Refraction from fascial plane
-
A.
-
7.
Following are advantages of using curvilinear probe in LUS except
-
A.
Smaller footprint
-
B.
Higher penetration
-
C.
Ideal for assessment of diaphragm
-
D.
Lower frequency
-
A.
-
8.
Blue protocol is one of the commonly employed methods for comprehensive assessment of lung using ultrasound. A positive blue point represents
-
A.
Presence of two B-lines
-
B.
Presence of one B-line
-
C.
Presence of three B-lines
-
D.
Presence of four B-lines
-
A.
-
9.
Absence of lung sliding is one of the essential features of LUS to diagnose pneumothorax. Presence of the following respiratory condition will cause false lung sliding due to vigorous intercostal muscle contraction
-
A.
Emphysema
-
B.
Chronic bronchitis
-
C.
Acute respiratory distress syndrome
-
D.
Bronchial asthma
-
A.
-
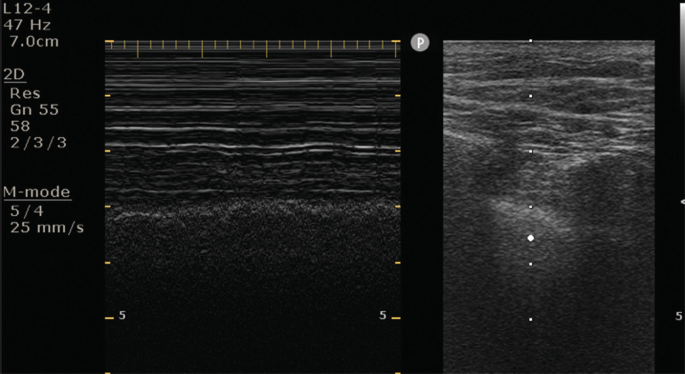
10.
The highlighted structure/artifact in the following ultrasound image represents

-
A.
A-line
-
B.
Pleural line
-
C.
T-line
-
D.
B-line
-
A.
-
11.
You have high peak ventilation pressures after intubating a patient with advanced COPD. You find bilateral anterior B-lines but cannot find lung sliding over the right anterior thorax. What is the most likely cause of high peak pressures?
-
A.
Pleural effusion
-
B.
Pulmonary edema
-
C.
Pneumothorax
-
D.
Pericardial tamponade
-
A.
-
12.
You are taking care of a trauma patient who is admitted after a collision between the car that he was an unrestrained driver in ran into a tree. The patient has multiple rib fractures and has a high oxygen requirement of 70% oxygen on a noninvasive BiPAP machine to maintain oxygenation. He is also complaining of dyspnea and chest fullness. You perform a lung ultrasound, and the attached picture is displayed. What is the most likely reason for his respiratory condition?

-
A.
Pleural effusion
-
B.
Pulmonary contusions
-
C.
Pericardial effusion
-
D.
Pneumothorax
-
A.
-
13.
A 50-year-old patient presents with a week-long history of dyspnea. Fever, and cough. His blood pressure is 90/50 and he is requiring four liters of oxygen to maintain his saturation. The attached picture represents the ultrasound exam with the probe held in place at the base of the lung. What is the most likely diagnosis?

-
A.
COPD
-
B.
Pneumonia
-
C.
Pericardial effusion
-
D.
Pneumothorax
-
A.
-
14.
A 75-year-old woman, with chronic myeloid leukemia presents with dyspnea and fever. She presented to her doctor a week ago with fever and cough, for which she was treated with azithromycin. She was feeling better for a while but has been declining for the past couple of days. Please interpret her lung ultrasound findings

-
A.
Pleural effusion
-
B.
Pneumonia
-
C.
Pericardial effusion
-
D.
Pneumothorax
-
A.
-
15.
You are called on the floor to evaluate a 90-year-old man with diastolic dysfunction. His diuretics have been held for the past week due to renal dysfunction (currently his creatinine has plateaued at 4.2 mg/dL). He has been placed on BiPAP but continues having substantial work of breathing. The following images are obtained from his right thorax. What is the most likely cause of his pulmonary dysfunction, based on the ultrasound findings

-
A.
Pleural effusion
-
B.
Pneumonia
-
C.
Pericardial effusion
-
D.
Pulmonary edema
-
A.
-
16.
A 29-year-old male, weighing 134 kg is brought to the emergency department after a motor vehicle accident. He has lost a lot of blood and is hypotensive and anemic with a Hb of 6.2. An emergent central line is placed in his right internal jugular and is challenging to place, given his body habitus. The patient becomes hemodynamically unstable after line placement and there is some concern that he might have developed an iatrogenic pneumothorax due to accidental puncture during line placement. A lung ultrasound over the right upper chest shows the following picture
What is the most accurate statement?
-
A.
Patient does not have pneumothorax
-
B.
Patient does not have pneumothorax, at that point. A more comprehensive lung exam is required
-
C.
Patient needs an emergent chest tube
-
D.
Patient has a hemothorax that needs to be drained
-
A.
-
17.
Which one of the following statements about B-lines is TRUE?
-
A.
B-lines are reverberation artifacts arising from volumetric variations between aerated and fluid-filled parts of the lung tissue
-
B.
B-lines are evenly spaced horizontal lines at integer multiples of the distance from the skin to the pleural line
-
C.
B-lines indicate well-aerated lung
-
D.
B-lines are diagnostic with for pneumothorax
-
A.
-
18.
Absence of pleural lung sliding can occur in all of the following situations except
-
A.
Pneumothorax
-
B.
Apnea
-
C.
Bronchial intubation
-
D.
Bronchial obstruction
-
E.
Pleural adhesion
-
F.
All of the above
-
A.
-
19.
A 64-year-old female, with a history of HTN, HLD, and COPD has an onset of shortness of breath and sudden chest pain for the past few hours, after a coughing spell. The physician evaluates the heart and lungs with ultrasound. When looking at the lungs, the physician notices multiple horizontal lines between two hypoechoic columns as well as a lung point however he does not see any lung sliding. What is the most likely diagnosis?
-
A.
Pleural effusion
-
B.
Pneumonia
-
C.
Pericardial effusion
-
D.
Pneumothorax
-
A.
-
20.
A 82-year-old male with a past history of CAD, systolic heart failure with EF of 30%, COPD, and a 3-year history of progressively worsening dyspnea on exertion finally presents to his PCP for workup. The doctor notices distended jugular veins and upon auscultation hears an S3 and a holosystolic murmur over the apex. The physician performs a chest ultrasound exam and sees the following. Based on this exam, which of the following is true?

-
A.
Patient has a pleural effusion
-
B.
Patient has fluid in the hepatorenal recess
-
C.
Patient has free fluid surrounding the bladder
-
D.
Patient is completely healthy
-
A.
Rights and permissions
Copyright information
© 2022 The Author(s), under exclusive license to Springer Nature Singapore Pte Ltd.
About this chapter
Cite this chapter
Sharma, A., Subramani, S. (2022). Point-of-Care Ultrasound of the Lungs. In: Chakraborty, A., Ashokka, B. (eds) A Practical Guide to Point of Care Ultrasound (POCUS). Springer, Singapore. https://doi.org/10.1007/978-981-16-7687-1_4
Download citation
DOI: https://doi.org/10.1007/978-981-16-7687-1_4
Published:
Publisher Name: Springer, Singapore
Print ISBN: 978-981-16-7686-4
Online ISBN: 978-981-16-7687-1
eBook Packages: MedicineMedicine (R0)