Abstract
Evidence shows that patients affected by Parkinson’s disease (PD) display the tendency toward making risky choices. This is due, at least in part, to the pathophysiological characteristics of the disease that affects neural areas underlying decision making (DM), in which a pivotal role is played by nonmotor corticostriatal circuits and dopamine. Executive functions (EFs), which can be impaired by PD as well, may sustain optimal choices in DM processes. However, few studies have investigated whether EFs can support PD patients to make good decisions. Adopting the sco** review approach, the present article is designed to deepen the cognitive mechanisms of DM under conditions of ambiguity and risk (that are conditions common to everyday life decisions) in PD patients without impulse control disorders. We focused our attention on the Iowa Gambling Task and the Game of Dice Task, because they are the most commonly used and reliable tasks to assess DM under ambiguity and under risk, respectively, and analyzed the performances in such tasks and their relationships with EFs tests in PD patients. The analysis supported the relationships between EFs and DM performance, especially when a higher cognitive load is required to make optimal decisions, as it happens under conditions of risk. Possible knowledge gaps and further research directions are suggested to better understand DM mechanisms in PD sustaining patients’ cognitive functioning and preventing negative consequences in everyday life derived from suboptimal decisions.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Parkinson’s disease (PD) is the second most common neurodegenerative disease, with an incidence of approximately 1-2% in older adults (Chen et al., 2022). PD can be described as a slowly degenerative neurological disease, due to a loss of dopaminergic neurons in the substantia nigra pars compacta of the mesencephalon and an accumulation of the α-synuclein protein, which constitutes insoluble aggregates forming the basis of Lewy bodies. Alterations in the nigrostriatal circuit occur as well (Balestrino & Schapira, 2020; Zgaljardic et al., 2006). Progressing the disease, other brain areas are involved, such as cortical regions, in particular the prefrontal cortex (PFC) (Braak et al., 2003; Braak & Del Tredici, 2008; Ferrer, 2009), and the corticostriatal pathways. Focusing on the latter ones, they are composed of five different circuits receiving partially overlap** corticostriatal inputs and projecting to distinct striatal regions. They are the motor and the oculomotor circuits (that are usually categorized as motor circuits), the dorsolateral prefrontal, the (lateral) orbitofrontal, and the anterior cingulate circuits (usually classified as complex or non-motor circuits) (Alexander et al., 1986; Zgaljardic et al., 2006). Focusing on the nonmotor circuits, each of them underlies a specific prefrontal area and it is assumed to be linked with distinct cognitive and behavioral functions: Respectively, the dorsolateral prefrontal cortex (dlPFC) is thought to mediate cognitive functions, such as executive functions (EFs); The orbitofrontal cortex (OFC) has been linked to functions such as impulse control, decision making based on reinforcement and reward, mood regulation; The anterior cingulate cortex (ACC) is thought to be involved in control and attentional processes (Zgaljardic et al., 2003).
PD is mainly characterized by the presence of motor symptoms (e.g., bradykinesia, resting tremor, rigidity of limbs and trunk, and postural instability) (Balestrino & Schapira, 2020; Moustafa et al., 2016). Motor symptoms are associated with a broad spectrum of nonmotor disturbances as well, including behavioral, affective, and cognitive disorders (Pfeiffer, 2016). Among the cognitive abilities, attention, EFs (e.g., divided attention, set-shifting and flexibility, inhibition, working memory, planning, executive control), speed processing, visuospatial skills, and learning (Dujardin & Laurent, 2003; Pillon et al., 1993; Poletti & Bonuccelli, 2010) are mainly affected. PD patients also can display impairments in Theory of Mind (ToM), increasing in severity with the progression of the disease (Bora et al., 2015; Coundouris et al., 2020). ToM can be described as the capacity to attribute mental states to oneself and others, including emotions, intentions, desires, beliefs, and knowledge (Premack & Woodruff, 1978).
During the past 20 years, studies also have paid attention to possible impairments in value-based decision making (DM) in PD, which is characterized by making a choice through the attribution of subjective values to the different choice options (Rangel et al., 2008). On the basis of information available to make the decision, two conditions can be conceptualized: DM under ambiguity and DM under risk. In the previous condition, the probabilities of the occurrence of positive and negative consequences—associated with at least one of the possible choices—are unknown. In the latter condition, the probabilities of the occurrence of positive and negative consequences are known (Brand et al., 2007; Lauriola et al., 2007; Schultz et al., 2008) (for more details about DM, see Table 1).
Reviews of literature showed that patients affected by PD generally present a tendency toward making more risky choices under both conditions of ambiguity and risk compared with healthy controls (HCs), although results are controversial when exploring possible significant differences between PD patients and HCs in DM tasks (Colautti et al., 2021; Evens et al., 2016; Kjær et al., 2018). Conversely, it appears crucial to acquire more knowledge regarding patients’ trend toward making risky choices and the underlying mechanisms, because in everyday life it may lead to behavioral disturbances, such as impulse control behaviors (ICBs) or more severe forms of impulse control disorders (ICDs) (for a definition, see Weintraub et al., 2015), that can give rise to negative consequences for patients’ care process and quality of life (Baig et al., 2019; Drew et al., 2020; Stenberg, 2016).
To better understand such an issue, with the further goal to promote optimal levels of cognitive functioning and wellbeing in PD patients, the present sco** review was designed to delve into the cognitive mechanisms of DM in PD patients, analyzing the relationship between DM under conditions of ambiguity and risk and EFs, which are pivotal in the decisional process (Brand et al., 2006; Del Missier et al., 2010; Schiebener and Brand, 2015; Colautti et al., 2022), the underlying neural substrates, and their possible involvement in PD. First, a brief overview of the DM process in PD is reported, followed by an analysis of the underlying neural mechanisms. Afterward, results derived from a sco** review analysis are provided and discussed to deepen the relationship between DM and EFs in PD patients, highlighting possible outstanding questions about the decisional processes in PD and suggesting directions for new research.
What is known about decision making in Parkinson’s disease
There is a broad consensus about the presence of a preference toward risky choices in PD patients—probably due to an impairment in anticipating the unrewarding consequences or to an insensitiveness to punishment—at least in part due to the involvement of brain structures supporting decisional processes and affected by the disease (Colautti et al., 2021; Kobayakawa et al., 2010). Conversely, results are mixed when behavioral responses are statistically analyzed to investigate possible overt differences between patients and healthy controls in DM tasks, probably due to the variability of the processes involved. In fact, it is assumed that PD affects selectively some steps of DM rather than leading to a general and unspecific impairment (Ryterska et al., 2014). Whilst some cognitive processes of DM (such as recognizing and representing the decisional situation) are mostly spared, others are crucially impaired. One of these is the evaluation of choice options, in which it is required to make a “cost-benefit analysis” according to personal goals, to set values in terms of positive or negative outcomes to the possible options, and to anticipate consequences. Other processes that are affected are the evaluation of the outcome and learning from feedback, essential to make further optimal choices. Hence, in those decisional tasks where these processes cover a pivotal role, as it happens at different levels in situations under ambiguity and risk, the behavioral tendency of patients to make risky and suboptimal choices can be clearer (Foerde & Shohamy, 2011; Ryterska et al., 2014).
Possible explications for such a behavior can be inferred from the type of neural structures affected in PD, the progressive loss of dopamine in the disease evolution, and the dopaminergic therapy (Kjær et al., 2018; Kobayashi et al., 2019). The progressive decrease in dopamine in PD reduces the functionality of corticostriatal circuits. Specifically, two of them are assumed to be more related to cognitive impairments: the dorsolateral circuit—counting dlPFC, striatum (dorsolateral caudate nucleus), globus pallidus, and thalamus—and the orbitofrontal circuit—counting OFC, striatum (ventromedial caudate nucleus), globus pallidus, and the thalamus (Poletti & Bonuccelli, 2013; Zgaljardic et al., 2003). In both circuits, two loops connect the striatum to the PFC: the direct excitatory loop (Go pathway of the BG) and the indirect inhibitory loop (No-go pathway), which modulate motivation and reward processes. Rewards and punishments induce respectively phasic dopamine bursts or dips (Kravitz et al., 2012; Volkow & Morales, 2015). Bursts arouse the Go pathway (easing a cortical response—reward processing), whereas dips act on the No-go pathway (inhibiting actions from being executed to contrast negative consequences—punishment learning) (Argyelan et al., 2018). In this way, the depletion of dopamine, as it happens in PD, may promote No-go pathway activity, increasing punishment learning. Whilst increased levels of dopamine, as it may happen with dopaminergic drugs intakes, can elicit the opposite result, promoting the Go pathway that can both increase sensitivity to reward (Cools et al., 2022; Hikida et al., 2010) and prevent dopamine dips (Poletti & Bonuccelli, 2013). Studies exploring dopamine replacement therapy withdrawals showed a decreased sensitivity toward punishment in pharmacological “on” conditions rather than “off” conditions and a decreased neural response to negative feedback as well (Argyelan et al., 2018; McCoy et al., 2019). Therefore, this condition may sustain greater processing of reward than punishment (Benussi et al., 2017), which can explain both the patients’ trend to be more focused on positive consequences (regardless of possible higher negative ones) and the possible behavioral impulsivity displayed in making hasty choices in everyday life situations (Kjær et al., 2018). In fact, the imbalance in learning from punishment and reward together with the higher sensitivity to the latter one can lead patients to develop risky behaviors, with detrimental personal, social, financial, and medical consequences for themselves and their families (Drew et al., 2020).
Moreover, the tendency toward making risky choices and the insensitiveness to unrewarding consequences detected in PD patients have been explained by other mechanisms focused on the possible effect of dopamine on the ventral striatum. Specifically, during the onset stages of PD, the decrease in dopamine mainly involves the dorsolateral circuit affecting the functioning of EFs, whereas the orbitofrontal circuit (mainly underlying emotion-based representations, processing of reward, implicit and probabilistic reversal learning) is usually affected in later stages (Cools et al., 2022; Poletti & Bonuccelli, 2013). According to the dopamine overdose hypothesis (for more details, see Gotham et al., 1986; Cools et al., 2022), the administration of dopaminergic drugs may produce differential cognitive effects on such frontostriatal circuits, improving cognitive functions, such as EFs, mainly relying on the dorsolateral circuit, while affecting those related to the more spared ventral striatum and orbitofrontal circuit, which are involved in DM under ambiguity and risk, by “overdosing” them. This hypothesis is in line with studies investigating the effects of dopaminergic drugs withdrawals, where the pharmaceutical “off” condition shows increasing difficulties in tasks related to components of the dorsolateral circuit, such as tasks requiring set-shifting, but improvements in tasks related to the orbitofrontal circuit, such as tasks requiring reversal learning (Cools et al., 2001; Jahanshahi et al., 2010). Thus, the involvement of neural structures pivotal for learning contingencies under ambiguous situations, cost-benefit analysis, reward anticipation, reward and risk processing, such as OFC and ventral striatum (Colautti et al., 2021; Pascucci et al., 2017; Ryterska et al., 2014; Seymour et al., 2007; Zha et al., 2022), can explain, at least in part, the selective impairments in DM steps that are involved in risky and ambiguous conditions.
The important role of executive functions in decision making
DM implies many cognitive functions (e.g., general cognitive abilities, long-term memory, numerical and probability processing), among which EFs appear to be crucial (Schiebener and Brand, 2015; Colautti et al., 2022). Specifically, decision makers are required to inhibit the drive to be attracted by impulsive choices planning a strategy that allows them to achieve long-term wins rather than making choices characterized by possible higher immediate wins but also long-term higher losses (Colombo et al., 2020). Furthermore, decision makers have to compare possible choices’ outcomes holding in mind relevant data, remember the outcomes of previous choices, update representations of subjective values of the possible options, and shift their future decisions according to the available data and the updated representations (Colautti et al., 2021). These cognitive operations mainly involve flexibility, inhibition, planning, and working memory, which are included in EFs and can be impaired in PD patients. As shown by recent studies focusing on healthy adults (Colautti et al., 2022; Damme et al., 2019), the degree of involvement of EFs in DM depends on some elements, such as the nature of the decisional problem, the kind of information available, the affective components triggered by the situation, and the level of the decision maker’s cognitive functioning.
Data from neuroimaging studies highlighted overlaps between brain areas implied in DM tasks and in EFs tests, where a crucial role is played by the frontostriatal loops (in which PFC and basal ganglia (BG) are pivotal) and dopaminergic pathways. They are considered fundamental in motivation, reward processing, and learning (Brand et al., 2006; Costello et al., 2021; Euteneuer et al., 2009), as well as in EFs, such as working memory and set-shifting (Giehl et al., 2019; Kehagia et al., 2013; Monchi et al., 2006). Specifically, BG, ventromedial and ventrolateral PFC (vmPFC and vlPFC), and OFC are assumed to be involved in processing of feedback, emotionally connoted stimuli, and in the ability to anticipate future consequences (Gleichgerrcht et al., 2010; Pascucci et al., 2017; Rolls, 2000). In addition, the dlPFC and medial PFC (mPFC), as well as the ACC, may be engaged in risk/reward processing, error-detection ability, and cognitive control (Kondo et al., 2004; McCormick et al., 2019; Ramchandran et al., 2020).
Nevertheless, considering PD population and its pathophysiological features, and in particular (a) the patients’ risk-taking tendency described in literature, (b) the possible effects of dopamine on neural structures underlying EFs functioning and DM under ambiguity and risk, and (c) the crucial contribution of EFs on the decisional process, it appears important to focus on the relationship between DM and EFs to clarify those EF cognitive abilities that can support DM in patients or that, if impaired, may contribute to DM alterations.
Goals
According to the goals of a sco** review (Munn et al., 2018), the present article wants to provide the emergent results of a thorough analysis of the studies in literature about DM under ambiguity and risk in PD patients, exploring the relationship between decisional performance and EFs, highlighting possible gaps and further research questions. To date, no literature reviews have systematically investigated this relationship in PD patients through a comprehensive overview of the issue.
To investigate decisional competencies, we decided to focus principally on the Iowa Gambling Task (IGT; Bechara et al., 1994; Bechara, 2007) and the Game of Dice Task (GDT; Brand et al., 2005), which assess DM under ambiguity and under risk, respectively (see Table 2 for a detailed description of the tasks). We made this decision since they are considered the most commonly used and reliable tasks by the literature to address situations of ambiguity and risk (Buelow, 2015).
Method
The review was led according to the Preferred Reporting Items for Systematic Reviews and Meta-Analysis Extension for Sco** Reviews (PRISMAScR) (Tricco et al., 2018). A registered protocol is not required for sco** review (Munn et al., 2018).
The methodology of the review was designed according to the five-stage framework (Arksey & O’Malley, 2005) to provide transparency and to increase the reliability of the findings and the replicability of search strategies. Below, the five stages are reported in detail.
Identifying the research question (Stage 1)
The present sco** review was led to answer the following questions: Is there a relationship between EFs and DM under ambiguity in PD patients? Is there a relationship between EFs and DM under risk in PD patients?
Identifying relevant studies (Stage 2)
We examined studies that investigate DM under ambiguity and risk through the IGT and the GDT, which are the most reliable tasks investigating these constructs (see Goals paragraph for further details).
The last search update was made in May 2022. It encompassed articles published since 2000 in peer-reviewed journals indexed in Scopus, PubMed, and PsycINFO. The keywords entered were “Iowa Gambling Task AND (executive functions) AND (Parkinson’s Disease),” “Game of Dice Task AND (executive functions) AND (Parkinson’s Disease).” After Stage 3, the references of the selected studies were checked to include other possible eligible studies.
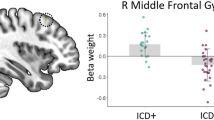
Then, the following inclusion criteria were adopted, ensuring comparisons among the studies to be analyzed: 1) studies that recruited samples of patients affected by PD in treatment with dopaminergic replacement therapies, which is the most common clinical condition for PD patients; 2) studies that assessed EFs through the administration of validated instruments; 3) studies that did not present a modified version of the IGT nor the GDT.
The exclusion criteria were: 1) studies in which patients are affected by an atypical parkinsonism (i.e., progressive supranuclear palsy, multiple system atrophy, corticobasal degeneration); 2) studies in which patients presented a diagnosis of ICD; 3) samples of subjects affected by psychiatric comorbidity (e.g., major depression, obsessive-compulsive behaviors, schizophrenia); 4) studies in which patients received deep brain stimulation; 5) studies in which participants underwent interventions to foster cognitive functioning (e.g., cognitive training, transcranial electric stimulation techniques); 6) book chapters.
Study selection (Stage 3)
Relevant articles were screened by one author (LC): first by title, keywords, and language used, and then by reading abstracts and full texts. The PRISMA Statement (Moher et al., 2009) was followed for the selection of the studies (Fig. 1). Possible doubts concerning the inclusion of the studies were analyzed by two other authors (AA and PI).
Charting the data (Stage 4)
A form was drafted to determine which variables to examine. When possible, the extraction of data followed Arksey and O’Malley’s (2005) recommendations to ensure comparisons between studies. Data reported concern authors and year of publication, countries in which the studies were led, samples characteristics (i.e., size of the sample, age and education information, the duration and the severity of the disease, “on”/“off” conditions in which patients were tested—considering the timing of dopaminergic drugs intake; Levodopa-equivalent daily dose – LEDD), parameters of the decisional tasks, assessed EFs and other cognitive functions and the tools used, and main results.
Collating, summarizing, and reporting the results (Stage 5)
To provide a narrative report of the results, an analytic framework was considered following the PRISMA guidelines – extension for sco** review (Tricco et al., 2018).
Results
Characteristics of the selected studies
A total of ten studies had been selected (Fig. 1), among which nine had administered the IGT (Euteneuer et al., 2009; Gescheidt et al., 2012; Ibarretxe-Bilbao et al., 2009; Kobayakawa et al., 2008; Kobayakawa et al., 2010; Mimura et al., 2006; Pagonabarraga et al., 2007; Perretta et al., 2005; ** brain. Developmental Review, 38, 55–68. https://doi.org/10.1016/j.dr.2015.07.001 " href="/article/10.3758/s13415-023-01106-3#ref-CR105" id="ref-link-section-d5963003e3165">2015). Although this conceptualization of EFs is not commonly used and only recent works considered it (Colautti et al., 2022; Damme et al., 2019), it may be useful for a comprehensive and more in-depth analysis of DM processes under ambiguity and risk and the relationship with EFs, considering both the affective aspects involved in reward processing and the cognitive load required by the task.
Furthermore, it appears promising to keep the focus on investigating the possible relationships between cognition (and especially EFs) and the affective aspects (including reward processing) in PD patients also to better understand DM in everyday life situations, which usually occur in a social context and implying direct or indirect consequences for oneself and others (Rilling & Sanfey, 2011). In this respect, moral DM has been recently considered, involving both the ability to infer others’ intentions (and more in general ToM) and cognitive control and EFs (Rosen et al., 2013, 2015). Results showed the presence of differences between HCs and PD patients in cognitive mechanisms related to moral DM. In HCs the decisional performance was related to ToM (Rosen et al., 2013), empathy, and EFs (Rosen et al., 2015), assuming that healthy participants may strategically use such abilities, in particular ToM, facilitating the anticipation and the evaluation of possible consequences implied in choice options. While in PD group no correlation emerged, indicating that patients may not (or present difficult to) integrate these abilities in the decisional process, possibly due to dysfunctions encompassing structures belonging to the corticostriatal circuits (Rosen et al., 2013, 2015), which may result in suboptimal or selfish decisions. Similarly, studies that investigated deceptive DM (a specific type of moral DM; Ponsi et al., 2021) found impaired or reduced deceptive behaviors in patients affected by PD and essential tremor compared with HC groups (Abe et al., 2009; Abe et al., 2018; Mameli et al., 2013). Patients’ displayed performance involved i) difficulties in managing deceptive responses underlain executive dysfunctions, which can be linked to dorsolateral prefrontal circuit functioning (Abe et al., 2009; Mameli et al., 2013), and ii) a reduced motivation to engage in dishonest behaviors, possibly underlain impairment in reward processing where nucleus accumbens may be pivotal (Abe et al., 2018; Ponsi et al., 2021). Such a finding also can be supported by patients affected by movement disorders with ICDs, who generally show the opposite behaviors characterized by a higher tendency in engaging in suboptimal and dishonest decisions, such as lying frequently to hide their pathological behaviors (Brusa et al., 2016; Cilia et al., 2014). Such a tendency may possibly underlie an increased neural response in the nucleus accumbens and more in general in the ventral striatum, which can foster the salience for rewarding stimuli (Abe et al., 2014; Martini et al., 2018; Ponsi et al., 2021). Such findings are consistent with those of the present review, highlighting the presence of a delicate balance in movement disorders between high-order cognition and affective/reward processes supported by cortical and subcortical structures belonging to corticostriatal circuits and affected by the disease.
Importance of longitudinal studies in studying DM performance and its relationship with EFs
Regarding the possible effects of dopaminergic treatment reported in literature on DM, in the considered studies no direct relationships emerged between the decisional performance and neither the dosage of dopaminergic replacement therapies nor patients’ clinical conditions. A possible explanation may be that the decisional performance can be influenced by the long-term neurobiological or molecular effects of dopamine replacement therapy on reward-processing circuits (Pignatelli & Bonci, 2015; Volkow & Morales, 2015, for neuroplasticity in dopamine circuits). It may be not sufficient to design cross-sectional studies to investigate possible relationships between DM performances and dopaminergic drugs in PD patients or—to have a more comprehensive framework—between DM and EFs and whether and how the dopaminergic therapy can affect such a relationship. In fact, considering the relationship between DM under ambiguity and risk, EFs, and the neural changes that can occur in corticostriatal circuits with the progression of PD, future studies, including longitudinal designs, may be required to explore possible changes in decisional processes and in the relationships with EFs over time. This could be useful to i) take under control the PD samples’ clinical variability, which can undermine possible comparisons and generalizations of the results; ii) observe possible modifications of the relations between DM and EFs over time, bearing in mind that both cognitive efficiency and neural areas involved by PD change throughout the disease progression; iii) delve into the possible role that dopaminergic drugs play in the relationship between DM and EFs, assessing and observing patients over time, also before the first intake of the dopamine replacement therapy (i.e., de novo patients); iv) provide further results that can explain—and maybe confirm—findings that are present in the literature so far (Colautti et al., 2021; Cools et al., 2022; Kjær et al., 2018).
Limitations
The present study has some limitations. First of all, heterogeneity among the studies was present, even though inclusion/exclusion criteria were designed to reduce it ensuring comparisons. Such heterogeneity may depend on the different study designs, methodologies adopted for collecting and analyzing data, and tests used to assess EFs. Furthermore, clinical features of PD patients varied across the studies (e.g., the duration of the disease was different, possibly underlying different stages of the PD progression, and consequently different subcortical and cortical impairments due to the disease; LEDD also varies across patients of the same study). Thus, we cannot exclude that, at least in part, results may be biased by these clinical features, undermining possible generalizations of the findings. Otherwise, PD patients are generally characterized by higher subjective variability in clinical characteristics, making it difficult to make a strict homogeneous selection of the patients considering all the clinical parameters. Another limitation concerns the low number of studies that investigated the relationships between DM and EFs in PD patients (especially those that administered the GDT), due to the constraint to investigate only the IGT and the GDT. Such a constraint can be seen as another limitation, because the IGT and the GDT are the only tasks that we considered to study this relationship, thus potentially losing information from studies that used other instruments. However, we believe that limiting the focus only to the two most used and reliable tasks to address conditions of ambiguity and risk could facilitate the comparison of studies’ results, by controlling in this way potential differences in behavioral responses that may be due to the different structures and feedback modalities of the several DM tasks (Schiebener and Brand, 2015). To sum up, further studies would be desirable to replicate results increasing the number of studies considering other decisional tasks and to better understand how EFs can support DM in PD patients.
Conclusions and clinical implications
In the present sco** review, we tried to shed light on the DM mechanisms in PD patients, investigating results in literature concerning the relationship between DM under ambiguity and risk and EFs. Findings suggested that such a relationship is complex and dynamic and EFs seem to have a pivotal role, especially when the cognitive load required by the decisional situation is high, as it happens under situations of risk where more data are available to make a decision. Whilst, when a low number of data are available, it seems that EFs play a minor role. This is in line with the assumption that DM under conditions of ambiguity mainly involves circuits that link BG with OFC and the limbic system (in line with correlations found between the IGT and ToM tests), while DM under risk also underlies the circuit linking BG with dlPFC, which mostly sustains EFs functioning (Brand et al., 2004; Euteneuer et al., 2009; ** dementia and affecting patients’ autonomy (Saredakis et al., 2019).
Data availability
Not applicable.
References
Abe, N., & Greene, J. D. (2014). Response to anticipated reward in the nucleus accumbens predicts behavior in an independent test of honesty. Journal of Neuroscience, 34(32), 10564–10572. https://doi.org/10.1523/JNEUROSCI.0217-14.2014
Abe, N., Fujii, T., Hirayama, K., Takeda, A., Hosokai, Y., Ishioka, T., et al. (2009). Do parkinsonian patients have trouble telling lies? The neurobiological basis of deceptive behaviour. Brain, 132(5), 1386–1395. https://doi.org/10.1093/brain/awp052
Abe, N., Kawasaki, I., Hosokawa, H., Baba, T., & Takeda, A. (2018). Do patients with Parkinson’s disease exhibit reduced cheating behavior? A neuropsychological study. Frontiers in Neurology, 9, 378. https://doi.org/10.3389/fneur.2018.00378
Alexander, G. E., DeLong, M. R., & Strick, P. L. (1986). Parallel organization of functionally segregated circuits linking basal ganglia and cortex. Annual review of neuroscience, 9(1), 357–381. https://doi.org/10.1146/annurev.ne.09.030186.002041
Argyelan, M., Herzallah, M., Sako, W., DeLucia, I., Sarpal, D., Vo, A., & Gluck, M. (2018). Dopamine modulates striatal response to reward and punishment in patients with Parkinson’s disease: A pharmacological challenge fMRI study. Neuroreport, 29(7), 532. https://doi.org/10.1097/WNR.0000000000000970
Arksey, H., & O’Malley, L. (2005). Sco** studies: Towards a methodological framework. International Journal of Social Research Methodology, 8(1), 19–32. https://doi.org/10.1080/1364557032000119616
Baig, F., Kelly, M. J., Lawton, M. A., Ruffmann, C., Rolinski, M., Klein, J. C., & Hu, M. T. (2019). Impulse control disorders in Parkinson disease and RBD: A longitudinal study of severity. Neurology, 93(7), e675–e687. https://doi.org/10.1212/WNL.0000000000007942
Balestrino, R., & Schapira, A. H. V. (2020). Parkinson disease. European Journal of Neurology, 27(1), 27–42. https://doi.org/10.1111/ene.14108
Bechara, A., Damasio, A. R., Damasio, H., & Anderson, S. W. (1994). Insensitivity to future consequences following damage to human prefrontal cortex. Cognition, 50, 7–15. https://doi.org/10.1016/0010-0277(94)90018-3
Bechara, A., Damasio, H., Damasio, A. R., & Lee, G. P. (1999). Different contributions of the human amygdala and ventromedial prefrontal cortex to decision-making. Journal of Neuroscience, 19(13), 5473–5481. https://doi.org/10.1523/JNEUROSCI.19-13-05473.1999
Bechara, A. (2007). Iowa gambling task professional manual. Psychological Assessment Resources.
Benussi, A., Alberici, A., Cantoni, V., Manenti, R., Brambilla, M., Dell’Era, V., et al. (2017). Modulating risky decision-making in Parkinson’s disease by transcranial direct current stimulation. European Journal of Neurology, 24(5), 751–754. https://doi.org/10.1111/ene.13286
Bodden, M. E., Kübler, D., Knake, S., Menzler, K., Heverhagen, J. T., Sommer, J., et al. (2013). Comparing the neural correlates of affective and cognitive theory of mind using fMRI: Involvement of the basal ganglia in affective theory of mind. Advances in Cognitive Psychology, 9(1), 32. https://doi.org/10.5709/acp-0129-6
Bora, E., Walterfang, M., & Velakoulis, D. (2015). Theory of mind in Parkinson’s disease: A meta-analysis. Behavioural Brain Research, 292, 515–520. https://doi.org/10.1016/j.bbr.2015.07.012
Braak, H., Del Tredici, K., Rüb, U., De Vos, R. A., Steur, E. N. J., & Braak, E. (2003). Staging of brain pathology related to sporadic Parkinson’s disease. Neurobiology of Aging, 24(2), 197–211. https://doi.org/10.1016/S0197-4580(02)00065-9
Braak, H., & Del Tredici, K. (2008). Cortico-basal ganglia-cortical circuitry in Parkinson’s disease reconsidered. Experimental Neurology, 212(1), 226–229. https://doi.org/10.1016/j.expneurol.2008.04.001
Brand, M., Labudda, K., Kalbe, E., Hilker, R., Emmans, D., Fuchs, G., et al. (2004). Decision-making impairments in patients with Parkinson’s disease. Behavioural Neurology, 15(3-4), 77–85. https://doi.org/10.1155/2004/578354
Brand, M., Fujiwara, E., Borsutzky, S., Kalbe, E., Kessler, J., & Markowitsch, H. J. (2005). Decision-making deficits of Korsakoff patients in a new gambling task with explicit rules: Associations with executive functions. Neuropsychology, 19, 267–277. https://doi.org/10.1037/0894-4105.19.3.267
Brand, M., Labudda, K., & Markowitsch, H. J. (2006). Neuropsychological correlates of decision-making in ambiguous and risky situations. Neural Networks, 19(8), 1266–1276. https://doi.org/10.1016/j.neunet.2006.03.001
Brand, M., Recknor, E. C., Grabenhorst, F., & Bechara, A. (2007). Decisions under ambiguity and decisions under risk: Correlations with executive functions and comparisons of two different gambling tasks with implicit and explicit rules. Journal of Clinical and Experimental Neuropsychology, 29(1), 86–99. https://doi.org/10.1080/13803390500507196
Brusa, L., Pavino, V., Massimetti, M. C., Ceravolo, R., Stefani, S., & Stanzione, P. (2016). Pathological Gambling in Parkinson's disease patients: Dopaminergic medication or personality traits fault? Journal of the Neurological Sciences, 366, 167–170. https://doi.org/10.1016/j.jns.2016.03.032
Buelow, M. T. (2015). Predicting performance on the Columbia Card Task: Effects of personality characteristics, mood, and executive functions. Assessment, 22(2), 178–187. https://doi.org/10.1177/1073191114539383
Chan, R. C., Shum, D., Toulopoulou, T., & Chen, E. Y. (2008). Assessment of executive functions: Review of instruments and identification of critical issues. Archives of Clinical Neuropsychology, 23(2), 201–216. https://doi.org/10.1016/j.acn.2007.08.010
Chen, H., Wang, K., Scheperjans, F., & Killinger, B. (2022). Environmental triggers of Parkinson’s disease–Implications of the Braak and dual-hit hypotheses. Neurobiology of Disease, 163, 105601. https://doi.org/10.1016/j.nbd.2021.105601
Cilia, R., Siri, C., Colombo, A., & Pezzoli, G. (2014). Multiple compulsive behaviors in multiple system atrophy: The importance of predisposition to addiction. Parkinsonism & Related Disorders, 20(3), 355–357. https://doi.org/10.1016/j.parkreldis.2013.12.010
Colautti, L., Iannello, P., Silveri, M. C., & Antonietti, A. (2021). Decision making in Parkinson’s disease: An analysis of the studies using the Iowa Gambling Task. European Journal of Neuroscience, 54(10), 7513–7549. https://doi.org/10.1111/ejn.15497
Colautti, L., Antonietti, A., & Iannello, P. (2022). Executive functions in decision making under ambiguity and risk in healthy adults: A sco** review adopting the hot and cold executive functions perspective. Brain Sciences, 12(10), 1335. https://doi.org/10.3390/brainsci12101335
Colombo, B., Iannello, P., Puglisi, G., & Antonietti, A. (2020). Personal impulsivity mediates the effects of neuromodulation in economic intertemporal choices: A pilot study. Studia Psychologica, 62, 123–137. https://doi.org/10.31577/sp.2020.02.795
Cools, R., Barker, R. A., Sahakian, B. J., & Robbins, T. W. (2001). Enhanced or impaired cognitive function in Parkinson’s disease as a function of dopaminergic medication and task demands. Cerebral Cortex, 11(12), 1136–1143. https://doi.org/10.1093/cercor/11.12.1136
Cools, R., Tichelaar, J. G., Helmich, R. C., Bloem, B. R., Esselink, R. A., Smulders, K., & Timmer, M. H. (2022). Role of dopamine and clinical heterogeneity in cognitive dysfunction in Parkinson’s disease. Progress in Brain Research, 269(1), 309–343. https://doi.org/10.1016/bs.pbr.2022.01.012
Costello, H., Berry, A. J., Reeves, S., Weil, R. S., Joyce, E. M., Howard, R., & Roiser, J. P. (2021). Disrupted reward processing in Parkinson’s disease and its relationship with dopamine state and neuropsychiatric syndromes: A systematic review and meta-analysis. Journal of Neurology, Neurosurgery & Psychiatry, 93(5), 555–562. https://doi.org/10.1136/jnnp-2021-327762
Coundouris, S. P., Adams, A. G., & Henry, J. D. (2020). Empathy and theory of mind in Parkinson’s disease: A meta-analysis. Neuroscience & Biobehavioral Reviews, 109, 92–102. https://doi.org/10.1016/j.neubiorev.2019.12.030
Damme, K. S. F., Kelley, N. J., Quinn, M. E., Glazer, J. E., Chat, I. K.-Y., Young, K. S., et al. (2019). Emotional content impacts how executive function ability relates to willingness to wait and to work for reward. Cognitive, Affective, & Behavioral Neuroscience, 19(3), 637–652. https://doi.org/10.3758/s13415-019-00712-4
Del Missier, F., Mäntylä, T., & Bruine de Bruin, W. (2010). Executive functions in decision making: An individual differences approach. Thinking & Reasoning, 16(2), 69–97. https://doi.org/10.1080/13546781003630117
Drew, D. S., Muhammed, K., Baig, F., Kelly, M., Saleh, Y., Sarangmat, N., et al. (2020). Dopamine and reward hypersensitivity in Parkinson’s disease with impulse control disorder. Brain, 143(8), 2502–2518. https://doi.org/10.1093/brain/awaa198
Dujardin, K., & Laurent, B. (2003). Dysfunction of the human memory systems: Role of the dopaminergic transmission. Current Opinion in Neurology, 16, S11–S16.
Evens, R., Hoefler, M., Biber, K., & Lueken, U. (2016). The Iowa Gambling Task in Parkinson’s disease: A meta-analysis on effects of disease and medication. Neuropsychologia, 91, 163–172. https://doi.org/10.1016/j.neuropsychologia.2016.07.032
Euteneuer, F., Schaefer, F., Stuermer, R., Boucsein, W., Timmermann, L., Barbe, M. T., & Kalbe, E. (2009). Dissociation of decision-making under ambiguity and decision-making under risk in patients with Parkinson’s disease: A neuropsychological and psychophysiological study. Neuropsychologia, 47(13), 2882–2890. https://doi.org/10.1016/j.neuropsychologia.2009.06.014
Fein, G., McGillivray, S., & Finn, P. (2007). Older adults make less advantageous decisions than younger adults: Cognitive and psychological correlates. Journal of the International Neuropsychological Society, 13(3), 480–489. https://doi.org/10.1017/S135561770707052X
Ferrer, I. (2009). Early involvement of the cerebral cortex in Parkinson’s disease: Convergence of multiple metabolic defects. Progress in Neurobiology, 88(2), 89–103. https://doi.org/10.1016/j.pneurobio.2009.02.004
Foerde, K., & Shohamy, D. (2011). The role of the basal ganglia in learning and memory: Insight from Parkinson’s disease. Neurobiology of Learning and Memory, 96(4), 624–636. https://doi.org/10.1016/j.nlm.2011.08.006
Folstein, M. F., Folstein, S. E., & McHugh, P. R. (1975). “Mini-mental state”: A practical method for grading the cognitive state of patients for the clinician. Journal of Psychiatric Research, 12(3), 189–198.
Forte, G., Morelli, M., & Casagrande, M. (2021). Heart rate variability and decision-making: Autonomic responses in making decisions. Brain Sciences, 11(2), 243. https://doi.org/10.3390/brainsci11020243
Gescheidt, T., Czekóová, K., Urbánek, T., Mareček, R., Mikl, M., Kubíková, R., et al. (2012). Iowa Gambling Task in patients with early-onset Parkinson’s disease: Strategy analysis. Neurological Sciences, 33(6), 1329–1335. https://doi.org/10.1007/s10072-012-1086-x
Giehl, K., Tahmasian, M., Eickhoff, S. B., & van Eimeren, T. (2019). Imaging executive functions in Parkinson's disease: An activation likelihood estimation meta-analysis. Parkinsonism & Related Disorders, 63, 137–142. https://doi.org/10.1016/j.parkreldis.2019.02.015
Gleichgerrcht, E., Ibáñez, A., Roca, M., Torralva, T., & Manes, F. (2010). Decision-making cognition in neurodegenerative diseases. Nature Reviews Neurology, 6(11), 611. https://doi.org/10.1038/nrneurol.2010.148
Gotham, A. M., Brown, R. G., & Marsden, C. D. (1986). Levodopa treatment may benefit or impair “frontal” function in Parkinson’s disease. The Lancet, 328(8513), 970–971. https://doi.org/10.1016/S0140-6736(86)90617-3
Hartmann, A. J., Mueller, M., & Kirchler, E. (2020). Tax Compliance. In Research Methods and Decision Processes (pp. 291–330). Springer International Publishing. https://doi.org/10.1007/978-3-030-45500-2_13
Hikida, T., Kimura, K., Wada, N., Funabiki, K., & Nakanishi, S. (2010). Distinct roles of synaptic transmission in direct and indirect striatal pathways to reward and aversive behavior. Neuron, 66(6). https://doi.org/10.1016/j.neures.2011.07.311
Hoehn, M., & Yahr, M. (1967). Parkinsonism: Onset, progression and mortality. Neurology, 17(5), 427–442. https://doi.org/10.1212/wnl.17.5.427
Ibarretxe-Bilbao, N., Junque, C., Tolosa, E., Marti, M. J., Valldeoriola, F., Bargallo, N., & Zarei, M. (2009). Neuroanatomical correlates of impaired decision-making and facial emotion recognition in early Parkinson’s disease. European Journal of Neuroscience, 30(6), 1162–1171. https://doi.org/10.1111/j.1460-9568.2009.06892.x
Jahanshahi, M., Wilkinson, L., Gahir, H., Dharminda, A., & Lagnado, D. A. (2010). Medication impairs probabilistic classification learning in Parkinson’s disease. Neuropsychologia, 48(4), 1096–1103. https://doi.org/10.1016/j.neuropsychologia.2009.12.010
Kehagia, A. A., Barker, R. A., & Robbins, T. W. (2013). Cognitive impairment in Parkinson’s disease: The dual syndrome hypothesis. Neurodegenerative diseases, 11(2), 79–92. https://doi.org/10.1159/000341998
Kim, S., & Lee, D. (2011). Prefrontal cortex and impulsive decision making. Biological Psychiatry, 69(12), 1140–1146. https://doi.org/10.1016/j.biopsych.2010.07.005
Kjær, S. W., Damholdt, M. F., & Callesen, M. B. (2018). A systematic review of decision-making impairments in Parkinson’s disease: Dopaminergic medication and methodological variability. Basal Ganglia, 14, 31–40. https://doi.org/10.1016/j.baga.2018.07.003
Kobayashi, S., Asano, K., Matsuda, N., & Ugawa, Y. (2019). Dopaminergic influences on risk preferences of Parkinson’s disease patients. Cognitive, Affective, & Behavioral Neuroscience, 19(1), 88–97. https://doi.org/10.3758/s13415-018-00646-3
Kobayakawa, M., Koyama, S., Mimura, M., & Kawamura, M. (2008). Decision making in Parkinson’s disease: Analysis of behavioral and physiological patterns in the Iowa gambling task. Movement Disorders, 23(4), 547–552. https://doi.org/10.1002/mds.21865
Kobayakawa, M., Tsuruya, N., & Kawamura, M. (2010). Sensitivity to reward and punishment in Parkinson’s disease: An analysis of behavioral patterns using a modified version of the Iowa gambling task. Parkinsonism & Related Disorders, 16(7), 453–457. https://doi.org/10.1016/j.parkreldis.2010.04.011
Kondo, H., Osaka, N., & Osaka, M. (2004). Cooperation of the anterior cingulate cortex and dorsolateral prefrontal cortex for attention shifting. Neuroimage, 23(2), 670–679. https://doi.org/10.1016/j.neuroimage.2004.06.014
Kravitz, A. V., Tye, L. D., & Kreitzer, A. C. (2012). Distinct roles for direct and indirect pathway striatal neurons in reinforcement. Nature Neuroscience, 15(6), 816–818. https://doi.org/10.1038/nn.3100
Labudda, K., Frigge, K., Horstmann, S., Aengenendt, J., Woermann, F. G., Ebner, A., et al. (2009). Decision making in patients with temporal lobe epilepsy. Neuropsychologia, 47(1), 50–58. https://doi.org/10.1016/j.neuropsychologia.2008.08.014
Lauriola, M., Levin, I. P., & Hart, S. S. (2007). Common and distinct factors in decision making under ambiguity and risk: A psychometric study of individual differences. Organizational Behavior and Human Decision Processes, 104(2), 130–149. https://doi.org/10.1016/j.obhdp.2007.04.001
Lejuez, C. W., Read, J. P., Kahler, C. W., Richards, J. B., Ramsey, S. E., Stuart, G. L., et al. (2002). Evaluation of a behavioral measure of risk taking: The Balloon Analogue Risk Task (BART). Journal of Experimental Psychology: Applied, 8(2), 75. https://doi.org/10.1037//1076-898x.8.2.75
Mameli, F., Tomasini, E., Scelzo, E., Fumagalli, M., Ferrucci, R., Bertolasi, L., & Priori, A. (2013). Lies tell the truth about cognitive dysfunction in essential tremor: An experimental deception study with the guilty knowledge task. Journal of Neurology, Neurosurgery & Psychiatry, 84(9), 1008–1013. https://doi.org/10.1136/jnnp-2012-304674
Martini, A., Dal Lago, D., Edelstyn, N. M., Salgarello, M., Lugoboni, F., & Tamburin, S. (2018). Dopaminergic neurotransmission in patients with Parkinson's disease and impulse control disorders: A systematic review and meta-analysis of PET and SPECT studies. Frontiers in Neurology, 9, 1018. https://doi.org/10.3389/fneur.2018.01018
McCormick, M., Reyna, V. F., Ball, K., Katz, J., & Deshpande, G. (2019). Neural underpinnings of financial decision bias in older adults: Putative theoretical models and a way to reconcile them. Frontiers in Neuroscience, 13, 184. https://doi.org/10.3389/fnins.2019.00184
McCoy, B., Jahfari, S., Engels, G., Knapen, T., & Theeuwes, J. (2019). Dopaminergic medication reduces striatal sensitivity to negative outcomes in Parkinson’s disease. Brain, 142(11), 3605–3620. https://doi.org/10.1093/brain/awz276
Mimura, M., Oeda, R., & Kawamura, M. (2006). Impaired decision-making in Parkinson’s disease. Parkinsonism & Related Disorders, 12(3), 169–175. https://doi.org/10.1016/j.parkreldis.2005.12.003
Moher, D., Liberati, A., Tetzlaff, J., Altman, D. G., & PRISMA Group. (2009). Preferred reporting items for systematic reviews and meta-analyses: The PRISMA statement. Annals of Internal Medicine, 151(4), 264–269. https://doi.org/10.7326/0003-4819-151-4-200908180-00135
Monchi, O., Ko, J. H., & Strafella, A. P. (2006). Striatal dopamine release during performance of executive functions: A [11C] raclopride PET study. Neuroimage, 33(3), 907–912. https://doi.org/10.1016/j.neuroimage.2006.06.058
Moustafa, A. A., Chakravarthy, S., Phillips, J. R., Gupta, A., Keri, S., Polner, B., et al. (2016). Motor symptoms in Parkinson’s disease: A unified framework. Neuroscience & Biobehavioral Reviews, 68, 727–740. https://doi.org/10.1016/j.neubiorev.2016.07.010
Munn, Z., Peters, M. D., Stern, C., Tufanaru, C., McArthur, A., & Aromataris, E. (2018). Systematic review or sco** review? Guidance for authors when choosing between a systematic or sco** review approach. BMC Medical Research Methodology, 18(1), 1–7. https://doi.org/10.1186/s12874-018-0611-x
Nelson, H. E. (1976). A modified card sorting test sensitive to frontal lobe defects. Cortex, 12(4), 313–324. https://doi.org/10.1016/S0010-9452(76)80035-4
Pagonabarraga, J., García-Sánchez, C., Llebaria, G., Pascual-Sedano, B., Gironell, A., & Kulisevsky, J. (2007). Controlled study of decision-making and cognitive impairment in Parkinson’s disease. Movement Disorders, 22(10), 1430–1435. https://doi.org/10.1002/mds.21457
Pascucci, D., Hickey, C., Jovicich, J., & Turatto, M. (2017). Independent circuits in basal ganglia and cortex for the processing of reward and precision feedback. NeuroImage, 162, 56–64. https://doi.org/10.1016/j.neuroimage.2017.08.067
Perretta, J. G., Pari, G., & Beninger, R. J. (2005). Effects of Parkinson disease on two putative nondeclarative learning tasks: Probabilistic classification and gambling. Cognitive and Behavioral Neurology, 18(4), 185–192. https://doi.org/10.1097/01.wnn.0000187939.81541.1d
Pfeiffer, R. F. (2016). Non-motor symptoms in Parkinson’s disease. Parkinsonism & Related Disorders, 22, S119–S122. https://doi.org/10.1016/j.parkreldis.2015.09.004
Pignatelli, M., & Bonci, A. (2015). Role of dopamine neurons in reward and aversion: A synaptic plasticity perspective. Neuron, 86(5), 1145–1157. https://doi.org/10.1016/j.neuron.2015.04.015
Pillon, B., Deweer, B., Agid, Y., & Dubois, B. (1993). Explicit memory in Alzheimer’s, Huntington’s, and Parkinson’s diseases. Archives of Neurology, 50(4), 374–379. https://doi.org/10.1001/archneur.1993.00540040036010
Poletti, M., & Bonuccelli, U. (2010). Funzioni cognitive nella Malattia di Parkinson. [Cognitive functions in Parkinson’s disease]. Giornale Italiano di Psicologia, 37, 523–550. https://doi.org/10.1421/32900
Poletti, M., & Bonuccelli, U. (2013). Acute and chronic cognitive effects of levodopa and dopamine agonists on patients with Parkinson’s disease: A review. Therapeutic Advances in Psychopharmacology, 3(2), 101–113. https://doi.org/10.1177/2045125312470130
Ponsi, G., Scattolin, M., Villa, R., & Aglioti, S. M. (2021). Human moral decision-making through the lens of Parkinson’s disease. npj. Parkinson's Disease, 7(1), 18. https://doi.org/10.1038/s41531-021-00167-w
Premack, D., & Woodruff, G. (1978). Does the chimpanzee have a theory of mind? Behavioral and Brain Sciences, 1(4), 515–526. https://doi.org/10.1017/S0140525X00076512
Ramchandran, K., Tranel, D., Duster, K., & Denburg, N. L. (2020). The role of emotional vs. cognitive intelligence in economic decision-making amongst older adults. Frontiers in Neuroscience, 14, 497. https://doi.org/10.3389/fnins.2020.00497
Rangel, A., Camerer, C., & Montague, P. R. (2008). A framework for studying the neurobiology of value-based decision making. Nature Reviews Neuroscience, 9(7), 545–556. https://doi.org/10.1038/nrn2357
Rilling, J. K., & Sanfey, A. G. (2011). The neuroscience of social decision-making. Annual review of psychology, 62, 23–48. https://doi.org/10.1146/annurev.psych.121208.131647
Rogers, R. D., Owen, A. M., Middleton, H. C., Williams, E. J., Pickard, J. D., Sahakian, B. J., & Robbins, T. W. (1999). Choosing between small, likely rewards and large, unlikely rewards activates inferior and orbital prefrontal cortex. Journal of Neuroscience, 19(20), 9029–9038. https://doi.org/10.1523/JNEUROSCI.19-20-09029.1999
Rolls, E. T. (2000). The orbitofrontal cortex and reward. Cerebral Cortex, 10(3), 284–294. https://doi.org/10.1093/cercor/10.3.284
Rosen, J. B., Brand, M., Polzer, C., Ebersbach, G., & Kalbe, E. (2013). Moral decision-making and theory of mind in patients with idiopathic Parkinson’s disease. Neuropsychology, 27(5), 562. https://doi.org/10.1037/a0033595
Rosen, J. B., Rott, E., Ebersbach, G., & Kalbe, E. (2015). Altered moral decision-making in patients with idiopathic Parkinson's disease. Parkinsonism & related disorders, 21(10), 1191–1199. https://doi.org/10.1016/j.parkreldis.2015.08.016
Ryterska, A., Jahanshahi, M., & Osman, M. (2014). Decision-making impairments in Parkinson’s disease as a by-product of defective cost–benefit analysis and feedback processing. Neurodegenerative Disease Management, 4(4), 317–327. https://doi.org/10.2217/nmt.14.23
Salehinejad, M. A., Ghanavati, E., Rashid, M. H. A., & Nitsche, M. A. (2021). Hot and cold executive functions in the brain: A prefrontal-cingular network. Brain and Neuroscience Advances, 5, 23982128211007769. https://doi.org/10.1177/23982128211007769
Salvatore, M. F., Soto, I., Alphonso, H., Cunningham, R., James, R., & Nejtek, V. A. (2021). Is there a neurobiological rationale for the utility of the Iowa Gambling Task in Parkinson’s disease? Journal of Parkinson’s Disease, 11(2), 405–419. https://doi.org/10.3233/JPD-202449
Saredakis, D., Collins-Praino, L. E., Gutteridge, D. S., Stephan, B. C., & Keage, H. A. (2019). Conversion to MCI and dementia in Parkinson’s disease: A systematic review and meta-analysis. Parkinsonism & Related Disorders, 65, 20–31. https://doi.org/10.1016/j.parkreldis.2019.04.020
Schiebener, J., & Brand, M. (2015). Decision making under objective risk conditions–a review of cognitive and emotional correlates, strategies, feedback processing, and external influences. Neuropsychol Review 25, 171–198. https://doi.org/10.1007/s11065-015-9285-x
Schultz, W., Preuschoff, K., Camerer, C., Hsu, M., Fiorillo, C. D., Tobler, P. N., & Bossaerts, P. (2008). Explicit neural signals reflecting reward uncertainty. Philosophical Transactions of the Royal Society B: Biological Sciences, 363(1511), 3801–3811. https://doi.org/10.1098/rstb.2008.0152
Seymour, B., Daw, N., Dayan, P., Singer, T., & Dolan, R. (2007). Differential encoding of losses and gains in the human striatum. Journal of Neuroscience, 27(18), 4826–4831. https://doi.org/10.1523/JNEUROSCI.0400-07.2007
Shurman, B., Horan, W. P., & Nuechterlein, K. H. (2005). Schizophrenia patients demonstrate a distinctive pattern of decision-making impairment on the Iowa Gambling Task. Schizophrenia research, 72(2-3), 215–224. https://doi.org/10.1016/j.schres.2004.03.020
Stenberg, G. (2016). Impulse control disorders–The Continuum Hypothesis. Journal of Parkinson’s disease, 6(1), 67–75. https://doi.org/10.3233/JPD-150770
Strauss, E., Sherman, E. M. S., & Spreen, O. (2006). A compendium of neuropsychological tests: Administration, norms, and commentary (3rd ed.). Oxford University Press.
Tricco, A. C., Lillie, E., Zarin, W., O’Brien, K. K., Colquhoun, H., Levac, D., et al. (2018). PRISMA extension for sco** reviews (PRISMA-ScR): Checklist and explanation. Annals of Internal Medicine, 169(7), 467–473. https://doi.org/10.7326/M18-0850
Volkow, N. D., & Morales, M. (2015). The brain on drugs: From reward to addiction. Cell, 162(4), 712–725. https://doi.org/10.1016/j.cell.2015.07.046
Weintraub, D., David, A. S., Evans, A. H., Grant, J. E., & Stacy, M. (2015). Clinical spectrum of impulse control disorders in Parkinson’s disease. Movement Disorders, 30(2), 121–127. https://doi.org/10.1002/mds.26016
**, C., Zhu, Y., Mu, Y., Chen, B., Dong, B., Cheng, H., et al. (2015). Theory of mind and decision-making processes are impaired in Parkinson’s disease. Behavioural Brain Research, 279, 226–233. https://doi.org/10.1016/j.bbr.2014.11.035
Zelazo, P. D. (2015). Executive function: Reflection, iterative reprocessing, complexity, and the develo** brain. Developmental Review, 38, 55–68. https://doi.org/10.1016/j.dr.2015.07.001
Zgaljardic, D. J., Borod, J. C., Foldi, N. S., & Mattis, P. (2003). A review of the cognitive and behavioral sequelae of Parkinson's disease: Relationship to frontostriatal circuitry. Cognitive and behavioral neurology, 16(4), 193–210.
Zgaljardic, D. J., Borod, J. C., Foldi, N. S., Mattis, P. J., Gordon, M. F., Feigin, A., & Eidelberg, D. (2006). An examination of executive dysfunction associated with frontostriatal circuitry in Parkinson’s disease. Journal of Clinical and Experimental Neuropsychology, 28(7), 1127–1144. https://doi.org/10.1080/13803390500246910
Zha, R., Li, P., Liu, Y., Alarefi, A., Zhang, X., & Li, J. (2022). The orbitofrontal cortex represents advantageous choice in the Iowa gambling task. Human Brain Map**, 43(12), 3840–3856. https://doi.org/10.1002/hbm.25887
Code availability
Not applicable.
Funding
Open access funding provided by Università Cattolica del Sacro Cuore within the CRUI-CARE Agreement. No funds, grants, or other support was received.
Author information
Authors and Affiliations
Contributions
All authors meet authorship criteria. LC conceptualized the study, designed the methodology, provided the study materials, curated the data, and mainly wrote the manuscript. PI conceptualized the study, designed the methodology, reviewed and edited the manuscript, and supervised the study. MCS reviewed and edited the manuscript and supervised the study. AA conceptualized the study, designed the methodology, reviewed and edited the manuscript, and supervised the study. All authors certify that they have participated sufficiently in work to take public responsibility for the content, including participation in the manuscript’s concept, design, analysis, writing, or revision. All authors have approved the final article.
Corresponding author
Ethics declarations
Ethics approval
Not applicable.
Consent to participate
Not applicable.
Consent for publication
Not applicable.
Conflicts of interest/Competing interests
The authors have no competing interests to declare that are relevant to the content of this article.
Additional information
Open practices statement
A registered protocol is not required for sco** review (Munn et al., 2018).
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Colautti, L., Iannello, P., Silveri, M.C. et al. Decision-making under ambiguity and risk and executive functions in Parkinson’s disease patients: A sco** review of the studies investigating the Iowa Gambling Task and the Game of Dice. Cogn Affect Behav Neurosci 23, 1225–1243 (2023). https://doi.org/10.3758/s13415-023-01106-3
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.3758/s13415-023-01106-3