Abstract
Background
Due to increased life expectancy, the number of elderly patients with gastric cancer is increasing. This study was designed to determine the role of preoperative frailty (PF) as a risk factor for postoperative complications and prognosis in the oldest elderly gastric cancer patients undergoing curative resection.
Methods
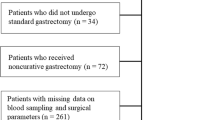
A total of 165 patients older than 80 years who underwent radical gastrectomy for primary gastric cancer between 2000 and 2012 were analyzed. We collected data on the inflammation-nutritional status, morbidity, and survival of these patients. The relationship between postoperative complications and PF was analyzed by logistic regression, and a Cox proportional hazards model was performed to identify the prognostic factors.
Results
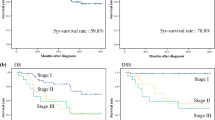
A total of 54 (32.7%) patients were considered frail. PF was associated with an increased risk for postoperative complications [odds ratio (OR) 3.396; 95% confidence interval (CI) 1.046–11.025; P = 0.042]. With a median follow-up of 37.0 (range 1.0–77.8) months, the 3 year overall survival (OS), recurrence-free survival (RFS), and cancer-specific survival (CSS) rates in the entire cohort were 46.1, 34.4, and 49.2%, respectively. A multivariate analysis of the inflammation-based prognostic factors showed that only PF was independently associated with OS (OR 1.613; 95% CI 1.052–2.473; P = 0.028), RFS (OR 1.859; 95% CI 1.279–2.703; P = 0.001), and CSS (OR 1.859; 95% CI 1.279–2.703; P = 0.001).
Conclusions
Frailty based on an easily calculable preoperative measure is a useful marker to identify patients at increased risk for postoperative complications and is more predictive of survival than an inflammation-based prognostic score after gastrectomy. Thus, PF status should be included in the routine assessment of the oldest elderly patients with gastric cancer.


Similar content being viewed by others
References
Jemal A, Siegel R, Xu J, et al. Cancer statistics, 2010. CA Cancer J Clin. 2010;60(5):277–300.
Amrock LG, Neuman MD, Lin HM, et al. Can routine preoperative data predict adverse outcomes in the elderly? Development and validation of a simple risk model incorporating a chart-derived frailty score. J Am Coll Surg. 2014;219(4):684–94.
Robinson TN, Eiseman B, Wallace JI, et al. Redefining geriatric preoperative assessment using frailty, disability and co-morbidity. Ann Surg. 2009;250(3):449–55.
Oresanya LB, Lyons WL, Finlayson E. Preoperative assessment of the older patient: a narrative review. JAMA. 2014;311(20):2110–20.
Roxburgh CS, McMillan DC. Role of systemic inflammatory response in predicting survival in patients with primary operable cancer. Future Oncol. 2010;6(1):149–63.
Lee DY, Hong SW, Chang YG, et al. Clinical significance of preoperative inflammatory parameters in gastric cancer patients. J Gastric Cancer. 2013;13(2):111–6.
Coussens LM, Werb Z. Inflammation and cancer. Nature. 2002;420(6917):860–7.
Mantovani A, Allavena P, Sica A, et al. Cancer-related inflammation. Nature. 2008;454(7203):436–44.
Colotta F, Allavena P, Sica A, et al. Cancer related inflammation, the seventh hallmark of cancer: links to genetic instability. Carcinogenesis. 2009;30(7):1073–81.
Chiba T, Marusawa H, Ushijima T. Inflammation-associated cancer development in digestive organs: mechanisms and roles for genetic and epigenetic modulation. Gastroenterology. 2012;143(3):550–63.
Ishizuka M, Nagata H, Takagi K, et al. Inflammation-based prognostic score is a novel predictor of postoperative outcome in patients with colorectal cancer. Ann Surg. 2007;246(6):1047–51.
Zhou X, Du Y, Huang Z, Xu J, et al. Prognostic value of PLR in various cancers: a meta-analysis. PLoS One. 2014;9(6):e101119.
McMillan DC. The systemic inflammation-based Glasgow prognostic score: a decade of experience in patients with cancer. Cancer Treat Rev. 2013;39:534–40.
Edge SB, Byrd DR, Compton CC, et al. AJCC cancer staging manual, 7th edn. New York: Springer; 2009.
Japanese Gastric Cancer Association. Japanese classification of gastric carcinoma. 3rd English edition. Gastric Cancer. 2011;14(2):101–12.
Japanese Gastric Cancer Association. Japanese gastric cancer treatment guidelines 2010 (ver.3). Gastric Cancer. 2011;14(2):113–23.
GS. Cho, W. Kim, HH. Kim, et al. Multicentre study of the safety of laparoscopic subtotal gastrectomy for gastric cancer in the elderly. Br J Surg. 2009;96:1437–42.
Dindo D, Demartines N, Clavien PA. Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg. 2004;240(2):205–13.
Dasgupta M, Rolfson DB, Stolee P, et al. Frailty is associated with postoperative complications in older adults with medical problems. Arch Gerontol Geriatr. 2009;48(1):78–83.
Fried LP, Tangen CM, Walston J, et al. Frailty in older adults: evidence for a phenotype. J Gerontol A Biol Sci Med Sci. 2001;56(3):M146–56.
Rockwood K, Mitnitski A. Frailty in relation to the accumulation of deficits. J Gerontol A Biol Sci Med Sci. 2007;62(7):722–7.
Rolfson DB, Majumdar SR, Tsuyuki RT, et al. Validity and reliability of the Edmonton Frail Scale. Age Ageing. 2006;35(5):526–9.
Rockwood K, Andrew M, Mitnitski A. A comparison of two approaches to measuring frailty in elderly people. J Gerontol A Biol Sci Med Sci. 2007;62(7):738–43.
Theou O, Brothers TD, Mitnitski A, et al. Operationalization of frailty using eight commonly used scales and comparison of their ability to predict all-cause mortality. J Am Geriatr Soc. 2013;61(9):1537–51.
Hamel MB, Henderson WG, Khuri SF, et al. Surgical outcomes for patients aged 80 and older: morbidity and mortality from major noncardiac surgery. J Am Geriatr Soc. 2005;53(3):424–9.
Kristjansson SR, Nesbakken A, Jordhoy MS, et al. Comprehensive geriatric assessment can predict complications in elderly patients after elective surgery for colorectal cancer: a prospective observational cohort study. Crit Rev Oncol Hematol. 2010;76(3):208–17.
Role of frailty and nutritional status in predicting complications following total gastrectomy with D2 lymphadenectomy in patients with gastric cancer: a prospective study. 2016. [Epub ahead of print]. doi:10.1007/s00423-016-1490-4.
Jiang N, Deng JY, Ding XW, et al. Prognostic nutritional index predicts postoperative complications and long-term outcomes of gastric cancer. World J Gastroenterol. 2014;20(30):10537–44.
Vulliamy P, McCluney S, Mukherjee S, et al. Postoperative elevation of the neutrophil: lymphocyte ratio predicts complications following esophageal resection. World J Surg. 2016;40(6):1397–403.
Neuman HB, Weiss JM, Leverson G, et al. Predictors of short-term postoperative survival after elective colectomy in colon cancer patients ≥80 years of age. Ann Surg Oncol. 2013,20(50):1427–35.
Tegels JJ, de Maat MF, Hulsewe KW, et al. Value of geriatric frailty and nutritional status assessment in predicting postoperative mortality in gastric cancer surgery. J Gastrointest Surg. 2014;18(3):439–45.
Jung MR, Park YK, Jeong O, et al. Elevated preoperative neutrophil to lymphocyte ratio predicts poor survival following resection in late stage gastric cancer. J Surg Oncol. 2011;104(5):504–10.
Aizawa M, Gotohda N, Takahashi S, et al. Predictive value of baseline neutrophil/lymphocyte ratio for T4 disease in wall-penetrating gastric cancer. World J Surg. 2011;35(12):2717–22.
Jung MR, Park YK, Jeong O, et al. Elevated preoperative neutrophil to lymphocyte ratio predicts poor survival following resection in late stage gastric cancer. J Surg Oncol. 2011;104:504–10.
Ishizuka M, Kubota K, Kita J, et al. Impact of an inflammation-based prognostic system on patients undergoing surgery for hepatocellular carcinoma: a retrospective study of 398 Japanese patients. Am J Surg. 2012;203(1):101–6.
Pinato DJ, North BV, Sharma R. A novel, externally validated inflammation-based prognostic algorithm in hepatocellular carcinoma: the prognostic nutritional index (PNI). Br J Cancer. 2012;106(8):1439–45.
Smith RA, Bosonnet L, Raraty M, et al. Preoperative platelet:lymphocyte ratio is an independent significant prognostic marker in resected pancreatic ductal adenocarcinoma. Am J Surg. 2009;197(4):466–72.
Sakurai K, Ohira M, Tamura T, et al. Predictive potential of preoperative nutritional status in long-term outcome projections for patients with gastric cancer. Ann Surg Oncol. 2016;23(2):525–33.
Acknowledgement
All of the authors are grateful for the statistics related consultation provided by the Public Health School of Fujian Medical University.
Disclosure
All of the authors declare that they have no potential commercial conflicts of interest relevant to this article.
Funding
This work was supported by the National Key Clinical Specialty Discipline Construction Program of China (No. [2012] 649) and Key Projects of Science and Technology Plan of Fujian Province (No. 2014Y0025).
Author information
Authors and Affiliations
Corresponding author
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Lu, J., Cao, Ll., Zheng, Ch. et al. The Preoperative Frailty Versus Inflammation-Based Prognostic Score: Which is Better as an Objective Predictor for Gastric Cancer Patients 80 Years and Older?. Ann Surg Oncol 24, 754–762 (2017). https://doi.org/10.1245/s10434-016-5656-7
Received:
Published:
Issue Date:
DOI: https://doi.org/10.1245/s10434-016-5656-7