Abstract
Background
Rheumatic disease (RD) patients are liable for severe coronavirus disease 2019 (COVID-19). It is noticeable that RD patients’ practices have changed during the late COVID-19 pandemic. This study aimed to assess the knowledge, attitudes, practices, and compliance of RD patients during the late pandemic.
Results
This study included 188 patients with various RDs. The majority were female (61.7%) and were rheumatoid arthritis (RA) and systemic lupus erythematosus (SLE) patients (40.4% and 30.9%, respectively). We found knowledge deficiencies regarding some symptoms, contact isolation, and transmission. Negative attitudes toward COVID-19 final control were detected in a large proportion (50%). Furthermore, the majority did not think they were at risk of COVID-19 due to either RD (61.7%) or their drugs (66%). Their practices were also negative; the majority stopped wearing masks (56.4%) and went to crowded places recently (83%). Moreover, most did not stop or reduce their drugs for fear of COVID-19 but for availability issues (5.3% and 9.6% vs. 37.2%). Male gender and higher education and socioeconomic levels were significantly associated with better knowledge. In addition, RDs such as reactive arthritis, steroid use, lower steroid doses, COVID-19 vaccination, high education and socioeconomic levels, and Internet use as main knowledge sources had a significant association with better attitudes. Conventional disease-modifying anti-rheumatic drugs (DMARDs) use, biologics non-use, high education, severe functional impact, and compliance before the pandemic were significantly associated with higher practice scores. Knowledge was positively correlated with attitudes and practice (P = 0.0001 and 0.003, respectively). Moreover, attitudes were negatively correlated with age (P = 0.016). In multiple linear regression analysis, education, socioeconomic status, and practice were significant positive predictors of knowledge (P = 0.002, 0.001, and 0.046, respectively). Good knowledge, COVID-19 vaccination, younger age, and lower steroid doses were significant predictors of better attitudes (P = 0.02, 0.001, 0.02, and 0.002, respectively). Furthermore, non-use of biologics and functional disability were significant predictors of good practice (P = 0.002 and 0.015, respectively).
Conclusion
Improving knowledge and educating RD patients about the importance of protective measures is essentially needed to decrease the pandemic fatigue consequences and prevent serious COVID-19 complications in those patients.
Similar content being viewed by others
Background
Studying coronavirus disease 2019 (COVID-19) in rheumatic disease (RD) patients is of concern as immune-mediated inflammatory disease patients, especially those with inflammatory joint disease (especially rheumatoid arthritis, psoriatic arthritis, and ankylosing spondylitis), inflammatory bowel disease (especially Crohn’s disease, ulcerative colitis, and unclassified inflammatory bowel disease), and inflammatory skin disease (especially psoriasis and hidradenitis suppurativa), had a greater risk of COVID-19-related death compared with the general population (HR 127, 95% CI 123–131) [1].
Autoimmune disorders can weaken patients’ immunity [2]. In addition, certain conventional synthetic disease-modifying anti-rheumatic drugs (csDMARDs), biologics, Janus kinase (JAK) inhibitors, and glucocorticoids can increase the infections risk [3]. However, some biologics are being used as COVID-19 treatments, including anti-interleukin-6 inhibitors that have been used in COVID-19 cytokine storm syndrome [4].
There was evidence of tremendous anxiety, depression, and panic during COVID-19’s beginning compared to other epidemics, such as severe acute respiratory syndrome (SARS) [5]. RD patients also developed increased fears and worries during the early pandemic because of their diseases and medications. Such worry affected their practices as well as medication compliance [6, 7].
There is evidence of a greater risk of COVID-19 and bad outcomes in RD patients, such as hospitalization rate, intensive care unit admission rate, mechanical ventilation rate, and case fatality [8]. Furthermore, RD patients have a higher prevalence and severity of post-COVID-19 syndrome symptoms than control subjects [9]. Although there are previous studies that studied the knowledge, attitudes, and practice of RD patients in the early pandemic [6, 10, 11], a change in attitudes and practices was noticed during the late pandemic. Assessment of RD patients’ knowledge, attitudes, practices, and compliance is essential throughout the pandemic to examine their adherence to medications and protective measures against COVID-19 and improve it. Hence, this study aimed to assess the knowledge, attitudes, practices, and compliance of RD patients during the late pandemic and the association of the demographic and disease data with total knowledge, attitudes, and practice scores.
Methods
Patients and study design
This study was carried out as a cross-sectional analytical study between February 2022 and July 2022.
Study population
We recruited 188 adult literate patients with various RDs, aged 18–70 years, from the Physical Medicine, Rheumatology, and Rehabilitation Clinic. The participants fulfilled the criteria of their RD as rheumatoid arthritis (RA) [12], systemic lupus erythematosus (SLE) [13], psoriatic arthritis [14], Behçet’s disease [15], ankylosing spondylitis (AS) [16], reactive arthritis [17], and systemic sclerosis [18]. Those with mental or severe psychiatric problems were excluded. The sample size was calculated with a margin of error of 5% and a 95% confidence level.
Data collection tool
We used the survey questionnaire designed by Vaidya et al. that was originally produced by Zhong et al. to assess the knowledge, attitudes, and practices of the Chinese population during the early pandemic [19] and modified by Vaidya et al. to be used in RD patients (internal consistency between each questionnaire item was satisfactory, with Cronbach’s α = 0.769) [10]. We obtained the corresponding author’s permission and translated it into Arabic by two independent English language professionals. The Arabic versions were back-translated to English by two independent English speakers blind to the original English version. After sorting the discrepancies between the original and back-translated questionnaires, a prefinal Arabic questionnaire was developed. It was tested in five RD patients and finalized based on their comments. The final Arabic version was produced and tested in a pilot study of 15 patients to ensure it was completely comprehensible.
The survey questionnaire includes thirteen questions concerning COVID-19 knowledge, six assessing attitudes toward COVID-19, and six about practices. The questions have categorized responses as true, false, or not sure.
The Ethical Committee Board of the Faculty of Medicine approved the study protocol (the reference number was 4797/1-3-2022). The study was performed in accordance with the relevant principles of the Declaration of Helsinki (2000 revision). We obtained informed written consent from all participants after explaining the research purpose.
All participants provided a complete history, including demographic data, the main knowledge source, compliance before the pandemic, previous COVID-19 infection and vaccination, and their disease data, including disease type, duration, steroid use and dosage, and DMARDs.
In addition to the previous data, participants filled out the following questionnaires:
-
1.
The updated socioeconomic scale by El-Gilany and El-Wehady
The socioeconomic status scale, constructed by Fahmy and El Sherbini [20], was extended and updated by El-Gilany and El-Wehady [21] to include seven domains: education and culture, economics, family possessions, home sanitation, and health care. This socioeconomic status was classified as high, middle, low, or very low.
-
2.
The Health Assessment Questionnaire-Disability Index (HAQ-DI)
We used the Arabic-validated HAQ-DI as a measure of the functional impact of the RD [22]. HAQ-DI is a self-reported questionnaire covering 20 items in eight domains: difficulty in performing daily activities like arising, eating, walking, dressing, hygiene, reaching, gri**, and ordinary daily activities. Scores of 0–1 were considered mild, 1–2 were moderate, and 2–3 were severe [23].
-
3.
The Arabic version of the translated survey questionnaire
We calculated a total knowledge score, where the correct answer was assigned 1 point and an incorrect or unsure answer was assigned 0 points. The total scores for attitude and practice were computed by assigning one to positive attitude or practice and zero to negative attitude or practice.
Statistical analysis
All the data were coded and imported into the Statistical Package for the Social Sciences (SPSS version 25) software. All variables were expressed as means, standard deviations, and percentages. Kruskal–Wallis tests, Spearman correlation coefficients, and multiple linear regression analysis were used to identify significant associations, correlations, and predictors. The results were considered significant if P was ≤ 0.05.
Results
The majority of study participants were RA patients (40.4%) and females (F:M was 1.61:1). The clinical and demographic data are shown in Table 1.
Most of the studied patients have moderate to fair knowledge about COVID-19, where most know the symptoms (100%), the methods of transmission (85.1%), the treatments (83%), and the risky groups (60.6%). However, some did not know that sneezing and runny nose are common symptoms (17%), and the majority responded incorrectly to the questions of contact person isolation and transmission of the virus in the absence of fever (Table 2).
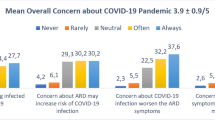
We detected some negative attitudes among the study participants, where a large proportion (44.7%) were uncertain whether COVID-19 would be finally controlled. The majority thought that they were not at high risk of COVID-19 infection due to RD or medications (61.7% and 66%, respectively). Regarding their practices and compliance, a large proportion did not wear masks when going outdoors (56.4%), and the most admitted to going to crowded places last week (83%). The majority did not stop their medications for fear of COVID-19 (93.6%) but for availability issues (37.2%) (Table 3).
The association of total knowledge, attitudes, and practice scores with all study variables is described in Table 4. Male gender, high education, and high socioeconomic levels were associated with higher total knowledge scores (P = 0.02, 0.0001, and 0.0001, respectively). In addition, diseases such as reactive arthritis and psoriatic arthritis, steroid use, the lower dose of steroids, vaccination, higher education and socioeconomic levels, and the Internet as main knowledge sources were associated with positive attitudes (P = 0.002, 0.001, 0.022, 0.0001, 0.016, 0.014, and 0.03, respectively). Regarding practice, conventional DMARD use, biologics non-use, high education, severe functional impact, and compliance before the pandemic were associated with more positive practices (P = 0.038, 0.002, 0.026, 0.002, and 0.014, respectively) (Table 4).
The total practice score significantly correlates positively with disease duration (P = 0.037). Age has a significant negative correlation with attitudes; older patients had more negative attitudes (P = 0.016). In addition, knowledge had a significant positive correlation with attitudes and practices (P = 0.0001 and 0.003, respectively) (Table 4).
We designed three multiple linear regression models to identify predictors of knowledge, attitudes, and practices. Education, socioeconomic status, and practice were significant positive predictors of knowledge (Table 5). Moreover, good knowledge, COVID-19 vaccination, younger age, and lower steroid doses were detected as significant predictors of positive attitudes (Table 6). In addition, the biologics’ non-use and severe functional impact of RD were significant predictors of good practice (Table 7).
Discussion
Studying the knowledge, attitudes, and practices of RD patients can influence COVID-19 outcomes in such high-risk patients. In the present study, acceptable knowledge was detected. However, we found some knowledge deficiencies in some aspects. Good knowledge was expected because the pandemic has been ongoing for 2 years and all data on transmission methods, prognosis, and risk groups are available to everyone via various media sources.
In comparison to the early pandemic, Vaidya et al. reported awareness of the clinical features, route of transmission, and methods of prevention of COVID-19 in most of their participants (> 90%), and 70.6% of them knew that patients with comorbidities were liable to bad outcomes [10].
Fernández-Ávila et al. also studied knowledge, attitude, practice, and compliance in Latin American patients with RDs after 1 year of the pandemic’s start. About 43.7% of the studied patients demonstrated an adequate level of understanding about modes of transmission, lethality, and current treatments [6].
Regarding attitudes, only 50% of our participants thought that COVID-19 would finally be controlled, compared to 71.5% in Vaidya et al.’s study during the early pandemic. Moreover, the COVID-19 worry has decreased. Only 7.4% of our participants thought that they had a greater chance of getting COVID-19 than the general population because of their comorbidity in comparison to 31.5% in the Vaidya et al. study, and 3.3% believed that the anti-rheumatic medications increased their susceptibility to infection compared to 18.9% in the Vaidya et al. study [10].
Negative practices toward COVID-19 protective measures were also detected in most of the participants in our study. There were great differences from what was reported during the early pandemic: Vaidya et al. reported the practice of preventive measures among the majority of participants, like wearing a mask (94.7%) and avoiding public or crowded places (97.9%) [10].
Another study conducted during the early pandemic reported increased worry among RD patients in a large proportion of the studied population, and most were following COVID-19 protective measures such as wearing masks, performing hand sanitation, and avoiding going out [6].
Hammad et al. detected significant differences between the RD patients and the control group regarding the attitudes and behaviors of washing hands, going outdoors, wearing masks, and staying in their rooms during the early pandemic. RD patients showed more anxiety, irritability, and depression in response to the pandemic than the control group [11].
Fernández-Vila et al. reported that the risk of becoming infected with COVID-19 was perceived as high by 24.6% of patients or both for themselves and their relatives (19.9%). Concerning practices, such as avoiding public gatherings, wearing face masks, and frequent hand washing, they were adequate in most of them (77.8%) [6].
This shift in attitudes and practice in our study can be explained by the lower severity of COVID-19 infection during the late pandemic compared to the first waves due to lower virulence strains. The availability of vaccinations may also be a contributing factor to the negative practices.
In terms of the compliance, 9.6% of our participants reduced the dose of their DMARD independently for fear of COVID-19 compared to 13.6% in Vaidya et al. study during the early pandemic [10]. Pineda-Sic et al. reported that 85% of patients had not changed their medication schemes and that changes were mainly due to lack of availability (48.1%), followed by fear of contracting COVID-19 (25%) [24].
Fernández-Ávila et al. found that one anti-rheumatic medication was suspended by 23.4% of their sample: 29.3% suspended antimalarials and 18.2% discontinued methotrexate. About 27.7% of them stated that the decision was based on the fear of COVID-19 infection. Other patients claimed that it was due to financial constraints or the uncovering of the drug by the health insurance [7].
So, the awareness of RD patients about the importance of continuing their drugs and the hazards of stop** them seems to have improved in the late pandemic. The increased anxiety and a lack of adequate immunosuppressive recommendations can explain compliance during the early pandemic. Also, the lockdown in the early stages of the pandemic could be a cause.
Regarding the significant associations in knowledge and attitudes with high educational levels in the present study, this holds some logic since these people can easily know, via multiple sources, the updates, and their attitudes can be more positive.
Hassen et al. also studied RD patients’ experiences during the early pandemic and its implications on their health perception and behavior. It was found that patients’ knowledge about COVID-19 was correlated with social media use (P = 0.012), fear of COVID-19 infection (P = 0.024), and fear of disease deterioration with the infection (P = 0.035) [25].
In the present study, Internet users had more positive attitudes than those who reported other main sources of knowledge. The applicability and higher published data on the Internet about COVID-19 updates and prognosis can significantly impact the attitudes. The disease activity affecting steroid dose and use significantly associated with the attitudes. Those on steroids might be controlled, so their attitude could be more positive, and those on higher doses of steroids mostly had severe diseases that negatively affected their attitude. Regarding the negative correlation of age with attitudes, it can be attributed to increased worry concerning age or other chronic illnesses in the elderly.
Hassen et al. reported in their study that patients’ perceptions of worsened disease activity were correlated with unplanned healthcare visits (P < 0.001), medication non-adherence (P = 0.01), and difficulty accessing medication (P = 0.006) [25].
Regarding the negative association of practice with biological DMARDS use, it is previously known that biologics can increase the infection risk overall, but these results can be attributed to the fact that some biologics were used in COVID-19 treatment with great success. This might have affected their practice during the pandemic. Concerning the significant association of the RD functional impact with practice, those with severe functional impairment mostly improve their practice to prevent disease flares and more disability.
Compared to our results, Vaidya et al. found no significant relationships between demographic variables like sex, education, or use of immunosuppressants and responses to knowledge-, attitude-, and practice-related questions [10].
Despite the higher rate of infections and the higher number of infected individuals in the late pandemic, RD patients had a significant shift in attitude and practices. These changes in attitude and practices can be attributed to the term “pandemic fatigue” or “burnout.” Pandemic fatigue can be caused by the pandemic’s long duration, the availability of vaccinations, and the lower severity of infections than at the start of the pandemic due to lower virulence coronavirus strains.
Pandemic fatigue also happened in the general populations [26], not only in RD patients. The reopening of the economy may have also contributed partially to the poor practices owing to workplace hazards such as poor ventilation and crowding [27]. Moreover, the COVID-19 worry has decreased and affected adherence to protective measures and practices [26].
The significant positive correlation of knowledge with attitudes and practices implies the importance of improving awareness about COVID-19 and health education about the importance of COVID-19 protective measures throughout the pandemic.
This study has points of strength; it studied knowledge, attitude, and practice during the late pandemic in RD patients. Moreover, it refers to pandemic fatigue in such a high-risk group of patients. The limitation of this study is that it was a cross-sectional study, which does not allow the study of causal relationships. Another limitation is that it was uni-governmental.
Conclusions
Some deficiencies in knowledge were detected in RD. Concerns about COVID-19 have significantly decreased compared to the early pandemic. These attitudes affected their practices; their practices were wrong and unhealthy as they stopped wearing masks and avoiding crowded places. Most of them were compliant with their medications. So, improving the knowledge and health education of RD patients about the importance of strict COVID-19 measures is essential since they are prone to serious complications and COVID-19 is still going on and not over.
Availability of data and materials
The datasets analyzed during the current study are available with the corresponding author upon request.
Abbreviations
- COVID-19:
-
Coronavirus disease 2019
- RD:
-
Rheumatic disease
- CsDMARDs:
-
Conventional synthetic disease-modifying anti-rheumatic drugs
- JAK:
-
Janus kinase
- SARS:
-
Severe acute respiratory syndrome
- RA:
-
Rheumatoid arthritis
- SLE:
-
Systemic lupus erythematosus
- AS:
-
Ankylosing spondylitis
- HAQ-DI:
-
Health Assessment Questionnaire-Disability Index
- SPSS:
-
Statistical Package for the Social Sciences
References
MacKenna B, Kennedy NA, Mehrkar A, Rowan A, Galloway J, Matthewman J et al (2022) Risk of severe COVID-19 outcomes associated with immune-mediated inflammatory diseases and immune-modifying therapies: a nationwide cohort study in the OpenSAFELY platform. Lancet Rheumatol 4(7):e490–e506
Wiseman AC (2016) Immunosuppressive medications. Clin J Am Soc Nephrol 11(2):332–343
Au K, Reed G, Curtis JR, Kremer JM, Greenberg JD, Strand V et al (2011) High disease activity is associated with an increased risk of infection in patients with rheumatoid arthritis. Ann Rheum Dis 70(5):785–791
Mehta P, McAuley DF, Brown M, Sanchez E, Tattersall RS, Manson JJ (2020) COVID-19: consider cytokine storm syndromes and immunosuppression. Lancet (London, England) 395(10229):1033–4
Wu KK, Chan SK, Ma TM (2005) Posttraumatic stress, anxiety, and depression in survivors of severe acute respiratory syndrome (SARS). J Trauma Stress 18(1):39–42
Ma MH, Tay SH, Cheung PP, Santosa A, Chan YH, Yip JW et al (2021) Attitudes and behaviors of patients with rheumatic diseases during the early stages of the COVID-19 outbreak. J Rheumatol 48(1):35–39
Fernández-Ávila DG, Barahona-Correa J, Romero-Alvernia D, Kowalski S, Sapag A, Cachafeiro-Vilar A et al (2022) Impact of COVID-19 pandemic on patients with rheumatic diseases in Latin America. Rheumatol Int 42(1):41–49
Wang F, Ma Y, Xu S, Liu H, Chen Y, Yang H et al (2022) Prevalence and risk of COVID-19 in patients with rheumatic diseases: a systematic review and meta-analysis. Clin Rheumatol 41(7):2213–23
Ismail ZNE, Hefny MA, Hendi AE, Tawfik MG (2023) Assessment of symptoms of the post-COVID-19 syndrome in patients with different rheumatic diseases. Egypt Rheumatol Rehabil 50(1):24
Vaidya B, Bhochhibhoya M, Baral R, Nakarmi S (2020) Knowledge, attitudes, and practice regarding COVID-19 among patients with musculoskeletal and rheumatic diseases in Nepal: a web-based cross-sectional study. Open Access Rheumatol: Res Rev 12:167
Hammad MA, Eissa M, Dawa GA (2020) Impact of coronavirus disease 2019 (COVID-19) pandemic on attitude, behavior, and mental health of patients with rheumatic diseases. Egypt Rheumatol Rehabil 47(1):1–13
Aletaha D, Neogi T, Silman AJ, Funovits J, Felson DT, Bingham CO III et al (2010) 2010 rheumatoid arthritis classification criteria: an American College of Rheumatology/European League Against Rheumatism collaborative initiative. Arthritis Rheum 62(9):2569–2581
Aringer M, Costenbader K, Daikh D, Brinks R, Mosca M, Ramsey-Goldman R et al (2019) 2019 European League Against Rheumatism/American College of Rheumatology classification criteria for systemic lupus erythematosus. Arthritis Rheumatol 71(9):1400–1412
Tillett W, Costa L, Jadon D, Wallis D, Cavill C, McHUGH J et al (2012) The ClASsification for Psoriatic ARthritis (CASPAR) criteria–a retrospective feasibility, sensitivity, and specificity study. J Rheumatol 39(1):154–156
ITR-ICBD, (2014) The International Criteria for Behçet’s Disease (ICBD): a collaborative study of 27 countries on the sensitivity and specificity of the new criteria. J Eur Acad Dermatol Venereol 28(3):338–347
Rudwaleit M, Van Der Heijde D, Landewé R, Listing J, Akkoc N, Brandt J et al (2009) The development of Assessment of SpondyloArthritis international Society classification criteria for axial spondyloarthritis (part II): validation and final selection. Ann Rheum Dis 68(6):777–783
Selmi C, Gershwin ME (2014) Diagnosis and classification of reactive arthritis. Autoimmun Rev 13(4–5):546–549
Van Den Hoogen F, Khanna D, Fransen J, Johnson SR, Baron M, Tyndall A et al (2013) 2013 classification criteria for systemic sclerosis: an American College of Rheumatology/European League against Rheumatism collaborative initiative. Arthritis Rheum 65(11):2737–2747
Zhong B-L, Luo W, Li H-M, Zhang Q-Q, Liu X-G, Li W-T et al (2020) Knowledge, attitudes, and practices towards COVID-19 among Chinese residents during the rapid rise period of the COVID-19 outbreak: a quick online cross-sectional survey. Int J Biol Sci 16(10):1745
Fahmy S (1983) Determining simple parameters for social classifications for health research. Bull High Inst Public Health 13:95–108
El-Gilany A, El-Wehady A, El-Wasify M (2012) Updating and validation of the socioeconomic status scale for health research in Egypt. East Mediterr Health J 18(9):962–8
El Meidany YM, El Gaafary MM, Ahmed I (2003) Cross-cultural adaptation and validation of an Arabic Health Assessment Questionnaire for use in rheumatoid arthritis patients. Joint Bone Spine 70(3):195–202
Bruce B, Fries JF (2003) The Stanford health assessment questionnaire: dimensions and practical applications. Health Qual Life Outcomes 1(1):1–6
Pineda-Sic RA, Galarza-Delgado DA, Serna-Peña G, Castillo-Torres SA, Flores-Alvarado DE, Esquivel-Valerio JA et al (2021) Treatment adherence behaviours in rheumatic diseases during COVID-19 pandemic: a Latin American experience. Ann Rheum Dis 80(6):e85
Hassen LM, Almaghlouth IA, Hassen IM, Daghestani MH, Almohisen AA, Alqurtas EM et al (2020) Impact of COVID-19 outbreak on rheumatic patients’ perceptions and behaviors: a cross-sectional study. Int J Rheum Dis 23(11):1541–1549
Chai C-S, Chua W-J, Tung Y-Z, Sindeh W, Ibrahim MA, Sham SFB et al (2022) Knowledge, attitude, and practices among the general population during the later stage of the COVID-19 pandemic in Malaysia: a cross-sectional study. Risk Manag Healthc Policy 15:389
Rahman A, Jasmin A, Schmillen A (2020) The vulnerability of jobs to COVID-19: the case of Malaysia. Economics working paper
Acknowledgements
We kindly acknowledge all the study participants for their trust, time, and patience.
Funding
No author has any financial interest or has received any financial benefit from this research.
Author information
Authors and Affiliations
Contributions
All authors are significantly involved in the preparation of the manuscript. MS and ON generated the idea; ZN drafted the manuscript and performed the study statistics. ME and MS revised it critically. All authors took part in interpreting the results and approved the final version.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The study protocol was approved by the Ethical Committee Board of the Faculty of Medicine, Suez Canal University. The reference number was 4797/1-3-2022. Methods were performed following the principles of the Declaration of Helsinki (2000 revision). Written informed consent was obtained from all participants after explaining the study.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Ismail, Z.N.E., Ibrahim, O.N., Ghaly, M.S. et al. Knowledge, attitudes, practices, and compliance of rheumatic disease patients toward COVID-19 during the late pandemic. Egypt Rheumatol Rehabil 50, 36 (2023). https://doi.org/10.1186/s43166-023-00205-w
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s43166-023-00205-w