Abstract
Background
Otosclerosis is one of the most common causes of hearing loss in adults with clinical onset between 20 and 40 years of age. Vestibular symptoms may be the most agonizing and primary symptom in cases with otosclerosis, so the assessment of patients is important. The vestibular-evoked myogenic potentials test (VEMP) is used to assess the saccular and the utricular functions using cervical and ocular vestibular-evoked myogenic potentials (cVEMP and oVEMP), respectively. The video head impulse test (vHIT) which measure vestibulo-ocular reflex (VOR) to rapid impulsive head acceleration in the plane of each semicircular canal (SCC) has allowed quantitative monitoring of each canal function.
Methods
Twenty subjects with bilateral otosclerosis were studied, ranging in age from 30 to 55 years, divided into two groups. One group consisted of 10 adult patients with bilateral conductive otosclerosis. The second group consisted of 10 adult patients with bilateral mixed otosclerosis. All the patients underwent cVEMP and oVEMP, using a BC 500Hz tone burst stimulus and vHIT in three planes, left anterior right posterior (LARP), right anterior left posterior (RALP), and lateral SCCs.
Results
The findings indicate statistically significant differences in the peak-to-peak amplitudes of cVEMP and oVEMP in the two studied groups, and the mixed cases had lower amplitudes than conductive cases and a significant increase in p13 latencies. Also, there is a statistically significant difference in the lateral SCC gain between the two groups, as mixed cases had lower gain than conductive cases, but not for anterior or posterior SCCs, with no gain less than 0.8 in all three canals.
Conclusion
The findings suggested that the saccule is more liable to be affected by cochlear otosclerosis followed by the utricle. The three SCCs are mostly spared.
Similar content being viewed by others
Background
Otosclerosis refers to the presence of a localized hereditary disorder that affects the bone metabolism of otic capsule enchondral bone resulting in progressive hearing loss [1]. Otosclerosis can be determined histologically by the presence of occasional histopathological lesions in temporal bone autopsies that do not involve the stapes, stapedio-vestibular joint, or cochlear endosteum, and hence, there are no symptoms during life [2]. When otosclerosis fixes the stape footplate, stapediovestibular joint, or round window membrane, it causes conductive hearing loss and is defined as clinical otosclerosis [3]. Cochlear otosclerosis refers to lesions involving the cochlear endosteum causing sensorineural hearing loss with or without stapes fixation. It usually fixes the stapes; thus, cochlear otosclerosis is classified as a mixed type or a sensorineural type depending on the clinical appearance [4].
Hearing loss often begins between the ages of 15 and 45 years. Female-to-male ratio is 2:1. Otosclerosis has been reported to advance more rapidly in females than males. Hormonal factors may play a role; some females with otosclerosis appear to have their condition worsen during pregnancy [5].
The area anterior to the oval window is affected in 80% of histologic otosclerosis and in 50% of cases. Fossula ante-fenestrum is usually involved within the lesion, but is not necessarily the site of origin of the lesion. Other sites might be involved such as the round window niche (30%), cochlea (21%), and internal auditory canal (19%) [6]. Less frequent sites include foci posterior to the oval window, the semicircular canals, the entire footplate, and the involvement of the middle ear ossicles [7].
In the cochlear type of otosclerosis, the otosclerotic focus might extend till reaching the cochlear endosteum leading to deposition of hyalin inside the spiral ligament [8]. Deposition of abnormal otosclerotic bone in the cochlea might happen, it often happens close to the round window within the 1st half of the basal turn [9]. These events are suggested to account for dysfunctions of the hair cells of the cochlea as they cause disruption of homeostasis of ions [10].
Vestibular symptoms associated with otosclerosis occur in 10–45% of patients. The otosclerotic affection of the vestibular organs is suggested to cause such vestibular symptoms [11]. The mechanisms of the vestibular symptoms have been explained as (1) detachment of the otoconia (mostly from the utricle invading the endolymph of the posterior semicircular canal), (2) degeneration of Scarpa’s ganglion and affection of superior SCC, and (3) dizziness might be because of the alterations in the biochemical structure of perilymph [12, 13]. (4) It may also be caused by comorbid pathology, such as Ménière’s disease. Otosclerotic foci may rarely involve the vestibular aqueduct [14].
The cVEMP is an ipsilateral inhibitory surface potential from the sternocleidomastoid (SCM) muscles generated in the saccule [15]. The oVEMP is a contralateral excitatory potential from the extraocular muscles beginning in the utricle [16]. The video head impulse test (vHIT) is a more physiologic test of the SCCs for assessing the high-frequency angular VOR and has been introduced to accurately quantify and follow up the VOR gain [17].
The aim of this study is to assess the function of the saccule, the utricle, and the three semicircular canals using cVEMP, oVEMP, and video HIT in patients with cochlear otosclerosis.
Methods
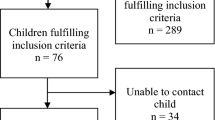
The study was carried out on 20 adult subjects in the Audio Vestibular Medicine Unit, Department of Otorhinolaryngology, Alexandria Main University Hospital. They were divided into two groups: the first group contains ten adult patients with bilateral conductive otosclerosis. The second group contains ten adult patients with bilateral mixed otosclerosis. All the patients were more than 18 years old, with normal otoscopy, type A or As tympanogram, absent acoustic reflex, and had either conductive or mixed hearing loss. No history of trauma or chronic discharge or neck stiffness and no sex limit. Informed consent was provided for all participants of both groups. Pure tone audiometry (PTA) was done using the commercial system Interacoustics AD629 Diagnostic Audiometer (Interacoustics, Denmark) for the frequency range of 0.250 to 8 kHz for air conduction testing (AC). The air conduction pure tone (AC.PTA) average was calculated at frequencies 0.5, 1.0, and 2.0 kHz. This was followed by bone conduction (BC) testing at audiometric frequencies 0.25, 0.5, 1.0, 2.0, and 4.0Hz and BC PTA average at the same frequencies to avoid Carhart notch. The mean air-bone gab (ABG) was measured as the average of differences between AC and BC hearing thresholds at the frequencies 0.25, 0.5, 1.0, 2.0, and 4.0Hz. The tympanometry and acoustic reflex thresholds using a 226 Hz probe tone were done with Clarinet Clinical Middle Ear Analyzer (Inventis, Italy). Tympanometry was performed by varying pressure ranging from + 200 to − 400 mmH2O. Ipsilateral and contralateral acoustic reflex thresholds elicited with pure tones at frequencies of 0.5, 1, 2, and 4 kHz.
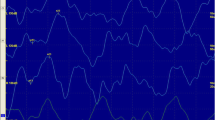
Vestibular function was evaluated using cVEMP, oVEMP, and vHIT. Cervical and ocular VEMPs were done using the commercial system Eclipse A/S Audiometer Allé (Interacoustics, Denmark). Using 500Hz tone burst stimulus via bone vibrator B71, stimuli were Blackman gated (2:2:2), with rate 5.1/s and intensity 40 dBnHL, band pass filter between 10 and 750Hz and electrode impedance less than 5kohms, with interelectrode impedance less than 3kOhm. A recording epoch of 100ms with a 10-ms prestimulus recording period and a 90-ms post-stimulus recording period was used. Approximately 150 sweeps per waveform were collected for each run. The EMG-controlled stimulus was 50 to 150µV RMS.
For cVEMP, the SCM muscle ipsilateral to tested ear was selected where the reference electrode was located on its upper third, the active electrode was placed on the sterno-clavicular junction, and the ground electrode was positioned on the forehead [18]. The patient was seated and instructed to turn his head to the right or left to activate the muscle on the test side. The patient monitor was used to guide the patient during testing to obtain optimum contraction. At least 2 runs were performed [18]. The initial positive–negative biphasic response comparing P13 and n23 was traced. The mean peak latencies of p13 and n23 waves were measured. The P13-n23 amplitude was calculated. The absence of the biphasic responses and the replicability of the wave was defined as an absence of VEMP.
The stimulus and recording parameters of oVEMP were similar to cVEMP. The contralateral eye to the tested ear was selected for recoding the oVEMP. The reference electrode was located just inferior to the center of the lower eyelid margin. The active electrode was placed on the chin. The ground electrode was located on the forehead [18]. The patient was seated and instructed to look up about 30° and hold his gaze without moving his head. It is believed that the effect of upward gaze accomplishes two things that collectively increase the amplitude of the oVEMP over the amplitude when the eyes are staring at the center gaze: (1) upward gaze moves the contralateral inferior oblique muscle closer to the active electrode and (2) it increases the tonic EMG activity in the contralateral IO muscle that is then either attenuated or augmented by the driving acoustical stimulus [19, 20]. The initial negative–positive biphasic waveform comprising n1 and p1 peaks on the contralateral side of stimulation was traced. The latencies of n1 and p1 peaks, and n1-p1 peak-to-peak amplitude were measured.
The vHIT was done using the ICS impulse system (GN Otometrics) in lateral semicircular canals, right anterior left posterior (RALP), and left anterior right posterior (LARP) planes. The person was seated 1 m from the targeted mark wearing a pair of lightweight, tightly fitting goggles on which mounted a very light, very fast, and very small, USB video camera and a mirror that reflects the image of the patient’s right eye into the camera [21]. The patient was instructed to fixate on the target in a central position because from that central position, the direction of the head impulse is unpredictable. The operator thrust the head passively into a 15–20 degree angle. The patient is given passive small, unexpected, and abrupt head rotations in the direction of each canal plane [22]. The gain was calculated.
All data were collected and entered into the computer and analyzed using IBM SPSS software package version 20.0. (Armonk, NY: IBM Corp). Data were entered as numerical or categorical. Qualitative data were described using numbers and percentages. Quantitative data were described using range (minimum and maximum), mean, and standard deviation. The significance of the obtained results was judged at the 5% level.
Results
The current study tested 20 subjects with bilateral otosclerosis, divided into two groups. One group with 10 adult subjects with bilateral conductive otosclerosis included (40%) males and (60%) females with an age range between 30 and 50 years (38.0 ± 7.14 years). The other group consisted of 10 subjects with bilateral mixed otosclerosis (30%) males and more females (70%). The age range was between 33 and 50 years (40.20 ± 5.73 years). No statistically significant difference between both groups was found ensuring good matching of both groups regarding age and gender. Considering the PTA results, the mean values of the 3-tone AC.PTA in conductive and mixed groups were 45.06 ± 9.44 and 62.50 ± 9.46, respectively, with a significant difference (p value < 0.001). Also the mean values of the 5-tone BC.PTA were 17.50 ± 3.47 for the conductive group and (35.55 ± 4.45) for mixed otosclerotic patients showing a significant difference (p value < 0.001). Calculated 5 frequencies ABG mean was (28.90 ± 6.75) in the CHL group and (28.85 ± 8.50) in the other group without any significant difference. Three patients (30%) presented with tinnitus in the mixed group and 2 patients (20%) in the conductive group, 4 patients (40%) presented with vertigo in the mixed group, and 1 patient (10%) in conductive cases and dizziness (10%) in the 2 groups with no significant difference.
Cervical VEMP was successfully recorded in 10 out of 20 ears (50%) in the conductive group and in 7 out of 20 ears (35%) in the mixed group with no significant difference. The findings of cVEMP in ears with responses showed significantly lower peak-to-peak amplitudes in the mixed otosclerotic group than in the conductive group, a significant increase of p13 latencies, and no difference in n23 latencies (Table 1).
Ocular VEMP was successfully recorded in 8 out of 20 ears (40%) in the conductive group and in 6 out of 20 ears (30%) in a mixed group, with significantly lower peak-to-peak amplitudes in the mixed group than conductive group and no significant differences in latencies of N1 and P1 (Table 2).
The measured vHIT mean gain of the lateral SCC in the conductive group was 1.01 ± 0.10 and 0.90 ± 0.08 in the mixed group showing a statistically significant difference. The mean gain of the anterior SCC in the conductive group was 0.90 ± 0.06 and 0.87 ± 0.03 in the mixed group. Finally, the mean gains of the posterior SCC were 0.89 ± 0.04 and 0.87 ± 0.03 in the conductive and mixed groups, respectively. Insignificant mean differences were found between the two groups in the anterior and posterior canals (Table 3).
Relationship and correlation analysis
The incidences of cVEMP and oVEMP showed significant associations with the mean of the 3 tones AC.PTA and the mean of the 5 tones BC.PTA but no significant difference with the mean of the 5 tones ABG (Tables 4 and 5).
The results of the current study showed significant correlations between the AC.PTA and BC.PTA with cVEMP parameters (p13 latency and peak-to-peak amplitude) in mixed group only. No correlations were reported in the conductive group or in all parameters of oVEMPs. Also, no correlation was found between ABG and cVEMPs or oVEMPs results (Tables 6 and 7).
Finally, we did not report any correlation between the AC, BC.PTA, and ABG and the means of each SCC (Table 8).
Discussion
Vestibular symptoms are relatively common in patients affected with otosclerosis. According to cVEMP, it was successfully recorded (50%) in the conductive group and (35%) in the mixed group with no significant difference. Trivelli et al. reported (38.1%) present responses using BC cVEMP in the otosclerotic ears of their patients before stapedectomy surgery [23]. And Tramontal et al. percentage was (44.03%) with no significant difference [24]. The variable of incidences of cVEMP responses in cases suffering otosclerosis might be explained by the variability in the severity of the disease as well as the parameters used. We used a stimulus with an intensity of 40 dB and bone vibrator B71, while other studies used stimuli with higher intensities and different bone vibrators as a minishaker. Another explanation for decreased cVEMP incidence in the conductive group might be that the otosclerotic foci produce toxic metabolites that result in subclinical absence of the response in cases suffering CHL prior to the development of mixed hearing loss.
The current study findings showed that the cVEMP was either absent or had significantly lower peak-to-peak amplitudes in the mixed otosclerotic group than in the conductive group using 500 HZ BC cVEMP. Amali et al. reported lower peak-to-peak amplitudes in 8 ears with otosclerosis (16.32%) compared to normal individuals using the same stimulus and explained the cause as the direct biotoxic effect on saccular receptors, released from the otosclerosis foci may be responsible for such findings with loss of vestibular hair cells and dark cells in several years with severe otosclerosis [12].
Lin et al. found normal peak-to-peak amplitudes (102 ± 38 μV) in 18 ears and absent in 19 ears in patients with otosclerosis and vertigo, but in the group without vertigo, the cVEMP response consists of 15 ears with normal p13-n23 amplitudes (104 ± 43 μV), 17 ears with the absent response, and 1 ear with reduced amplitude using minishaker 4810 vibrator [13].
In the current study, a statistically significant increase in latency of the p13 was found in the affected ears with mixed otosclerosis compared to the affected ears with conductive ears. In studies done by Tramontal et al. and Amali et al., they reported a significant increase in p13 latency in the otosclerotic group compared to the control group [12, 24].
On the other hand, differences in n23 latency did not reach a statistically significant level between the two groups in the current study. Amali, et al. reported the same result between control and patient groups [12] while a significant statistical difference was noted in another study which had normal and otosclerotic ears [24].
For oVEMP, it was successfully recorded in (40%) in the conductive group and (30%) in the mixed group with no significant difference. Lin et al. reported normal oVEMP response (16%) in the otosclerotic group with vertigo and (48%) in the nonvertiginous otosclerotic group that explained as the utricular deficits are involved in triggering the vertiginous attacks [13].
A higher incidence rate was observed in a study by Winters et al., using a minishaker 4810 vibrator with 500 HZ stimulus. It was 90.4% in healthy subjects and 78.3% in otosclerosis patients with no significant difference [11]. The difference in incidences was explained by Rosengren et al. as the B-71 bone vibrator located on the mastoid producing good cVEMPs but poorer oVEMPs, also this bone vibrator is difficult to attach firmly to the forehead, but a stronger electromechanical conductor, like a minishaker, evokes good reflexes from either site [25, 26].
The amplitude of oVEMP was significantly lower peak-to-peak amplitudes in the mixed group than the conductive group. Lin et al. found a normal peak-to-peak amplitude (8.4 ± 2.5 μV) in 6 ears and an abnormal response was 84% consisting of 25 ears with absent oVEMP, 5 ears with reduced oVEMP and 1 ear with augmented oVEMP in otosclerotic patients with vertigo. In the nonvertiginous otosclerotic patients, the normal peak-to-peak amplitude (8.8 ± 3.2 μV) was observed in 16 ears and the abnormal response was 51% in the form of 11 ears with absent responses, 5 ears with reduced responses, and only 1 ear with augmented response [13]. Winters et al. reported no significant difference in amplitudes between normal and otosclerotic subjects [11].
No significant differences in latencies of oVEMP are observed between the two groups in this study. The oVEMP test in a certain study revealed normal n1 and p1 latencies in two otosclertic groups (6 ears with vertigo and 16 ears without vertigo) [13].
The vHIT results showed a decrease in the gain of lateral SCC in the mixed group only but not for anterior or posterior SCCs with no gain less than 0.8 for all three canals. We explained the decreased VOR gain in the mixed group in the plane of lateral SCC only as it is closer to the sclerotic foci than other SCCs. In a study done by Satar et al. with a sample containing normal subjects, otosclerotic and post-stapedotomy patients, they found that the mean VOR gains for the lateral canal were 0.93 ± 0.05 (0.82–1.06) in the control group, 0.88 ± 0.09 (0.75–1.05) in the otosclerosis group, and 0.82 ± 0.07 (0.74–0.92) in the operated group with a statistically significant difference, but not for anterior or posterior canals [27].
Another study published by Catalano et al. documented a significant difference in left vHIT gain between healthy and otosclerosis patients, all cases had a gain of more than 0.8. No difference was observed in comparison of gains between operated and post-operated groups. They also observed the absence of overt and covert saccades. Considering the small size of their study group, they postulated that the function of the SCCs is not modified by otosclerosis itself and does not change after stapes surgery [28].
Conclusion
We concluded that the peak-to-peak amplitude is suggested to be the best parameter in BC.VEMP in osteosclerotic cases. Also, bone conduction VEMP testing can help in the detection of the site of balance problems in otosclerosis cases. Significant relations were detected between cVEMP and oVEMP abnormalities and the degree of SNHL. Finally, we concluded that lateral SCC is the only involved one among the 3 SCCs in terms of gain and the vHIT gain did not correlate with the severity of hearing loss.
Availability of data and materials
Not applicable.
Abbreviations
- ABG:
-
Air bone gap
- cVEMP:
-
Cervical vestibular myogenic potentials
- IOM:
-
Inferior oblique muscle
- oVEMP:
-
Ocular vestibular myogenic potentials
- PTA:
-
Pure tone audiometry
- SCM:
-
Sternocliomastoid muscle
- vHIT:
-
Video head impulse test
- VOR:
-
Vestibulo-ocular reflex
References
Zafar N, Jamal Z, Khan M (2022) Otosclerosis. StatPearls Publishing, Treasure Island
Ahmad M, Chari DA, McKenna MJ, Quesnel AM (2022) Mixed and sensorineural hearing loss in otosclerosis: incidence, pathophysiology, and treatment. Curr Otorhinolaryngol Rep 10(1):8–15. https://doi.org/10.1007/s40136-021-00390-2
Cureoglu S, Baylan MY, Paparella MM (2010) Cochlear otosclerosis. Curr Opin Otolaryngol Head Neck Surg 18(5):357–362. https://doi.org/10.1097/MOO.0b013e32833d11d9
de Souza C, Glasscock I, Michael E (2004) Cochlear otosclerosis. In: de Souza C, Glasscock I, Michael E (eds) Otosclerosis and stapedectomy diagnosis, management, and complications. Thieme Verlagsgruppe, New York, pp 51–53
Crompton M, Cadge BA, Ziff JL et al (2019) The epidemiology of otosclerosis in a British Cohort. Otol Neurotol 40(1):22–30. https://doi.org/10.1097/mao.0000000000002047
Viza Puiggrós I, Granell Moreno E, Calvo Navarro C, Bohé Rovira M, Orús Dotu C, Quer IAM (2020) Diagnostic utility of labyrinth capsule bone density in the diagnosis of otosclerosis with high resolution tomography. Acta Otorrinolaringol Esp (Engl Ed) 71(4):242–248. https://doi.org/10.1016/j.otorri.2019.09.004
Hodge SE, Ishiyama G, Lopez IA, Ishiyama A (2021) Histopathologic analysis of temporal bones with otosclerosis following cochlear implantation. Otol Neurotol 42(10):1492–1498. https://doi.org/10.1097/MAO.0000000000003327
Quesnel AM, Ishai R, McKenna MJ (2018) Otosclerosis: temporal bone pathology. Otolaryngol Clin North Am 51(2):291–303. https://doi.org/10.1016/j.otc.2017.11.001
Gildener-Leapman N, Linthicum FH (2011) Histopathology of cochlear otosclerosis: implications for cochlear implantation. Otol Neurotol 32(7):e56-57. https://doi.org/10.1097/MAO.0b013e3181fcec6c
Wiatr A, Składzień J, Świeży K, Wiatr M (2019) A biochemical analysis of the stapes. Med Sci Monit 25:2679–2686. https://doi.org/10.12659/msm.913635
Winters SM, Klis SF, Kool AC, Kraaijenga SA, Tange RA, Grolman W (2013) Perioperative bone-conducted ocular vestibular-evoked myogenic potentials in otosclerosis patients. Otol Neurotol 34(6):1109–1114. https://doi.org/10.1097/MAO.0b013e318283969a
Amali A, Mahdi P, Karimi Yazdi A et al (2014) Saccular function in otosclerosis patients: bone conducted-vestibular evoked myogenic potential analysis. Acta Med Iran 52(2):111–115
Lin KY, Young YH (2015) Role of ocular VEMP test in assessing the occurrence of vertigo in otosclerosis patients. Clin Neurophysiol 126(1):187–193. https://doi.org/10.1016/j.clinph.2014.03.032
Paparella MM, Cureoglu S, Shao W, Schachern PA (2007) Otosclerosis and associated otopathologic conditions. Adv Otorhinolaryngol 65:31–44. https://doi.org/10.1159/000098666
Hain TC Vestibular evoked myogenic potential (VEMP) testing–cervical (SCM). Available from: https://dizziness-and-balance.com/testing/VEMP/index.html. Accessed May 2022
Silva TR, Labanca L, Caporali JFM et al (2019) Ocular vestibular evoked myogenic potential (VEMP) reveals mesencephalic HTLV-1-associated neurological disease. PLoS One 14(12):e0217327. https://doi.org/10.1371/journal.pone.0217327
Ismail N, Behairy R, Brakat D (2019) Video head impulse test finding in vestibular lesions. J Otolaryngol ENT Res 11(1):29–36
Murnane OD, Akin FW, Kelly KJ, Byrd S (2011) Effects of stimulus and recording parameters on the air conduction ocular vestibular evoked myogenic potential. J Am Acad Audiol 22(7):469–480. https://doi.org/10.3766/jaaa.22.7.7
Kantner C, Gürkov R (2014) The effects of commonly used upward gaze angles on ocular vestibular evoked myogenic potentials. Otol Neurotol 35(2):289–293. https://doi.org/10.1097/MAO.0b013e318299a812
Rosengren SM, Aw ST, Halmagyi GM, Todd NP, Colebatch JG (2008) Ocular vestibular evoked myogenic potentials in superior canal dehiscence. J Neurol Neurosurg Psychiatry 79(5):559–568. https://doi.org/10.1136/jnnp.2007.126730
MacDougall HG, Weber KP, McGarvie LA, Halmagyi GM, Curthoys IS (2009) The video head impulse test: diagnostic accuracy in peripheral vestibulopathy. Neurology 73(14):1134–1141. https://doi.org/10.1212/WNL.0b013e3181bacf85
Halmagyi GM, Chen L, MacDougall HG, Weber KP, McGarvie LA, Curthoys IS (2017) The video head impulse test. Front Neurol 8:258. https://doi.org/10.3389/fneur.2017.00258
Trivelli M, D’Ascanio L, Pappacena M, Greco F, Salvinelli F (2010) Air- and bone-conducted vestibular evoked myogenic potentials (VEMPs) in otosclerosis: recordings before and after stapes surgery. Acta Otorhinolaryngol Ital 30(1):5–10
Tramontani O, Gkoritsa E, Ferekidis E, Korres SG (2014) Contribution of vestibular-evoked myogenic potential (VEMP) testing in the assessment and the differential diagnosis of otosclerosis. Med Sci Monit 20:205–213. https://doi.org/10.12659/msm.889753
Rosengren SM, Govender S, Colebatch JG (2011) Ocular and cervical vestibular evoked myogenic potentials produced by air- and bone-conducted stimuli: comparative properties and effects of age. Clin Neurophysiol 122(11):2282–2289. https://doi.org/10.1016/j.clinph.2011.04.001
Rosengren SM, Colebatch JG, Young AS, Govender S, Welgampola MS (2019) Vestibular evoked myogenic potentials in practice: methods, pitfalls and clinical applications. Clin Neurophysiol Pract 4:47–68. https://doi.org/10.1016/j.cnp.2019.01.005
Satar B, Karaçaylı C, Çoban VK, Özdemir S (2021) Do otosclerosis and stapedotomy affect semicircular canal functions? Preliminary results of video head impulse test. Acta Otolaryngol 141(4):348–353. https://doi.org/10.1080/00016489.2021.1873416
Catalano N, Cammaroto G, Galletti B et al (2017) The role of cVEMPs and vHIT in the evaluation of otosclerosis and its eventual vestibular impairment: preliminary findings. B-ENT 13(1 Suppl 27):31–36
Acknowledgements
We would like to thank the patients for participating in this research.
Funding
Not applicable.
Author information
Authors and Affiliations
Contributions
SIA and SMZ: supervision and conceptualization. SMZ and DME: software, writing original draft, and methodology. SMZ: resources. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Ethical approval was granted by the ethics committee of the Faculty of Medicine – Alexandria University according to ICH GCP guidelines and applicable local and institutional regulations and guidelines that govern EC operation. Informed consent was provided for all participants of both groups.
Consent for publication
Written informed consent has been obtained.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Elmoazen, D.M., Asal, S.I. & Ziton, S.M. Vestibular-evoked myogenic potentials and video head impulse test in cochlear otosclerosis. Egypt J Otolaryngol 39, 182 (2023). https://doi.org/10.1186/s43163-023-00544-7
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s43163-023-00544-7