Abstract
Objective
To outline the main results of the 2021 International Conference on Robotics and Automation (ICRA 2021) of the Institute of Electrical and Electronics Engineers (IEEE) and review the advances in artificially intelligent joint surgery in China.
Methods
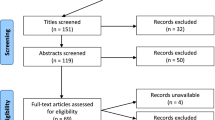
The keynote speeches of the 2021 ICRA were summarized in detail, and publications indexed by five core electronic databases (PubMed, Cochrane, Medline, Embase and CNKI) were systematically surveyed (cutoff date: July 30, 2021) in terms of the main topics of the conference. Publications directly related to artificially intelligent joint surgery in China were identified by using the search strategies of (robotic AND arthroplasty OR replacement), (navigation AND arthroplasty OR replacement), (artificial intelligent AND arthroplasty OR replacement), and (mixed reality AND arthroplasty OR replacement) and systemically reviewed.
Results
While robot-assisted arthroplasty in China is mainly performed using robots made in other countries (e.g., Mako from Stryker, USA), China’s domestic R&D of robots and clinical studies of robotic joint surgery have made some achievements. Although reports on the safety, effectiveness and clinical efficacy of China’s domestic robot-assisted joint surgery were presented at conferences, they have rarely been published in journals. Existing data indicate that, after the learning curve is overcome, robot-assisted hip and knee replacement surgery can fully achieve the established goals of precision and individualization and can significantly improve the accuracy of prosthesis placement angle and the recovery of the mechanical axis as compared with conventional surgery. The downside is that the low level of intelligentization and individualization means that existing designs are not conducive to personalization during surgery, resulting in low cost-effectiveness.
Conclusion
The safety and efficacy of domestic robot-assisted arthroplasty in China are well documented, and its accuracy and short-term clinical efficacy have been reported. However, the long-term clinical efficacy and the cost-effectiveness of large-scale clinical application of this technique warrants further study. The inadequacies of robot-assisted surgery should be remedied through the deep integration of medicine, engineering and the network.
Similar content being viewed by others
Introduction
With the full support of Chinese governments, local and central, artificial intelligence (AI)-assisted joint surgery in China is prepared for a fast track of development. Against this background, the International Conference on Robotics and Automation (ICRA 2021), sponsored by the Institute of Electrical and Electronics Engineers (IEEE), was held in ** in the virtual space to reflect the full life cycle of the corresponding physical item through a simulation process involving a multidisciplinary, multiphysical, multiscale and multiprobability integration that makes full use of physical models, sensor updates, operation history and other data. It can be seen as a digital map** system involving one or more important and interdependent equipment system(s). When applied to orthopedics, it assists in the construction of full-dimensional digital models of “live” human body systems via full-range, cross-scale data perception and digital modeling of the human body for precision and smart medicine. By taking advantage of computer-generated graph and image description techniques, finite element analysis, equivalent mechanics and AI calibration, Dr. Tang’s team conducted a theoretical mechanics analysis and mechanical validation of the three-element stabilization system of the proximal femur. They proposed, for the first time, a machine learning-based fracture classification system upon examining intertrochanteric femoral fracture patterns using the AI clustering algorithm and generated views of anterior, posterior, lateral and medial fractures. They analyzed 504 cases of femoral intertrochanteric fractures and found that most of the fracture lines (anterior view: 85.9%; posterior view: 52.0%; internal lateral view: 49.0%; external lateral view: 62.7%) ran along the intertrochanteric line, which was highly consistent with conventional fracture classification results based on clinical experience, suggesting that the established system is of great significance for describing morphological characteristics and adjuvant therapy [3, 4] (Table 1).
Smart solutions for orthopedic surgery are based mainly on automatic preoperative planning with next-generation AI technology to establish a knowledge- and data-driven method and a systematic, hierarchical and expandable knowledge description system that performs knowledge-aided image processing and preoperative planning and ultimately yields a clear and thorough surgical plan [5]. In recent years, AI and deep learning have flourished in various fields, and the clinical use of robots in joint surgery is a milestone in the development of orthopedics. At this conference, the robot design team presented the process used to design and develop robots for joint surgery. Professor Qinghu Meng from Southern University of Science and Technology first reviewed the development of robots, from industrial robots to conventional medical robots to minimally invasive surgery robots, focusing on wireless capsule endoscopy robots and image-based automatic diagnosis systems, which have a diagnostic accuracy up to 100% [6]. According to Prof. Meng, intelligent medical care will be developed for frequent, real-time and home-based physical examinations, unmanned intelligent care in infectious disease wards and intensive care units (ICU), supermarket- and home-based diagnosis and treatment of digestive diseases, the specialization and miniaturization of robot-assisted surgery, and the digitalization and intelligentization of orthopedic robot-assisted surgery.
The speech given by Professor Fangwen Zhai from the Intelligent Robot Research Center, Institute for Artificial Intelligence, Tsinghua University, was about “The Future of Orthopedic Robots”. He pointed out that most orthopedic surgical robots, such as spinal surgical robots, joint surgical robots and trauma surgical robots, can perform only relatively simple surgical procedures at present. Therefore, multiple sets of surgical robots must be purchased to operate on different body parts, which increases cost, lengthens the learning curve (LC), and consume more surgical resources. More importantly, the lack of standards and sharing mechanisms among industries and the lack of openness or compatibility of software for various robot systems render it impossible for preoperative planning and robot control software to interact with each other and cause serious data segmentation, which seriously prevents the industry from moving forward. Therefore, it is imperative to develop a unified infrastructure and a common software and hardware platform and to work out various functional modules based on that platform to allow compatibility among surgical modes for different surgeries. Surgery 4.0, launched by Johnson & Johnson, is just one of such unified platforms [7].
Professor Zhai pointed out that intraoperative registration is a bottleneck for robotic surgery because of high skill requirements on doctors, the radiation exposure during long-time intraoperative imaging and point registration and surface scanning methods that affect the surgical process. Therefore, it is necessary to develop a highly efficient automatic registration mode that offers clear and radiation-free real-time imaging support and fast registration algorithms coupled with more flexible scene perception methods and to establish a registration-free surgical navigation mode that provides preoperative qualitative planning, intraoperative multimodal real-time perception and real-time surgical plan generation. In addition, he emphasized that, at present, surgical robots are still a high-degree-of-freedom locator, lacking real-time environmental perception and complex decision-making ability and having weak force control. In the future, robot designs need to be customized and specialized to make robots more dexterous, gentler and more adaptive to various types of surgery.
From the perspective of a surgeon, Professor Jiying Chen comprehensively answered the question “What kind of robot is needed for joint surgery?”. He focused on the shortcomings of existing robots for joint surgery, such as the lack of data accumulation, a low level of intelligentization and the need for manual assistance to complete the operation. The high demand for wide-scope preoperative radiography and the implantation of the reference frame in robot-assisted hip and knee surgery are likely to cause damage to the patient. The cumbersome intraoperative registration procedure and high failure rate will prolong the operation time. The inability of robots to perceive soft tissue tension makes them unable to provide forecasting factors of the impact and dislocation. In view of this, Professor Chen proposed a vision for the future of joint surgery robots: a focus on improving the function and effectiveness of robots, increasing their 3D accuracy and enhancing the individualization of force lines, positions and angles; continuously incorporating the latest knowledge into preoperative planning and enriching personalized design, e.g., by considering the role of the hip-spine relationship in the hip joint and the roles of developmental deformities and extra-articular deformities in the knee joint.
The clinical benefits and ethical risks of robotic joint surgery are an important research direction that cannot be ignored. The speech made by professor ** Lin from Peking Union Medical College Hospital was titled “Focus on Clinical Value: Reflections on the Innovation of the TKA Robot, a Chinese Domestic Product”. In his keynote speech, he defined the clinical value from six dimensions, i.e., patient benefits, clinical pain point resolution, doctors’ self-realization, clinical application costs, learning curve (LC), and the payer’s net expenditure. Of these, patient benefits, clinical pain point resolution, and doctors’ self-realization were used as the numerator items, and clinical application costs, doctors’ LC and the payer’s net expenditure as the denominator items. He asserted that if a product can achieve breakthroughs in two of the six dimensions, the product can be called a “great breakthrough”. Furthermore, he stated that the “one-vote veto” should be avoided due to the difficulty in moving forward along certain dimensions. He further pointed out that robotic surgery is a powerful tool for achieving technological breakthroughs and that although it currently has some shortcomings, surgeons should put more trust in the robot-assisted surgery.
5G network and mixed reality in orthopedics
China has built up the largest 5G network base stations in the world, and the widespread application of 5G network offers great opportunities for telemedicine. By taking advantage of 5G communication technology, experts at the General Hospital of PLA remotely guided its surgeons at Hainan Branch to complete a robot-assisted total hip arthroplasty (THA) on two patients. During these procedures, the human-robot communication was smooth, the manipulators and software worked stably, and the surgeries achieved satisfactory short-term efficacy. These surgeries combined robotic operation and 5G communication technology, two state-of-the-art technologies, and attained preliminary results that supported the safety and potential value of 5G communication technology in telemedicine. 5G communication technology-based telemedicine can provide technical support for the hierarchical diagnosis and treatment policies, and what the PLA General Hospital did represents a valuable attempt to apply telemedicine into surgical operations [8].
Mixed reality (MR) technology is a brand-new digital holographic imaging technology and a new interdisciplinary frontier [ The datasets used and/or analyzed in the current study are available from the corresponding author on reasonable request. Proceedings of 2005 IEEE Computational Systems Bioinformatics Conference. August 8-11, 2005. Stanford, California, USA. Proc IEEE Comput Syst Bioinform Conf. 2005:3–402. Konig IR, Fuchs O, Hansen G, von Mutius E, Kopp MV. What is precision medicine?. Eur Respir J. 2017;50(4):1700391. https://doi.org/10.1183/13993003.00391-2017. Li J, Tang S, Zhang H, Li Z, Deng W, Zhao C, et al. Clustering of morphological fracture lines for identifying intertrochanteric fracture classification with Hausdorff distance-based K-means approach. Injury. 2019;50(4):939–49. Li M, Li ZR, Li JT, Lei MX, Su XY, Wang GQ, et al. Three-dimensional map** of intertrochanteric fracture lines. Chin Med J. 2019;132(21):2524–33. Maier-Hein L, Vedula SS, Speidel S, Navab N, Kikinis R, Park A, et al. Surgical data science for next-generation interventions. Nat Biomed Eng. 2017;1(9):691–6. Soffer S, Klang E, Shimon O, Nachmias N, Eliakim R, Ben-Horin S, et al. Deep learning for wireless capsule endoscopy: a systematic review and meta-analysis. Gastrointest Endosc. 2020;92(4):831–9. Teber D, Engels C, Maier-Hein L, Ayala L, Onogur S, Seitel A, et al. Surgery 4.0-are we ready? Urologe A. 2020;59(9):1035–43. Kong XP, Fu J, Chen JY, Chai W, Wu D, Li ZF, et al. 5G communication technology remotely guides two cases of robot-assisted total hip arthroplasty. Chin J Reparative Reconstr Surg. 2020;34(11):1492–3. Hu HZ, Feng XB, Shao ZW, **e M, Xu S, Wu XH, et al. Application and prospect of mixed reality technology in medical field. Curr Med Sci. 2019;39(1):1–6. Lei PF, Su SL, Kong LY, Wang CG, Zhong D, Hu YH. Mixed reality combined with three-dimensional printing technology in total hip arthroplasty: an updated review with a preliminary case presentation. Orthop Surg. 2019;11(5):914–20. Lacy AM, Bravo R, Otero-Pineiro AM, Pena R, De Lacy FB, Menchaca R, et al. 5G-assisted telementored surgery. Br J Surg. 2019;106(12):1576–9. Wu X, Liu R, Xu S, Yang C, Yang S, Shao Z, et al. Feasibility of mixed reality-based intraoperative three-dimensional image-guided navigation for atlanto-axial pedicle screw placement. Proc Inst Mech Eng H. 2019;233(12):1310–7. Guo XZ, Dou BX, Liu Q, Huang Y, Zhou YX. Comparison of the acetabular orientation after minimally-invasive total hip arthroplasty with and without computer-navigation: a clinical report of 106 hip in 87 patients. Natl Med J China. 2007;87(35):2489–93. Zhang GQ, Chen JY, Chai W, Liu M, Wang Y. Comparison between computer-assisted-navigation and conventional total knee arthroplasties in patients undergoing simultaneous bilateral procedures: a randomized clinical trial. J Bone Joint Surg Am. 2011;93(13):1190–6. Hampp EL, Chughtai M, Scholl LY, Sodhi N, Bhowmik-Stoker M, Jacofsky DJ, et al. Robotic-arm assisted total knee arthroplasty demonstrated greater accuracy and precision to plan compared with manual techniques. J Knee Surg. 2019;32(3):239–50. Zhang Y, Gu WH. Artificial intelligence in knee surgery: status and prospect. J Trauma Surg. 2020;22(02):81–6. Liu ZY, Zhang J, Li J, He K, Zhang YM, Zhang Y. The role of continuous optimization program in damage control of perioperative blood loss during primary total knee arthroplasty. J Trauma Surg. 2020;22(02):94–100. Zhou Y, Shao H, Huang Y, Deng W, Yang D, Bian T. Does robotic assisted technology improve the accuracy of acetabular component positioning in patients with DDH? J Orthop Surg (Hong Kong). 2021;29(2):1872660909. Li JC, Li M, Ji QB, Sun JY, Zheng QY, Zhang GQ, et al. Comparison of lower limb length difference between robot-assisted and traditional methods of total hip arthroplasty. Chin J Orthop. 2021;41(08):480–7. Chai W, Kong X, Yang M, Puah KL, Tang P, Chen J. Robot-assisted total hip arthroplasty for arthrodesed hips. Ther Clin Risk Manag. 2020;16:357–68. Chai W, Guo RW, Puah KL, Jerabek S, Chen JY, Tang PF. Use of robotic-arm assisted technique in complex primary total hip arthroplasty. Orthop Surg. 2020;12(2):686–91. DelSole EM, Vigdorchik JM, Schwarzkopf R, Errico TJ, Buckland AJ. Total hip arthroplasty in the spinal deformity population: does degree of sagittal deformity affect rates of safe zone placement, instability, or revision? J Arthroplast. 2017;32(6):1910–7. Ike H, Dorr LD, Trasolini N, Stefl M, McKnight B, Heckmann N. Spine-pelvis-hip relationship in the functioning of a total hip replacement. J Bone Joint Surg Am. 2018;100(18):1606–15. Zhang J, Huang Y, Zhou B, Zhou Y. Mid-term follow-up of acetabular revision arthroplasty using jumbo cups. Orthop Surg. 2019;11(5):811–8. Fu J, Chai W, Ni M, Li X, Liu K, Kong XP, et al. Learning curve difference between robotic-assisted and conventional Oxford unicompartmental knee arthroplasties. Chin J Joint Surg (Electronic Edition). 2019;13(05):547–53. Di Martino A, Bordini B, Barile F, Ancarani C, Digennaro V, Faldini C. Unicompartmental knee arthroplasty has higher revisions than total knee arthroplasty at long term follow-up: a registry study on 6453 prostheses. Knee Surg Sports Traumatol Arthrosc. 2021;29(10):3323–9. Zhu KC, Wang QJ, Chen YS, Shen H, Peng XC, Zhang XL, et al. Short-term clinical outcomes of robotic-assisted unicompartmentalknee arthroplasty. Chin J Joint Surg (Electronic Edition). 2019;13(05):547–53. Wang W, Chen X, Fan Y, Lin J. A clinical study on robotic-assisted total knee arthroplasty for severe knee osteoarthritis. Chin J Bone Joint Surg. 2021;14(05):393–8. **a R, Zhai Z, Zhang J, Yu D, Wang L, Mao Y, et al. Verification and clinical translation of a newly designed “Skywalker” robot for total knee arthroplasty: a prospective clinical study. J Orthop Translat. 2021;29:143–51. **a RZ, Tong ZC, Zhang JW, et al. Early clinical study of domestic “Skywalker” surgical robot knee arthroplasty. J Pract Orthop. 2021;27(02):108–13. Chai W, **e J, Zang XG, Yan TF, Zhao YL, He CA, et al. Animal experimental study on domestic robot-assisted total knee arthroplasty. Chin J Reparative Reconstr Surg. 2020;34(11):1376–81. Chai W, **e J, Zang XG, He C, Yan TF, Liu L, et al. A cadaveric experimental study on domestic robot-assisted total knee arthroplasty. Chin J Reparative Reconstr Surg. 2021;35(04):409–13. Kayani B, Konan S, Huq SS, Tahmassebi J, Haddad FS. Robotic-arm assisted total knee arthroplasty has a learning curve of seven cases for integration into the surgical workflow but no learning curve effect for accuracy of implant positioning. Knee Surg Sports Traumatol Arthrosc. 2019;27(4):1132–41. Not applicable. None of the following authors or any immediate family members has received anything of value from or has stock or stock options held in a commercial company or institution related directly or indirectly to the subject of this article. Technological Innovation and Application Demonstration Project of Chongqing (cstc2018jscx-msyb0541); Innovative Technology in Military and Clinical Medicine (2018JSLC0035); Continual Medical Education Project of Chongqing (2020-04-07-067); Central Committee Guiding Local Technology Development Project (0028). Zhonghua Xu: Data curation, Data analysis, Writing. Yuan Zhang: Conceptualization, review and revision. The author(s) read and approved the final manuscript. Not applicable. All patients provided consents to participate in this study, as per our institution’s standards as stated in the research consent forms, which specify that the research information obtained may be used for publication. The authors have no conflicts of interest or competing interests in the study implementation, publication or data interpretation. Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations. Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. Xu, Z., Zhang, Y. What’s new in artificially intelligent joint surgery in China? The minutes of the 2021 IEEE ICRA and literature review.
Arthroplasty 4, 10 (2022). https://doi.org/10.1186/s42836-021-00109-0 Received: Accepted: Published: DOI: https://doi.org/10.1186/s42836-021-00109-0Availability of data and materials
References
Acknowledgements
Disclosure
Funding
Author information
Authors and Affiliations
Contributions
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Consent for publication
Competing interests
Additional information
Publisher’s Note
Rights and permissions
About this article
Cite this article
Keywords