Abstract
Background
Uterine smooth muscle tumor of uncertain malignant potential (STUMP) is a group of uterine smooth muscle tumors which cannot be classified as a subtype of leiomyoma or leiomyosarcoma. Diagnosis, prognosis, and treatment of these tumors are challenging due to recurrence, potential of malignancy, and metastasis.
Methods
A retrospective cohort study was conducted in southern Iran during 2011 to 2020. We included records of 21 patients with STUMP and 24 patients with leiomyoma by simple randomized sampling in the tertiary health care centers in Shiraz, southern Iran. Slides were reviewed by an expert pathologist for examining mitosis, necrosis, and atypia, and also proper blocks were selected for immunohistochemistry (IHC) staining.
Results
From 45 participants, 21 (46.7%) and 24 (53.3%) patients were in the STUMP and normal leiomyoma groups, respectively. Odds ratio and 95% confidence interval (OR (95% C.I)) of pathologic size in the range of 5–10 cm was significantly higher in the STUMP group compared with normal leiomyoma. (CI: 7.22 (1.44–36.22)). Additionally, hyaline necrosis 0.05 (0.0-0.91), mild to moderate atypia 0.02 (0.0-0.4), moderate to severe atypia 0.01 (0.0-0.22), focal atypia 0.01 (0-0.26) and diffuse atypia 0.01 (0-0.26) were significantly fewer in normal leiomyoma compared to the STUMP group. Negative P16 0.01 (0.0007-0.24) and negative Bcl2 0.22 (0.06–0.81) were significantly higher in the normal leiomyoma group compared with the STUMP group. The cut-off points for predicting STUMP were 2.5% (sensitivity = 62% and specificity = 100%) and 45% (sensitivity = 43% and specificity = 96%) for P16 and bcl2, respectively.
Conclusion
The category and management of STUMP continues to progress. The diagnosis for STUMP mainly depends on the histopathological manifestations. No single IHC marker such as P53, P16, and Bcl-2 has proved robust enough in separating STUMP from other leiomyoma variants; however, according to our study, we suggest combination use of P16 and Bcl-2 (cut off 2.5 and 45%, respectively) to distinguish equivocal cases of STUMP.
Similar content being viewed by others
Background
Smooth muscle tumors of the uterus, most common gynecological complaint worldwide, are generally divided into benign (leiomyoma) and malignant (leiomyosarcoma) tumors [1] which mostly affect women during the reproductive age (mainly before menarche) [2] and often regress after menopause. Leiomyoma is diagnosed in 70% of white and 80% of black women [3]. It can be asymptomatic or present with a wide range of symptoms including heavy menstrual bleeding, fatigue, painful periods, non-cyclic pain, painful intercourse, pelvic pressure, urinary incontinence, constipation, infertility, abortion, and pregnancy complications [4]. Therefore, diagnosis of STUMP is clinically difficult and definite diagnosis can be confirmed after surgery [5].
There are other variants of uterine smooth muscle neoplasm which can present like leiomyomas, classified into smooth muscle tumors of uncertain malignant potential (STUMP) and different types of malignant mesenchymal tumors (sarcomas) [6]. The term uterine smooth muscle tumor of uncertain malignant potential was firstly used by Kempson in 1973 [1]. World Health Organization (WHO) defines STUMP as intermediate group of uterine smooth muscle tumors which cannot be assigned to either a benign or a malignant tumor, but concern of malignancy remains [5]. Etiology and risk factors of STUMP have not been identified yet. Differentiation of various types of uterine smooth muscle tumors can be made based on three main histopathologic features including cytologic atypia, mitotic count, and tumor cell necrosis [7, 8]. Presence of ambiguous tumor necrosis with difficult differentiation, diffuse atypia and/or mitotic count is not compatible with a benign or malignant category [9]. As the definition of STUMP is variable, the exact recurrence rate of STUMP, means patients underwent operation for the second time due to uterine tumor and pathologic findings showed STUMP again, is not clear, but based on different studies the recurrence rate is almost 7.3 to 26.7% [10]. Distant metastasis by STUMP defines as finding of tumor outside of uterus suspected to have the same origin with STUMP in CT scan/ MRI or proved by pathology. This phenomenon is rare, but it has been reported in different sites such as the ovary, pelvis, abdomen, omentum, liver, lung, pleura, bone, spine, and retro-peritoneum [11].
Immunohistochemistry could be helpful in diagnosis of STUMP, and several tumor markers such as ER, PR, Ki67, P53, P16, and Bcl-2 have been studied recently [12, 13]. Studies showed that the expression of Bcl-2 was more prominent in leiomyomas compared to leiomyosarcoma and STUMP [13]. In contrast to leiomyosarcomas, expression of Bcl-2 was concomitant with poor prognosis in STUMP [14]. P16 expression was more significant in leiomyosarcoma. Similarly, it has adverse prognostic value in STUMP and its strong expression was detected in metastasizing STUMP [15, 16]. Mutated P53 is generally found in leiomyosarcomas and can be an indicator of malignancy. However, expression of P53 in STUMP was more similar to leiomayomas than leiomyosarcoma [17]. Detection of P16 and P53 overexpression can be helpful to determine high risk patients [18].
In this study, we aimed to determine the clinical and histological features besides immunohistochemistry profile, with focus on P16, P53 and Bcl2, among patients with STUMP diagnosed at the hospitals of Shiraz University of Medical Sciences between the years 2012 to 2021.
Methods
Study settings and participants
A retrospective cohort study was conducted in Faghihi hospital, Shiraz University of Medical Sciences. Clinical documents of all patients diagnosed with STUMP since 2011 to 2020 were collected from archives of gynecology oncology department of Motahari clinic and Faghihi hospital, Shiraz University of Medical Sciences. During this period, 33 patients diagnosed with STUMP were documented in our department, but due to absence of clinical data or pathologic slides/blocks or corruption of them, 21 cases were collected at the end. Slides were reviewed by two expert pathologists for examining mitosis, necrosis, and atypia; also, proper blocks were selected for immunohistochemistry (IHC) staining.
Immunohistochemistry
Tissue samples included 45 cases of STUMP and leiomyoma. Immunohistochemistry was performed on formalin fixed paraffin blocks. The largest and well-fixed block of each patient was selected. Tissue slides (4 mm thick) were deparaffinized in xylene and rehydrated in alcohol solutions. Antigen retrieval of tissues was carried out by boiling in EDTA buffer at PH 8 (Master Diagnostica) for 20 min. Tissues treated for 10 min at room temperature using peroxidase solution (Master Diagnostica) and then incubated with primary antibody (different time for different antibodies) (Table 1). The stained tissue sections with haematoxylin were reviewed separately by two pathologists who were blinded to clinical parameters.
According to intensity and percentage of positive cells, Bcl-2 expression was classified. Scores of 2 + and 3 + of intensity within more than 40% of cells were defined as Bcl-2 positive as shown in Table 2. Expression of P16 by any percentage of cells was classified as positive.
P53 was interpreted as below:
-
Wild type (normal): scattered nuclear staining, mild epithelial (basal sparing)
-
Aberrant (mutational type): 80% strong and diffuse nuclear staining, complete absence of nuclear staining in all cells, moderate to strong cytoplasmic staining.
Statistical analysis
Frequency (relative frequency) was used to describe the variables qualitatively. Chi-Square test, exact Fisher test, and binary logistic regression were used to analyze the data. Odds ratio and corrected odds ratio with 95% confidence interval (OR (95% C.I)) were reported [19], and receiver operating characteristic (ROC) analysis with Uden index = sensitivity + specificity-1 (to determine cutoffs) were used. IBM SPSS (Statistical Package for the Social) version 22 software was used. The significance level was considered 0.05.
Results
From 45 participants, 21 (46.7%) and 24 (53.3%) were in STUMP and leiomyoma groups, respectively. Patients had a mean ± SD aged of 41.57 ± 9.21 (range: 25–69) years. Age, gravid, menopause status, history of radiotherapy, past medical history, and type of operation between STUMPs and leiomyomas has been compared and presented in Table 3.
The majority of participants were under 50 years of age (82.2%), had gravid greater and equal to three (42.2%), were not menopaused (95.6%), had no history of radiotherapy (97.8%), had no past medical history (97.8%), and had bilateral or unilateral sal**o-oophorectomy in addition to hysterectomy or myomectomy (40%). Only one of STUMP patient had undergone radiotherapy because of fragmented specimen. So myometrial invasion and/or leiomyosarcoma could not be ruled out and the physician decided to do radiotherapy for her. Furthermore, the STUMP and normal leiomyoma groups were the same regarding age, gravid, menopause state, history of radiotherapy, past medical history, and type of operation (p-value > 0.05 for all). Positive history of diabetes mellitus or hypertension was considered as “yes” in the past medical history.
The size and myoma status in sonography, sonographic count, sign and symptom of the patients, follow-up distance, recurrence, sign of metastasis/sarcoma, Hb, and LDH of the STUMP group are shown in Table 4. Non-myoma means uterine tumor was not described as ‘myoma’ in ultrasonography or MRI report on the basis of shape, border and other radiologic findings.
Tumor marker (CA-125, CA19-9, HE4), pathological size, mitosis, necrosis, severity of atypia, distribution of atypia, immunohistochemistry status (P53, P16, Bcl2), and different variants were compared between the STUMP and leiomyoma groups in Table 5.
Tumor markers were negative in 95.6% (43/45) of patients; 44% (19/43) and 56% (24/43) were in the STUMP and leiomyoma groups, respectively. All the patients in the leiomyoma group had negative tumor marker. Tumor size of 5- 10 cm was significantly higher in the STUMP group compared with leiomyoma (p-value < 0.05); however, no difference was seen regarding size ≥ 10 cm between the groups (p-value > 0.05).
Considering histopathologic features, from 45 participants, 97.8% had mitosis less than five; 45% (20/44) and 55% (24/44) of them were in the STUMP and leiomyoma groups, respectively. Hyaline necrosis is characterized by accumulation of a pink, homogenous material known as hyaline that significantly less in leiomyoma compared with the STUMP group (p-value < 0.05); however, there was no significant difference regarding coagulative necrosis, hitologically diagnosed by an area of necrosis palisades with karyorrhexis, nuclear debries and inflammatory cells infiltration, between the two groups (p-value > 0.05). This type of necrosis is highly advised leiomyosarcoma. However, some of STUMPs with non or mild atypia and afew mitotic figures show this type of necrosis [8]. The difference of severity and distribution of atypia between the STUMP and leiomyoma groups was statistically significant (p-value < 0.05).
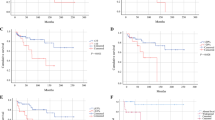
P16 and Bcl2 expression is defined as the combination of nuclear and cytoplasmic immunoreactivity for P16 and nuclear staining for Bcl2. Our immunohistochemistry results demonstrated that negativity for P16 and Bcl2 was significantly higher in the leiomyoma group compared to the STUMP group (p-value < 0.05 for both). To get a better understanding of the optimal cut-off points of the P16 and Bcl2 predicting STUMP, we presented ROC curve results in Fig. 1; Table 6. The P16 and Bcl-2 of more than 2.5% and 45% could predict STUMP, respectively with sensitivity and specificity of 62% and 100% for P16 and 43% and 96% for Bcl-2 (Figs. 2 and 3). All the cases in the STUMP and leiomyoma groups were negative for P53. Four out of 20 STUMP cases showed recurrence, and two of them had distant involvement. Bcl-2 presented with intensity of 5% and.
P16 negativity in one of the cases with local recurrence and the latter one shows Bcl-2 expression of 90% and 10% P16 expression. One of the cases with distant metastasis showed negativity of all markers and another one expressed 20% P16 and 10% Bcl-2.
Discussion
Diagnosis and treatment of STUMPs are challenging as their features cannot fulfill the criteria of benign or malignant tumor. Clinical, imaging or laboratory methods can be somehow helpful in diagnosis of STUMP; however, final diagnosis can be made by pathologic evaluation after hysterectomy or myomectomy.
As in previous studies, the majority of STUMP cases were in the premenstrual phase (95.2%) and younger than 50 years old (85.7%) [12, 20]. Similar studies showed that leiomyomas mostly occurred in the 4th decade of life and reproductive ages [4].
The gold standard of management of STUMP is hysterectomy, but in childbearing ages it is not a choice because of fertility issues and making decision for the type of operation can be challenging due to the risk of recurrence and chance of fertility [21]. In our study, most of the STUMP cases (33.3%), similar to leiomyomas (45.8%), underwent TAH/BSO or USO. In STUMPs, TAH (28.6%) and myomectomy (23.8%) were more prevalent after TAH/BSO or USO, respectively. In a similar conclusion, Rizzo’s study showed that hysterectomy was more common than myomectomy [12]. TAH/BSO or USO plus omenectomy were done in 14.3% of STUMPs; however, none of leiomyoma cases had omentectomy. In a systematic review of 34 studies and 189 cases of STUMP, 79 patients had myomectomy (42%), 60 had TAH/BSO (32%), and 50 patients underwent TAH (26%) [19]. In Yordanov’s study, the type of operation was hysterectomy and myomectomy in 85.7% and 16.7% among the STUMP cases, respectively [1]. However, myomectomy (41.7%) was more prevalent than TAH (12.5%) in our cases with leiomyomas.
In ultrasound or magnetic resonance imaging (MRI) examination, about 50% of the STUMP group were 5-10 cm, and the rest were equal or more than 10 cm. Considering echogenicity and radiologist report, most of STUMP cases were similar to myomas, but 33.3% of them showed atypical findings. Additionally, ultrasonography or MRI of most of STUMP subjects showed multiple lesions. One study about ultrasound features of uterine smooth muscle tumor revealed that cystic areas within the lesion was detected in typical leiomyomas, leiomyoma variants, adenomyomas, and also in the cases of STUMP and leiomyosarcoma. Detection of regular borders, echogenicity, size and presence of shadowing was similar in benign and malignant lesions [22]. Bonneau et al. compared sonography and MRI findings of 85 leiomyoma with 23 malignant mesenchymal tumor and STUMP cases; their results revealed that single tumor, presence of free fluid, and absence of acoustic shadowing were detected in STUMP [23]. However, STUMP can be detected as leiomyoma or leiomyosarcoma on MRI; its common feature on MRI included homogeneously low T2 signal or areas of T2 hyperintense necrosis [24].
In our study, most of the patients with STUMP presented with abnormal uterine bleeding (AUB), and the rest of them presented with pelvic pain (23.8%), incidental finding by mass sensation or routine ultrasonography (14.3%), and during infertility work ups (14.3%). Similarly, the study on 16 cases of STUMP demonstrated that AUB was the most common presentation of STUMP as well [25]. A review study mentioned that STUMPs could present as typical leiomyomas with AUB, anemic symptoms, pelvic mass or pressure and combination of them that supports our results [10, 26, 27].
Patients with STUMP should have been followed up every six months during five years after diagnosis and then annually for next five years. In these patients, follow up included history taking and physical examination. Additionally, imaging studies such as chest radiography, pelvic ultrasonography, MRI and/or PET-CT should be performed each year to detect recurrences [27]. In a systematic review of 189 STUMP cases, recurrence was detected in 37 cases (19.5%): 23 local recurrences (62.2%) and 14 distant metastasis (37.8%) to the lung, abdomen, and other organs [20]. Guntupalli et al. conducted a review on 41 patients with STUMP in which three patients had recurrence during the mean follow-up time of 45 months [28]. In the research of Deohar et al., out of 21 STUMP cases, one patient presented with metastatic liver disease 3 years after the first surgery [29]. Canciani et al. and Shapiro et al. reported metastasis to the lung and humerus during the follow up of the STUMP cases, respectively [30, 31]. Similarly, another study reported an intraperitoneal mass 3 years after myomectomy with diagnosis of STUMP [32]. In our research, duration of follow up in 90% of the STUMP patients was under 12 months to 120 months, and just 10% of them (two patients) had a longer follow up of more than 120 months. During the follow up, there was recurrence in 4 out of 20 patients (20% of STUMPs); two of them had distant involvement; pelvic sarcoma and lung metastasis was detected in one of them and adnexal mass, lung metastasis, and probable liver involvement occurred in another one.
Serum level of lactate dehydrogenase (LDH) can be helpful in predicting the tumor prognosis, development, metastasis, and progression [33]. Several studies showed increased serum level of LDH in uterine sarcomas compared to leiomyomas. Similarly, the study of Zhang et al. demonstrated higher levels of LDH in leiomyosarcomas in comparison to degenerated uterine fibroids [34]. Matsuda et al. evaluated the serum level of LDH in 21 usual leiomyomas, 7 atypical leiomyomas, and 6 leiomyosarcomas; high LDH was detected in 3 cases of leiomyosarcomas [35]. In our study, one out of 21 cases of STUMP had high serum level of LDH with the cut-off point of 480 IU/L.
There are different histopathologic criteria hel** STUMP definition in which mitosis, cellular atypia, and necrosis are the most important features. In our study, 20 out of 21 STUMP cases had less than five mitoses in 10 high power field (HPF) which was similar to leiomyomas. Most of the STUMPs (42.9%) had moderate to severe atypia and no necrosis (57.1%). In a similar way, original criteria of STUMP defines it as a tumor with 3–5 mitosis per HPF and atypia or 6–9 mitosis per HPF, mild atypia and increased cellularity or mitosis more than 15 per HPF [9]. In a retrospective study by Lanqing Huo et al. on 67 STUMP cases, the majority of cases had 5–10 mitosis per HPF (52.3%), mild atypia (65.7%), and no necrosis (77.6%) [36]. The study of Zhang et al. showed that seven out of 18 cases had moderate to severe atypia and 5–10 mitosis per HPF [37]. A review study of leiomyoma variants defines STUMP as a tumor with focal or diffuse atypia and mitotic count under 10 per 10 HPF; or coagulative necrosis and mitotic count less than 10 per 10 HPF; or high cellularity and mitosis more than 15 per 10 HPF [38]. Similar to our study, Gupta et al. analyzed 22 cases of STUMP; 15 cases had moderate to severe atypia, 9 focal or multifocal atypia, and 6 diffuse atypia. 18 out of 22 cases had less than 10 mitosis, and four cases had more than 10 mitosis. Necrosis was detected in seven cases, one coagulative necrosis, and six hyaline necrosis [9]. Patel et al. evaluated 67 cases including 57 leiomyoma, eight leiomyosarcoma and two STUMPs, in which leiomyoma had no atypia and less than five mitoses per 10 HPF in the same way our research but five cases had ischemic necrosis. Additionally, two STUMP cases had less than five mitoses per 10 HPF, ischemic necrosis, and moderate-to-severe atypia, similar to our study [39].
Because of difficulties in diagnosis of STUMP, researchers have figured out that the combination of immunohistochemistry (IHC) and clinicopathological findings can be more helpful in determining the final diagnosis and risk of recurrence in STUMP. We analyzed Bcl-2, P16 and P53 IHC markers in STUMP and leiomyoma cases. P16, a tumor suppressor protein, plays an important role in regulation of cell cycle, and the related gene was deleted in a variety of malignant cells and tissues [40]. In our results, positive P16 was detected in 13 STUMP cases (out of 21) although none of leiomyoma cases expressed this marker that was statistically significant (P value < 0.001). Positivity of P16 (intensity > 2.5%; sensitivity 62%, specificity 100%) is a helpful diagnostic marker for equivocal cases of STUMP. Besides, P53 was the wild type (normal) in all our STUMP and leiomyoma cases. TP53 gene can be mutated frequently, and its protein, so called P53, acts as a tumor suppressor [18]. In the study of Tabrizi et al., none of STUMP cases had positive P53 that was in the same line with our study [41]. In another research, one out of 18 STUMP cases showed positive P53 [37]. Similarly, Manxhuka et al.’s results revealed positive P53 in one out of six STUMPs, none of leiomyoma cases, and 16 out of 34 leiomyosarcoma cases [13].
Some studies demonstrated the higher expression of P16 and P53 in leiomyosarcoma cases compared to STUMP and leiomyoma cases [15, 42]. Although in our results presentation of P16 was higher in STUMPs in comparison to leiomyoma cases, study of O’Neill et al. showed no P16 expression difference among STUMP and usual leiomyoma variants [15]. Bodner-Adler found out that the presentation of P16 in STUMP resembled that of leiomyoma cases and differed from leiomyosarcoma [40]. Similarly in another study, one out of three STUMPs and 20/21 leiomyosarcoma cases and none of leiomyoma cases had positive P16 [43]. Atkins et al. observed that P16 was diffusely positive in three out of eight STUMPs [16].
According to several studies, expression of P16 and P53 was associated with higher recurrence rate and more aggressive tumor behavior [11, 26, 36]. Travaglino et al. found the abnormal expression of p53 and/or p16, suggesting a risk of recurrence more than 50%; however, in normal expression of them the risk of recurrence was less than 10% [42].
Bcl-2 protein is the product of apoptosis-inhibiting gene which prevents the normal process of apoptotic cell death and also reduces the requirements of growth factors in cell replication, so it promotes the cell replication [13]. Bcl-2 was positive in 16/21 STUMP cases and 10/24 leiomyoma cases. Therefore, our results revealed a statistically significant difference between the STUMP and leiomyoma groups regarding Bcl-2 (p-value = 0.03). Thus, we suggest positivity of Bcl-2 with more than 45% intensity could be useful in distinguishing STUMP (sensitivity: 43%, specificity: 96%). In contrast to ours, several studies revealed that presentation of Bcl-2 was more frequent and stronger in leiomyoma cases in comparison to STUMP and leiomyosarcoma [16, 18, 29, 37]. However, it can be used as a good prognostic marker to distinguish benign and malignant smooth muscle tumors. Despite the differences in presentation of Bcl-2 in leiomyosarcoma, leiomyoma and STUMP cases, it cannot be an exclusive diagnostic tool in this field.
Conclusion
The category and management of STUMP continues to progress. The diagnosis for STUMP mainly depends on the histopathological manifestations. No single IHC marker such as P53, P16, and Bcl-2 has proved robust enough in separating STUMP from other leiomyoma variants; however, according to our study, we suggest combined use of P16 and Bcl-2 (cut off 2.5 and 45%, respectively) to distinguish the equivocal cases of STUMP that are larger than 5 cm with at least moderate atypia and hyaline necrosis.
Availability of data and materials
All data generated or analyzed during this study are included in this published article.
Abbreviations
- AUB:
-
Abnormal uterine bleeding
- BSO:
-
Bilateral sal**ectomy
- IHC:
-
Immunohistochemistry
- LDH:
-
Lactate dehydrogenase
- PMHx:
-
Past medical history
- STUMP:
-
Smooth muscle tumors of uncertain malignant potential
- TAH:
-
Trans-abdominal hysterectomy
- USO:
-
Unilateral sal**ectomy
References
Yordanov AD, Tantchev L, Vasileva P, Strashilov S, Vasileva-Slaveva M, Konsoulova A. Uterine smooth muscle tumours of uncertain malignant potential: single-centre experience and review of the literature. Prz Menopauzalny. 2020;19(1):30–4.
Picerno TM, Wasson MN, Gonzalez Rios AR, Zuber MJ, Taylor NP, Hoffman MK, et al. Morcellation and the incidence of Occult Uterine Malignancy: A Dual-Institution Review. Int J Gynecol Cancer. 2016;26(1):149–55.
Giuliani E, As-Sanie S, Marsh EE. Epidemiology and management of uterine fibroids. Int J Gynaecol Obstet. 2020;149(1):3–9.
Stewart EA, Cookson CL, Gandolfo RA, Schulze-Rath R. Epidemiology of uterine fibroids: a systematic review. BJOG. 2017;124(10):1501–12.
Jang TK, Kwon SH, Cho CH, Lee HW, Shin SJ. Giant uterine mass with uterine smooth muscle tumor of uncertain malignant potential: a case report. Gynecol Oncol Rep. 2020;34:100663.
Porter AE, Kho KA, Gwin K. Mass lesions of the myometrium: interpretation and management of unexpected pathology. Curr Opin Obstet Gynecol. 2019;31(5):349–55.
Bell SW, Kempson RL, Hendrickson MR. Problematic uterine smooth muscle neoplasms. A clinicopathologic study of 213 cases. Am J Surg Pathol. 1994;18(6):535–58.
Cree IA. WHO Classification of Tumours, Female Genital tumours; 5th ed. 2020. 4:279 – 80.
Gupta M, Laury AL, Nucci MR, Quade BJ. Predictors of adverse outcome in uterine smooth muscle tumours of uncertain malignant potential (STUMP): a clinicopathological analysis of 22 cases with a proposal for the inclusion of additional histological parameters. Histopathology. 2018;73(2):284–98.
Ip PP, Tse KY, Tam KF. Uterine smooth muscle tumors other than the ordinary leiomyomas and leiomyosarcomas: a review of selected variants with emphasis on recent advances and unusual morphology that may cause concern for malignancy. Adv Anat Pathol. 2010;17(2):91–112.
Gadducci A, Zannoni GF. Uterine smooth muscle tumors of unknown malignant potential: a challenging question. Gynecol Oncol. 2019;154(3):631–7.
Rizzo A, Ricci AD, Saponara M, Perrone ADEL. Recurrent uterine smooth-muscle tumors of Uncertain Malignant potential (STUMP): state of the art. Anticancer Res. 2020;40(3):1229–38.
Manxhuka-Kerliu S, Kerliu-Saliu I, Sahatciu-Meka V, Kerliu L, Shahini L. Atypical uterine leiomyoma: a case report and review of the literature. J Med Case Rep. 2016;10:22.
Conconi D, Chiappa V, Perego P, Redaelli S, Bovo G, Lavitrano M, et al. Potential role of BCL2 in the recurrence of uterine smooth muscle tumors of uncertain malignant potential. Oncol Rep. 2017;37(1):41–7.
O’Neill CJ, McBride HA, Connolly LE, McCluggage WG. Uterine leiomyosarcomas are characterized by high p16, p53 and MIB1 expression in comparison with usual leiomyomas, leiomyoma variants and smooth muscle tumours of uncertain malignant potential. Histopathology. 2007;50(7):851–8.
Atkins KA, Arronte N, Darus CJ, Rice LW. The Use of p16 in enhancing the histologic classification of uterine smooth muscle tumors. Am J Surg Pathol. 2008;32(1):98–102.
Hewedi IH, Radwan NA, Shash LS. Diagnostic value of progesterone receptor and p53 expression in uterine smooth muscle tumors. Diagn Pathol. 2012;7:1.
Rubisz P, Ciebiera M, Hirnle L, Zgliczyńska M, Łoziński T, Dzięgiel P et al. The usefulness of immunohistochemistry in the Differential diagnosis of Lesions originating from the myometrium. Int J Mol Sci. 2019;20(5):1136.
Valenzuela C. 2 solutions for estimating odds ratios with zeros. Rev Med Chil. 1993;121(12):1441–4.
Di Giuseppe J, Grelloni C, Giuliani L, Delli Carpini G, Giannella L, Ciavattini A. Recurrence of uterine smooth muscle tumor of Uncertain Malignant potential: a systematic review of the literature. Cancers (Basel). 2022;14(9):2323.
Vilos GA, Marks J, Ettler HC, Vilos AG, Prefontaine M, Abu-Rafea B. Uterine smooth muscle tumors of uncertain malignant potential: diagnostic challenges and therapeutic dilemmas. Report of 2 cases and review of the literature. J Minim Invasive Gynecol. 2012;19(3):288–95.
Russo C, Camilli S, Martire FG, Di Giovanni A, Lazzeri L, Malzoni M, Zupi E, Exacoustos C. Ultrasound features ofhighly vascularized uterine myomas (uterine smooth muscle tumors) and correlation with histopathology. Ultrasound Obstet Gynecol. 2022;60:269–76.
Bonneau C, Thomassin-Naggara I, Dechoux S, Cortez A, Darai E, Rouzier R. Value of ultrasonography and magnetic resonance imaging for the characterization of uterine mesenchymal tumors. Acta Obstet Gynecol Scand. 2014;93(3):261–8.
Bolan C, Caserta MP. MR imaging of atypical fibroids. Abdom Radiol 2016;41(12):2332–49.
Ip PP, Cheung AN, Clement PB. Uterine smooth muscle tumors of uncertain malignant potential (STUMP): a clinicopathologic analysis of 16 cases. Am J Surg Pathol. 2009;33(7):992–1005.
Ng JS, Han A, Chew SH, Low J. A clinicopathologic study of uterine smooth muscle tumours of uncertain malignant potential (STUMP). Ann Acad Med Singap. 2010;39(8):625–8.
Bacanakgil BH, Deveci M, Karabuk E, Soyman Z. Uterine smooth muscle tumor of Uncertain Malignant potential: clinicopathologic-sonographic characteristics, Follow-Up and recurrence. World J Oncol. 2017;8(3):76–80.
Guntupalli SR, Ramirez PT, Anderson ML, Milam MR, Bodurka DC, Malpica A. Uterine smooth muscle tumor of uncertain malignant potential: a retrospective analysis. Gynecol Oncol. 2009;113(3):324–6.
Deodhar KK, Goyal P, Rekhi B, Menon S, Maheshwari A, Kerkar R, et al. Uterine smooth muscle tumors of uncertain malignant potential and atypical leiomyoma: a morphological study of these grey zones with clinical correlation. Indian J Pathol Microbiol. 2011;54(4):706–11.
Canciani GN, Burbos N, Duncan TJ, Lonsdale R, Nieto JJ. Late presentation of metastatic smooth muscle neoplasm of the uterus with low malignant potential. J Gynecol Oncol. 2012;23(1):69–71.
Shapiro A, Ferenczy A, Turcotte R, Bruchim I, Gotlieb WH. Uterine smooth-muscle tumor of uncertain malignant potential metastasizing to the humerus as a high-grade leiomyosarcoma. Gynecol Oncol. 2004;94(3):818–20.
Tossamartvorakul M, Mendoza M, Huang KG, Chang SH. Metastatic smooth muscle tumor of Uncertain Malignant potential after laparoscopic presuming myomectomy. Gynecol Minim Invasive Ther. 2021;10(3):187–90.
Song KJ, Yu XN, Lv T, Chen YL, Diao YC, Liu SL, et al. Expression and prognostic value of lactate dehydrogenase-A and -D subunits in human uterine myoma and uterine sarcoma. Med (Baltim). 2018;97(14):e0268.
Zhang F, Liu Y, Quan Q, Meng Y, Mu X. Diagnostic value of preoperative CA125, LDH and HE4 for Leiomyosarcoma of the female Reproductive System. Cancer Manag Res. 2021;13:4657–64.
Matsuda M, Ichimura T, Kasai M, Murakami M, Kawamura N, Hayashi T, et al. Preoperative diagnosis of usual leiomyoma, atypical leiomyoma, and leiomyosarcoma. Sarcoma. 2014;2014:498682.
Huo L, Wang D, Wang W, Cao D, Yang J, Wu M, et al. Oncologic and reproductive outcomes of uterine smooth muscle tumor of uncertain malignant potential: a single center retrospective study of 67 cases. Front Oncol. 2020;10:647.
Zhang Q, Ubago J, Li L, Guo H, Liu Y, Qiang W, et al. Molecular analyses of 6 different types of uterine smooth muscle tumors: emphasis in atypical leiomyoma. Cancer. 2014;120(20):3165–77.
Arleo EK, Schwartz PE, Hui P, McCarthy S. Review of Leiomyoma variants. AJR Am J Roentgenol. 2015;205(4):912–21.
Patel V, **ng D, Feely M, Schoolmeester JK. Smooth muscle tumors of the visceral adnexal and uterine ligaments and Adnexal Connective tissue: a clinicopathologic study of 67 cases. Int J Gynecol Pathol. 2020;39(1):55–67.
Bodner-Adler B, Bodner K, Czerwenka K, Kimberger O, Leodolter S, Mayerhofer K. Expression of p16 protein in patients with uterine smooth muscle tumors: an immunohistochemical analysis. Gynecol Oncol. 2005;96(1):62–6.
Dastranj Tabrizi A, Ghojazadeh M, Thagizadeh Anvar H, Vahedi A, Naji S, Mostafidi E, et al. Immunohistochemical Profile of Uterine Leiomyoma with bizarre nuclei; comparison with conventional leiomyoma, smooth muscle tumors of Uncertain Malignant potential and Leiomyosarcoma. Adv Pharm Bull. 2015;5(5):683–7. 2015/12/31.
Travaglino A, Raffone A, Gencarelli A, Neola D, Oliviero DA, Alfano R, et al. p53, p16 and ki67 as immunohistochemical prognostic markers in uterine smooth muscle tumors of uncertain malignant potential (STUMP). Pathol Res Pract. 2021;226:153592.
Ünver NU, Acikalin MF, Öner Ü, Ciftci E, Ozalp SS, Colak E. Differential expression of P16 and P21 in benign and malignant uterine smooth muscle tumors. Arch Gynecol Obstet. 2011;284(2):483–90.
Acknowledgements
The authors would like to thank Shiraz University of Medical Sciences, Shiraz, Iran and also Center for Development of Clinical Research of Nemazee Hospital and Dr. Nasrin Shokrpour for editorial assistance.
Funding
This article was extracted from the thesis written by Nafiseh Todarbary and was financially supported by Research Dean of Shiraz University of Medical Sciences grants No.22538.
Author information
Authors and Affiliations
Contributions
MAJ, FSA and FN designed and MAJ conducted the study. MAJ and FA reviewed pathology slides. MZ analysed and interpreted the patients’ data. FA and NT contributed in writing and editing the manuscript. FA and MAJ read and approved the final manscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Akbarzadeh-Jahromi, M., Todarbary, N., Aslani, F.S. et al. Uterine smooth muscle tumors of uncertain malignant potential: a retrospective evaluation of clinical pathology and immunohistochemistry features. Surg Exp Pathol 7, 2 (2024). https://doi.org/10.1186/s42047-024-00145-5
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s42047-024-00145-5