Abstract
Background
Breast cancer is estimated to comprise about 290,560 new cases in 2022. Aromatase inhibitors (AIs) are recommended as adjuvant treatment for estrogen-receptor positive (ER+) breast carcinoma in postmenopausal women, which includes approximately two-thirds of all women with breast cancer. AIs inhibit the peripheral conversion of androgens to estrogen by deactivation of the aromatase enzyme, leading to a reduction in serum estrogen level in postmenopausal women with ER+ breast carcinoma. Estrogen is known for its cardiovascular (CV) protective properties through a variety of mechanisms including vasodilation of blood vessels and inhibition of vascular injury resulting in the prevention of atherosclerosis. In clinical trials and prospective cohorts, the long-term use of AIs can increase the risk for hypertension and hyperlipidemia. Studies demonstrate mixed results as to the impact of AIs on actual CV events and overall survival.
Methods
A single arm longitudinal study of 14 postmenopausal women with ER+ breast cancer prescribed adjuvant AIs at the University of Minnesota (UMN). Subjects with a history of known tobacco use, hypertension, hyperlipidemia, and diabetes were excluded to eliminate potential confounding factors. Participants underwent routine labs, blood pressure assessments, and vascular testing at baseline (prior to starting AIs) and at six months. Vascular assessment was performed using the EndoPAT 2000 and HDI/PulseWave CR-2000 Cardiovascular Profiling System and pulse contour analysis on two occasions as previously described. Vascular measurements were conducted by one trained vascular technician. Assessments were performed in triplicate, and the mean indices were used for analyses. All subjects were on an AI at the follow-up visit. The protocol was approved by the UMN Institutional Review Board and all participants were provided written informed consent. Baseline and follow-up characteristics were compared using Wilcoxon signed-rank tests. Analyses were performed using R version 3.6.1 (R Foundation for Statistical Computing, Vienna, Austria).
Results
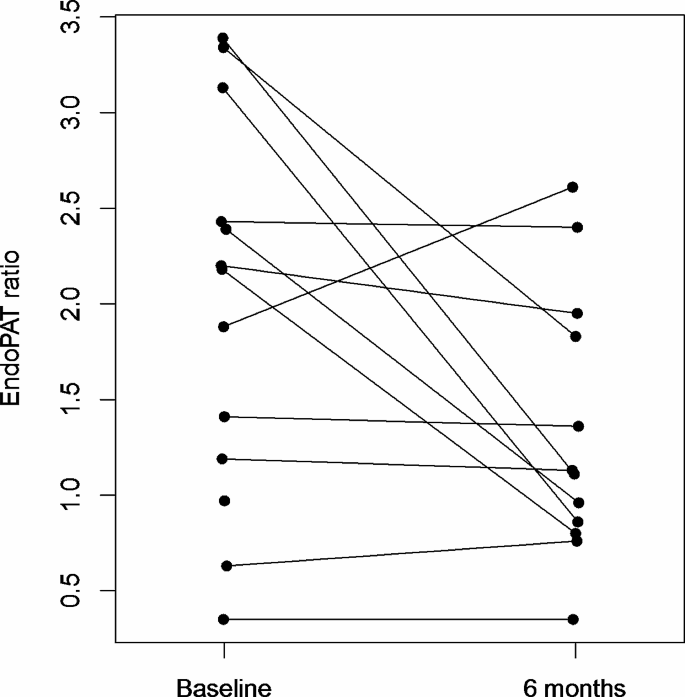
After six months of AI treatment, EndoPAT® ratio declined to a median 1.12 (Q1: 0.85, Q3: 1.86; p = 0.045; Figure 1) and median estradiol levels decreased to 2 pg/mL (Q1: 2, Q3: 3; p=0.052). There was no evidence of association between change in EndoPAT® and change in estradiol level (p = 0.91). There were no statistically significant changes in small or large arterial elasticity.
Conclusions
We hypothesize that long-term use of AI can lead to persistent endothelial dysfunction, and further investigation is necessary. In our study, patients were on AI for approximately 5-10 years. As a result, we do not have data on whether these changes, such as EndoPAT® ratio and the elasticity of small and large arterial, are reversible with discontinuation of AI. These findings set the stage for a larger study to more conclusively determine the association between AI exposure and cardiovascular outcomes. Further studies should evaluate for multivariate associations withmodifiable risk factors for CV disease.
Similar content being viewed by others
Background
Breast cancer is estimated to comprise about 290,560 new cases in 2022 [1]. Aromatase inhibitors (AIs) are recommended as adjuvant treatment for estrogen-receptor positive (ER+) breast carcinoma in postmenopausal women, which includes approximately two-thirds of all women with breast cancer [2].
AIs inhibit the peripheral conversion of androgens to estrogen by deactivation of the aromatase enzyme, leading to a reduction in serum estrogen level in postmenopausal women with ER + breast carcinoma [3,4,5]. Estrogen is known for its cardiovascular (CV) protective properties through a variety of mechanisms including vasodilation of blood vessels and inhibition of vascular injury resulting in the prevention of atherosclerosis [6]. In clinical trials and prospective cohorts, the long-term use of AIs can increase the risk for hypertension and hyperlipidemia. Studies demonstrate mixed results as to the impact of AIs on actual CV events and overall survival [7, 8].
We hypothesized that the use of AIs and the associated reduction in estrogen would result in endothelial dysfunction, a predictor of early CV disease in women with breast cancer. Endothelial dysfunction, identified by reactive hyperemia using Endo-PAT, a non-invasive device that measures arterial vasoreactivity by assessing the peripheral arterial tone (Zoll Itamar), has been associated with an increased risk of CV events, independent of the Framingham risk score [9]. With the rising number of pre- and postmenopausal women on AIs for five to ten years, understanding the long-term impact of AIs on blood vessels and CV risk in cancer survivors is vital.
EndoPAT 2000
EndoPAT 2000, developed by Zoll Itamar, is a U.S. Food & Drug Administration approved non-invasive device that utilizes peripheral arterial tonometry (PAT) to measure pulse wave amplitude (PWA) abnormalities in response to hyperemia vasoreactivity [10, 11]. PWA abnormalities have been previously studied and found to be associated with endothelial dysfunction and CV disease [10, 12, 13].
Methods
We conducted a single arm longitudinal study of 14 postmenopausal women with ER + breast cancer prescribed adjuvant AI at the University of Minnesota (UMN). Subjects with a history of known tobacco use, hypertension, hyperlipidemia, and diabetes were excluded to eliminate potential confounding factors. Participants underwent routine labs, blood pressure assessments, and vascular testing at baseline (prior to starting AIs) and at six months. Vascular assessment was performed using the EndoPAT 2000 and HDI/PulseWave CR-2000 Cardiovascular Profiling System (Hypertension Diagnostic Inc., Eagan, MN) and pulse contour analysis on two occasions as previously described [14]. Vascular measurements were conducted by one trained vascular technician (NF). Assessments were performed in triplicate, and the mean indices were used for analyses. Biomarkers were obtained using a fasting blood draw to evaluate lipids, total cholesterol (TC), low-density lipoprotein cholesterol (LDL), high-density lipoprotein cholesterol (HDL), triglycerides (TG), high sensitivity CRP (hsCRP), serum glucose, 17-betaestradiol (estradiol), von Willebrand factor, tissue plasminogen activator, and plasminogen activator inhibitor-1. All subjects were on an AI at the follow-up visit. The protocol was approved by the UMN Institutional Review Board and all participants were provided written informed consent. Baseline and follow-up characteristics were compared using Wilcoxon signed-rank tests. Analyses were performed using R version 3.6.1 (R Foundation for Statistical Computing, Vienna, Austria).
Results
Nine (64.3%) of the 14 participants had stage I breast cancer, four (28.6%) had stage II disease, and one (7.1%) had stage III disease. All fourteen received neoadjuvant or adjuvant chemotherapy. Ten (71.4%) participants received radiation therapy (four left-sided, six right-sided). Anastrozole was the most commonly used AI (6; 42.9%) followed by letrozole (5; 35.7%) and exemestane (3; 21.4%). None of the participants were on tamoxifen.
Patient characteristics and outcomes are outlined in Table 1. All patients were postmenopausal women. A total of 20 patients met inclusion criteria; however, only 14 patients who had follow-up visits were included in the analyses. Median baseline age of participants was 58 years (1st quartile [Q1]: 56, 3rd quartile [Q3]: 60) and median baseline body mass index was 26.5 kg/m2 (Q1: 24.4, Q3: 31.6). Median systolic and diastolic blood pressure was 120 (Q1: 115, Q3: 124) and 70 (Q1: 61, Q3: 73) mm/Hg, respectively, and total cholesterol 228 mg/dL (Q1: 202, Q3: 244). Median baseline ultrasensitive estradiol level was 7 pg/mL (Q1: 4, Q3: 15) and hsCRP was 2.45 mg/L (Q1: 1.14, Q3: 6.07). Prior to AI therapy, EndoPAT ratio was 2.18 (Q1: 1.19, Q3: 2.43). Median baseline small arterial elasticity and large arterial elasticity was 4.1 mL/mmHg x100 (Q1: 3.2, Q3: 6.1) and 12.4 mL/mmHg x10 (Q1: 10.4, Q3: 14.2), respectively.
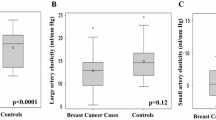
After six months of AI treatment, EndoPAT® ratio declined to a median 1.12 (Q1: 0.85, Q3: 1.86; p = 0.045; Fig. 1) and median estradiol levels decreased to 2 pg/mL (Q1: 2, Q3: 3; p = 0.052). There was no evidence of an association between change in EndoPAT® and change in estradiol level (p = 0.91). There were no statistically significant changes in small arterial elasticity, which at 6 months was 4.3 mL/mmHg x100 (Q1: 4.0, Q3: 5.7) or large arterial elasticity, which at 6 months was 14.1 mL/mmHg x 10 (Q1: 11.0, Q3: 17.2). There were no statistically significant differences in serum glucose, TC, LDL, HDL, nor hsCRP at 6 months compared to baseline. hsCRP remained elevated at median 2.98 mg/L. Biomarkers of von Willebrand factor, tissue plasminogen activator, and plasminogen activator inhibitor-1 did not change over time.
EndoPAT ratio measurements at baseline and 6 months with those from the same woman connected. Figure 1: Of the 14 women, one did not have EndoPAT ratios measured and one was missing the EndoPAT ratio at 6-month follow-up
Discussion
Endovascular dysfunction is an early sign for atherosclerosis and vascular impairment; therefore, measuring endovascular dysfunction using flow-mediated dilation or EndoPAT helps identify patients who may be at risk for CV events [9, 14]. Our EndoPAT pilot study suggests that postmenopausal breast cancer survivors on AIs therapy develop endothelial dysfunction, a predictor of adverse CV disease. These changes develop while on AIs, correlating with a decline in estradiol levels.
Large clinical studies report higher rates of hypertension, hypercholesterolemia, and ischemic CV disease in postmenopausal breast cancer survivors receiving AIs [7, 8, 15]. The Long Island Breast Cancer study demonstrated increased CV deaths and decreased survival after seven years of treatment with AI [15]; this study, however, did not differentiate whether findings were related to secondary causes such as the development of hypertension, hypercholesterolemia, or directly related to AI therapy. A more recent retrospective cohort of 15,815 breast cancer patients diagnosed 2006–2012 demonstrated an increase in heart failure in those treated over the age of 75 years when treated with an AI compared to tamoxifen. The risk of ischemic heart disease increased in those who took AIs for at least four years (hazard ratio (HR): 2.12; 95% CI: 1.40–3.25) compared to those who took no or had short term exposure to AI [8]. In the study cohort of the UK Clinical Practice Research Datalink of 17,922 breast cancer patients treated with AI, there was an increase in heart failure risk (HR: 1.86; 95% CI: 1.14–3.03) and CV mortality (HR: 1.50; 95% CI: 1.11–2.04) in those treated with AI compared to tamoxifen [7]. Contrarily, a randomized double blinded study compared anastrozole to placebo did not show an increase risk for CV events [16].
CV disease development is multifactorial due to risk factors such as aging, hypertension, hyperlipidemia and tobacco use. This development often begins with endothelial dysfunction and which ultimately leads to atherosclerosis and ischemic events. Inflammation, fibrosis, and estrogen depletion can lead to changes in the endothelium [6, 17, 18]. In this study, treatment of postmenopausal breast cancer with AI was associated with increased endothelial dysfunction, which coincided within six months of starting the medication and declines in estrogen. This finding is significantly lower than the 1.67 EndoPAT level which was previously linked to higher CV events by Shechter et al. [19]. Our prior work also demonstrated higher rates of impaired endothelial function compared with healthy postmenopausal controls [14]. There was a suggestion endothelial changes were associated with a decline in estrogen levels; however, this did not meet statistical significance [14]. Markers of inflammation (hsCRP) remained persistent; other biomarker work did not suggest the etiology of these changes [14].
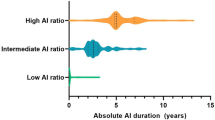
Given the high prevalence of breast cancer and recommendations for extended use of AIs in postmenopausal women, it is important to investigate further the risk of CV disease development due to AI use as prior studies have been inconclusive. Additionally, with further reductions in estrogen in premenopausal women, where ovarian suppression plus AI is often recommended, understanding the long-term implications of this treatment regimen on overall cardiac health is imperative. In the current literature, few studies have shown the correlation between estrogen levels and endothelial dysfunction. Luca et al. reported study results of ten premenopausal women who showed that estradiol serum levels were inversely proportional to endothelial dysfunction and subsequent CV events by measuring flow-mediated dilation [16]. Given our work, and prior published work, we hypothesize that long-term use of AI can lead to persistent endothelial dysfunction, and further investigation is necessary. In our study, patients were on AI for approximately 5–10 years. As a result, we do not have data on whether these changes, such as EndoPAT® ratio and the elasticity of small and large arterial, are reversible with discontinuation of AI.
Conclusion and limitations
This study has a few limitations. It is a pilot study, and as such, has a small sample size. Additionally, the population was predominantly Caucasian, limiting the generalizability. This study was designed to detect AI-specific risk because subjects with a known major risk factors such as tobacco use, hypertension, or hyperlipidemia were excluded. These findings set the stage for a larger study to more conclusively determine the association between AI exposure and cardiovascular outcomes. Further studies should evaluate for multivariate associations with modifiable risk factors for CV disease.
Postmenopausal breast cancer survivors prescribed AIs develop endothelial dysfunction, a predictor of adverse CV disease. Understanding the exact mechanisms through further detailed biomarker research long-term, along with potential interventions, such as modifications of CV risk factors, to mitigate these effects is necessary and warrants further investigation.
Data availability
The datasets used and/or analyzed during the current study are available from the corresponding author on request.
Abbreviations
- AI:
-
Aromatase inhibitors
- ER +:
-
Estrogen-receptor positive
- CV:
-
Cardiovascular
- CRP:
-
C-reactive protein
- HDL:
-
High-density lipoprotein cholesterol
- HR:
-
Hazard Ratio
- LDL:
-
Low-density lipoprotein cholesterol
- TC:
-
Total cholesterol
- TG:
-
Triglycerides
- tPA:
-
Tissue-type plasminogen activator
- PA-1:
-
Plasminogen-activator 1
- PAT:
-
Peripheral arterial tonometry
- PWA:
-
Pulse wave amplitude
- tPA:
-
Tissue-type plasminogen activator
- Q:
-
Quartile
- UMN:
-
University of Minnesota
References
Miller KD, Nogueira L, Mariotto AB et al. Cancer treatment and survivorship statistics, 2019. CA Cancer J Clin. 2019.
Cuzick J, Sestak I, Baum M, et al. Effect of anastrozole and tamoxifen as adjuvant treatment for early-stage breast cancer: 10-year analysis of the ATAC trial. Lancet Oncol. 2010;11(12):1135–41.
Brueggemeier RW, et al. Aromatase inhibitors in the treatment of breast cancer. Endocr Reviews vol. 2005;26(3):331–45. https://doi.org/10.1210/er.2004-0015.
Adhikari N, et al. Combating breast cancer with non-steroidal aromatase inhibitors (NSAIs): understanding the chemico-biological interactions through comparative SAR/QSAR study. Eur J Med Chem. 2017;137:365–438. https://doi.org/10.1016/j.ejmech.2017.05.041.
Smith IE, Dowsett M. Aromatase inhibitors in breast cancer. New Engl J Med vol. 2003;348:2431–42. https://doi.org/10.1056/NEJMra023246.
Meyer MR, Barton M. Estrogens and Coronary Artery Disease: New Clinical perspectives. Adv Pharmacol. 2016;77:307–60.
Khosrow-Khavar F, Filion KB, Bouganim N, Suissa S, Azoulay L. Aromatase inhibitors and the risk of Cardiovascular outcomes in women with breast Cancer: a Population-based Cohort Study. Circulation. 2020;141(7):549–59.
Sund M, Garcia-Argibay M, Garmo H, et al. Aromatase inhibitors use and risk for cardiovascular disease in breast cancer patients: a population-based cohort study. Breast. 2021;59:157–64.
Rubinshtein R, Kuvin JT, Soffler M, et al. Assessment of endothelial function by non-invasive peripheral arterial tonometry predicts late cardiovascular adverse events. Eur Heart J. 2010;31(9):1142–8.
Axtell AL, et al. Assessing endothelial vasodilator function with the Endo-PAT 2000. J Visualized Experiments: JoVE. 2010;44. https://doi.org/10.3791/2167. 2167. 15 Oct.
Zoll. itamar. https://www.itamar-medical.com/professionals/endopat/. Accessed on 3/28/2024.
Kuvin JT, et al. Assessment of peripheral vascular endothelial function with finger arterial pulse wave amplitude. Am Heart J vol. 2003;146(1):168–74. https://doi.org/10.1016/S0002-8703(03)00094-2.
Hedblad B, et al. Low pulse-wave amplitude during reactive leg hyperaemia: an independent, early marker for ischaemic heart disease and death. Results from the 21-year follow-up of the prospective cohort study ‘Men born in 1914’, Malmö, Sweden. J Intern Med vol. 1994;236(2):161–8. https://doi.org/10.1111/j.1365-2796.1994.tb01278.x.
Blaes A, Beckwith H, Florea N et al. Vascular function in breast cancer survivors on aromatase inhibitors: a pilot study. Breast Cancer Res Treat. 2017.
Bradshaw PT, Stevens J, Khankari N, Teitelbaum SL, Neugut AI, Gammon MD. Cardiovascular Disease Mortality among breast Cancer survivors. Epidemiology. 2016;27(1):6–13.
Luca MC, Liuni A, Harvey P, Mak S, Parker JD. Effects of estradiol on measurements of conduit artery endothelial function after ischemia and reperfusion in premenopausal women. Can J Physiol Pharmacol. 2016;94(12):1304–8.
Lew R, Komesaroff P, Williams M, Dawood T, Sudhir K. Endogenous estrogens influence endothelial function in young men. Circul Res. 2003;93(11):1127–33.
Shechter M, Matetzky S, Prasad M, Goitein O, Goldkorn R, Naroditsky M, Koren-Morag N, Lerman A. Endothelial function predicts 1-year adverse clinical outcome in patients hospitalized in the emergency department chest pain unit. Int J Cardiol. 2017;240:14–9. Epub 2017 May 1. PMID: 28477961.
Cuzick J, Sestak I, Forbes JF, Dowsett M, Cawthorn S, Mansel RE, Loibl S, Bonanni B, Evans DG, Howell A. IBIS-II investigators. Use of anastrozole for breast cancer prevention (IBIS-II): long-term results of a randomised controlled trial. Lancet. 2020;395(10218):117–122. doi: 10.1016/S0140-6736(19)32955-1. Epub 2019 Dec 12. Erratum in: Lancet. 2020;395(10223):496. Erratum in: Lancet. 2021;397(10276):796. PMID: 31839281; PMCID: PMC6961114.
Acknowledgements
Not applicable.
Funding
K12-HD055887, P30-CA77598, UL1TR002494.
Author information
Authors and Affiliations
Contributions
AS served as primary investigator and wrote majority of the manuscript. AP: Study statistician, helped in interpretation of data and generation of tables and figures. HB: All other co-authors helped the primary investigator in editing and writing the final draft for the manuscript. AB: Corresponding author had a major role in interpreting data and writing manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Shaaban, A., Petersen, A., Beckwith, H. et al. Endothelial dysfunction in breast cancer survivors on aromatase inhibitors: changes over time. Cardio-Oncology 10, 27 (2024). https://doi.org/10.1186/s40959-024-00227-z
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s40959-024-00227-z