Abstract
Background
Chronic diarrhea is a common disease causing morbidity and mortality of captive rhesus macaques (RMs, Macaca mulatta). Chronic diarrhea in RMs is typically characterized by long-term diarrhea and a weak response to antibiotic treatment. Diarrhea is also a common disease in humans and can cause death. However, the etiology of about half of diarrheal cases of humans is still unclear. Therefore, we performed shotgun metagenomic sequencing to characterize the differences in the gut microbiome and resistome of chronic diarrhea RMs and asymptomatic individuals.
Results
Our results showed Lactobacillus spp. (mainly L. johnsonii, L. reuteri and L. amylovorus) were significantly depleted in chronic diarrhea RM guts compared to asymptomatic individuals (5.2 vs 42.4%). Functional annotation of genes suggested these Lactobacillus spp. carried genes involved in the adhesion of intestinal epithelial cells and production of bacteriocin. Chronic diarrhea RM guts also had a significantly greater abundance of many other gut bacteria, including mucin-degrading bacteria and opportunistic pathogens. The metabolic pathways of chronic diarrhea RM gut microbiome were enriched in aerobactin biosynthesis, while the metabolic pathways of asymptomatic RM gut microbiome were enriched in the production of short-chain fatty acids (SCFAs). Chronic diarrhea RM guts had a significantly greater abundance of antibiotic resistance genes (ARGs), such as ermF, aph(3’)-IIIa, ermB, and floR. The strains isolated from feces and tissue fluid of chronic diarrhea RMs had higher resistance rates to the majority of tested antibiotics, but not cephamycin and carbapenem antibiotics. Gut microbial composition comparisons showed that several captive nonhuman primate (NHP) guts were more similar to the guts of humans with a non-westernized diet than humans with a westernized diet. Chronic diarrhea RM gut microbiome was strikingly similar to rural-living humans with diarrhea and humans with a non-westernized diet than asymptomatic RMs.
Conclusions
Our results suggested chronic diarrhea significantly altered the composition and metabolic pathways of the RM gut microbiome. The frequent use of antibiotics caused antibiotic resistance in chronic diarrhea RM gut microbiome with serious consequences for individual treatment and survival. The findings of this study will help us to improve the effective prevention and treatment of diarrhea in RMs.
Video Abstract
Similar content being viewed by others
Background
Chronic diarrhea is a common disease of captive rhesus macaques (RMs, Macaca mulatta) [1, 2]. Chronic diarrhea in RMs is often manifested by chronic inflammatory response of the colon, and long-term and recurrent diarrhea, yet there has been no specific pathogen identified and antibiotics treatment is frequently ineffective [3]. Chronic diarrhea in RMs can cause dehydration, malnutrition, growth retardation, weight loss, weak immune response, and even death, resulting in great losses of captive RM breeding potential [2, 4]. This diarrheal disease of humans is also one of the most widespread diseases across the world, which threatens human health and is a particular threat for children who experience higher morbidity and mortality [5,6,7]. Compared to developed countries, the incidence rate of diarrhea is higher in develo** countries due to poor hygiene and sanitation [7, 8]. However, the etiology of about half of human diarrheal cases cannot be clearly defined [97]. Nevertheless, the opposite dietary features shaped the different gut microbiome [97]. Since captive NHPs have a similar diet to humans with a non-westernized diet, this might highly influence the similarities in gut microbiome between captive NHPs and humans with a non-westernized diet [96, 98, 99]. However, the human gut microbiome was not consistently similar across all NHP species, with the captive P. troglodytes gut microbiome being most similar to the gut microbiome of humans. This higher similarity in gut microbiome composition may be due to the closer phylogeny and similar diet [100, 101].
Although the symptoms of chronic diarrhea of RMs are similar to UC disease in humans [30], the gut microbiome compositions of them were obviously different in our study. The differences may be caused by these humans with UC disease consuming a westernized diet, because the gut microbiome of RMs was more similar to humans with a non-westernized diet than humans with a westernized diet. We did not collect samples of the humans with IBD consuming a non-westernized diet, but we found that the gut microbiome of chronic diarrhea RMs was more similar to rural diarrheal humans and humans with a non-westernized diet. Therefore, due to more similarities in gut microbiomes, chronic diarrhea RMs could be more suitable models in diarrheal research of rural dwellers or humans with a non-westernized diet.
The frequent use of antibiotics has resulted in antibiotic selection pressure causing the prevalence of antibiotic resistance bacteria [102]. We found that there were most abundant tetracycline ARG in RM guts and most isolates from RM guts were resistant to tetracycline. Although tetracycline antibiotics were not used in the treatment of diarrhea of RMs, long-term and widespread use of tetracycline antibiotics has caused an extensive global tetracycline resistance [103]. Bacteroides spp. are reportedly the main carriers of the tetQ gene [104, 105]. Therefore, a prevalence of tetQ in RM guts might be due to abundant Bacteroides. Similarly, the widespread aminoglycoside ARGs in the chronic diarrhea RM gut microbiome may have resulted from the use of aminoglycoside antibiotics, and it also led to a high resistance rate to kanamycin. The use of florfenicol antibiotics may have caused a high abundance of floR in the guts of RMs [106]. Therefore, abundant ARGs in the guts of chronic diarrhea RMs may be strongly associated with the frequent use of antibiotics.
The testing of resistant phenotypes of isolates further demonstrated serious antibiotic resistance of chronic diarrhea RMs gut microbiome. Not only was there a high abundance of ARG in the gut microbiome of chronic diarrhea RMs, but these RM guts also had high antibiotic resistance rates within isolates. These isolates from chronic diarrhea RMs generally had higher antibiotic resistance rates to florfenicol, tetracycline, aminoglycoside, quinolone, and cephalosporin antibiotics according to our susceptibility testing. Most of these antibiotics were used in previous treatments of diarrhea. Therefore, a directed use of antibiotics in the treatment of diarrheal RMs is necessary to avoid more serious antibiotic resistance. It is worth noting that almost all isolates were susceptible to imipenem and cefoxitin. Due to a stronger stabilization compared to other cephalosporins, bacteria usually had low resistance rates to cefoxitin (a type of cephamycin antibiotics) and imipenem (a type of carbapenem antibiotics) [107, 108]. Therefore, cephamycin and carbapenem antibiotics may be effective to treat diarrhea in RMs and provide new treatment protocols. Nonetheless, the use of cephamycin and carbapenem antibiotics still needs to be treated with caution to avoid novel antibiotic resistance. It is also necessary to monitor resistance phenotype(s) of common antibiotic resistance bacteria, such as Escherichia coli, in RM guts and the captive environment. These measures could effectively decrease the emergence and spread of antibiotic resistance in captive RMs.
Conclusions
In conclusion, our results indicated that individuals with chronic diarrhea had significantly different gut microbiomes compared with asymptomatic individuals. We also identified that frequent use of antibiotics caused antibiotic resistance in RM guts, with serious consequences for the treatment of chronic diarrhea. According to our results, beneficial strains of Lactobacillus from RM guts could be regarded as a potential probiotic to prevent or relieve RM diarrhea in future research and treatment. It was necessary to monitor antibiotic resistance of bacteria in RMs’ environments to reduce the propagative risks from ARGs and multidrug-resistant bacteria. Our results also revealed a greater similarity in gut microbial compositions between captive NHPs including RMs and humans with a non-westernized diet. This result suggests that diarrheal RM could be considered a suitable model to research diarrhea in humans with a non-westernized diet. Overall, our results provided a clearer understanding of the gut microbiome and antibiotic resistome of chronic diarrhea RMs.
Availability of data and materials
The data that support the findings of this study have been deposited into the CNGB Sequence Archive (CNSA) of China National GeneBank DataBase (CNGBdb) with accession number CNP0001810.
References
Blackwood RS, Tarara RP, Christe KL, Spinner A, Lerche NW. Effects of the macrolide drug tylosin on chronic diarrhea in rhesus macaques (Macaca mulatta). Comparative Med. 2008;58(1):81–7.
Kanthaswamy S, Elfenbein HA, Ardeshir A, Ng J, Hyde D, Smith DG, et al. Familial aggregation of chronic diarrhea disease (CDD) in rhesus macaques (Macaca mulatta). Am J Primatol. 2014;76(3):262–70.
Westreich ST, Ardeshir A, Alkan Z, Kable ME, Korf I, Lemay DG. Fecal metatranscriptomics of macaques with idiopathic chronic diarrhea reveals altered mucin degradation and fucose utilization. Microbiome. 2019;7(1):41.
Prongay K, Park B, Murphy SJ. Risk factor analysis may provide clues to diarrhea prevention in outdoor-housed rhesus macaques (Macaca mulatta). Am J Primatol. 2013;75(8):872–82.
Prüss-Üstün A, Corvalán C. How much disease burden can be prevented by environmental interventions? Epidemiology. 2007;18(1):167–78.
Alexander KA, Carzolio M, Goodin D, Vance E. Climate change is likely to worsen the public health threat of diarrheal disease in Botswana. Int J Environ Res Public Health. 2013;10(4):1202–30.
Youmans BP, Ajami NJ, Jiang ZD, Campbell F, Wadsworth WD, Petrosino JF, et al. Characterization of the human gut microbiome during travelersʼ diarrhea. Gut Microbes. 2015;6(2):110–9.
Bonkoungou IJO, Haukka K, Osterblad M, Hakanen AJ, Traore AS, Barro N, et al. Bacterial and viral etiology of childhood diarrhea in Ouagadougou, Burkina Faso. BMC Pediatr. 2013;13:36.
Kain KC, Barteluk RL, Kelly MT, **n H, Hua GD, Yuan G, et al. Etiology of childhood diarrhea in Bei**g, China. J Clin Microbiol. 1991;29(1):90–5.
Yu JX, **g HQ, Lai SJ, Xu WB, Li MF, Wu JG, et al. Etiology of diarrhea among children under the age five in China: results from a five-year surveillance. J Infection. 2015;71(1):19–27.
Wilk JL, Maginnis GM, Coleman K, Lewis A, Ogden B. Evaluation of the use of coconut to treat chronic diarrhea in rhesus macaques (Macaca mulatta). J Med Primatol. 2008;37(6):271–6.
Vogt SL, Finlay BB. Gut microbiota-mediated protection against diarrheal infections. Journal of travel medicine. 2017;24(suppl_1):S39–43.
Coyte KZ, Schluter J, Foster KR. The ecology of the microbiome: networks, competition, and stability. Science. 2015;350(6261):663–6.
Ley RE, Hamady M, Lozupone C, Turnbaugh PJ, Ramey RR, Bircher JS, et al. Evolution of mammals and their gut microbes. Science. 2008;320(5883):1647.
Qin J, Li R, Raes J, Arumugam M, Burgdorf KS, Manichanh C, et al. A human gut microbial gene catalogue established by metagenomic sequencing. Nature. 2010;464(7285):59–65.
Human Microbiome Project C. Structure, function and diversity of the healthy human microbiome. Nature. 2012;486(7402):207–14.
Tremaroli V, Backhed F. Functional interactions between the gut microbiota and host metabolism. Nature. 2012;489(7415):242–9.
El Kaoutari A, Armougom F, Gordon JI, Raoult D, Henrissat B. The abundance and variety of carbohydrate-active enzymes in the human gut microbiota. Nat Rev Microbiol. 2013;11(7):497–504.
Rowland I, Gibson G, Heinken A, Scott K, Swann J, Thiele I, et al. Gut microbiota functions: metabolism of nutrients and other food components. Eur J Nutr. 2018;57(1):1–24.
Kim CH, Park J, Kim M. Gut microbiota-derived short-chain fatty acids, T cells, and inflammation. Immune Netw. 2014;14(6):277–88.
den Besten G, van Eunen K, Groen AK, Venema K, Reijngoud DJ, Bakker BM. The role of short-chain fatty acids in the interplay between diet, gut microbiota, and host energy metabolism. J Lipid Res. 2013;54(9):2325–40.
Rhoades N, Barr T, Hendrickson S, Prongay K, Haertel A, Gill L, et al. Maturation of the infant rhesus macaque gut microbiome and its role in the development of diarrheal disease. Genome Biol. 2019;20(1):173.
Russell RG, O’Donnoghue M, Blake DC Jr, Zulty J, DeTolla LJ. Early colonic damage and invasion of Campylobacter jejuni in experimentally challenged infant Macaca mulatta. J Infect Dis. 1993;168(1):210–5.
Sestak K, Merritt CK, Borda J, Saylor E, Schwamberger SR, Cogswell F, et al. Infectious agent and immune response characteristics of chronic enterocolitis in captive rhesus macaques. Infect Immun. 2003;71(7):4079–86.
Farkas T, Falkenstein KP, Bohm RP, Pecotte J, Sestak K. High incidence of rhesus enteric calicivirus infections and diarrhea in captive juvenile macaques: a likely association. J Med Primatol. 2012;41(5):325–8.
Wang KY, Christe KL, Yee J, Roberts JA, Ardeshir A. Rotavirus is associated with decompensated diarrhea among young rhesus macaques (Macaca mulatta). Am J Primatol. 2019;81(1):e22948.
Rockx B, Kuiken T, Herfst S, Bestebroer T, Lamers MM, Munnink BBO, et al. Comparative pathogenesis of COVID-19, MERS, and SARS in a nonhuman primate model. Science. 2020;368(6494):1012–5.
Itell HL, Kaur A, Deere JD, Barry PA, Permar SR. Rhesus monkeys for a nonhuman primate model of cytomegalovirus infections. Curr Opin Virol. 2017;25:126–33.
Sato K, Oiwa R, Kumita W, Henry R, Sakuma T, Ito R, et al. Generation of a nonhuman primate model of severe combined immunodeficiency using highly efficient genome editing. Cell Stem Cell. 2016;19(1):127–38.
Kapusinszky B, Ardeshir A, Mulvaney U, Deng X, Delwart E. Case-control comparison of enteric viromes in captive rhesus macaques with acute or idiopathic chronic diarrhea. J Virol. 2017;91(18):e00952–17.
Cizman M. The use and resistance to antibiotics in the community. Int J Antimicrob Agents. 2003;21(4):297–307.
Liu YW, Feng Y, Cheng DM, Xue JM, Wakelin S, Li ZJ. Dynamics of bacterial composition and the fate of antibiotic resistance genes and mobile genetic elements during the co-composting with gentamicin fermentation residue and lovastatin fermentation residue. Bioresour Technol. 2018;261:249–56.
Berendonk TU, Manaia CM, Merlin C, Fatta-Kassinos D, Cytryn E, Walsh F, et al. Tackling antibiotic resistance: the environmental framework. Nat Rev Microbiol. 2015;13(5):310–7.
He Y, Yuan QB, Mathieu J, Stadler L, Senehi N, Sun RN, et al. Antibiotic resistance genes from livestock waste: occurrence, dissemination, and treatment. NPJ Clean Water. 2020;3(1):1–11.
Gu YR, Shen SZ, Han BJ, Tian XL, Yang FX, Zhang KQ. Family livestock waste: an ignored pollutant resource of antibiotic resistance genes. Ecotoxicol Environ Saf. 2020;197:110567.
Sun J, Liao XP, DʼSouza AW, Boolchandani M, Li SH, Cheng K, et al. Environmental remodeling of human gut microbiota and antibiotic resistome in livestock farms. Nat Commun. 2020;11(1):1427.
Bolger AM, Lohse M, Usadel B. Trimmomatic: a flexible trimmer for Illumina sequence data. Bioinformatics. 2014;30(15):2114–20.
Langmead B, Salzberg SL. Fast gapped-read alignment with Bowtie 2. Nat Methods. 2012;9(4):357–9.
Li D, Liu CM, Luo R, Sadakane K, Lam TW. MEGAHIT: an ultra-fast single-node solution for large and complex metagenomics assembly via succinct de Bruijn graph. Bioinformatics. 2015;31(10):1674–6.
Hyatt D, Chen GL, Locascio PF, Land ML, Larimer FW, Hauser LJ. Prodigal: prokaryotic gene recognition and translation initiation site identification. BMC Bioinformatics. 2010;11:119.
Fu L, Niu B, Zhu Z, Wu S, Li W. CD-HIT: accelerated for clustering the next-generation sequencing data. Bioinformatics. 2012;28(23):3150–2.
Buchfink B, **e C, Huson DH. Fast and sensitive protein alignment using DIAMOND. Nat Methods. 2015;12(1):59–60.
Lombard V, Golaconda Ramulu H, Drula E, Coutinho PM, Henrissat B. The carbohydrate-active enzymes database (CAZy) in 2013. Nucleic Acids Res. 2014;42(Database issue):D490–5.
Moriya Y, Itoh M, Okuda S, Yoshizawa AC, Kanehisa M. KAAS: an automatic genome annotation and pathway reconstruction server. Nucleic Acids Res. 2007;35(Web Server issue):W182–5.
UniProt Consortium T. UniProt: the universal protein knowledgebase. Nucleic Acids Res. 2018;46(5):2699.
Patro R, Duggal G, Love MI, Irizarry RA, Kingsford C. Salmon provides fast and bias-aware quantification of transcript expression. Nat Methods. 2017;14(4):417–9.
Franzosa EA, McIver LJ, Rahnavard G, Thompson LR, Schirmer M, Weingart G, et al. Species-level functional profiling of metagenomes and metatranscriptomes. Nat Methods. 2018;15(11):962–8.
Suzek BE, Huang HZ, McGarvey P, Mazumder R, Wu CH. UniRef: comprehensive and non-redundant UniProt reference clusters. Bioinformatics. 2007;23(10):1282–8.
Wood DE, Salzberg SL. Kraken: ultrafast metagenomic sequence classification using exact alignments. Genome Biol. 2014;15(3):R46.
Segata N, Izard J, Waldron L, Gevers D, Miropolsky L, Garrett WS, et al. Metagenomic biomarker discovery and explanation. Genome Bio. 2011;12(6):R60.
Kaminski J, Gibson MK, Franzosa EA, Segata N, Dantas G, Huttenhower C. High-specificity targeted functional profiling in microbial communities with ShortBRED. Plos Comput Biol. 2015;11(12):e1004557.
Alcock BP, Raphenya AR, Lau TTY, Tsang KK, Bouchard M, Edalatmand A, et al. CARD 2020: antibiotic resistome surveillance with the comprehensive antibiotic resistance database. Nucleic Acids Res. 2020;48(D1):D517–D25.
Otasek D, Morris JH, Boucas J, Pico AR, Demchak B. Cytoscape automation: empowering workflow-based network analysis. Genome Biol. 2019;20(1):185.
Li XP, Liang SS, **a ZK, Qu J, Liu H, Liu C, et al. Establishment of a Macaca fascicularis gut microbiome gene catalog and comparison with the human, pig, and mouse gut microbiomes. GigaScience. 2018;7(9):giy100.
Campbell TP, Sun XQ, Patel VH, Sanz C, Morgan D, Dantas G. The microbiome and resistome of chimpanzees, gorillas, and humans across host lifestyle and geography. ISME J. 2020;14(6):1584–99.
Liu WJ, Zhang JC, Wu CY, Cai SF, Huang WQ, Chen J, et al. Unique features of ethnic Mongolian gut microbiome revealed by metagenomic analysis. Sci Rep. 2016;6:34826.
Asnicar F, Manara S, Zolfo M, Truong DT, Scholz M, Armanini F, et al. Studying vertical microbiome transmission from mothers to infants by strain-level metagenomic profiling. Msystems. 2017;2(1):e00164–16.
Costea PI, Coelho LP, Sunagawa S, Munch R, Huerta-Cepas J, Forslund K, et al. Subspecies in the global human gut microbiome. Mol Syst Biol. 2017;13(12):960.
Wen CP, Zheng ZJ, Shao TJ, Liu L, **e ZJ, Le Chatelier E, et al. Quantitative metagenomics reveals unique gut microbiome biomarkers in ankylosing spondylitis. Genome Biol. 2017;18(1):142.
Obregon-Tito AJ, Tito RY, Metcalf J, Sankaranarayanan K, Clemente JC, Ursell LK, et al. Subsistence strategies in traditional societies distinguish gut microbiomes. Nat Commun. 2015;6:6505.
Vogtmann E, Hua X, Zeller G, Sunagawa S, Voigt AY, Hercog R, et al. Colorectal cancer and the human gut microbiome: reproducibility with whole-genome shotgun sequencing. PloS One. 2016;11(5):e0155362.
Rampelli S, Schnorr SL, Consolandi C, Turroni S, Severgnini M, Peano C, et al. Metagenome sequencing of the Hadza hunter-gatherer gut microbiota. Curr Biol. 2015;25(13):1682–93.
Schirmer M, Franzosa EA, Lloyd-Price J, McIver LJ, Schwager R, Poon TW, et al. Dynamics of metatranscription in the inflammatory bowel disease gut microbiome. Nat Microbiol. 2018;3(3):337–46.
Monaghan TM, Sloan TJ, Stockdale SR, Blanchard AM, Emes RD, Wilcox M, et al. Metagenomics reveals impact of geography and acute diarrheal disease on the Central Indian human gut microbiome. Gut microbes. 2020;12(1):1752605.
Tailford LE, Crost EH, Kavanaugh D, Juge N. Mucin glycan foraging in the human gut microbiome. Front Genet. 2015;6(6):81.
Rossi M, Martinez-Martinez D, Amaretti A, Ulrici A, Raimondi S, Moya A. Mining metagenomic whole genome sequences revealed subdominant but constant Lactobacillus population in the human gut microbiota. Env Microbiol Rep. 2016;8(3):399–406.
Valeriano VDV, Balolong MP, Kang DK. Probiotic roles of Lactobacillus sp. in swine: insights from gut microbiota. J Appl Microbiol. 2017;122(3):554–67.
Jia J, Frantz N, Khoo C, Gibson GR, Rastall RA, McCartney AL. Investigation of the faecal microbiota associated with canine chronic diarrhoea. FEMS Microbiol Ecol. 2010;71(2):304–12.
Ma C, Zhao J, ** X, Ding J, Wang H, Zhang H, et al. Bovine mastitis may be associated with the deprivation of gut Lactobacillus. Benef Microbes. 2016;7(1):95–102.
Linninge C, Xu J, Bahl MI, Ahrne S, Molin G. Lactobacillus fermentum and Lactobacillus plantarum increased gut microbiota diversity and functionality, and mitigated Enterobacteriaceae, in a mouse model. Benef Microbes. 2019;10(4):413–24.
Reid G, Burton J. Use of Lactobacillus to prevent infection by pathogenic bacteria. Microbes Infect. 2002;4(3):319–24.
Boris S, Barbes C. Role played by lactobacilli in controlling the population of vaginal pathogens. Microbes Infect. 2000;2(5):543–6.
Spinler JK, Taweechotipatr M, Rognerud CL, Ou CN, Tumwasorn S, Versalovic J. Human-derived probiotic Lactobacillus reuteri demonstrate antimicrobial activities targeting diverse enteric bacterial pathogens. Anaerobe. 2008;14(3):166–71.
Van Tassell ML, Miller MJ. Lactobacillus adhesion to mucus. Nutrients. 2011;3(5):613–36.
Pridmore RD, Berger B, Desiere F, Vilanova D, Barretto C, Pittet AC, et al. The genome sequence of the probiotic intestinal bacterium Lactobacillus johnsonii NCC 533. Proc Natl Acad Sci U S A. 2004;101(8):2512–7.
Kemgang TS, Kapila S, Shanmugam VP, Kapila R. Cross-talk between probiotic lactobacilli and host immune system. J Appl Microbiol. 2014;117(2):303–19.
Chatterjee M, Pushkaran AC, Vasudevan AK, Menon KKN, Biswas R, Mohan CG. Understanding the adhesion mechanism of a mucin binding domain from Lactobacillus fermentum and its role in enteropathogen exclusion. Int J Biol Macromol. 2018;110:598–607.
Smaoui S, Elleuch L, Bejar W, Karray-Rebai I, Ayadi I, Jaouadi B, et al. Inhibition of fungi and gram-negative bacteria by bacteriocin BacTN635 produced by Lactobacillus plantarum sp. TN635. Appl Biochem Biotechnol. 2010;162(4):1132–46.
Coquelle N, Fioravanti E, Weik M, Vellieux F, Madern D. Activity, stability and structural studies of lactate dehydrogenases adapted to extreme thermal environments. J Mol Biol. 2007;374(2):547–62.
Mu Q, Tavella VJ, Luo XM. Role of Lactobacillus reuteri in human health and diseases. Front Microbiol. 2018;9:757.
Lai HH, Chiu CH, Kong MS, Chang CJ, Chen CC. Probiotic Lactobacillus casei: effective for managing childhood diarrhea by altering gut microbiota and attenuating fecal inflammatory markers. Nutrients. 2019;11(5):1150.
van Zyl WF, Deane SM, Dicks LMT. Molecular insights into probiotic mechanisms of action employed against intestinal pathogenic bacteria. Gut microbes. 2020;12(1):1831339.
Fernandez KR, Hansen LM, Vandamme P, Beaman BL, Solnick JV. Captive rhesus monkeys (Macaca mulatta) are commonly infected with Helicobacter cinaedi. J Clin Microbiol. 2002;40(6):1908–12.
Fox JG, Handt L, Xu S, Shen Z, Dewhirst FE, Paster BJ, et al. Novel Helicobacter species isolated from rhesus monkeys with chronic idiopathic colitis. J Med Microbiol. 2001;50(5):421–9.
Pullan RD, Thomas GAO, Rhodes M, Newcombe RG, Williams GT, Allen A, et al. Thickness of adherent mucus gel on colonic mucosa in humans and its relevance to colitis. Gut. 1994;35(3):353–9.
Johansson MEV, Hansson GC. Immunological aspects of intestinal mucus and mucins. Nat Rev Immunol. 2016;16(10):639–49.
Cantarel BL, Lombard V, Henrissat B. Complex carbohydrate utilization by the healthy human microbiome. PloS one. 2012;7(6):e28742.
Smith PM, Howitt MR, Panikov N, Michaud M, Gallini CA, Bohlooly YM, et al. The microbial metabolites, short-chain fatty acids, regulate colonic Treg cell homeostasis. Science. 2013;341(6145):569–73.
Tan J, McKenzie C, Potamitis M, Thorburn AN, Mackay CR, Macia L. The role of short-chain fatty acids in health and disease. Adv Immunol. 2014;121:91–119.
Wang MM, Wichienchot S, He XW, Fu X, Huang Q, Zhang B. In vitro colonic fermentation of dietary fibers: fermentation rate, short-chain fatty acid production and changes in microbiota. Trends Food Sci Tech. 2019;88:1–9.
Binder HJ. Role of colonic short-chain fatty acid transport in diarrhea. Annu Rev Physiol. 2010;72:297–313.
Liu B, Wang W, Zhu X, Sun X, **ao J, Li D, et al. Response of Gut Microbiota to dietary fiber and metabolic interaction with SCFAs in piglets. Front Microbiol. 2018;9:2344.
Johnson JR, Moseley SL, Roberts PL, Stamm WE. Aerobactin and other virulence factor genes among strains of Escherichia coli causing urosepsis: association with patient characteristics. Infect Immun. 1988;56(2):405–12.
Delorenzo V, Martinez JL. Aerobactin production as a virulence factor: a reevaluation. Eur J Clin Microbiol. 1988;7(5):621–9.
Kaushal D, Mehra S, Didier PJ, Lackner AA. The non-human primate model of tuberculosis. J Med Primatol. 2012;41(3):191–201.
Clayton JB, Vangay P, Huang H, Ward T, Hillmann BM, Al-Ghalith GA, et al. Captivity humanizes the primate microbiome. Proc Natl Acad Sci U S A. 2016;113(37):10376–81.
De Filippo C, Cavalieri D, Di Paola M, Ramazzotti M, Poullet JB, Massart S, et al. Impact of diet in sha** gut microbiota revealed by a comparative study in children from Europe and rural Africa. Proc Natl Acad Sci U S A. 2010;107(33):14691–6.
Yasuda K, Oh K, Ren B, Tickle TL, Franzosa EA, Wachtman LM, et al. Biogeography of the intestinal mucosal and lumenal microbiome in the rhesus macaque. Cell Host Microbe. 2015;17(3):385–91.
Manara S, Asnicar F, Beghini F, Bazzani D, Cumbo F, Zolfo M, et al. Microbial genomes from non-human primate gut metagenomes expand the primate-associated bacterial tree of life with over 1000 novel species. Genome Biol. 2019;20(1):299.
David LA, Maurice CF, Carmody RN, Gootenberg DB, Button JE, Wolfe BE, et al. Diet rapidly and reproducibly alters the human gut microbiome. Nature. 2014;505(7484):559–63.
Amato KR, Sanders JG, Song SJ, Nute M, Metcalf JL, Thompson LR, et al. Evolutionary trends in host physiology outweigh dietary niche in structuring primate gut microbiomes. ISME J. 2019;13(3):576–87.
Schechner V, Temkin E, Harbarth S, Carmeli Y, Schwaber MJ. Epidemiological interpretation of studies examining the effect of antibiotic usage on resistance. Clin Microbiol Rev. 2013;26(2):289–307.
Thaker M, Spanogiannopoulos P, Wright GD. The tetracycline resistome. Cell Mol Life Sci. 2010;67(3):419–31.
Bartha NA, Soki J, Edit U, Nagy E. Investigation of the prevalence of tetQ, tetX and tetX1 genes in Bacteroides strains with elevated tigecycline minimum inhibitory concentrations. Int J Antimicrob Agents. 2011;38(6):522–5.
Duan YJ, Chen ZY, Tan L, Wang XL, Xue YG, Wang SP, et al. Gut resistomes, microbiota and antibiotic residues in Chinese patients undergoing antibiotic administration and healthy individuals. Sci Total Environ. 2020;705:135674.
Cloeckaert A, Baucheron S, Flaujac G, Schwarz S, Kehrenberg C, Martel JL, et al. Plasmid-mediated florfenicol resistance encoded by the floR gene in Escherichia coli isolated from cattle. Antimicrob Agents Chemother. 2000;44(10):2858–60.
Colodner R. Extended-spectrum beta-lactamases: a challenge for clinical microbiologists and infection control specialists. Am J Infect Control. 2005;33(2):104–7.
Nordmann P, Dortet L, Poirel L. Carbapenem resistance in Enterobacteriaceae: here is the storm! Trends Mol Med. 2012;18(5):263–72.
Acknowledgements
We thank Miss Jiao Wang and Mr. Guanglun Lei for the sample collection.
Funding
This work was supported by the Sichuan Science and Technology Program (2020YJ0303) and the Key Research and Development Projects of the Science and Technology Department of Sichuan Province (Grant No.2019YFS0319).
Author information
Authors and Affiliations
Contributions
Shengzhi Yang, Yu Liu, Nan Yang, and Yue Lan performed the bioinformatics analyses and collected the samples; Weiqi Lan and **yi Feng performed the experiments; Shengzhi Yang and Yu Liu wrote the manuscript; Bisong Yue, Miao He, Liang Zhang, Anyun Zhang, and Megan Price revised the manuscript; **g Li and Zhenxin Fan designed and supervised the study. The authors read and approved the final manuscript.
Corresponding authors
Ethics declarations
Ethics approval and consent to participate
This study was approved by the Ethics Committee of the College of Life Sciences, Sichuan University (No. 20210308001). We strictly obeyed the guidelines of the management committee of experimental animals of Sichuan Province, China (SYXK-Sichuan, 2019-192) in the sample collection and utility protocols.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1: Table S1.
The summary of information of RMs. Table S2. The antibiotic resistant profiles of isolates from RMs
Additional file 2: Figure S1.
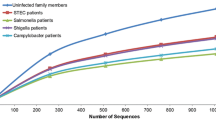
The gut microbiome of chronic diarrhea RMs and asymptomatic RMs. Figure S2. The functional comparison of gut microbiome. Figure S3. The gut bacterial composition of NHPs and human. Figure S4. The antibiotic resistance in gut microbiome of asymptomatic and chronic diarrhea RMs.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Yang, S., Liu, Y., Yang, N. et al. The gut microbiome and antibiotic resistome of chronic diarrhea rhesus macaques (Macaca mulatta) and its similarity to the human gut microbiome. Microbiome 10, 29 (2022). https://doi.org/10.1186/s40168-021-01218-3
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s40168-021-01218-3