Abstract
In KMT2A-rearranged acute lymphoblastic leukemia (ALL), an aggressive malignancy, oncogenic KMT2A-fusion proteins inappropriately recruit DOT1L to promote leukemogenesis, highlighting DOT1L as an attractive therapeutic target. Unfortunately, treatment with the first-in-class DOT1L inhibitor pinometostat eventually leads to non-responsiveness. To understand this we established acquired pinometostat resistance in pediatric KMT2A::AFF1+ B-ALL cells. Interestingly, these cells became mostly independent of DOT1L-mediated H3K79 methylation, but still relied on the physical presence of DOT1L, HOXA9 and the KMT2A::AFF1 fusion. Moreover, these cells selectively lost the epigenetic regulation and expression of various KMT2A-fusion target genes such as PROM1/CD133, while other KMT2A::AFF1 target genes, including HOXA9 and CDK6 remained unaffected. Concomitantly, these pinometostat-resistant cells showed upregulation of several myeloid-associated genes, including CD33 and LILRB4/CD85k. Taken together, this model comprehensively shows the adaptive potential of KMT2A-rearranged ALL cells upon losing dependency on one of its main oncogenic properties.
Similar content being viewed by others
Background
Chromosomal translocations involving the KMT2A (MLL) gene constitute the cytogenetic hallmark of acute lymphoblastic leukemia (ALL) diagnosed in infants (< 1 year of age), giving rise to an aggressive malignancy with high relapse rates and low event-free survival (EFS) chances of 30–40% [1, 2]. Hence, currently available treatment regimens for KMT2A-rearranged infant ALL are inadequate and require more effective therapeutic options to improve clinical outcome.
KMT2A translocations result in the fusion of KMT2A to one of its many translocation partner genes, [3] generating chimeric transcripts encoding highly oncogenic KMT2A fusion proteins. Among infant ALL patients, KMT2A is most recurrently fused to either AFF1 (AF4), MLLT1 (ENL), or MLLT3 (AF9) [3]. Functionally, wild-type KMT2A plays an essential role in definitive hematopoiesis [4] regulating gene expression through histone 3 lysine 4 (H3K4) methyltransferase activity, mediated by its Su(Var)3–9, Enhancer-of-zeste, Trithorax (SET) domain [5]. In contrast, KMT2A fusion proteins lose their SET domain, but instead recruit the histone 3 lysine 79 (H3K79) methyltransferase DOT1L through binding motifs encoded by the translocation partner genes [6,7,8]. Binding of DOT1L to KMT2A fusion proteins causes inappropriate H3K79 hypermethylation at KMT2A target genes, leading to an altered transcriptomic landscape that strongly favors leukemia development [6,7,8,9].
Interestingly, the mutational landscape of KMT2A-rearranged infant ALL is remarkably silent, with only 1.3–2.5 leukemia-specific, non-silent mutations in the dominant clone per patient, [10, 11] suggesting that the KMT2A translocation may well be the sole oncogenic lesion driving this aggressive type of leukemia [12]. Therefore, targeting DOT1L, through which KMT2A fusion proteins exert their oncogenic effects, represents an attractive therapeutic strategy. Accordingly, the development of the DOT1L inhibitor EPZ004777 and its successor EPZ5676 (pinometostat) [13, 14] were expected to become key to successful treatment of KMT2A-rearranged acute leukemias. However, despite promising preclinical results, subsequent clinical trials revealed that good initial responses in patients treated with pinometostat readily led to non-responsiveness due to acquired resistance and poor pharmacokinetics (PK) [15, 16]. Previously, it was reported that acquired resistance to pinometostat in KMT2A-rearranged acute leukemic cell lines is associated with enhanced drug efflux mediated by the elevated expression of the multidrug resistance transporters ABCB1 and ABCG2 [17].
Despite this, targeting DOT1L remains a promising avenue for treating KMT2A rearranged leukemias, and novel small-molecule DOT1L inhibitors with improved PK profiles have already been identified [40,41,42] and has been exploited as a therapeutic target for AML. In SEM a subpopulation of 20% of CD33-positive cells was identified, which was increased in SEMPINO_RES to about 40%, yet CD33-positive cells again were largely absent in SEMPINO−INT (Fig. 5D,F). Similarly, in RS4;11 a CD33-positive subpopulation of 9% was increased upon pinometostat resistance to 14% in RS4;11PINO_RES#1 and up to 50% in RS4;11PINO_RES#2 (Fig. 5D,F).
Together these data indicate that under prolonged pressure of DOT1L inhibition, KMT2A-rearranged ALL cells seem to initiate a reprogramming process that involves the acquisition (or selection) of myeloid-like characteristics.
Drug screens reveal minimal cross resistance, and sensitization towards venetoclax after acquired pinometostat resistance
Finally, acquired pinometostat resistance led to the upregulation of the multidrug efflux pump ABCB1 (Fig. 2F and Figure S6A,B), associated with multidrug resistance and previously reported as the mechanism of pinometostat resistance in KMT2A-rearranged acute leukemia cell lines [17]. However, our data challenges the concept that elevated ABCB1 expression alone is the mechanism of resistance to DOT1L inhibition as reported previously [17]. Despite significant ABCB1 upregulation, we still observe comparable inhibition of H3K79 methylation in SEM and SEMPINO_RES (Fig. 1D and E), indicating that the amount of pinometostat and/or its retention in SEMPINO_RES cells is sufficient to effectively reduce H3K79me2 levels, overriding the impact of ABCB1 upregulation.
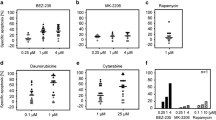
Since multidrug efflux pumps are associated with multidrug resistance [43, 44], we assessed whether SEMPINO_RES cells had become more resistant to current chemotherapeutics for KMT2A-rearranged infant ALL [1, 2] and whether we could identify agents to which SEMPINO_RES cells had become more sensitive by performing drug library screens (Table S2, Fig. 6A,B).
Moderate levels of cross-resistance and substantial sensitization towards venetoclax in pinometostat-resistant KMT2A-rearranged ALL cells. A. Drug response curves for prednisolone, dexamethasone, vincristine, daunorubicin, cladribine, cytarabine, and L-asparaginase as determined by 4-day MTT assays in SEM and SEMPINO_RES cells with n = 4 biological replicates, each comprising n = 3 technical replicates, and presented as the mean ± standard error of the mean (SEM). B. Comparison of the IC50 in SEM and SEMPINO_RES cells for a total of 679 compounds tested in drug library screens. C. Showing the top 10 agents with the highest fold-changes in IC50 values in SEMPINO_RES as compared to SEM, indicating enhanced resistance in SEMPINO_RES cells. D. The top 10 drugs with the lowest fold-changes in IC50 values in SEMPINO_RES as compared to SEM, indicating enhanced sensitivity in SEMPINO_RES cells. E. Drug response curves for venetoclax as determined by 4-day MTT assays in indicated cell lines models (in duplicate), presented as the mean ± standard error of the mean (SEM)
This revealed an increased resistance to the glucocorticoids dexamethasone and prednisolone (the liver-activated form of prednisone), vincristine, daunorubicin, and L-asparaginase, and increased sensitivity to cytarabine and for instance to the BCL-2 inhibitor venetoclax (Fig. 6A-E). Interestingly, cytarabine typically represents a drug commonly used in the treatment of myeloid leukemias, and the combination of venetoclax and cytarabine has successfully been tested in AML patients [45,46,47].
Discussion
The currently accepted dogma of KMT2A-fusion driven leukemogenesis dictates the requirement of DOT1L-mediated activation of KMT2A target genes through H3K79 methylation [6, 9, 48, 49]. Therefore, targeting DOT1L [13, 18, 19] represents an attractive therapeutic option for patients diagnosed with KMT2A-rearranged acute leukemia, despite the first-in-class DOT1L inhibitor pinometostat showing dissatisfying results in adult patients [15]. While next generation DOT1L inhibitors with improved pharmacokinetic profiles are in development, [18, 19] we reasoned that the mechanisms by which KMT2A-rearranged acute leukemia cells evade DOT1L inhibition may provide novel insights into the biology of these unique malignancies. Therefore, and in a similar fashion as published by Campbell and colleagues [17], we efficiently induced acquired pinometostat resistance in various cell line models, demonstrating how readily KMT2A-rearranged acute leukemia cells become resistant to DOT1L inhibition. The study of Campbell et al., mainly focused on examples of possible mechanisms of pinometostat resistance including increased expression of drug efflux transporters and activation of the PI3K/AKT and RAS/RAF/MEK/ERK pathways [17]. In contrast, we here specifically focused on the behavior and epigenetic regulation of DOT1L-associated KMT2A fusion-driven target genes and on how the transcriptomic landscape changes in KMT2A-rearranged ALL cells that are able to evade leukemic cell death during prolonged inhibition of DOT1L-mediated H3K79 methylation.
In concordance with the previous finding by Campbell et al., we found increased expression of the multi-drug efflux pump ABCB1 in our pinometostat-resistant SEMPINO_RES cells. However, despite the elevated levels of ABCB1 expression, pinometostat continued to inhibit H3K79 methylation in SEMPINO_RES. This strongly indicates that the increased levels of ABCB1 are insufficient to prevent pinometostat from exerting its inhibitory effects, and therefore cannot be the sole mechanism of acquired pinometostat resistance.
Interestingly, while cell viability of SEMPINO_RES cells was no longer affected by pinometostat-induced inhibition of DOT1L-mediated H3K79 methylation, these cells remained dependent on the physical presence of DOT1L protein. This may indicate that recently described biological functions of DOT1L that are independent of H3K79 methylation [50,51,52] are also important for KMT2A-rearranged acute leukemia cells. Thus, in addition to its enzymatic methylatransferase activity, DOT1L clearly has a scaffold function in assembling transcriptionally competent complexes. Therefore, therapeutic degradation of DOT1L instead of solely inhibiting its catalytic activities might be beneficial in the treatment of KMT2A-rearranged acute leukemia.
Another intriguing aspect of our model of acquired pinometostat resistance is the observation that SEMPINO_RES cells remained vulnerable to knockdown of the KMT2A::AFF1 fusion gene. This may suggest that inappropriate recruitment of DOT1L to loci otherwise not associated with H3K79me2 may not represent the sole KMT2A fusion-mediated attribute driving leukemogenesis and/or leukemia maintenance. If so, the identification of such DOT1L-independent oncogenic properties may well uncover important therapeutic targets and more effective treatment options for KMT2A-rearranged acute leukemias.
As shown, acquired resistance to pinometostat led to marked transcriptional downregulation of putative KMT2A-fusion target genes, which was accompanied by reductions in H3K79me2, as well as loss of binding of KMT2A and AFF1, and chromatin condensation at the corresponding loci. The complete loss of PROM1/CD133, which was shown to be transcriptionally regulated via KMT2A::AFF1-mediated H3K79me2/3 enhancer–promoter interactions, [29] in SEMPINO_RES is highly remarkable, since the expression of PROM1/CD133 was reported to be essential for leukemic cell growth in KMT2A-rearranged ALL [29, 30]. Consequently, targeting PROM1/CD133-positive cells has been proposed as a therapeutic option for KMT2A-rearranged ALL, although the expression of PROM1/CD133 on both fetal and adult hematopoietic stem cells (HSCs) may compromise the specificity of such an approach [29, 30, 53, 54]. Moreover, PROM1/CD133 is expressed in most, but not all, KMT2A-rearranged acute leukemia patients, and its presence seems to reflect the immunophenotype and/or cell of origin of the leukemia, as HSCs and early progenitors typically express PROM1/CD133, while more differentiated B-cell progenitors do not [29, 54, 55]. As acquiring resistance to DOT1L inhibition was accompanied by a complete loss of PROM1/CD133 expression, this may suggest that prolonged exposure to pinometostat triggered the differentiation towards (or selection of) a more mature immunophenotype. On the other hand, our data revealed that prolonged exposure of KMT2A-rearranged ALL cells to pinometostat seems to initiate a reprogramming process that involves the acquirement (or selection) of myeloid-like characteristics. Co-expression of myeloid CD markers, including CD33, [36] represents a familiar phenomenon in KMT2A-rearranged infant ALL with prognostic relevance [37, 38]. Moreover, a recent single-cell multiomics study by Chen and co-workers revealed the presence of pre-existing lymphomyeloid primed progenitors and myeloid blasts in diagnostic samples derived from KMT2A-rearranged B-ALL patients [56]. From this perspective, prolonged inhibition of DOT1L seems to favor KMT2A-rearranged leukemia cells that completely lack PROM1/CD133 but do display LILRB4/CD85k and CD33 expression. Interestingly, both LILRB4/CD85k and CD33 are therapeutic targets in AML [57,58,59,60,61,62,63] and have shown potential as therapeutic vulnerabilities in KMT2A-rearranged ALL. Targeting LILRB4/CD85k with antibody-conjugates [57] or anti-LILRB4 CAR-T cells [64, 65] and/or CD33 with gemtuzumab ozogamicin, could prevent resistance to DOT1L inhibitors in KMT2A-rearranged ALL. Moreover, combining BCL-2 inhibition by venetoclax with agents targeting DOT1L, LILRB4/CD85k, and/or CD33 may enhance the efficacy of these drug combinations. Venetoclax was found to synergize with DOT1L inhibitors [25, 66] and is being evaluated in clinical trials for pediatric KMT2A-rearranged leukemias [67, 68].
Taken together, we present an in vitro model of acquired resistance to DOT1L inhibition in KMT2A-rearranged ALL, revealing selective loss of epigenetic regulation and gene expression of KMT2A-fusion target genes, accompanied by upregulation of myeloid-like characteristics. This study may not only impact the development of novel DOT1L inhibitors, but also reveal key characteristics of KMT2A-rearranged ALL cells that are able to evade therapy, providing therapeutic targets to prevent that.
Availability of data and materials
The cell lines resistant to DOT1L inhibitor pinometostat generated in this study is available from the lead contact upon request. Data and code availability: Sequencing data generated for this publication have been deposited in the Gene Expression Omnibus (GEO), accession GSE230807. Any additional information required to reanalyze the data reported in this paper is available from the lead contact upon request.
References
Pieters R, De Lorenzo P, Ancliffe P, et al. Outcome of Infants younger than 1 year with Acute lymphoblastic leukemia treated with the Interfant-06 protocol: results from an International Phase III Randomized Study. J Clin Oncol. 2019;37(25):2246–56.
Pieters R, Schrappe M, De Lorenzo P, et al. A treatment protocol for infants younger than 1 year with acute lymphoblastic leukaemia (Interfant-99): an observational study and a multicentre randomised trial. Lancet. 2007;370(9583):240–50.
Meyer C, Burmeister T, Groger D, et al. The MLL recombinome of acute leukemias in 2017. Leukemia. 2018;32(2):273–84.
Ernst P, Wang J, Korsmeyer SJ. The role of MLL in hematopoiesis and leukemia. Curr Opin Hematol. 2002;9(4):282–7.
Krivtsov AV, Armstrong SA. MLL translocations, histone modifications and leukaemia stem-cell development. Nat Rev Cancer. 2007;7(11):823–33.
Bernt KM, Armstrong SA. A role for DOT1L in MLL-rearranged leukemias. Epigenomics. 2011;3(6):667–70.
Bernt KM, Zhu N, Sinha AU, et al. MLL-rearranged leukemia is dependent on aberrant H3K79 methylation by DOT1L. Cancer Cell. 2011;20(1):66–78.
Okada Y, Feng Q, Lin Y, et al. hDOT1L links histone methylation to leukemogenesis. Cell. 2005;121(2):167–78.
Krivtsov AV, Feng Z, Lemieux ME, et al. H3K79 methylation profiles define murine and human MLL-AF4 leukemias. Cancer Cell. 2008;14(5):355–68.
Agraz-Doblas A, Bueno C, Bashford-Rogers R, et al. Unraveling the cellular origin and clinical prognostic markers of infant B-cell acute lymphoblastic leukemia using genome-wide analysis. Haematologica. 2019;104(6):1176–88.
Andersson AK, Ma J, Wang J, et al. The landscape of somatic mutations in infant MLL-rearranged acute lymphoblastic leukemias. Nat Genet. 2015;47(4):330–7.
Sanjuan-Pla A, Bueno C, Prieto C, et al. Revisiting the biology of infant t(4;11)/MLL-AF4 + B-cell acute lymphoblastic leukemia. Blood. 2015;126(25):2676–85.
Daigle SR, Olhava EJ, Therkelsen CA, et al. Selective killing of mixed lineage leukemia cells by a potent small-molecule DOT1L inhibitor. Cancer Cell. 2011;20(1):53–65.
Daigle SR, Olhava EJ, Therkelsen CA, et al. Potent inhibition of DOT1L as treatment of MLL-fusion leukemia. Blood. 2013;122(6):1017–25.
Stein EM, Garcia-Manero G, Rizzieri DA, et al. The DOT1L inhibitor pinometostat reduces H3K79 methylation and has modest clinical activity in adult acute leukemia. Blood. 2018;131(24):2661–9.
Stein EM, Tallman MS. Mixed lineage rearranged leukaemia: pathogenesis and targeting DOT1L. Curr Opin Hematol. 2015;22(2):92–6.
Campbell CT, Haladyna JN, Drubin DA, et al. Mechanisms of Pinometostat (EPZ-5676) treatment-emergent resistance in MLL-Rearranged leukemia. Mol Cancer Ther. 2017;16(8):1669–79.
Perner F, Gadrey JY, **ong Y, et al. Novel inhibitors of the histone methyltransferase DOT1L show potent antileukemic activity in patient-derived xenografts. Blood. 2020;136(17):1983–8.
Chen C, Zhu H, Stauffer F, et al. Discovery of Novel Dot1L inhibitors through a structure-based Fragmentation Approach. ACS Med Chem Lett. 2016;7(8):735–40.
van der Linden MH, Willekes M, van Roon E, et al. MLL fusion-driven activation of CDK6 potentiates proliferation in MLL-rearranged infant ALL. Cell Cycle. 2014;13(5):834–44.
Spijkers-Hagelstein JA, Pinhancos SS, Schneider P, Pieters R, Stam RW. Chemical genomic screening identifies LY294002 as a modulator of glucocorticoid resistance in MLL-rearranged infant ALL. Leukemia. 2014;28(4):761–9.
Greil J, Gramatzki M, Burger R, et al. The acute lymphoblastic leukaemia cell line SEM with t(4;11) chromosomal rearrangement is biphenotypic and responsive to interleukin-7. Br J Haematol. 1994;86(2):275–83.
Waters NJ. Preclinical pharmacokinetics and pharmacodynamics of Pinometostat (EPZ-5676), a first-in-Class, small molecule S-Adenosyl methionine competitive inhibitor of DOT1L. Eur J Drug Metab Pharmacokinet. 2017;42(6):891–901.
Guenther MG, Lawton LN, Rozovskaia T, et al. Aberrant chromatin at genes encoding stem cell regulators in human mixed-lineage leukemia. Genes Dev. 2008;22(24):3403–8.
Kerry J, Godfrey L, Repapi E, et al. MLL-AF4 spreading identifies binding Sites that are distinct from super-enhancers and that govern sensitivity to DOT1L inhibition in Leukemia. Cell Rep. 2017;18(2):482–95.
Barzegar Behrooz A, Syahir A, Ahmad S. CD133: beyond a cancer stem cell biomarker. J Drug Target. 2019;27(3):257–69.
Wu Y, Wu PY. CD133 as a marker for cancer stem cells: progresses and concerns. Stem Cells Dev. 2009;18(8):1127–34.
Zhang Q, Shi S, Yen Y, Brown J, Ta JQ, Le AD. A subpopulation of CD133(+) cancer stem-like cells characterized in human oral squamous cell carcinoma confer resistance to chemotherapy. Cancer Lett. 2010;289(2):151–60.
Godfrey L, Crump NT, O’Byrne S, et al. H3K79me2/3 controls enhancer-promoter interactions and activation of the pan-cancer stem cell marker PROM1/CD133 in MLL-AF4 leukemia cells. Leukemia. 2021;35(1):90–106.
Mak AB, Nixon AM, Moffat J. The mixed lineage leukemia (MLL) fusion-associated gene AF4 promotes CD133 transcription. Cancer Res. 2012;72(8):1929–34.
Adamaki M, Lambrou GI, Athanasiadou A, Vlahopoulos S, Papavassiliou AG, Moschovi M. HOXA9 and MEIS1 gene overexpression in the diagnosis of childhood acute leukemias: significant correlation with relapse and overall survival. Leuk Res. 2015;39(8):874–82.
Hu YL, Fong S, Ferrell C, Largman C, Shen WF. HOXA9 modulates its oncogenic partner Meis1 to influence normal hematopoiesis. Mol Cell Biol. 2009;29(18):5181–92.
Dobrowolska H, Gill KZ, Serban G, et al. Expression of immune inhibitory receptor ILT3 in acute myeloid leukemia with monocytic differentiation. Cytometry B Clin Cytom. 2013;84(1):21–9.
Costa AFO, Menezes DL, Pinheiro LHS, et al. Role of new immunophenotypic markers on prognostic and overall survival of Acute myeloid leukemia: a systematic review and Meta-analysis. Sci Rep. 2017;7(1):4138.
Churchill HRO, Fuda FS, Xu J, et al. Leukocyte immunoglobulin-like receptor B1 and B4 (LILRB1 and LILRB4): highly sensitive and specific markers of acute myeloid leukemia with monocytic differentiation. Cytometry B Clin Cytom. 2021;100(4):476–87.
Hara J, Hosoi G, Okamura T, et al. CD33 + B-cell precursor acute lymphoblastic leukemia in children: a distinct subgroup of B-cell precursor acute lymphoblastic leukemia. Int J Hematol. 1995;61(2):77–84.
Stutterheim J, de Lorenzo P, van der Sluis IM, et al. Minimal residual disease and outcome characteristics in infant KMT2A-germline acute lymphoblastic leukaemia treated on the Interfant-06 protocol. Eur J Cancer. 2022;160:72–9.
Stutterheim J, van der Sluis IM, de Lorenzo P, et al. Clinical implications of minimal residual disease detection in infants with KMT2A-Rearranged Acute Lymphoblastic Leukemia treated on the Interfant-06 protocol. J Clin Oncol. 2021;39(6):652–62.
Laszlo GS, Estey EH, Walter RB. The past and future of CD33 as therapeutic target in acute myeloid leukemia. Blood Rev. 2014;28(4):143–53.
van Dongen JJ, Orfao A, EuroFlow C, EuroFlow. Resetting leukemia and lymphoma immunophenoty**. Basis for companion diagnostics and personalized medicine. Leukemia. 2012;26(9):1899–907.
van Dongen JJ, Lhermitte L, Bottcher S, et al. EuroFlow antibody panels for standardized n-dimensional flow cytometric immunophenoty** of normal, reactive and malignant leukocytes. Leukemia. 2012;26(9):1908–75.
Kalina T, Flores-Montero J, van der Velden VH, et al. EuroFlow standardization of flow cytometer instrument settings and immunophenoty** protocols. Leukemia. 2012;26(9):1986–2010.
Baguley BC. Multiple drug resistance mechanisms in cancer. Mol Biotechnol. 2010;46(3):308–16.
Szakacs G, Paterson JK, Ludwig JA, Booth-Genthe C, Gottesman MM. Targeting multidrug resistance in cancer. Nat Rev Drug Discov. 2006;5(3):219–34.
Dillon R, Maycock S, Jackson A, et al. Venetoclax combined with low dose cytarabine compared to standard of care intensive chemotherapy for the treatment of favourable risk adult acute myeloid leukaemia (VICTOR): study protocol for an international, open-label, multicentre, molecularly-guided randomised, phase II trial. BMC Cancer. 2022;22(1):1174.
Kadia TM, Reville PK, Wang X, et al. Phase II study of Venetoclax added to Cladribine Plus Low-Dose Cytarabine Alternating with 5-Azacitidine in older patients with newly diagnosed Acute myeloid leukemia. J Clin Oncol. 2022;40(33):3848–57.
Wei AH, Strickland SA Jr, Hou JZ, et al. Venetoclax Combined with Low-Dose Cytarabine for previously untreated patients with Acute myeloid leukemia: results from a phase Ib/II study. J Clin Oncol. 2019;37(15):1277–84.
Nguyen AT, He J, Taranova O, Zhang Y. Essential role of DOT1L in maintaining normal adult hematopoiesis. Cell Res. 2011;21(9):1370–3.
Kuntimaddi A, Achille NJ, Thorpe J, et al. Degree of recruitment of DOT1L to MLL-AF9 defines level of H3K79 Di- and tri-methylation on target genes and transformation potential. Cell Rep. 2015;11(5):808–20.
Cao K, Ugarenko M, Ozark PA, et al. DOT1L-controlled cell-fate determination and transcription elongation are independent of H3K79 methylation. Proc Natl Acad Sci U S A. 2020;117(44):27365–73.
Wu A, Zhi J, Tian T, et al. DOT1L complex regulates transcriptional initiation in human erythroleukemic cells. Proc Natl Acad Sci U S A. 2021;118:27.
Yi Y, Ge S. Targeting the histone H3 lysine 79 methyltransferase DOT1L in MLL-rearranged leukemias. J Hematol Oncol. 2022;15(1):35.
Li D, Hu Y, ** Z, et al. TanCAR T cells targeting CD19 and CD133 efficiently eliminate MLL leukemic cells. Leukemia. 2018;32(9):2012–6.
Bueno C, Velasco-Hernandez T, Gutierrez-Aguera F, et al. CD133-directed CAR T-cells for MLL leukemia: on-target, off-tumor myeloablative toxicity. Leukemia. 2019;33(8):2090–125.
O’Byrne S, Elliott N, Rice S, et al. Discovery of a CD10-negative B-progenitor in human fetal life identifies unique ontogeny-related developmental programs. Blood. 2019;134(13):1059–71.
Chen C, Yu W, Alikarami F, et al. Single-cell multiomics reveals increased plasticity, resistant populations, and stem-cell-like blasts in KMT2A-rearranged leukemia. Blood. 2022;139(14):2198–211.
Anami Y, Deng M, Gui X, et al. LILRB4-targeting antibody-drug conjugates for the treatment of Acute myeloid leukemia. Mol Cancer Ther. 2020;19(11):2330–9.
Gui X, Deng M, Song H, et al. Disrupting LILRB4/APOE Interaction by an efficacious humanized antibody reverses T-cell suppression and blocks AML Development. Cancer Immunol Res. 2019;7(8):1244–57.
Deng M, Chen H, Liu X, et al. Leukocyte immunoglobulin-like receptor subfamily B: therapeutic targets in cancer. Antib Ther. 2021;4(1):16–33.
Dhunputh C, Strullu M, Petit A et al. Single-dose (4.5 mg/m(2)) gemtuzumab ozogamicin in combination with fludarabine, cytarabine and anthracycline as reinduction therapy in relapsed or refractory paediatric acute myeloid leukaemia. Br J Haematol. 2022.
de Rooij JD, Zwaan CM, van den Heuvel-Eibrink M, Pediatric AML. From Biology to Clinical Management. J Clin Med. 2015;4(1):127–49.
Abuasab T, Rowe J, Tvito A. Emerging monoclonal antibody therapy for the treatment of Acute Lymphoblastic Leukemia. Biologics. 2021;15:419–31.
Percival MM, Estey EH. Current treatment strategies for measurable residual disease in patients with acute myeloid leukemia. Cancer. 2019;125(18):3121–30.
John S, Chen H, Deng M, et al. A novel Anti-LILRB4 CAR-T cell for the treatment of monocytic AML. Mol Ther. 2018;26(10):2487–95.
Smith CHR, **e J, Liu X, He Y, Ludwig K, Klesse L, Zhang C, John S. LILRB4 is a Novel Target for KMT2A rearranged Acute Leukemia. Blood; 2022.
Benito JM, Godfrey L, Kojima K, et al. MLL-Rearranged Acute Lymphoblastic Leukemias activate BCL-2 through H3K79 methylation and are sensitive to the BCL-2-Specific antagonist ABT-199. Cell Rep. 2015;13(12):2715–27.
Gibson A, Trabal A, McCall D et al. Venetoclax for Children and Adolescents with Acute Lymphoblastic Leukemia and Lymphoblastic Lymphoma. Cancers (Basel). 2021;14(1).
Winters AC, Maloney KW, Treece AL, Gore L, Franklin AK. Single-center pediatric experience with venetoclax and azacitidine as treatment for myelodysplastic syndrome and acute myeloid leukemia. Pediatr Blood Cancer. 2020;67(10):e28398.
Acknowledgements
We thank the members of the Stam group, as well as Jules P.P. Meijerink at the Princess Máxima Center for advice and discussions. We thank Utrecht Sequencing Facility for providing sequencing service and data. Utrecht Sequencing Facility is subsidized by the University Medical Center Utrecht, Hubrecht Institute, Utrecht University and The Netherlands X-omics Initiative (NWO project 184.034.019).
Funding
The present study was financially supported by Foundation KiKa (Stichting Kinderen Kankervrij/Foundation Children Cancer-free), the Netherlands. T.A.M., N.T.C. and A.L.S were funded by Medical Research Council (MRC, UK) Molecular Haematology Unit grants MC_UU_00016/6 and MC_UU_00029/6. N.T.C. was supported by a Kay Kendall Leukaemia Fund Intermediate Fellowship (KKL1443).
Author information
Authors and Affiliations
Contributions
R.W.S. and P.S. conceived and designed the study; R.W.S. arranged funding; P.S., S.T.C.J.M.A-P, R.S.B., F.R.S.A, A.J. and B.K. performed experiments; N.T.C., A.L.S. and R.H analyzed sequencing data; P.S. processed and analyzed data; P.S. performed statistical analysis; S.N., R.P. and T.A.M. contributed to interpreting data; P.S. made figures; P.S and R.W.S. wrote the paper; all authors co-authors performed critical review of the manuscript and gave their final approval; P.S., and R.W.S. supervised the project.
Corresponding author
Ethics declarations
Conflict of interest
T.A.M. and N.T.C. are paid consultants for and shareholders in Dark Blue Therapeutics Ltd. The other authors declare no competing financial interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Schneider, P., Crump, N.T., Arentsen-Peters, S.T. et al. Modelling acquired resistance to DOT1L inhibition exhibits the adaptive potential of KMT2A-rearranged acute lymphoblastic leukemia. Exp Hematol Oncol 12, 81 (2023). https://doi.org/10.1186/s40164-023-00445-8
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s40164-023-00445-8