Abstract
Background
Studies have shown that chemotherapy and radiotherapy can cause premature ovarian failure and loss of fertility in female cancer patients. Ovarian cortex cryopreservation is a good choice to preserve female fertility before cancer treatment. Following the remission of the disease, the thawed ovarian tissue can be transplanted back and restore fertility of the patient. However, there is a risk to reintroduce cancer cells in the body and leads to the recurrence of cancer. Given the low success rate of current in vitro culture techniques for obtaining mature oocytes from primordial follicles, an artificial ovary with primordial follicles may be a good way to solve this problem.
Methods
In the study, we established an artificial ovary model based on the participation of mesenchymal stem cells (MSCs) to evaluate the effect of MSCs on follicular development and oocyte maturation. P2.5 mouse ovaries were digested into single cell suspensions and mixed with bone marrow derived mesenchymal stem cells (BM-MSCs) at a 1:1 ratio. The reconstituted ovarian model was then generated by using phytohemagglutinin. The phenotype and mechanism studies were explored by follicle counting, immunohistochemistry, immunofluorescence, in vitro maturation (IVM), in vitro fertilization (IVF), real-time quantitative polymerase chain reaction (RT-PCR), and Terminal-deoxynucleotidyl transferase mediated nick end labeling(TUNEL) assay.
Results
Our study found that the addition of BM-MSCs to the reconstituted ovary can enhance the survival of oocytes and promote the growth and development of follicles. After transplanting the reconstituted ovaries under kidney capsules of the recipient mice, we observed normal folliculogenesis and oocyte maturation. Interestingly, we found that BM-MSCs did not contribute to the formation of follicles in ovarian aggregation, nor did they undergo proliferation during follicle growth. Instead, the cells were found to be located around growing follicles in the reconstituted ovary. When theca cells were labeled with CYP17a1, we found some overlapped staining with green fluorescent protein(GFP)-labeled BM-MSCs. The results suggest that BM-MSCs may participate in directing the differentiation of theca layer in the reconstituted ovary.
Conclusions
The presence of BM-MSCs in the artificial ovary was found to promote the survival of ovarian cells, as well as facilitate follicle formation and development. Since the cells didn’t proliferate in the reconstituted ovary, this discovery suggests a potential new and safe method for the application of MSCs in clinical fertility preservation by enhancing the success rate of cryo-thawed ovarian tissues after transplantation.
Similar content being viewed by others
Background
With rapid advancements in cancer therapy, children and reproductive-age women are benefitting from overall improved survival rates [1]. It is well-documented that treatment of girls and women for cancer with radiation, chemotherapeutic drugs, or a combination of the two therapies can result in significant, and often irreversible, side-effect damage to the reproductive system [2, 3]. Anti-cancer therapy is often a cause of premature ovarian insufficiency (POI) due to the high sensitivity of the ovarian follicle reserve to chemotherapy and radiotherapy [4, 5]. Thus, there is an increased number of patients who received a gonadotoxic treatment and who later face fertility issues [6]. Overall, compared to the general population, women who undergo cancer treatment are 38% less likely to become pregnant. This reduction in the likelihood of subsequent pregnancies has been observed in nearly all types of cancer [7]. Consequently, the preservation of the ovarian reserve and prevention of infertility have become the primary quality of life concerns for patients and their physicians.
Fertility preservation refers to the use of surgical, pharmacologic, or laboratory techniques to provide assistance to women or men at risk of infertility in protecting and preserving their ability to have genetically derived offspring [8]. For women, common fertility preservation methods currently used include egg, embryo, and ovarian tissue freezing, whereas for unmarried or prepubertal women, freezing of the ovarian cortex is more appropriate [9,10,11]. After the patient’s condition has improved or resolved, the preserved ovarian cortex can be thawed and transplanted back to the patient. However, to minimize the risk of reintroducing cancer cells, an alternative approach involves culturing and develo** the primordial follicles within the frozen cortex in vitro. This process can also incorporate biomaterials to construct an artificial ovary which can be transplanted into the patient’s body with the capability to produce mature eggs [6, 12]. Scientists have been trying to fully realize the in vitro culture and maturation of human follicles [13]. Telfer et al. applied a two-step culture method: ovarian tissue culture followed by follicle culture, and successfully obtained meiotic-capable eggs within a short period of time. However, further confirmation is still needed to determine whether these eggs have the ability to fertilize and support embryonic development [14].
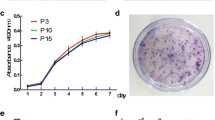
Ovary, as a female reproductive organ, has a non-renewable nature. In order to delay ovarian aging or provide fertility preservation services for people with POI, artificial ovary has always been a difficult and hot spot of research in the field of reproduction and regenerative medicine [15, 16]. 3D-printed hydrogel scaffolds are being widely explored for the development of artificial ovaries that can support the growth and development of primordial, primary, and secondary follicles [Full size image
Mouse mesenchymal stem cells reduced apoptosis in reconstituted ovaries
Next, we used the TUNEL assay to assess apoptosis in reconstituted ovaries with or without BM-MSCs and the aggregated ovaries were collected after 24, 48, and 96 h of culture. As shown in Fig. 4A and B, the reconstitution of ovary induced a lot of apoptosis in both somatic cells and oocytes (TUNEL+, VASA+). The highest cellular apoptosis (∼12%) was observed after 24 h of aggregation and then the apoptosis rate decreased gradually with less than 5% apoptotic cells in aggregated ovaries after 96 h of culture (Fig. 4C). However, nearly no apoptotic signals were found in BM-MSCs reconstituted ovary even at the 24-hour time point when a lot of apoptosis was observed in the control group. Thus, adding BM-MSCs promoted the survival of ovarian cells and avoided a large loss of oocytes shortly after reconstitution.
Mouse mesenchymal stem cells reduce apoptosis in reconstituted ovaries. (A) TUNEL assay of reaggregated ovaries after in vitro culture. (B) The Control group of rOvaries cultured in vitro for 24 h, TUNEL co-stained with immunofluorescence of germ cell marker VASA antibody. The apoptotic signal was present in VASA-positive oocytes. (Scale bar: 50 μm.). (C) The statistical analysis of TUNEL was performed to detect apoptosis within the tissues of rOvaries at various time points in the early post-recombinational period. ***p < 0.001. n = 4/each group. GFP-labeled MSCs were used to track the growth of reaggregated ovaries. (D) GFP-MSCs in reaggregated ovaries after recombination. (E) Analysis of scanning intensity statistics of green fluorescent signals carried by mesenchymal stem cells in MSC-rOvaries. n = 5/each group. *p<0.05. (F) Immunofluorescence labeling of proliferation by PCNA antibody, PCNA red fluorescent signal did not co-localize with GFP. (G) Western blot showed the increased phosphorylation of Akt, mTOR and RPS6 in BM-MSCs reconstituted ovaries after 96 h of culture.Scale bar, 50 μm.
Dynamic tracking of mouse MSCs during the growth of reconstituted ovaries
Mesenchymal stem cells have a strong ability to self-replicate in the process of in vitro culture, but this uncontrolled intensity of proliferation is risky for in vivo applications [25]. We reconstituted ovaries with green fluorescent protein (GFP)-labeled BM-MSCs (Figure S1B, 83% of GFP positive cells) and followed them to observe the proliferation and location of these cells involved in reconstituted ovaries. There was a clear downward trend in the density of green fluorescent cells from the first 24 h to 96 h after reconstitution (Fig. 4D). Statistical analysis of green fluorescence intensity further verified the result (Fig. 4E). We then labeled proliferating cells with PCNA staining and we found the PCNA signals did not coincide with green fluorescence labeled MSCs. This means that MSCs didn’t proliferate in the aggregated ovary, but the numbers of oocytes and ovarian somatic cells exhibited a gradual increase within the reconstituted ovary. (Fig. 4F). BM-MSCs function to maintain oocyte survival and accelerate the proliferation of ovarian somatic cells during the assembly of follicles. Western blot then revealed the increased phosphorylation of Akt, mTOR and RPS6 in BM-MSCs reconstitute ovaries after 96 h of culture. It suggests BM-MSCs may promote follicle formation and follicle activation through the activation of PI3K/mTOR signaling pathway (Fig. 4G).
To further explore how MSCs behaved and contributed in reconstituted ovaries, GFP labeled BM-MSCs were tracked in the reconstitution of the ovary and oocytes were labeled with VASA staining. In the first 96 h of ovarian reconstruction, the MSCs distributed evenly with ovarian cells, however, they didn’t involve in the reassembly of follicles. After aggregated ovaries being transplanted into recipient mice, follicular development was observed and we found MSCs mainly distributed in the stroma of reconstituted ovaries around growing follicles. Together, we also noticed a significant decrease of MSC cell numbers and fluorescence in the reconstituted ovary (Fig. 5). To see if the MSCs participate in the differentiation of theca cells, we first stained the reconstituted ovary with the MSC cell marker CD44 after transplantation for two weeks. While the majority of CD44-positive cells also exhibited GFP fluorescence, we observed a subset of cells that exclusively expressed GFP (Fig. 6A). Theca cells were then labeled with CYP17a1 and we found although in most cases, GFP and CYP17a1 positive cells were not colocalized with each other, double positive cells were still observed in the theca layer (Fig. 6B). Together, our result revealed the pivotal role of BM-MSCs in the restoration of the ovarian function. These cells aid in the survival of aggregated ovarian tissues during the first several days of reconstruction. Although they don’t proliferate or contribute to the formation of follicle structure, their presence around growing follicles indicates their involvement in the differentiation of the theca layer.






