Abstract
Background
Excellent partial upper sternotomy outcomes have been reported for patients undergoing aortic surgery, but whether this approach is particularly beneficial to obese patients remains to be established. This study was developed to explore the outcomes of aortic surgical procedures conducted via a partial upper sternotomy or a full median sternotomy approach in obese patients.
Methods
We retrospectively examined consecutive acute type A aortic dissection patients who underwent aortic surgery in our hospital between January 2015 to January 2021. Patients were divided into two groups based on body mass index: ‘non-obese’ and ‘obese’. We then further stratified patients in the obese and non-obese groups into partial upper sternotomy and full median sternotomy groups, with outcomes between these two sternotomy groups then being compared within and between these two body mass index groups.
Results
In total, records for 493 patients that had undergone aortic surgery were retrospectively reviewed, leading to the identification of 158 consecutive obese patients and 335 non-obese patients. Overall, 88 and 70 obese patients underwent full median sternotomy and partial upper sternotomy, respectively, while 180 and 155 non-obese patients underwent these respective procedures. There were no differences between the full median sternotomy and partial upper sternotomy groups within either BMI cohort with respect to preoperative baseline indicators and postoperative complications. Among non-obese individuals, the partial upper sternotomy approach was associated with reduced ventilation time (P = 0.003), shorter intensive care unit stay (P = 0.017), shorter duration of hospitalization (P = 0.001), and decreased transfusion requirements (Packed red blood cells: P < 0.001; Fresh frozen plasma: P < 0.001). Comparable findings were also evident among obese patients.
Conclusions
Obese aortic disease patients exhibited beneficial outcomes similar to those achieved for non-obese patients via a partial upper sternotomy approach which was associated with significant reductions in the duration of intensive care unit residency, duration of hospitalization, ventilator use, and transfusion requirements. This surgical approach should thus be offered to aortic disease patients irrespective of their body mass index.
Similar content being viewed by others
Introduction
Aortic root aneurysm and aortic dissection are extremely serious vascular emergencies associated with high morbidity and mortality rates [1, 2]. Appropriate approaches to the management of aortic arch aneurysm patients are still being developed and optimized [3]. The conventional surgical approach for these patients is full median sternotomy (FMS), although minimally invasive partial upper sternotomy (PUS) has been employed as an alternative approach since the 1990s [4], even in obese patients [5]. However, FMS remains the standard approach for complex aortic surgery to ensure appropriate exposure and safety [6]. Even so, recent studies have explored minimally invasive surgical approaches to accessing the aortic root [7,8,9], ascending aorta [10], or aortic arch [3, 11,12,13]. These authors have reported successful surgical outcomes without increasing mortality or major complications. However, few studies have compared outcomes in obese patients with aortic disease following treatment via a PUS approach or conventional FMS.
As such, this study was designed to compare aortic disease patient outcomes between obese and non-obese patients that underwent treatment via a PUS to those of patients that were treated using a conventional FMS approach.
Patients and methods
Following approval from the Ethics Committee of Fujian Medical University Union Hospital, China (Approval No.: 2014KY038; Date: July 25, 2014), the records of patients treated from January 2015 to January 2021 were reviewed. We received written informed consent from subjects or their legal representatives before study initiation.
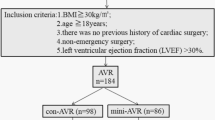
Patient groups
Patients were divided into two groups based on body mass index (BMI): ‘non-obese’ (BMI < 27.5 kg/m2) and ‘obese’ (BMI ≧ 27.5 kg/m2). The BMI thresholds selected to define obesity were based on the BMI criteria established by the World Health Organization for Asian populations [14]. We then divided the patients in the obese and non-obese groups into partial upper sternotomy and full median sternotomy groups based on the surgical approaches employed in their treatment. Patients were excluded if they: (1) had been diagnosed with aortitis, Marfan syndrome, metoxoarteritis, or systemic immune disorders, or (2) had previously undergone organ transplantation or experienced infective endocarditis, cardiogenic shock, malignancies, or chronic organ failure. The participant selection process is outlined in Fig. 1.
Study endpoints
Preoperative characteristics, operative parameters, and postoperative outcomes were compared between the FMS and PUS subgroups in the obese and non-obese cohorts. PUS was performed at the discretion of the operating surgeon through December 2016. Beginning in January 2017, PUS was the standard approach for all aortic surgical procedures. No additional preoperative assessments were performed for patients undergoing PUS. The expertise of the operating surgeons was similar for all patients, with all procedures having been performed by well-trained surgeons.
A pain chart with a maximum level of 10 was used to assess pain levels in unmedicated patients once per day after the patient is fully awake, with nursing staff recording the results.
Surgical techniques
Minimally invasive aortic surgery via a PUS approach
An 8–12 cm cutaneous incision was made, after which the sternum was incised in a J-form manner from the sternal notch to the right fourth intercostal space (Fig. 2A–C).
Aortic root reconstruction approach
A valve-sparing aortic root replacement (VSARR) procedure involved a modified David technique and a patch neointima technique [15] was used to repair the aortic valve in patients with severe AR, as detailed previously (Fig. 2D) [15, 16].
The Bentall procedure was defined as the replacement of the aortic root with a composite valve-graft device [17] (Fig. 2E).
Total arch and descending aortic replacement approach
Procedure details pertaining to the implantation of a modified triple-branched stent-graft (MTBSG) have been described previously [18]. Briefly, the branching arteries in the aortic arch were exposed, after which a MTBSG was implanted and released (Fig. 2F).
Statistical analysis
The Shapiro–Wilk test was used to assess data distributions. Continuous data are given as means ± standard deviations, and normally distributed data were compared between groups using t-tests. Categorical variables are given as percentages and were compared with chi-squared or Fisher’s exact tests, as appropriate. P < 0.05 was the significance threshold, and SPSS 26.0 (SPSS Inc.) was used for all analyses.
Results
Data
The Shapiro–Wilk test was applied to assess the distributions of all continuous variables, and all of these variables were found to conform to a normal distribution.
Patient characteristics
In total, 335 consecutive non-obese and 158 consecutive obese patients were identified. Overall, 88 and 70 obese patients underwent FMS and PUS, respectively, while 180 and 155 non-obese patients underwent these respective procedures. Similar risk profiles were observed when comparing these obese and non-obese patient cohorts with respect to their individual comorbidities (Table 1).
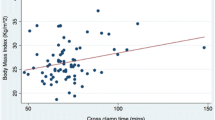
Operative characteristics
There were no significant differences in total operative duration, cardiopulmonary bypass time, SCP, or low body arrest when comparing surgical approaches in the obese and non-obese patient cohorts (Table 2), although the mean cross-clamp time was significantly longer in the PUS group for both non-obese (55.8 ± 26.9 min vs. 48.8 ± 17.8 min; P = 0.006) and obese patients (56.0 ± 19.8 min vs. 49.0 ± 16.5 min; P = 0.017).
Postoperative outcomes
For full details regarding the postoperative outcomes for patients included in this study, see Table 3. Rates of deep surgical site infection (DSSI) requiring revision, re-exploration, postoperative myocardial infarction, neurological dysfunction, renal dysfunction, hepatic insufficiency, pulmonary complications, and in-hospital mortality were also comparable between FMS and PUS subgroups in both the obese and non-obese cohorts. Neurological dysfunction was defined by delayed awakening, disorientation, convulsions, hemiplegia, severe limb muscle dysfunction, or coma. Renal dysfunction was defined as a 50% rise in baseline creatinine levels or a new need for dialysis. Hepatic insufficiency was defined as a bilirubin level greater than 5 mg/dL persisting for more than 5 days postoperatively. Pneumonia was defined by a chest roentgenogram-based diagnosis of pneumonia after cardiac surgery.
Among obese patients, PUS treatment was associated with decreases in ventilation time [106.2 ± 60.0 vs. 129.8 ± 77.8 h; P = 0.033], ICU stay length [5.5 ± 3.5 days vs. 7.8 ± 4.7 days; P = 0.001], hospitalization duration [17.2 ± 9.9 days vs. 21.5 ± 10.5 days; P = 0.010], and transfusion requirements (Packed red blood cells: 4.76 ± 3.08 units vs. 6.88 ± 4.66 units, P = 0.001; Fresh frozen plasma: 435.8 ± 108.5 ml vs. 511.9 ± 174.9 ml, P = 0.001). Similar trends were also evident for non-obese patients.
The postoperative daily (Day1–Day5) percentages of fully awake patients who reported either free of pain or experienced only minor pain (reporting a pain level below 3 on a scale with a maximum level of 10) were similar across groups (with all P > 0.05) (Fig. 3).
Discussion
Surgical procedures of the ascending aorta with or without total arch replacement and aortic root reconstruction have traditionally been performed via an FMS approach to ensure sufficient exposure. Recent advances in minimally invasive surgical techniques in combination with different partial sternotomy approaches have been employed as an alternative to FMS [12, 19,20,21,22], and have been used to conduct isolated heart valve disease treatment, Bentall, hemi-arch replacement, and ascending aorta repair procedures. These less invasive approaches have been linked to superior cosmetic and postoperative outcomes, including an overall reduction in surgical trauma, ventilator use, ICU stay duration, transfusion requirements, respiratory failure, and sternal stability as compared to the FMS approach [19, 23, 24].
Although the Bentall technique and valve-sparing aortic root surgery are complex procedures that necessitate good exposure, the value of PUS as an alternative access strategy for these complex procedures has been a topic of recent interest [9,10,11]. Hillebrand et al. [2] evaluated outcomes for 33 patients undergoing aortic root replacement with the Bentall procedure through a J-shaped PUS access and thereby confirmed the safety of PUS when conducting complex aortic surgery. Wachter et al. [25] also demonstrated the safety of valve-sparing aortic root replacement procedures when performing the David procedure using a PUS approach.
The degree of obesity is correlated with increases in the incidence of certain adverse outcomes including renal failure, sternal and wound infections, hospitalization duration, and prolonged mechanical ventilation [26,27,28,29]. To determine whether the benefits of PUS were reduced due to patient obesity among individuals undergoing aortic surgery, we herein compared PUS and FMS outcomes for obese and non-obese patients. To the best of our knowledge, this study is the most detailed analysis of this topic to date.
Comorbidities, operative duration, and major complication rates
In our study, we observed comparable preoperative risk profiles and operative durations for both obese and non-obese patients when comparing the PUS and FMS groups. Although PUS was associated with a longer cross-clamp duration, we do not believe that this difference, on the scale of minutes of ischemic time, is likely to be clinically relevant.
Rates of mortality and major complications were comparable in the PUS and FMS groups irrespective of BMI status, indicating that obese patients are good candidates for PUS treatment.
Pulmonary complications
Obesity has been linked to prolonged ventilator use and increased hypoxemia after surgical procedures when treating episodes of acute aortic dissection (AAD) [30]. MIS approaches better preserve the integrity of the chest wall and thus have the potential to decrease the length of postoperative ventilator use. While obese patients did exhibit prolonged ventilator use relative to non-obese patients when comparing the PUS patient cohorts, PUS treatment was nonetheless associated with reductions in ventilator use for both obese and non-obese patients as compared to FMS treatment. We additionally observed no significant differences in rates of pneumonia, reintubation, or tracheotomy in the PUS group for obese or non-obese patients, suggesting that limited surgical access does not result in unfavorable pulmonary outcomes even among obese patients.
Transfusion requirements
Patients in the present study that underwent treatment via a PUS approach exhibited reduced transfusion requirements as compared to patients treated via an FMS approach irrespective of whether or not they were obese. These results are in line with those of Wu et al. [31] and **e et al. [13, 20, 32, 33]. Previous evidence suggests that transfusions are associated with a negative impact on patient outcomes following cardiac surgery [34,35,36,37]. Obese participants in the present study that underwent PUS procedures did not exhibit any differences in transfusion requirements as compared to non-obese patients, further supporting the fact that this procedure does not expose obese individuals to greater risk.
Length of stay
MIS approaches are associated with decreased length of hospitalization and a shorter duration of ICU admittance [38]. Consistently, we found that both obese and non-obese patients in the PUS cohort exhibited shorter durations of hospitalization and ICU admittance as compared to patients in the FMS group. These findings are also consistent with previous meta-analyses [13, 23,24,25,26]. We did not observe any differences in ICU or hospital stay length for obese patients in this study relative to non-obese patients in the PUS cohort, indicating that this MIS approach is not associated with any increased risk for obese individuals.
Sternal infections
We did not observe any protective benefits with respect to the odds of postoperative sternum infection in the PUS cohort, potentially contradicting subjective clinical expectations. This may be attributable to the fact that the pathogenesis of sternal infections is multifactorial, and as such, the improved integrity of the sternum alone is not sufficient to reduce the risk of sternum infection. Notably, we did not observe any increased risk of postoperative sternal infections among obese patients in the PUS cohort in this study, suggesting that PUS does not expose obese patients to any additional risk of sternal infection.
Postoperative pain levels
Our results suggest that the PUS approach was associated with better postoperative pain levels. While these results do not align with those of a pooled analysis performed by Lim et al. [32], they are consistent with a meta-analysis conducted by Brown et al. [18] Overall, relatively limited data are available pertaining to this operative outcome, potentially explaining these contradictory results. We additionally found that obese and non-obese patients in the PUS cohort experienced comparable levels of postoperative pain.
Limitations
The present study was a retrospective analysis, and it is thus inherently subject to potneital bias. In addition, the study period was relatively long, and changes in perioperative therapeutic regimens over this period may have impacted these findings. Propensity score matching could not be performed, given that the inclusion criteria for the PUS group shifted over the course of the study period from being at the discretion of the operating surgeon to the standard departmental approach.
Conclusions
The results of this study indicate that it is both safe for obese patients to routinely undergo aortic root reconstruction or extensive total arch replacement via a PUS approach, and that this treatment approach is associated with good efficacy. This minimally invasive strategy did not adversely impact safety outcomes for obese patients, while still conferring benefits including reductions in postoperative ventilator use, ICU stay length, duration of hospitalization, and transfusion requirements. (see Fig. 4) However, further prospective randomized trials will be necessary to confirm and expand upon these findings.
Availability of data and materials
The data that support the findings of this study are available from Fujian Cardiac Medical Center but restrictions apply to the availability of these data, which were used under license for the current study, and so are not publicly available. Data are however available from the authors upon reasonable request and with permission of Fujian Cardiac Medical Center.
Abbreviations
- PUS:
-
Partial upper sternotomy
- FMS:
-
Full median sternotomy
- BMI:
-
Body mass index
- MIS:
-
Minimally invasive surgery
- VSARR:
-
Valve-sparing aortic root replacement
- MTBSG:
-
Modified triple-branched stent-graft
- AAD:
-
Acute aortic dissection
- ARDS:
-
Acute respiratory disease syndrome
- ICU:
-
Intensive care unit
References
Ji Q, Lai H, Sun YX, et al. Impact of presurgical mild acute respiratory distress syndrome on surgical mortality after surgical repair of acute type a aortic dissection. Int Heart J. 2017;58:739–45.
Hillebrand J, Alshakaki M, Martens S, et al. Minimally invasive aortic root replacement with valved conduits through partial upper sternotomy. Thorac Cardiovasc Surg. 2018;66:295–300.
Tokuda Y, Oshima H, et al. Extended total arch replacement via the L-incision approach: single-stage repair for extensive aneurysms of the aortic arch. Interact Cardiovasc Thorac Surg. 2016;22:750–5.
Bakir I, Casselman FP, Wellens F, et al. Minimally invasive versus standard approach aortic valve replacement. Ann Thorac Surg. 2006;81:1599–604.
Welp HA, Herlemann I, Martens S, et al. Outcomes of aortic valve replacement via partial upper sternotomy versus conventional aortic valve replacement in obese patients. Interact Cardiovasc Thorac Surg. 2018;27:481–6.
Roselli EE. Interventions on the aortic valve and proximal thoracic aorta through a minimally invasive approach. Ann Cardiothorac Surg. 2015;4:81–4.
Totaro P, Carlini S, Pozzi M, et al. Minimally invasive approach for complex cardiac surgery procedures. Ann Thorac Surg. 2009;88:462–7.
Shrestha M, Krueger H, Umminger J, et al. Minimally invasive valve sparing aortic root replacement (David procedure) is safe. Ann Cardiothorac Surg. 2015;4:148–53.
Monsefi N, Risteski P, Miskovic A, et al. Midterm results of a minimally invasive approach in David procedure. Thorac Cardiovasc Surg. 2018;66:301–6.
Perrotta S, Lentini S. Ministernotomy approach for surgery of the aortic root and ascending aorta. Interact CardioVasc Thorac Surg. 2009;9:849–58.
Ahmad A, Risteski P, Papadopoulos N, et al. Minimally invasive approach for aortic arch surgery employing the frozen elephant trunk technique. Eur J of Cardio-Thoracic Surg. 2016;50:140–4.
Oishi Y, Sonoda H, Tanoue Y, et al. Advantages of the L-incision approach comprising a combination of left anterior thoracotomy and upper halfmedian sternotomy for aortic arch aneurysms. Interact Cardiovasc Thorac Surg. 2011;13:280–3.
**e X-B, Dai X-F, Fang G-H, et al. Extensive repair of acute type A aortic dissection through a partial upper sternotomy and using complete stent-graft replacement of the arch. J Thorac Cardiovasc Surg. 2020;24(20):32885–93.
WHO Expert Consultation. Appropriate body-mass index for Asian populations and its implications for policy and intervention strategies. Lancet. 2004;363:157–63.
Chen L-W, **-Jie W, Li Q-Z, et al. A modifed valve-sparing aortic root replacement technique for acute type A aortic dissection:the patch neointima technique. Eur J Cardiothorac Surg. 2012;42:731–3.
Dai X-F, Fang G-H, Yan L-L, et al. Patch neointima technique in acute type A aortic dissection: mid-term results of 147 cases. Ann Thorac Surg. 2021;112:75–82.
Bentall H, DeBono A. A technique for complete replacement of the ascending aorta. Thorax. 1968;23:338–9.
Qiu Z-H, Chen L-W, Liao L-M, et al. Efficiency of modifified triple-branched stent graft in type I aortic dissection: two-year follow-up. Ann Thorac Surg. 2020;110:925–32.
Brown ML, McKellar SH, Sundt TM, et al. Ministernotomy versus conventional sternotomy for aortic valve replacement: a systematic review and meta-analysis. J Thorac Cardiovasc Surg. 2009;137:670-679.e5.
Scarci M, Young C, Fallouh H. Is ministernotomy superior to conventional approach for aortic valve replacement? Interact CardioVasc Thorac Surg. 2009;9:314–7.
Rodríguez-Caulo EA, Guijarro-Contreras A, Otero-Forero J, et al. Quality of life, satisfaction and outcomes after ministernotomy versus full sternotomy isolated aortic valve replacement (QUALITY-AVR): study protocol for a randomised controlled trial. Trials. 2018;19:114.
Morisaki A, Hattori K, Kato Y, et al. Evaluation of aortic valve replacement via the right parasternal approach without rib removal. Ann Thorac Cardiovasc Surg. 2015;21:139–45.
Tabata M, Khalpey Z, Aranki SF, et al. Minimal access surgery of ascending and proximal arch of the aorta: a 9-year experience. Ann Thorac Surg. 2007;84:67–72.
Filip G, Bryndza MA, Konstanty-Kalandyk J, et al. Ministernotomy or sternotomy in isolated aortic valve replacement? Early results. Kardiochir Torakochirurgia Pol. 2018;15:213–8.
Wachter K, Franke UF, Yadav R, et al. Feasibility and clinical outcome after minimally invasive valve-sparing aortic root replacement. Interact Cardiovasc Thorac Surg. 2017;24:377–83.
Birkmeyer NJ, Charlesworth DC, Hernandez F, et al. Obesity and risk of adverse outcomes associated with coronary artery bypass surgery. Northern New England Cardiovascular Disease Study Group. Circulation. 1998;97:1689–94.
Tolpin DA, Collard CD, Lee VV, et al. Obesity is associated with increased morbidity after coronary artery bypass graft surgery in patients with renal insuffificiency. J Thorac Cardiovasc Surg. 2009;138:873–9.
Roberts WC, Roberts CC, Vowels TJ, et al. Effect of body mass index on survival in patients having aortic valve replacement for aortic stenosis with or without concomitant coronary artery bypass grafting. Am J Cardiol. 2011;108:1767–71.
Smith RL 2nd, Herbert MA, Dewey TM, et al. Does body mass index affect outcomes for aortic valve replacement surgery for aortic stenosis? Ann Thorac Surg. 2012;93:742–6 (discussion 746–7).
Sheng W, Yang H-Q, Chi Y-F, et al. Independent risk factors for hypoxemia after surgery for acute aortic dissection. Saudi Med J. 2015;36:940–6.
Wu Y, Jiang W, Li D, et al. Surgery of ascending aorta with complex procedures for aortic dissection through upper mini-sternotomy versus conventional sternotomy. J Cardiothorac Surg. 2020;15:57.
Murtuza B, Pepper JR, Stanbridge RD, et al. Minimal access aortic valve replacement: Is it worth it? Ann Thorac Surg. 2008;85:1121–31.
Lim JY, Deo SV, Altarabsheh SE, et al. Conventional versus minimally invasive aortic valve replacement: pooled analysis of propensity-matched data. J Card Surg. 2015;30:125–34.
Ghanta RK, Lapar DJ, Kern JA, et al. Minimally invasive aortic valve replacement provides equivalent outcomes at reduced cost compared with conventional aortic valve replacement: a real-world multi-institutional analysis. J Thorac Cardiovasc Surg. 2015;149:1060–5.
Bhaskar B, Dulhunty J, Mullany DV, Fraser JF. Impact of blood product transfusion on short and long-term survival after cardiac surgery: more evidence. Ann Thorac Surg. 2012;94:460–7.
Reeves BC, Murphy GJ. Increased mortality, morbidity, and cost associated with red blood cell transfusion after cardiac surgery. Curr OpinCardiol. 2008;23:607–12.
von Heymann C, Kaufner L, Sander M, et al. Does the severity of preoperative anemia or blood transfusion have a stronger impact on long-term survival after cardiac surgery? J Thorac Cardiovasc Surg. 2016;152:1412–20.
Santana O, Reyna J, Grana R, et al. Outcomes of minimally invasive valve surgery versus standard sternotomy in obese patients undergoing isolated valve surgery. Ann Thorac Surg. 2011;91:406–10.
Acknowledgements
We highly acknowledge the contribution by the participators: Han-Fan Qiu, **, 353000, People’s Republic of China
Contributions
Z-RL and L-WC designed the study. Z-RL and Y-XC collected and analyzed data together. Z-RL drafted the article and submitted the manuscript. L-WC supervised this study. All authors read the final version of this article and approved for publication.
Corresponding author
Ethics declarations
Ethical approval and consent to participate
The present study was approved by the ethics committee of Fujian Medical University, China and adhered to the tenets of the Declaration of Helsinki.
Consent for publication
Not applicable.
Competing interests
All authors declare that they have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Luo, ZR., Chen, YX. & Chen, Lw. Surgical outcomes associated with partial upper sternotomy in obese aortic disease patients. J Cardiothorac Surg 17, 135 (2022). https://doi.org/10.1186/s13019-022-01890-y
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13019-022-01890-y