Abstract
Background
The reduction of slipped vertebra is often performed during surgery for degenerative lumbar spondylolisthesis (DLS). This approach, while potentially improving clinical and radiological outcomes, also carries a risk of increased complications due to the reduction process. To address this, we introduced an innovative lever reduction technique for DLS treatment. This study aims to investigate the clinical efficacy, radiological outcomes, and complications of fusion with or without lever reduction.
Methods
We conducted a retrospective review of prospectively collected data from a registry of patients who underwent lumbar fusion surgery for DLS, with a follow-up of at least 24 months. Self-reported measures included visual analog scale (VAS) for back or leg pain, Oswestry Disability Index (ODI), and the achievement of minimal clinically important difference (MCID). Radiological assessments encompassed spondylolisthesis percentage (SP), focal lordosis (FL), and lumbar lordosis (LL). Complications were categorized using the modified Clavien–Dindo classification (MCDC) scheme. Patients were assigned to the reduction group (RG) and non-reduction group (NRG) based on the application of the lever reduction technique. Clinical and radiological outcomes at baseline, immediately after surgery, and at the last follow-up were compared.
Results
A total of 281 patients were analyzed (123 NRG, 158 RG). Baseline patient demographics, comorbidities, and surgical characteristics were similarly distributed between groups except for operating time (NRG 129.25 min, RG 138.04 min, P = .009). Both groups exhibited significant clinical improvement after surgery (all, P = .000), with no substantial difference between groups (VAS, ODI, or the ability to reach MCID). Patients in RG showed statistically lower SP and higher FL during follow-up (all, P = .000). LL was comparable at different time points within each group or at the same time point between the two groups (all, P > .050). The overall complication rate (NRG 38.2%, RG 27.2%, P = .050) or specific complication rates per MCDC were similar between groups (all, P > .050). Patients in RG were predisposed to a lower risk of adjacent segment degeneration (ASDeg) (NRG 9.8%, RG 6.3%, P = .035).
Conclusions
There were no significant differences in postoperative measures such as VAS scores for back and leg pain, ODI, the ability to reach MCID, overall complication rate, or specific complication rates per MCDC between surgical approaches. However, fusion with lever reduction demonstrated a notable advantage in restoring segmental spinal sagittal alignment and reducing the occurrence of ASDeg compared to in situ fusion.
Similar content being viewed by others
Background
Degenerative lumbar spondylolisthesis (DLS) is a common pathological condition in the elderly population, characterized by the anterior displacement of a superior vertebra over the adjacent caudal vertebra, while the neural arch remains intact [1, 2]. Due to the spinal canal stenosis, compression of the nerve root in the lateral recess or in the foramen, and segmental instability secondary to spondylolisthesis, patients with DLS usually present with neurogenic claudication, radicular leg pain, or back pain [3]. In severe cases or when conservative treatments fail, decompression of the affected neural structures and stabilization of the spinal segment, so-called decompression and fusion surgery, are considered as a means to provide satisfactory long-term results [4, 5]. Besides the aforementioned interventions, whether or not to reduce the spondylolisthesis intraoperatively still needs to be determined by surgeons. Theoretically, the reduction procedure contributes to reducing slip distance, increasing segmental lumbar lordosis or intervertebral disc height, and potentially leads to better clinical outcomes or a higher fusion rate [6,7,8,9]. Nonetheless, conventional reduction methods predominantly rely on distraction of the disc space and direct elevating pull of the pedicle screws, which may also introduce a higher risk of complications, such as neurologic deficits, hardware failure (screw loosening or pull out), prolonged operating time, or loss of reduction [6, 10,11,12,13].
To reduce the surgical-related complications linked to the reduction procedure, we introduced a composite reduction technique encompassing both traditional elevating-pull reduction and innovative lever reduction. The clinical utility of this technique was previously demonstrated in case series [14]. This study aims to delve deeper into the clinical efficacy, radiological outcomes, and complications associated with fusion with or without lever reduction for DLS treatment. By doing so, we intend to offer valuable insights into the comparative effectiveness and safety of these two surgical approaches for DLS.
Methods
Patient population
Following approval by the ethics committee at our hospital, a retrospective review of the spine registry data was conducted on a consecutive cohort of 488 patients diagnosed with lumbar spondylolisthesis between May 2015 and December 2020. All the clinical and radiological data had been prospectively collected at the respective follow-up visits. Inclusion criteria were as follows: (1) single-level DLS (Meyerding grade I or II), (2) refractory to conservative treatments for more than 6 months, and (3) at least 2 years’ of follow-up with complete clinical and radiological data. Patients with other types of spondylolisthesis, multilevel (≥ 2) spondylolisthesis, high-grade spondylolisthesis (Meyerding grade III or IV), hip disorders, previous spinal surgery or trauma, or incomplete data, were excluded from analysis.
Surgical techniques
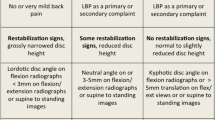
All included patients experienced stenosis caused by DLS and underwent decompression and lumbar interbody fusion during subsequent surgery. The surgeries were performed through an open posterior midline approach. Before bony decompression, bilateral pedicle screws were placed. Decompression consisted of bilateral facetectomy and partial foraminotomy, including the hypertrophic ligament flavum. The disc space was opened and thoroughly cleaned with intradiscal drills and pituitary rongeurs. The cartilaginous endplates were cleaned with caution so as to not cause injury to the bone endplates. Bilateral nerve roots were liberated before reduction. The reduction of the slipped vertebra was conducted following lever reduction technique (Fig. 1) [14]. The extent of slip reduction was verified with fluoroscopy. Then, the interspace was packed with autologous bone graft material, and an appropriately sized polyetheretherketone cage filled with bone was inserted into the disc space.
Reduction process of a slipped vertebrae. (1) Forward slippage of L5; (2) pedicle screws were placed at both vertebra of the slipped levels; (3) the nerve roots were decompressed before reduction. After removal of the disk tissues and endplate preparation, a rod was placed unilaterally and the pedicle screw of the lower vertebrae was locked; (4) a lever repositioner was placed at the anterior rim of the slipped vertebrae under fluoroscopy; (5) with the lower vertebrae as the lever fulcrum, force was applied to gradually pry the slipped vertebrae upward; 6) the pedicle screws of the slipped vertebrae were locked. Then, an addition rod was placed and all screws were locked. Quote from the study by Chao et al. (https://doi.org/10.1186/s12891-019-3028-8)
Patients undergoing fusion with lever reduction were assigned to the reduction group (RG). Conversely, patients undergoing in situ fusion (where intentional surgical reduction was not performed) were assigned to the non-reduction group (NRG). The assignment was made per surgeon's choice.
Clinical measurements
Clinical assessments including visual analog scale (VAS) for back pain, VAS for leg pain, and Oswestry Disability Index (ODI). The VAS was utilized to measure the severity of back and leg pain for patients based on a 10-cm line, with “painless” (0) and “most severe pain” (10 cm) at each respective end [15]. The validated ODI is a self-administered questionnaire for evaluating back-specific functional disability, consisting of 10 items with scores from 0 to 5, and higher ODI indicates more severe disability [16]. Minimal clinically important difference (MCID) was introduced to analyze the clinical significance of variations in clinical outcomes [17]. MCID values were set at 14.9 points for ODI, 2.1 points for VAS back pain, and 2.8 points for VAS leg pain [18]. All clinical outcomes were assessed by research assistants before surgery, immediately after surgery, and at each follow-up.
Radiological data acquisition
Measurements of radiological parameters are illustrated in Fig. 2, covering: (1) spondylolisthesis percentage (SP), the ratio of the interval between two extended lines of the posterior aspect of superior slipped vertebra and the inferior normal vertebra to the length of the superior endplate of the inferior normal vertebra; (2) focal lordosis (FL), the Cobb angle between the superior endplate of the upper slipped vertebra and the inferior endplate of the lower normal vertebra; and (3) lumbar lordosis (LL), the Cobb angle between the superior endplates of both L1 and S1. All radiological measurements were taken by two trained spinal surgeons (WW and YW) before surgery, immediately after surgery, and at each follow-up. The average of two measurements was taken as the final result.
Illustration of the radiological measurements. A SP, spondylolisthesis percentage, the ratio of the interval between two extended lines of the posterior aspect of superior slipped vertebra and the inferior normal vertebra to the length of the superior endplate of the inferior normal vertebra; B FL, focal lordosis, the Cobb angle between the superior endplate of the upper slipped vertebra and the inferior endplate of the lower normal vertebra; C LL, lumbar lordosis, the Cobb angle between the superior endplates of both L1 and S1
Complications assessment
All complications were recorded in light of the modified Clavien–Dindo classification (MCDC) scheme containing five types of complications: Type I–normal recovery without any treatment; Type II–pharmacologic treatment needed; Type III–invasive intervention under general anesthesia needed; Type IV–intensive care unit admission needed; Type V–death [19]. Adjacent segment degeneration (ASDeg) was diagnosed when plain radiographs, computerized tomography, or magnetic resonance imaging demonstrated one or more of the following lesions at the segment adjacent to the fused segment that were not present preoperatively: (1) development of anterolisthesis or retrolisthesis > 4 mm, (2) range of motion between adjacent vertebral bodies > 10°, (3) loss of disc height > 10%, (4) osteophyte formation > 3 mm, as well as (5) spinal stenosis caused by facet joint hypertrophy, compression fracture, or degenerative scoliosis [20, 21]. Symptomatic ASDeg requiring reoperation was diagnosed as adjacent segment disease (ASDis). Radiographic fusion was assessed using Bridwell's grading criteria, and both grades I and II were considered radiographic signs of successful fusion, while grades III and IV vice versa [22]. Pedicle screw or cage loosening was defined as a radiolucency of ≥ 1 mm around the screw or the cage [23].
Statistical analysis
Data were analyzed using SPSS Statistics software (version 26.0, IBM Corp., Armonk, NY, USA). Statistical significance was set at a level of P < 0.05.
Continuous data are reported as mean values ± standard deviation. The assumption of normal distribution for the data was verified using the Shapiro–Wilk test. The independent samples t test and the Mann–Whitney U test were employed for intergroup comparison in each time point. The paired t test was used for the intra-group comparison of different time points. The Chi-square test was utilized to compare categorical variables between groups. Intraclass correlation coefficients (ICC) were calculated to evaluate the inter-rater reliability of radiographic assessments. ICC values below 0.5, between 0.5 and 0.75, between 0.75 and 0.9, and above 0.90 indicate poor, moderate, good, and excellent reliability, respectively.
Results
Demographics
A total of 312 patients initially met the inclusion and exclusion criteria. However, 31 patients (9.94%) were lost to follow-up. Among the remaining 281 patients, 123 underwent in situ fusion, while 158 underwent fusion with lever reduction (Fig. 3). The enrolled patients were followed up for an average duration of 29 months, ranging from 24 to 41 months. The gender distribution was similar in both groups, with the majority being female (NRG: 74.8% vs. RG: 70.9%, P = 0.466). Surgery at the L4-L5 level was the most common for both groups (NRG: 77.2% vs. RG: 70.9%, P = 0.231). Notably, there was a significant difference in operating time between the groups (NRG: 129.25 ± 27.41 min vs. RG: 138.04 ± 28.02 min, P = 0.009), while no statistically significant differences were observed in other demographic metrics (Table 1).
Patient-reported outcomes
In terms of back pain measured by the VAS, there was a remarkable reduction in NRG from 4.89 ± 1.45 preoperatively to 1.80 ± 1.32 postoperatively (P = 0.000) and 1.95 ± 1.12 at the final follow-up. Similarly, in RG, VAS back pain significantly improved from 5.06 ± 1.43 before surgery to 1.73 ± 1.21 (P = 0.000) postoperatively and 1.81 ± 1.14 at the last follow-up. However, no substantial differences in back pain intensity were observed between the two groups at corresponding evaluation time points. Following surgery, 70.7% of NRG patients and 78.5% of RG patients achieved MCID, though the statistical difference was not significant (P = 0.136) (Table 2).
When considering VAS leg pain, there was a decrease from 5.00 ± 1.82 to 1.84 ± 1.45 postoperatively (P = 0.000) and 1.56 ± 1.10 at the last follow-up in NRG. In RG, VAS leg pain decreased from 5.17 ± 1.74 before surgery to 1.78 ± 1.20 (P = 0.000) postoperatively and 1.73 ± 1.16 at the last follow-up. Comparable VAS leg pain scores were noted between groups at corresponding assessment time points. The proportion of patients achieving MCID was similar between NRG (78.0%) and RG (82.3%) without a statistically significant difference (P = 0.375) (Table 2).
A similar decreasing trend was evident in the ODI, with scores reducing from 49.40 ± 11.58 to 15.99 ± 11.08 postoperatively (P = 0.000) and 15.37 ± 8.99 at the last follow-up in NRG. In RG, preoperative ODI decreased from 48.61 ± 10.45 to 16.35 ± 9.07 postoperatively (P = 0.000) and 16.87 ± 6.28 at the last follow-up. No statistically significant differences were detected between groups at any assessment time points. The proportion of patients achieving MCID was similar between NRG (79.7%) and RG (80.4%), with no significant statistical difference (P = 0.883) (Table 2).
Radiological outcomes
Results of ICC analysis indicated good or excellent reliability for all radiographic assessments (SP: 0.771, FL: 0.816, LL: 0.901).
The preoperative SP was 21.68% ± 6.18% in NRG and 20.25% ± 6.46% in RG. This value significantly decreased to 16.85% ± 6.23% (P = 0.000) and 5.69% ± 4.31% (P = 0.000), respectively. At the final follow-up, SP increased to 19.70% ± 7.67% (P = 0.000) in NRG and 7.67% ± 4.43% (P = 0.000) in RG. Notably, patients who underwent fusion with lever reduction consistently exhibited significantly lower SP during the follow-up period compared to those who underwent in situ fusion (Table 3).
The preoperative FL was similar between the two groups (NRG: 11.58° ± 6.10° vs. RG: 12.68° ± 6.01°, P = 0.130). However, FL significantly increased to 13.99° ± 6.22° (P = 0.000) in NRG and 17.13° ± 5.90° (P = 0.000) in RG after surgery. There were no statistically significant differences in FL at the last follow-up compared to the postoperative values in both groups. Patients in the RG demonstrated greater FL both postoperatively and at the last follow-up compared to those in the NRG (Table 3).
Regarding LL, no statistically significant differences were observed at different time points within each group or at the same time point between the two groups (Table 3).
Complications and reoperations
A total of 90 complications were documented based on the MCDC classification, comprising 47 complication (Type I: 28, Type II: 16, Type III: 3) in the NRG and 43 complications (Type I: 24, Type II: 17, Type III: 2) in the RG, respectively. Patients undergoing in situ fusion demonstrated a higher incidence of ASDeg compared to those undergoing fusion with lever reduction (NRG: 9.8% vs. RG: 6.3%, P = 0.035). L4-5 reduction would be more beneficial in terms of prevention of ASDeg; however, a larger sample size is still needed to validate this finding. No significant differences were observed between the groups in the proportion of ASDis, cage malposition, cerebrospinal fluid leakage, unsuccessful fusion, residual pain or numbness, screw loosening, wound infection, and other general complications (Table 4).
Two patients, one from each group, required revision surgery due to ASDis. One patient in the NRG experienced recurrent pain caused by cage malposition 3 months postoperatively and resolved through reoperation. Wound infection was observed in two patients, with one case identified in each group, necessitating postoperative debridement.
Discussion
The necessity of a concomitant reduction procedure during the fusion surgery for DLS remains a controversial topic. Currently, conventional wisdom suggests that the reduction of spondylolisthesis holds theoretical appeal due to its potential for indirect decompression of neuroforamina and restoration of the sagittal lumbosacral alignment. Within this context, multiple reduction approaches, such translation reduction, distract and slip reduction, cantilever technique, or minimally invasive slip reduction, have been developed and utilized in the treatment of DLS [24,25,26,27]. However, the implementation of these methods relies upon adequate contact force between the instrumentation and vertebra and might instead result in implant-related complications, especially for elderly DLS patients with diminished bone quality. In response to these challenges, our clinical center introduced a novel lever reduction procedure in combination with transforaminal lumbar interbody fusion [14]. The present study compared the clinical efficacy, radiographic outcomes, and complications of in situ fusion versus fusion with lever reduction in a cohort of 281 patients. Results of our study highlighted the benefits associated with lever reduction in terms of restoring segmental sagittal alignment and reducing complications, while no superiority of the additional reduction procedure over in situ fusion in improving clinical outcomes was exhibited.
The impact of reduction on clinical outcomes in lumbar spondylolisthesis remains uncertain, as comparative studies have yielded conflicting results. A randomized trial conducted by Lian et al. involving 73 patients with DLS revealed similar postoperative VAS, ODI, and Japanese Orthopedic Association (JOA) scores between patients who underwent fusion with or without reduction [6]. Another study involving 65 patients with symptomatic spondylolisthesis, conducted by Heo et al., demonstrated that intraoperative reduction led to greater improvements in ODI after surgery [8]. Conversely, Tay et al. did not find any significant clinical benefits associated with reduction in cohorts with low-grade spondylolisthesis [23]. Regarding high-grade spondylolisthesis, a recent meta-analysis indicated that slip reduction correlated with more substantial overall enhancements in ODI when compared to in situ fusion [28]. In our current investigation, we did not identify a connection between spondylolisthesis reduction and improvements in clinical outcomes or an increased proportion of patients achieving the MCID (Table 2). Considering that the majority of patients in this study showed only slight degenerative spondylolisthesis, one plausible explanation for this result might be that the indirect decompression effect resulting from reduction was marginal when contrasted with the direct decompression achieved during the fusion procedure. Therefore, the reduction procedure had minimal effect on clinical improvement.
In line with previous findings, our results also indicate that the focal lordosis increases significantly as the spondylolisthesis percentage decreases [6, 8]. In contrast, the overall lumbar lordosis shows variation with no substantial differences across the three assessment time points, whether reduction was performed or not (Table 3). From a practical standpoint, establishing a connection between the restoration of spinal alignment and the perceived enhancements in treatment effectiveness for patients is crucial. In a prospective study enrolling 57 patients with DLS who underwent lumbar fusion surgery, Kuhta et al. reported that obtaining adequate SL was correlated with favorable ODI 5 years postoperatively [29]. Similarly, Takahashi et al. showed that DLS patients with a higher increase in SL were predisposed to a higher JOA recovery rate after lumbar fusion surgery for DLS [30]. On the contrary, loss of overall lumbar lordosis resulted in a higher risk of poor clinical outcomes [31]. Therefore, despite our inability to identify a statistical distinction in clinical outcomes between NRG and RG as mentioned earlier, the significance of the reduction procedure remains worthy of contemplation since it both improves segmental morphology and maintains overall lordosis, which provides potential therapeutic benefit in patients with DLS.
The choice of the most appropriate surgical plan for a surgeon can be influenced by the complications associated with various surgical techniques. However, there remains a lack of consensus regarding the definition and grading of complications arising from spine surgeries. In this study, all complications were categorized according to the MCDC system [19]. The results indicated that patients undergoing fusion with lever reduction were inclined to experience a lower overall complication rate and MCDC Type I complication rate compared to those undergoing in situ fusion, although this difference was not statistically significant. Regarding specific categories, the reduction technique exhibited a distinct advantage in reducing the incidence of ASDeg compared to in situ fusion (Table 4). This difference might be attributed to the increased FL resulting from the reduction procedure. As reported in previous studies, the proper restoration of FL curbs the compensatory increase in mobility and loading at the adjacent fused segment, thereby delaying the degeneration process [32, 33]. Moreover, the additional stresses during the reduction maneuvers might induce a higher risk of screw loosening or even pullout, as previously reported [6, 34]. Nonetheless, such negative effects were not evident in patients who underwent fusion with the lever reduction procedure in our research (Table 4). The lever device's distractive force can mitigate the pull force exerted on the instrumentation to some extent, potentially leading to fewer implant-related complications [14]. Considering these factors collectively, the superiority of fusion with lever reduction is primarily manifested in reducing the risk of complications rather than enhancing patient-reported outcomes. We believe that fusion with lever reduction could emerge as a viable alternative for DLS patients and is worthy of application, contributing to an enhanced long-term prognosis.
Our study has certain limitations that need to be acknowledged. Firstly, the retrospective nature of our study made it challenging to completely eliminate selection bias and attrition bias. Secondly, the decision to pursue lever reduction was primarily influenced by surgeon preferences and, in some cases, the availability of the lever reduction device. This introduces the possibility of unmeasured factors affecting the decision-making process, not accounted for in our study. Thirdly, only patients undergoing fusion with lever reduction and in situ fusion were included in the analysis. Therefore, the present study cannot conclusively prove the superiority or inferiority of lever reduction technique compared to other reduction techniques. The ongoing data collection of relevant research may address this gap in the future. Lastly, it is important to note that our cohort size was relatively small, which might marginally impact the robustness of our conclusions. Despite these limitations, our study yields valuable insights into the efficacy and safety of the innovative lever reduction technique for DLS. Furthermore, it contributes previously unavailable data that can help reconcile the ongoing debate surrounding fusion options with or without reduction.
Conclusions
We conducted a comparison of clinical effectiveness, radiological outcomes, and complications between fusion with and without the innovative lever reduction technique in a group of 281 patients with DLS. There were no significant differences in postoperative measures such as VAS scores for back and leg pain, ODI, the ability to reach MCID, overall complication rate, or specific complication rates per MCDC between surgical approaches. However, a notable advantage was observed in fusion with lever reduction compared to in situ fusion in terms of restoring segmental spinal sagittal alignment and reducing the occurrence of ASDeg. In the long-term perspective, fusion with lever reduction might be a considerable alternative for the treatment of DLS.
Availability of data and materials
The datasets are used and/or analyzed during the current study available from the corresponding author on reasonable request.
Abbreviations
- DLS:
-
Degenerative lumbar spondylolisthesis
- RG:
-
Reduction group
- NRG:
-
Non-reduction group
- VAS:
-
Visual analog scale
- ODI:
-
Oswestry Disability Index
- MCID:
-
Minimal clinically important difference
- SP:
-
Spondylolisthesis percentage
- FL:
-
Focal lordosis
- LL:
-
Lumbar lordosis
- MCDC:
-
Modified Clavien–Dindo classification
- ASDeg:
-
Adjacent segment degeneration
- ASDis:
-
Adjacent segment disease
- JOA:
-
Japanese Orthopedic Association
References
Wiltse LL. The etiology of spondylolisthesis. J Bone Jt Surg Am. 1962;44-a:539–60.
Wang YXJ, Káplár Z, Deng M, Leung JCS. Lumbar degenerative spondylolisthesis epidemiology: a systematic review with a focus on gender-specific and age-specific prevalence. J Orthop Translat. 2017;11:39–52.
Sengupta DK, Herkowitz HN. Degenerative spondylolisthesis: review of current trends and controversies. Spine (Phila Pa 1976). 2005;30(6 Suppl):S71–81.
Kornblum MB, Fischgrund JS, Herkowitz HN, Abraham DA, Berkower DL, Ditkoff JS. Degenerative lumbar spondylolisthesis with spinal stenosis: a prospective long-term study comparing fusion and pseudarthrosis. Spine (Phila Pa 1976). 2004;29(7):726–33.
Turunen V, Nyyssönen T, Miettinen H, Airaksinen O, Aalto T, Hakumäki J, Kröger H. Lumbar instrumented posterolateral fusion in spondylolisthetic and failed back patients: a long-term follow-up study spanning 11–13 years. Eur Spine J. 2012;21(11):2140–8.
Lian XF, Hou TS, Xu JG, Zeng BF, Zhao J, Liu XK, Zhao C, Li H. Posterior lumbar interbody fusion for aged patients with degenerative spondylolisthesis: is intentional surgical reduction essential? Spine J. 2013;13(10):1183–9.
Kawakami M, Tamaki T, Ando M, Yamada H, Hashizume H, Yoshida M. Lumbar sagittal balance influences the clinical outcome after decompression and posterolateral spinal fusion for degenerative lumbar spondylolisthesis. Spine (Phila Pa 1976). 2002;27(1):59–64.
Heo DH, Jang JW, Lee JK, Park CK. Slippage reduction of lumbar spondylolisthesis using percutaneous pedicle screw with reduction fixation system after interbody fusion: a comparison with traditional open fusion and pedicle screw fixation. J Clin Neurosci. 2019;67:156–62.
Park B, Noh SH, Park JY. Reduction and monosegmental fusion for lumbar spondylolisthesis with a long tab percutaneous pedicle screw system: “swing” technique. Neurosurg Focus. 2019;46(5):E11.
Scheer JK, Auffinger B, Wong RH, Lam SK, Lawton CD, Nixon AT, Dahdaleh NS, Smith ZA, Fessler RG. Minimally invasive Transforaminal Lumbar Interbody Fusion (TLIF) for spondylolisthesis in 282 patients: in situ arthrodesis versus reduction. World Neurosurg. 2015;84(1):108–13.
Martiniani M, Lamartina C, Specchia N. “In situ” fusion or reduction in high-grade high dysplastic developmental spondylolisthesis (HDSS). Eur Spine J. 2012;21(Suppl 1):S134-140.
Petraco DM, Spivak JM, Cappadona JG, Kummer FJ, Neuwirth MG. An anatomic evaluation of L5 nerve stretch in spondylolisthesis reduction. Spine (Phila Pa 1976). 1996;21(10):1133–8.
Floman Y, Millgram MA, Ashkenazi E, Smorgick Y, Rand N. Instrumented slip reduction and fusion for painful unstable isthmic spondylolisthesis in adults. J Spinal Disord Tech. 2008;21(7):477–83.
Kong C, Wang W, Li X, Sun X, Ding J, Lu S. A new lever reduction technique for the surgical treatment of elderly patients with lumbar degenerative spondylolisthesis. BMC Musculoskelet Disord. 2020;21(1):11.
Jensen MP, Chen C, Brugger AM. Interpretation of visual analog scale ratings and change scores: a reanalysis of two clinical trials of postoperative pain. J Pain. 2003;4(7):407–14.
Fairbank JC, Pynsent PB. The oswestry disability index. Spine (Phila Pa 1976). 2000;25(22):2940–52.
McGlothlin AE, Lewis RJ. Minimal clinically important difference: defining what really matters to patients. JAMA. 2014;312(13):1342–3.
Parker SL, Adogwa O, Paul AR, Anderson WN, Aaronson O, Cheng JS, McGirt MJ. Utility of minimum clinically important difference in assessing pain, disability, and health state after transforaminal lumbar interbody fusion for degenerative lumbar spondylolisthesis. J Neurosurg Spine. 2011;14(5):598–604.
Dindo D, Demartines N, Clavien PA. Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg. 2004;240(2):205–13.
Bae JS, Lee SH, Kim JS, Jung B, Choi G. Adjacent segment degeneration after lumbar interbody fusion with percutaneous pedicle screw fixation for adult low-grade isthmic spondylolisthesis: minimum 3 years of follow-up. Neurosurgery. 2010;67(6):1600–7.
Cheh G, Bridwell KH, Lenke LG, Buchowski JM, Daubs MD, Kim Y, Baldus C. Adjacent segment disease following lumbar/thoracolumbar fusion with pedicle screw instrumentation: a minimum 5-year follow-up. Spine (Phila Pa 1976). 2007;32(20):2253–7.
Bridwell KH, Lenke LG, McEnery KW, Baldus C, Blanke K. Anterior fresh frozen structural allografts in the thoracic and lumbar spine. Do they work if combined with posterior fusion and instrumentation in adult patients with kyphosis or anterior column defects? Spine (Phila Pa 1976). 1995;20(12):1410–8.
Tay KS, Bassi A, Yeo W, Yue WM. Intraoperative reduction does not result in better outcomes in low-grade lumbar spondylolisthesis with neurogenic symptoms after minimally invasive transforaminal lumbar interbody fusion-a 5-year follow-up study. Spine J. 2016;16(2):182–90.
Ruf M, Koch H, Melcher RP, Harms J. Anatomic reduction and monosegmental fusion in high-grade developmental spondylolisthesis. Spine (Phila Pa 1976). 2006;31(3):269–74.
Hart RA, Domes CM, Goodwin B, D’Amato CR, Yoo JU, Turker RJ, Halsey MF. High-grade spondylolisthesis treated using a modified Bohlman technique: results among multiple surgeons. J Neurosurg Spine. 2014;20(5):523–30.
Bouras T, Korovessis P. Management of spondylolysis and low-grade spondylolisthesis in fine athletes. A comprehensive review. Eur J Orthop Surg Traumatol. 2015;25(Suppl 1):S167–75.
Isaacs RE, Sembrano JN, Tohmeh AG. Two-year comparative outcomes of MIS lateral and MIS transforaminal interbody fusion in the treatment of degenerative spondylolisthesis: part II: radiographic findings. Spine (Phila Pa 1976). 2016;41(Suppl 8):S133–44.
Lak AM, Abunimer AM, Devi S, Chawla S, Aydin L, Tafel I, Smith TR, Mekary RA, Zaidi HA. Reduction versus in situ fusion for adult high-grade spondylolisthesis: a systematic review and meta-analysis. World Neurosurg. 2020;138:512-520.e512.
Kuhta M, Bošnjak K, Vengust R. Failure to maintain segmental lordosis during TLIF for one-level degenerative spondylolisthesis negatively affects clinical outcome 5 years postoperatively: a prospective cohort of 57 patients. Eur Spine J. 2019;28(4):745–50.
Takahashi Y, Okuda S, Nagamoto Y, Matsumoto T, Sugiura T, Iwasaki M. Effect of segmental lordosis on the clinical outcomes of 2-level posterior lumbar interbody fusion for 2-level degenerative lumbar spondylolisthesis. J Neurosurg Spine. 2019;31:670–5.
Makino T, Kaito T, Fujiwara H, Honda H, Sakai Y, Takenaka S, Yoshikawa H, Yonenobu K. Risk factors for poor patient-reported quality of life outcomes after posterior lumbar interbody fusion: an analysis of 2-year follow-up. Spine (Phila Pa 1976). 2017;42(19):1502–10.
Okuda S, Nagamoto Y, Takenaka S, Ikuta M, Matsumoto T, Takahashi Y, Furuya M, Iwasaki M. Effect of segmental lordosis on early-onset adjacent-segment disease after posterior lumbar interbody fusion. J Neurosurg Spine. 2021;35(4):454–9.
Tian H, Wu A, Guo M, Zhang K, Chen C, Li X, Cheng X, Zhou T, Murray SS, Sun X, et al. Adequate restoration of disc height and segmental lordosis by lumbar interbody fusion decreases adjacent segment degeneration. World Neurosurg. 2018;118:e856–64.
Lian XF, Hou TS, Xu JG, Zeng BF, Zhao J, Liu XK, Yang EZ, Zhao C. Single segment of posterior lumbar interbody fusion for adult isthmic spondylolisthesis: reduction or fusion in situ. Eur Spine J. 2014;23(1):172–9.
Acknowledgements
Not applicable.
Funding
This subject was supported by grants from Bei**g Hospitals Authority Ascent Plan (DFL20190802) and Bei**g Hospitals Authority Clinical Medicine Development of special funding support (XMLX202116).
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design. CK and DW helped in writing, reviewing, editing; WW and YW contributed to radiographic data measurement, methodology and data curation; SL supervised and guided the study. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
All procedures performed in this study involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards. Informed consents were obtained from all participants in the study. All experiments were performed in accordance with relevant guidelines and regulations. All experimental protocols were approved by the Ethics Committee of the Xuanwu Hospital Capital Medical University.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Kong, C., Wang, D., Wang, W. et al. Fusion with and without lever reduction in degenerative lumbar spondylolisthesis: a retrospective study. J Orthop Surg Res 19, 17 (2024). https://doi.org/10.1186/s13018-023-04507-9
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13018-023-04507-9