Abstract
Background
The distal tibiofibular syndesmosis (DTS) is a complex fibrous joint that contributes to the stability and weight-bearing function of the ankle. As such, repair of DTS injury is required, providing fixation strength while maintaining ankle range of motion. The aim of this study was to compare a new elastic fixation technique, using an encircling and binding technique, for DTS stabilization, compared to the traditional cortical bone screw fixation.
Methods
This was a retrospective analysis of 67 patients treated for a DTS injury at our hospital, between June 2019 and June 2021. Of them, 33 were treated with encircling and binding (EB group) and 34 using a cortical screw (CS group). The following outcomes were compared between groups: time to inferior tibiofibular fixation; length of hospital stay; time to partial weight bearing; time to complete weight bearing; complications; imaging data; and functional scores.
Results
Successful stabilization was achieved in all cases, with a mean follow-up period of 15.78 ± 2.97 months. Time to fixation and time to partial and complete weight bearing were shorter for the EB than that for the CS group. The length of hospital was not different between groups. With regard to complications, a superficial infection developed in one patient in each group, with wound healing achieved after active treatment. Screw fracture occurred in two patients in the CS group. At 3 months post-surgery, the American Foot Surgery Association Ankle-Hindfoot score (AOFAS) was higher and the pain score lower for the EB than that for the CS group, but with no between-group difference at the final follow-up. On imaging, the tibiofibular clear space and tibiofibular overlap were not different between groups.
Conclusions
DTS fixation using encircling and binding yielded better clinical and functional outcomes than did cortical screw fixation at 3 months post-surgery, with no difference at the final follow-up. This novel fixation technique provides firm fixation, combined with earlier return to postoperative exercise and recovery of ankle function.
Similar content being viewed by others
Background
The stability of the distal tibiofibular syndesmosis (DTS) complex, which contributes to the stability and load-bearing capacity of the ankle joint, is provided by the anterior inferior tibiofibular, posterior inferior tibiofibular, inferior transverse, and interosseous ligaments [1]. Injury to any two of these ligaments will result in ankle joint instability, with a change in the contact area of the tibiotalar joint surface. Dattani et al. [2] demonstrated that a 1-mm displacement of the talus within the ankle mortise can reduce the tibiotalar contact area by 42%, aggravate articular cartilage wear, and lead to complications, such as chronic pain, traumatic arthritis, and ankle instability. Anatomical reduction and rigid internal fixation for a DTS injury is thus required.
Fixation using a cortical screw has been considered the gold standard for treatment of a DTS injury, providing a local stable environment, with restraint against external rotational stress, to allow remodeling of the ligaments [3]. However, as the DTS is a fibrous joint, with a range of motion (ROM) of 2–5° along all three planes of motion, coronal, sagittal, and transverse [4], the screw must be removed before weight bearing to avoid metal fatigue, which can lead to screw fracture. This complication can increase the risk of perioperative infection, functional ankle joint impairments, and the economic burden to patients. Moreover, owing to the hardness of cortical screws, any deviation in the placement of the screw can result in misalignment of the fibula in the fibular notch and in ankle stiffness. This is an important clinical issue considering that the incidence of poor reduction of the DTS is high, at 25.5–52% for medial collateral ligament (MCL) injuries [5]. As such, the use of rigid fixation for DTS injuries has gradually been replaced by elastic fixation to retain a certain ROM while satisfying the requirement for strength of the fixation and to avoid the related complications caused by long-term rigid fixation [6, 7].
Different types of elastic fixation techniques have been described, including autogenous ligament repair, artificial ligament repair, rivet technique, endo-button system, and suture-button system [8,9,10]. Among these, the suture-button system has been associated with good imaging outcomes and ankle function scores on follow-up; however, complications, such as sinking of the internal fixation device, osteolysis, and enlargement of tibial boreholes, have been reported [8, 11]. The above has highlighted the importance of the DTS for ankle stability and the need for anatomic reduction and strong internal fixation for surgical treatment. Currently, the commonly used fixation methods have their own advantages and disadvantages. How to have a fixation method that can not only achieve the fixed strength of rigid fixation but also satisfy the elastic fretting of the joint under the premise of few complications is still a hot topic in the research of foot and ankle surgery.
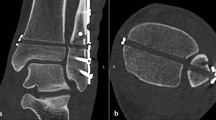
The strength of the elastic fixation can be improved by using a nice knot, which is a double-layer folding and sliding knot that provides high tension and stable fixation, which is maintained over time, while resisting fatigue of the fixation and retaining the ROM characteristics of the DTS joint [12,13,Full size image
Postoperative management
After surgery, a cotton gauze bandage was applied with an elastic wrap, and the limb was elevated. Routine anti-inflammation, detumescence, and pain relief were provided. At 24 h postoperatively, active ankle ROM in flexion/extension was initiated, with a gradual increase in exercise intensity. Weight bearing was initiated at 8 weeks postoperatively, progressing to full weight bearing as tolerated.
Evaluation index
The following outcomes were evaluated: intraoperative time of fixation of the DTS; operative time; length of hospital stay; time to partial weight bearing; and time to full weight bearing. During the follow-up period, complications such as incision infection, poor wound healing, deep venous thrombosis, loosening of the elastic fixation device, fracture of the inferior tibiofibular screw, and loss of reduction were closely monitored. Patient-reported outcomes included the visual analog scale (VAS) for pain and the American Foot Surgery Association Ankle-Hindfoot Score (AOFAS) for pain, function, and objective measurement of alignment. The reduction criteria were evaluated according to the measurement of the tibiofibular space (TFCS) and inferior tibiofibular overlap distance (TFOS) on radiographs obtained immediately after surgery and at the last follow-up.
Statistical analysis
Data were reported as the mean and standard deviation. Between-group differences were evaluated using an independent sample t-test for continuous data and the Chi-squared (X2) or Fisher’s exact test for categorical data. Within-group comparison between time points was evaluated using paired-sample t-test or one-way analysis of variance for normally distributed data and a rank sum test for non-normally distributed data. A p value < 0.05 was significant. All analyses were performed using SPSS (version 26.0).