Abstract
The role of cytoplasmic fragmentation in human embryo development and reproductive potential is widely recognized, albeit without standard definition nor agreed upon implication. While fragmentation is best understood to be a natural process across species, the origin of fragmentation remains incompletely understood and likely multifactorial. Several factors including embryo culture condition, gamete quality, aneuploidy, and abnormal cytokinesis seem to have important role in the etiology of cytoplasmic fragmentation. Fragmentation reduces the volume of cytoplasm and depletes embryo of essential organelles and regulatory proteins, compromising the developmental potential of the embryo. While it has been shown that degree of fragmentation and embryo implantation potential are inversely proportional, the degree, pattern, and distribution of fragmentation as it relates to pregnancy outcome is debated in the literature. This review highlights some of the challenges in analysis of fragmentation, while revealing trends in our evolving knowledge of how fragmentation may relate to functional development of the human embryos, implantation, and pregnancy outcome.
Similar content being viewed by others
Introduction
Human preimplantation embryo scoring systems have been widely used to predict blastocyst development and implantation rate after in-vitro fertilization (IVF). The grading of embryos on day-2 and -3 after fertilization is largely subjective and interpretation varies across IVF laboratories, as it is commonly based on morphological appearance. Characteristics in early embryo grading schema include the amount of cytoplasmic fragmentation (CF) during early cleavage, speed of cellular division, number, size, and symmetry of cells (blastomeres). As defined by the Istanbul consensus workshop on embryo assessment, a fragment is “an extracellular membrane-bound cytoplasmic structure that is < 45 µm diameter in a day-2 embryo and < 40 µm diameter in a day-3 embryo” [1]. There are several different systems to evaluate embryo morphology including Hill’s scoring system [2] Cummins' grading system [3] ASEBIR grading system [1], the UK/ACE grading scheme [4]; each system has its own classification for degree of fragmentation as well as embryo grade. This heterogeneity further complicates analysis of fragmentation in relation to outcomes.
CF has been shown to occur early in embryonic division and is a common phenomenon seen in embryos cultured in vitro. CF has traditionally been used as a metric of embryo implantation potential [3, 5,6,7]. The amount and pattern of fragments are analyzed in early development, incorporated into the embryo grade depending on grading system, and used to help select the most developmentally competent embryo to be transferred during an IVF cycle. This classification system is important as a proportion of embryos within a single cohort will not successfully develop to the blastocyst stage in vitro. Although there are various contributing factors to an embryo’s developmental capacity and viability, it is largely agreed upon that fragmentation plays an important role. It seems that the etiology of embryo fragmentation is not fully understood but it may be related to several factors like gamete quality, culture condition, and genetic abnormalities in the embryo [8]. It is difficult to directly compare and quantify relative degrees of fragmentation across studies. However, it has been repeatedly shown that the extent of fragmentation and implantation potential are inversely proportional [5, 7, 9,10,11,12,13,14,15,16,17,18,19,20,21]. While a low degree of fragmentation does not seem to significantly impact embryo viability, severe fragmentation does [7, 22, 23]. Alongside the cell to cytoplasmic ratio, the pattern and distribution of fragmentation influence the developmental quality of the embryo [7, 24]. There are two main patterns of embryo cytoplasmic fragments: scattered and concentrated. The former is characterized by fragment contact within several blastomeres and is related to aneuploidy [25]. Time-lapse studies have shown that fragmentation is thought to be a dynamic process, where some fragments can be expelled or reintroduced into the cells as the embryo continues to divide [25, 26]. Fragments can also easily move or rotate around the associated blastomere and change their position in the embryo [27].
Current grading systems used to evaluate cleavage-stage embryos are largely based on day-2 or -3 morphology. This can be problematic, as developmental growth of an embryo is variable and the grade of a develo** embryo at one point in time is not guaranteed to persist. For example, studies have suggested that embryo selection on day-2 or -3 based on morphological grade can be unreliable and lead to negative pregnancy outcomes [28,29,30]. Accordingly, new parameters for predicting implantation success have been proposed including extended embryo culture to the blastocyst stage to day-5, -6 or -7 [31]. Delaying embryo transfer to the blastocyst stage is advantageous as it can limit the number of unsuccessful embryo transfers and biochemical pregnancies or clinical pregnancy losses in IVF. While there are multiple reports on the impact of cleavage-stage embryo quality on blastocyst formation and blastocyst quality [32, 33], few have specifically looked at the degree of fragmentation as a predictive variable.
In this systematic review, we comprehensively reviewed the available literature on the origin and characteristics of CF, factors affecting CF, and the effect of CF and fragment removal on embryo development and pregnancy rate.
Materials and methods
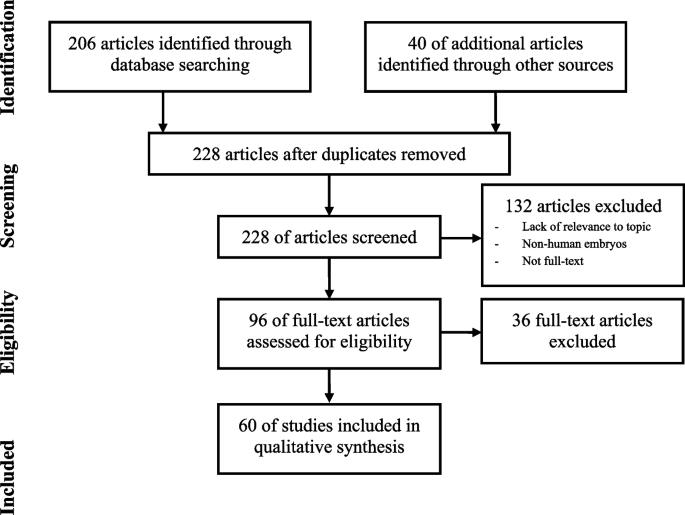
A search was conducted on October 10, 2023, using PubMed and Google Scholar databases in accordance with Preferred Reporting Items for Systematic Reviews and Meta-Analysis guidelines [34]. In PubMed, the search terms “embryo*[tw] OR cleavage stage [tw] OR "Embryonic Structures"[Mesh] OR "Embryonic Development"[Mesh] OR "Embryo, Mammalian"[Mesh] OR "Cleavage Stage, Ovum"[Mesh]” AND “cytoplasm*[tw] AND fragment*[tw] AND “(Blastocyst*[tw] OR "Blastocyst"[Mesh]) AND (form* OR develop* OR quality*)” were used. A title search in Google Scholar using search terms as above and “embryo cytoplasm fragmentation”, “blastocyst quality”, “blastocyst development” was performed. Only full-text publications in English were included. Full-text articles which did not have any mention of cytoplasmic or embryo fragmentation were excluded, however articles which mentioned both DNA fragmentation and CF were included. Since most of the studies discussing CF also discussed other morphologic features of the embryo, studies that mention embryo morphology, grade or quality were also included. Articles that looked at non-human embryo fragmentation, case reports, case series, book chapters and review papers were excluded. Titles and abstracts were screened, and study quality and bias were assessed. The primary outcomes of interest were embryo quality, blastocyst formation, and pregnancy outcome.
Results
Figure 1 provides details of study screening and inclusion. There were 206 studies screened between the two search engines PubMed (n=106) and Google Scholar (n=100). There were 18 duplicates giving a total of 188 articles. Due to the small number of studies from the search criteria, no filter of time was placed. After removal of non-full text articles, articles that used non-human embryos, and articles not relevant to the topic, 20 articles were eligible for inclusion. Forty relevant references from the articles were also extracted, reviewed, and included in this review. These additional articles were reviewed with the same inclusion and exclusion criteria as mentioned above. A total of 60 articles were included in the qualitative synthesis of this review.
Origin and etiology of CF
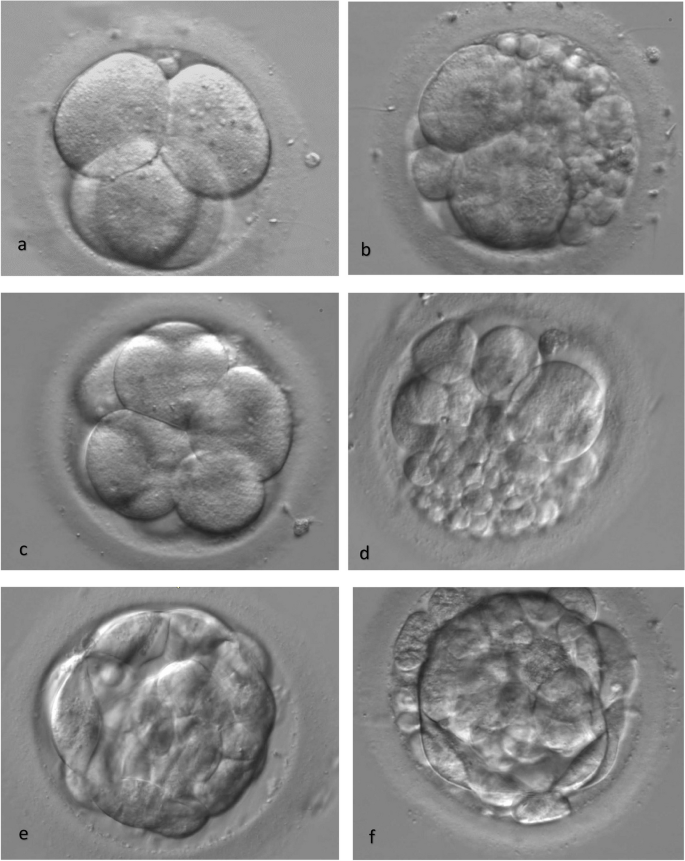
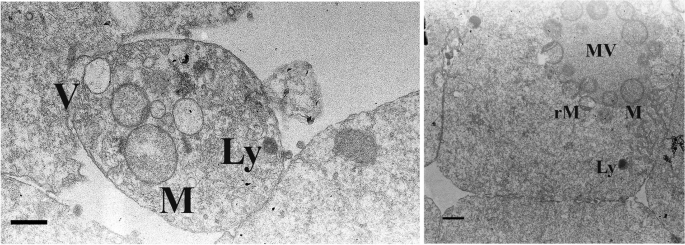
The etiology of CF is not completely understood. There are several proposed theories as to why embryos display variable degrees of fragmentation. Fragmentation has been shown to be a natural, unpredictable process both in vitro and in vivo and is documented in various species [35, 36]. This suggests that embryo fragmentation is neither species-specific nor solely a byproduct of in vitro culture. Assisted reproductive technology (ART) and IVF techniques, such as time-lapse microscopy (TLM) and transmission electron microscopic (TEM) analyses, have recently allowed for further understanding of embryo developmental potential and fragmentation (Figs. 2 and 3). Seven of the included studies in this review propose potential hypotheses as to the origin of CF (Table 1). Three of the articles evaluated gamete quality as related to fragmentation in a develo** embryo [37,38,39].
An early study showed that sperm DNA oxidation has been associated with embryo development and quality, and therefore linked to CF [37]. Nucleolar asynchrony in the zygote from sperm DNA fragmentation has previously been shown to predict future low-quality blastocyst development. A positive correlation has also been found between the percentage of sperm OxiDNA-stained cells with embryo fragmentation on day-2 and -3 of development. Sperm DNA oxidation may therefore be associated with fragmented, nonviable, poor-quality embryos [37] . A recent study also showed the negative correlation between sperm DNA fragmentation and blastomere DNA fragmentation and blastulation rate [40]. Further studies are needed to confirm the impact of sperm DNA oxidation on embryo fragmentation.
An observational study documented the degree of fragmentation of human embryos as they progressed through mitotic cell cycles [38]. In this study, the authors analyzed nearly 2,000 oocytes and 372 embryos, and found that increased embryo fragmentation (>50%) was associated with a specific pattern of development: delayed first division (oocyte spindle detected at 36.2 hours after hCG injection vs. 35.5 hours in low fragmentation), a significantly earlier start of the second mitosis (8.9 hours vs. 10.8 hours after the first mitosis), and a significant delay of the third mitosis after the second mitosis (2.2. hours vs. 0.6 hours). The authors did not comment on whether fragmentation could be a result of the cell dividing before proper chromosome alignment, or if existing aneuploidy resulted in erroneous cleavage patterns [38].
Polar body (PB) fragmentation has also been investigated in relation to cytoplasmic fragmentation. Ebner et al., in a prospective study analyzed the relationship between a fragmented first PB and embryo quality in patients undergoing ICSI. Two groups of oocytes were analyzed according to PB fragmentation: intact first PBs and those with fragmented PBs. Forty-two hours after ICSI, embryo morphology (i.e., number of blastomeres and degree of fragmentation) was recorded. Overall, a significantly higher percentage of cytoplasmic fragmentation was seen in day-2 embryos that originated from oocytes with fragmented first PBs than those with intact PBs (P < 0.05). This study further supports the concept that oocyte quality contributes to overall embryo fragmentation and provides evidence that preselection of oocytes may contribute to the prognosis of embryo quality and blastocyst development [39]. The role of PB fragmentation on embryo quality was confirmed in other studies [41, 42], however, a recent study has not recommended considering PB status as a tool for embryo selection [43].
Beyond analysis of gamete quality, other studies have shown a biochemical relationship between embryo competence and fragmentation. One study showed that disturbances in E-cadherin, a cell adhesion protein that plays a critical role in morphogenesis, occur in embryos with cleavage abnormalities and extensive cytoplasmic fragmentation, suggesting a possible mechanism to the loss of embryonic viability [44]. Further, by using mitochondrial fluorescence techniques, Van Blerkom et al., found that mitochondrial distribution at the pronuclear stage may be an epigenetic factor related to the organization of the embryo and further embryonic development [45]. Blastomeres that were deficient in mitochondria and thus ATP at the first or second cell division remained undivided and often died during subsequent culture. Although this study examined morphologically normal (unfragmented) cleavage-stage embryos, it may support the idea that perinuclear mitochondrial distribution and microtubular organization influence developmental capacity of early cleavage-stage embryos [45]. Higher numbers of mitochondria reported in fragmented compared to the normal blastomeres show the rapid depletion of ATP in the fragmented embryos [21]. There have also been reports of increased gene transcription of mitochondrial factors like OXPHOS complexes, ATP synthase, and mtDNA content in highly fragmented embryos compared to controls [46]. Mitochondrial activity is lower and more centralized in fragmented embryos compared to good quality embryos on day-3 [47]. Mitochondria are the main source of ATP for embryo mitosis, and their proper function is essential for embryo development. More research is needed to elucidate the morphology and role of mitochondria in embryo development, especially in relation to fragmentation.
A subsequent study by Van Blerkom et al., analyzed the temporal and spatial aspects of fragmentation through TLM and TEM analyses from the pronuclear to the 10-12-cell stage. Through TLM, the authors visualized the non-discrete, dynamic nature of fragments and noted that many were “bleb-elaborations” of the plasma membrane and cytoplasm. They characterized two patterns of fragmentation: definitive and pseudo-fragmentation. Definitive fragmentation was described as fragments detached from a blastomere, and pseudo-fragmentation was assigned when the fragments were no longer detectable during subsequent development. Often one develo** embryo would show both fragmentation patterns at different stages of development, suggesting that these patterns may have different etiologies and effects on embryo development competence [47]. Hardarson et al., similarly used TLM to document that fragments are dynamic and can be internalized throughout cleavage during culture periods. The contents of the fragments were noted to be internalized and released into the cytoplasm of the blastomere and seen on multiple time-lapse photographs as a cytoplasmic turbulence. This is the first reported evidence that cellular fragments can “disappear” during the culture period in human IVF [26]. It seems that in mild to moderate CF, the timing of embryo evaluation and grading can affect the reported percent of fragmentation.
Lastly, we have included a preliminary study performed by Sermondade et al., that suggests a specific subgroup of patients who have had repeated IVF failures (presumably due to a recurring high rate of fragmented embryos) may benefit from early intrauterine embryo transfer at the zygote stage (2PN) [48]. Data showed a delivery rate per oocyte retrieval of 18.9%, which was significantly higher than the delivery rate of 7.5% in the matched control group. The results were encouraging and suggestive of a safe, non-invasive rescue strategy for patients who experience recurrent highly fragmented embryos and failed IVF attempts. The data further suggests that fertilized oocytes of this subgroup may have deficiencies in certain maternal factors (i.e., stress-response factors) that do not allow normal embryo development in culture environments [48]. Another study was also confirmed application of zygote transfer in patients with history of low-quality embryos [49]. However, further studies are required to verify the impact of this technique for patients with history of fragmented embryos.
Apoptosis is another proposed etiology of fragmentation. Apoptosis may occur in blastomeres with defective cytoplasm or abnormal chromosomes, leading to embryo fragmentation [50]. There are several studies reporting apoptosis in both fragments and neighboring blastomeres in a fragmented embryo [24, 50]. Chi et al., showed that fragments are associated with both apoptosis and necrosis [21]. One of the factors that appears to induce apoptosis in blastomeres is suboptimal culture conditions such as hypoxia [51]. In addition, there are controversial reports on the role of reactive oxygen species (ROS) in embryo fragmentation [52, 53]. It has been shown that ROS are present at high levels in the culture media of fragmented embryos [52, 54]. Chen et al., recently showed that embryo culture in 5% oxygen, from days 1 to 3, is associated with higher embryo quality and live birth rate compared to 20% oxygen [55]. The effects of culture condition modifications, such as hypoxia and ROS, on embryo fragmentation need to be clarified to understand the importance of culture condition in this process.
Membrane compartmentalization of DNA, abnormal cytokinesis, and extra vesicular formation are other proposed theories for embryo fragmentation [8]. Defects or damages in mitochondria are associated with low ATP and high ROS production leading to a compromised cell division and cytokinesis [27]. In addition, there is a correlation between embryo fragmentation and ploidy status. Chavez et al., showed that CF was seen in a high proportion of aneuploid embryos, and that meiotic and mitotic errors may cause fragmentation in different cell development stages. Meiotic errors were associated with fragmentation at one-cell stage while mitotic errors were associated with fragmentation at interphase or after first cytokinesis [56]. Chromosomally abnormal embryos often have severe fragmentation, which may be another cause of CF [55, 57].
Overall, the precise cause of CF has yet to be clearly defined. The above investigations have elucidated potential sources and associations of what is likely a complex and multifactorial process and represent our current understanding of CF origin.
What is contained in CF?
Four of the included studies used various technological advances to study the contents of CF in human embryos (Table 2). Two studies used TEM methods to evaluate fragment ultrastructure (Fig. 3) [21, 58]. Fragments were extracted from embryos with 10-50% fragmentation and the ultrastructure evaluated by TEM. Micrographs showed that the fragments had a distinct membrane containing cytoplasmic organelles including mitochondria, mitochondria-vesicle complexes, Golgi apparatus, primary lysosomes, and vacuoles. Mitochondria were the most abundant structure.
In an additional evaluation of CF contents, Johansson et al., analyzed DNA content of fragments to define a cutoff diameter for an anucleate fragment or blastomere. Findings showed that 98% of fragments <45 µm on day-2 and 97% of those <40 µm on day-3 contained no DNA and, if not reabsorbed into a blastomere, showed a loss of cytoplasm. Presence of essential blastomere organelles such as mitochondria, mRNA, and proteins within cytoplasmic fragments were related to embryo development arrest [59]. Lastly, Chi et al., also used TEM to examine ultrastructure of the human fragmented embryos and found that blastomeres with anucleate fragments contained fewer mitochondria in their cytoplasm compared to normal blastomeres [21].
Cell death and CF
Eight of the included studies analyzed the relationship between cell death and embryo fragmentation (Table 3). Five studies analyzed the status of chromatin in arrested fragmented embryos through a combined technique for simultaneous nuclear and terminal transferase-mediated DNA end labelling (TUNEL) [24, 60,61,62,63]. Two studies used a comet assay to analyze DNA fragmentation [21, 63]. Four of the eight studies used Annexin V staining [21, 61,62,63] with three including the presence of propidium iodide (PI) to compare apoptosis to necrosis [21, 61, 63].
Jurisicova et al., used a combined nuclear and fragmented DNA labeling approach which allowed distinction between chromatin status and DNA fragmentation, which serve as markers of apoptosis versus necrosis respectively [60]. After fertilization, embryos were stained with 4,6-diamidino-2-phenylindole (DAPI). In cases of compromised cell membrane integrity, DAPI stain was observed in the cytoplasm as a sign of necrosis. Concomitant use of TUNEL labeling reflected the integrity of the DNA and allowed distinction between necrotic and apoptotic cells. Through combined techniques of DAPI/TUNEL, TEM, scanning electron microscopy (SEM) and stereomicroscopic observations, 153 of 203 (75.4%) fragmented early cleavage-stage embryos displayed signs of apoptosis (i.e., chromatin condensation, cellular shrinkage, DNA fragmentation, presence of cell corpses) with or without normal nuclei [60].
Similarly, Levy et al., analyzed early arrested or fragmented preimplantation embryos and the pattern of DNA fragmentation using TUNEL assay and the presence of phosphatidylserine through Fluorescein isothiocyanate (FITC)-labelled Annexin V, a phosphatidylserine binding protein. The authors observed TUNEL staining in one or more nuclei of 15 out of 50 (30%) arrested embryos from the 2-cell stage to uncompacted morulae, all of which had high degrees of CF. Furthermore, embryos with regular-sized blastomeres without fragmentation were all TUNEL negative [50].
A separate prospective study by Antczak et al., explored the possible association between fragmentation and apoptosis using PI and Annexin V staining of plasma membrane phosphatidylserine and TUNEL analysis of blastomere DNA [24]. In contradistinction to prior studies, these authors found no direct correlation between fragmentation and apoptosis. Virtually all blastomeres that were PI negative, intact or fragmented, showed no TUNEL or annexin V fluorescence, suggesting no signs of apoptosis [24].
Liu et al., used a similar methodology of TUNEL labeling and Annexin V staining to detect markers of apoptosis in fragmented human embryos derived from IVF [61]. Overall, highly fragmented embryos had apoptotic features including bright fluorescence (positive TUNEL labeling signifying DNA fragmentation) on the cell corpses and in intact blastomeres [61]. By staining cells with both annexin V and PI, this study was able to demonstrate that apoptosis occurs frequently in fragmented human embryos and the coexistence of apoptotic, necrotic and viable sibling blastomeres can occur. Sibling blastomeres within an embryo often showed apoptotic features that led to secondary necrosis while others did not initiate apoptosis. The authors did not find a significant difference in the expression frequency of apoptotic genes between viable and nonviable or arrested embryos [61].
Chi et al., stained human embryos (n=10) with annexin V and PI and found that human fragmented embryos exhibited characteristics of both necrosis and apoptosis [20]. Rather than TUNEL assay, these authors used a modified sperm comet assay to investigate DNA fragmentation of human fragmented embryos. They found that 6/7 human fragmented embryos (85.1%) stained positively for PI with the intensity of staining increasing with the degree of fragmentation. Of note, DNA fragmentation was observed in fragmented human embryos but not in the normal embryo [21].
Metcalfe et al., analyzed the expression of 11 BCL-2 family genes in normally develo** embryos and in severely fragmented embryos [64]. They found that the expression of BCL-2 family genes was highest in the pronuclear stage and eight-cell stages, and lowest at the two-cell, four-cell, and blastocyst stages in developmentally intact embryos. Furthermore, the expression did not change in fragmented embryos, suggesting that embryo fragmentation does not likely compromise mRNA integrity and gene detection [64]. However, like Liu et al., [61] these authors did detect far fewer pro-apoptotic BCL-2 genes in fragmented embryos at the eight-cell stage. The authors noted that these findings do not distinguish between iatrogenic apoptosis from suboptimal in-vitro culture conditions [64]. A separate study by Jurisicova et al. similarly analyzed gene expression at the 2-, 4- and 8-cell stage of fragmented embryos. Embryos that had 30-50% fragmentation showed a significant increase in Hrk mRNA levels, a BCL-2 protein encoding gene (P = 0.016). Further, these authors found an increase in Caspase-3 mRNA in fragmented embryos, as well as induction of Caspase-3-like enzyme activity in nucleated fragments, although this finding was not statistically significant [65].
Van Blerkom et al., also used TUNEL assay in conjunction with the comet assay as a method of identifying the specific pattern of cell death (necrosis, lysis or apoptosis) and the extent of DNA damage in develo** embryos [47]. They analyzed the integrity of the plasma membrane through annexin V staining with PI. They examined both transient and persistent fragment clusters at day-3 and 3.5 embryos for evidence of programed cell death using time-lapse video and TEM. In contrast to previous studies, they found no indication of nuclear DNA damage or loss of membrane integrity. These results, led the authors to hypothesize that the fragmentation observed was not characteristic of programed cell death, but rather resembled features of oncosis. The culture in this study was not severely oxygen-deprived and thus the authors concluded that this oncosis-like process was potentially a result of disproportionate mitochondrial segregation during the first cleavage division. Without sufficient mitochondria, the early blastomeres did not maintain adequate ATP for normal cell function which may have precipitated an ATP-driven oncosis-like process [47].
Lastly, a study by Bencomo et al., found correlations between the degree of apoptosis in human granulosa-lutein (GL) cells, the outcome of IVF-ET cycle, the percentage of embryo fragmentation, and patient’s age [66]. Human GL cells were collected from follicular fluid, cultured for 48 hours, and marked with caspACE FITC-VAD-FMK, a fluorescent marker for activated caspases. Results showed that GL cells of older women (>38 years old) were significantly more susceptible to apoptosis at 43.2 ± 18.0% compared to the younger group (<38 years old) with a mean percentage of apoptotic cells 33 ± 17.2%. Women who had a positive pregnancy had a lower level of apoptosis in GL cultures than those who did not get pregnant (30.2 ± 14% vs. 40.4 ± 19.5%). There was a positive correlation between embryo fragmentation and GL cell apoptosis (r = 0.214). Overall, the level of apoptosis of cultured GL cells was correlated with IVF outcome [66].
These studies demonstrate the diversity among techniques to evaluate cell death in the develo** embryo. TUNEL labeling, sperm comet assay, annexin V staining or some combination of these techniques have been described. Furthermore, there are discrepancies between the stage at which apoptosis might occur, with majority of studies cited here suggesting that cell death occurs in early stages of development before blastocyst formation. While some studies suggest that fragmented embryos display signs of apoptosis, these findings are still disputed and the distinction between apoptosis and necrosis is not clearly defined in the literature.
Patient age and CF
There are inconsistencies within the literature regarding the relationship between maternal age and CF. A total of six studies in this review focused on this relationship (Table 4). Three of the studies found a positive correlation between patient age and degree of embryo fragmentation [67,68,69]. The other three studies found no age-related correlation between embryo fragmentation or quality [7, 70, 71].
A retrospective study by Ziebe et al., compared the relationship between age of women undergoing IVF and the proportion of anucleate fragmentation in cleavage-stage embryos. Using a logistic regression analysis, the authors compared the percentage of transfers using fragmented embryos with age; the odds of fragmentation increased by 3% per year (OR 1.033 [95% CI 0.996, 1.071]). There was a linear relationship between age and embryo fragmentation rate, with an increase in fragmentation of 0.76% per year (95% CI -0.09%, 1.61%) [68].
Keltz et al., assessed various predictors of embryo fragmentation in IVF and found that increased maternal age and lower number of oocytes and embryos were associated with increased embryo fragmentation. There was a significant difference between cycles with fragmented embryos (n=74) at a mean age of 36.9 ± 4.24 years as compared to cycles with no fragmented embryos (n=234) at a mean age of 35.4 ± 4.74 years. Overall, this retrospective analysis of fresh IVF cycles found that embryo fragmentation is indeed associated with older age and ultimately poor cycle outcome [67].
Contrary to these findings, an early study by Alikani et al., showed no relationship between maternal age and CF [7]. In a retrospective analysis of degree and pattern of embryo fragmentation on days 2 and 3, they defined five patterns of fragmentation. Both the degree and pattern of fragmentation impacted pregnancy and implantation rate, but the authors found no correlation between appearance of any CF pattern and maternal age. The average maternal age in their population was 35.7 ± 4.25 years [7]. Another study by Stensen et al., analyzed the effect of chronological age on oocyte quality (assessed by maturity) and embryo quality (assessed by cleavage-stage, blastomere size and embryo fragmentation). Women were divided into five age groups: ≤25, 26–30, 31–35, 36–40 and ≥41 years. The embryo morphological score was based on fragmentation and blastomere size with score of 0-4 where score of 4 being equally sized blastomeres and no fragmentation and score of 0 being cleavage arrest or morphologically abnormal embryo. The mean oocyte score and embryo morphology score were not found to be significantly different across the age groups [70]. Wu et al., also showed that age does not influence embryo fragmentation. Patient ages ranged from 20 to 44 years with a mean age of 30.6 ± 4.6 years and were divided into age groups of ≤29, 30–34, 35–37, 38–40, and ≥41 years of age. Analysis of embryos with similar degrees of fragmentation was used to assess whether maternal age was associated with embryo fragmentation and blastocyst development. There was no correlation between age and embryo fragmentation as a continuous variable (r = 0.02; P = 0.25) nor was there a correlation when age was divided into the groups (P = 0.2). They also found that neither age (r = -0.08; P=0.16) nor degree of fragmentation (r = -0.01; P = 0.81) had a significant impact on blastocyst development [71].
Recently, a retrospective time-lapse study evaluated the implantation rate of 379 fragmented embryos. The results showed that there was an association between advanced maternal age and fragmentation. Fragmentation rate was higher in patients ˃35 compared to patients ≤35 years old. It seems that the lower quality of oocytes in older patients results in increasing fragmentation [69]. Overall, the included studies have differing conclusions on the effect of maternal age and CF; varying definitions and analysis of CF remain a limitation.
IVF vs ICSI procedures and CF
Five of the included studies compared embryo quality between conventional IVF and intracytoplasmic sperm injection (ICSI) procedures (Table 5). Two of these studies found that ICSI was associated with impaired embryo morphology compared to IVF [72, 73], while the other three showed no difference in embryo quality between the two fertilization modalities [74,75,76]. There were no studies within our search that identified embryos created by ICSI having greater morphology grade, or less embryo fragmentation, than IVF.
Frattarelli et al., directly examined the effect of ICSI on embryo fragmentation and implantation rate compared to IVF. There was a significant difference in mean embryo grade between IVF and ICSI. IVF patients had significantly more grade I, or non-fragmented, embryos compared to the ICSI group (P < 0.01). However, there was no significant difference in mean number of embryos per embryo grade II – IV [72].
Similarly, Hsu et al., compared embryo quality, morphology, and cleavage after ICSI with standard IVF patients. They defined the grading system from 1 – 5, ranging from no fragments (grade 1) to severe or complete fragmentation (grade 5). They found that for the overall population, when comparing ICSI and IVF patients after matching for age and number of embryos transferred, the number of embryos with good morphology was significantly greater in the IVF group compared to ICSI (P < 0.006). The average morphology scores, similar to the results of Frattarelli et al., were significantly different between the ICSI group and the IVF group. They also found IVF patients’ embryos to have significantly better cleavage rate than those from ICSI patients (P < 0.001) [73].
Garello et al., evaluated if fertilization via ICSI influences pronuclear orientation, PB placement, and embryo quality when compared to IVF. Embryos were assessed using morphology, and grouped as good (grades 1-2), average (grades 3-4), or poor (grades 5-6). Embryos were also assessed for cleavage regularity and proportion of fragmentation (0, <20%, 20–50%, >50%). There was no statistically significant difference in mean morphology (good, average, poor) between the groups, although they did note an apparent increase in grade 4 versus grade 3 embryos after ICSI procedure. The two groups had similar proportions of fragmentation [74].
Two other studies took a unique approach in comparing embryo quality in ICSI and IVF patients by using randomized sibling oocytes [75, 76]. Yoeli et al., studied oocytes retrieved from patients with a less than 40% fertilization rate in a previous standard IVF cycle and divided these oocytes into a conventional insemination group and an ICSI group. Each group had over 1400 oocytes. Overall, there was no significant difference between the IVF and ICSI groups in terms of cleavage rate or rate of high-quality embryos (both Grade A embryos with ≤10% fragmentation and embryos with ≤20% fragmentation) [75]. Ruiz et al., also analyzed sibling oocytes in patients who had failed intrauterine insemination attempts. The authors similarly found no significant difference in fertilization rates and degree of fragmentation between ICSI and standard IVF groups [76]. Most studies included in the search criteria showed that ART techniques such as ICSI do not significantly impact fragmentation rate in develo** embryos, suggesting that ICSI is not a significant contributor to poorer outcomes by way of embryo fragmentation. Of note, the timing of cumulus cell denudation after conventional IVF is a matter of debate; none of the included studies in this review performed short-time insemination. In a meta-analysis reviewing denudation times, the number of good quality embryos produced after retaining cumulus cells was similar to those produced after early removal of these cells, suggesting that brief insemination has no impact on CF [96]. Although they did not attempt to remove fragments themselves, this study is included as ZP-free oocytes are sometimes encountered in or because of ART procedures, i.e., ICSI. The results suggest that the rate of fragmentation is decreased after mechanical ZP removal. The authors concluded that ZP is not always necessary for normal embryo development since the ZP-free embryos developed normally, maintained their cell adhesions, and had a decreased rate of fragmentation [96]. It seems that defragmentation of an aneuploid or severely fragmented embryo, only improves the embryo morphology grade but the quality and fate of embryo is not changed [97].
CF and chromosomal abnormalities in embryo
Although the relationship between DNA fragmentation and chromosomal abnormalities has been more commonly explored in the literature, CF may also be related to intrinsic chromosomal abnormalities in develo** embryos. Fourteen studies included in this review explored this relationship (Table 9) [55, 56, 85, 98,99,100,101,102,103,104,105,106,107,108].
CF was rarely seen in embryos with normal chromosomal content. Findikli et al., studied DNA fragmentation and aneuploidy in poor quality embryos by TUNEL and fluorescent in situ hybridization (FISH) techniques. Within seven chromosomally abnormal embryos, each had variable degrees of CF [98]. This study suggests that DNA fragmentation, being a sign of chromosomal abnormalities, may exist together with CF.
An earlier study by Munne et al., examined 524 embryos using FISH analysis for three to five chromosomes. While controlling for age, they divided the embryos into three groups: arrested, slow and/or fragmented, or morphologically and developmentally normal. They found that polyploidy was the most common chromosomal abnormality in the arrested embryo group and decreased with increasing embryonic competence, with 44.5% polyploidy in arrested compared to 2.1% in morphologically normal embryos. Maternal age was not associated with polyploidy rates, but aneuploidy significantly increased with maternal age in morphologically normal human embryos [57]. Another early study by Almeida and Bolton also examined the relationship between chromosomal abnormalities and embryonic developmental potential. They found that cleavage-stage embryos with poor morphology, defined as irregular shaped blastomeres with severe fragmentation, showed a higher incidence of chromosomal abnormalities than those with good morphology [100]. Magli et al., found a more direct relationship between chromosomal abnormalities and embryo fragmentation in a larger retrospective study of nearly 1600 embryos. There was a strong association between percentage of fragmentation and chromosomal abnormalities (monosomies and trisomies), where 90% of chromosomal abnormalities were found in embryos with greater than 40% fragmentation [101].
Another retrospective study comparing maternal age to embryo morphology and chromosomal abnormalities was conducted by Moayeri et al., By examining nine chromosomes in day-3 embryos, they found that morphology predicted chromosomal status in the advanced maternal age group (≥38 years old), but not in younger patients. Fragmentation alone predicted euploidy in both the advanced maternal age and younger groups. This suggests that cellular fragmentation may be a predictor of chromosomal competence and thus embryo developmental potential [102].
In contrast, Baltaci et al., examined 1,000 embryos and concluded that embryo morphology was not predictive of euploidy and that a considerable number of chromosomally abnormal embryos with good development potential may be selected for embryo transfer. They used FISH for five chromosomes and found that a large proportion of both normal and aneuploid embryos were evaluated as top quality (grade I). For example, 66% of chromosomally abnormal embryos were of good quality (grade I and II). They found no significant difference among aneuploid embryos when distributed by age. However, a higher embryo quality found in normal compared to aneuploid embryos [103].
In addition, Pellestor et al., compared the relationship between morphology and chromosomal abnormalities in two separate studies. The first study found that aneuploidy was the most frequently observed abnormality after cytogenetic analysis of preimplantation embryos [55]. They defined the quality of embryos as good (grade I and II) and poor (grades III and IV). There was an increased chromosomal abnormality in poor quality embryos (84.3%) when compared to embryos with good quality (33.9%). Both aneuploidy and fragmentation were shown to be predominant in poor quality embryos, whereas mosaicism and polyploidy were the most frequent abnormalities in good quality embryos [55]. Pellestor et al., also performed cytogenetic analysis on 411 poor-quality embryos (grade IV) [85]. Ninety percent of the successfully analyzed cases showed abnormal chromosome complements, with aneuploidy being the most frequently observed. These results further support that a large majority of poor grade embryos are chromosomally abnormal and ultimately offer low chance of reproductive success for either embryo transfer or cryopreservation [85].
A separate study by Chavez et al., combined time-lapse imaging with karyotypic status of blastomeres in the 4-cell embryo to test whether blastomere behavior may reflect chromosomal abnormalities, using array comparative genomic hybridization (aCGH), during early cleavage [56]. In time-lapse observations, a large proportion of aneuploid and triploid, but not euploid embryos, exhibited cellular fragmentation. They showed that the probability of aneuploidy increased with higher fragmentation and only 65% of the fragmented embryo would be expected to form blastocyst. Furthermore, all the aneuploid embryos with additional unbalanced sub-chromosomal errors exhibited CF. The authors concluded that although fragmentation alone at a single point in time does not predict embryo developmental potential, time-lapse imaging with dynamic fragmentation screening may help detect embryonic aneuploidy [56].
Two more recent studies also used aCGH to evaluate the association between embryo ploidy and fragmentation. Vera-Rodriguez et al., in a retrospective study, compared the rate of embryo aneuploidy between two groups of high (≥25%) and low (˂25%) fragmentation. They found that the rate of aneuploidy in high and low fragmentation was 62.5 and 46.3%, respectively. However, the difference was not statistically significant concluding that using degree of fragmentation alone is not suggested to predict the embryo ploidy status [107]. Minasi et al., in a case series evaluated 1730 blastocyst ploidy with aCGH. They showed that there is no significant difference between day-3 embryo morphology and embryo ploidy. However, the quality of blastocyst (inner cell mass grade, trophectoderm grade, degree of expansion) was associated with embryo ploidy [106].
In a recent meta-analysis, it was shown there is trend between degree of fragmentation and rate of aneuploidy [109]. A major source of controversy in both early and recent studies on aneuploidy and fragmentation is the variation in the methods and criteria used to evaluate these factors. One of the aspects that differ across studies include the technique for detecting aneuploidy; FISH vs aCGH. Recent studies have used aCGH to detect aneuploidy and found no clear relationship in this regard. Also, the quality of the matching between groups, the design of the study (retrospective vs prospective), the timing of the fragmentation assessment, the use of time-lapse imaging to monitor the fate of fragments are the other reasons for this discrepancy. There is still the lack of a clear cut-off point for the percentage of fragmentation to predict aneuploidy. Further powerful studies using new methods like next gene sequencing and tile-lapse systems are recommended to shed light on the relationship between fragmentation and aneuploidy.
The literature highlights that poor quality embryos have a higher incidence of chromosomal abnormalities. Notably, CF is rarely observed in embryos with normal chromosomal content. Technological advancements, such as TLM, offer promising avenues to enhance our understanding and detection of embryonic aneuploidy. Overall, these studies underscore the complexity of the relationship between fragmentation and chromosomal abnormalities, emphasizing the need for continued research to refine embryo selection strategies and improve reproductive outcomes.
Discussion and conclusion
The role of fragmentation in human embryo development and reproductive potential is widely recognized, albeit without standard definition nor agreed upon implication. While it has been shown that degree of fragmentation and embryo implantation potential are inversely proportional [5, 7, 9,10,11,12,13,14,15,16,17,18,19,20,21], the degree, pattern, and distribution of fragmentation as it relates to pregnancy outcome is debated in the literature. Our qualitative synthesis of 60 articles related to the study of embryo fragmentation and reproductive outcomes highlighted some of the challenges in analysis of fragmentation, while revealing trends in our evolving knowledge of how fragmentation may relate to functional development of the human embryo.
While fragmentation is best understood to be a natural process across species, the origin of fragmentation remains incompletely understood and likely multifactorial. Degree of fragmentation has been plausibly correlated to sperm DNA oxidation [37], errors in division [37], mitochondrial distribution [45], and overall embryo quality [39]. However, some causes of fragmentation are based on outdated studies and require validation in future research with higher quality and more advanced techniques. While cause of fragmentation remains a focus of investigation, advances in technology have allowed for more detailed analysis of its effect on embryo development and reproductive outcome. At the cellular level, increased fragmentation has been shown to be associated with higher rates of apoptosis, necrosis, and programmed cell death of cleavage-stage embryos [60,61,62]. Given the recognized significance of fragmentation on embryo development, it follows that many studies have been focused on IVF and ART impacts on fragmentation, as well as determining quantitative reproductive outcomes. In terms of other influences on degree of fragmentation, patient age was not universally found to be significantly associated with fragmentation [7, 70, 71] although age is certainly known to influence embryo quality. Most studies included in the search criteria showed that ART such as ICSI do not significantly impact fragmentation rate in develo** embryos [74,75,76]. Those studies that found significant differences in embryo grading either between conventional fertilization and ICSI either did not find a difference in implantation or pregnancy rate or did not study it, suggesting that ICSI is not a significant contributor to poorer ART outcomes by way of embryo fragmentation.
In synthesizing the available data on ART and pregnancy outcomes with varying degrees of embryo fragmentation, most included studies did find a negative impact of increasing fragmentation on reproductive success while severe fragmentation does appear to be associated with poorer implantation rate and clinical pregnancy rate. This association may be related to the observation that increased fragmentation at the cleavage-stage embryo is related to chromosomal abnormalities incompatible with ongoing development or pregnancy.
The reviewed studies have several limitations. There are different grading systems in use that may impact detecting and reporting the degree of CF. Different criteria and terminology used in different studies may in turn make the comparison of outcome measures difficult. Another factor is the distribution pattern of CF. There are two types of scattered and concentrated fragments with different prognoses that is not considered in grading systems. Therefore, due to the lack of a standard cleavage-stage embryo grading system, comparing different studies should be done with caution. In addition, evaluation of embryo fragmentation is mostly based on individual observation which is subjective and has inter- and intra-observer subjectivity leading to high variable results even if performed by an experienced embryologist [110]. TLM is considered as a non-invasive tool and evaluates the embryo quality continuously and without the need to remove the embryo from the incubator [111]. The use of this technology allows for the analysis of embryo morphokinetics and has advanced knowledge of the develo** embryo. Recently, artificial intelligence (AI) including machine learning and neural network has gained popularity in various fields of medicine including IVF and embryology. Accuracy of AI in prediction of fragmentation has been studied with encouraging results [112]. Further advances in technology will promote the use of AI as a tool in defining the effect of fragmentation on human embryo development and reproductive potential.
Although the precise origin and the importance of external or iatrogenic factors on fragmentation of cleavage-stage embryos varies in the literature, there is more consensus regarding severe fragmentation worsening reproductive outcomes. Given this important pattern, and the availability of increasingly sophisticated embryologic technology, further research is warranted to characterize more completely preventative or rescue techniques to improve reproductive outcomes.
Availability of data and materials
No datasets were generated or analysed during the current study.
References
Balaban B, Brison D, Calderon G, Catt J, Conaghan J, Cowan L, et al. The Istanbul consensus workshop on embryo assessment: proceedings of an expert meeting. Hum Reprod. 2011;26:1270–83.
Hill GA, Freeman M, Bastias MC, Jane Rogers B, Herbert CM, Osteen KG, et al. The influence of oocyte maturity and embryo quality on pregnancy rate in a program for in vitro fertilization-embryo transfer. Fertil Steril. 1989;52:801–6.
Cummins JM, Breen TM, Harrison KL, Shaw JM, Wilson LM, Hennessey JF. A formula for scoring human embryo growth rates in in vitro fertilization: Its value in predicting pregnancy and in comparison with visual estimates of embryo quality. J In Vitro Fertil Embryo Transfer. 1986;3:284–95.
Cutting R, Morroll D, Roberts SA, Pickering S, Rutherford A, on behalf of the BFS and ACE. Elective Single Embryo Transfer: Guidelines for Practice British Fertility Society and Association of Clinical Embryologists. Hum Fertil. 2008;11:131–46.
Edwards RG, Fishel SB, Cohen J, Fehilly CB, Purdy JM, Slater JM, et al. Factors influencing the success of in vitro fertilization for alleviating human infertility. J In Vitro Fert Embryo Transf. 1984;1:3–23.
Puissant F, Van Rysselberge M, Barlow P, Deweze J, Leroy F. Embryo scoring as a prognostic tool in IVF treatment. Hum Reprod. 1987;2:705–8.
Alikani M, Cohen J, Tomkin G, Garrisi GJ, Mack C, Scott RT. Human embryo fragmentation in vitro and its implications for pregnancy and implantation. Fertil Steril. 1999;71:836–42.
Cecchele A, Cermisoni GC, Giacomini E, Pinna M, Vigano P. Cellular and Molecular Nature of Fragmentation of Human Embryos. Int J Mol Sci. 2022;23:1349.
Claman P, Armant DR, Seibel MM, Wang TA, Oskowitz SP, Taymor ML. The impact of embryo quality and quantity on implantation and the establishment of viable pregnancies. J In Vitro Fert Embryo Transf. 1987;4:218–22.
Ebner T, Yaman C, Moser M, Sommergruber M, Pölz W, Tews G. Embryo fragmentation in vitro and its impact on treatment and pregnancy outcome. Fertil Steril. 2001;76:281–5.
Erenus M, Zouves C, Rajamahendran P, Leung S, Fluker M, Gomel V. The effect of embryo quality on subsequent pregnancy rates after in vitro fertilization. Fertil Steril. 1991;56:707–10.
Giorgetti C, Terriou P, Auquier P, Hans E, Spach JL, Salzmann J, et al. Embryo score to predict implantation after in-vitro fertilization: based on 957 single embryo transfers. Hum Reprod. 1995;10:2427–31.
Holte J, Berglund L, Milton K, Garello C, Gennarelli G, Revelli A, et al. Construction of an evidence-based integrated morphology cleavage embryo score for implantation potential of embryos scored and transferred on day 2 after oocyte retrieval. Hum Reprod. 2007;22:548–57.
Roseboom TJ, Vermeiden JP, Schoute E, Lens JW, Schats R. The probability of pregnancy after embryo transfer is affected by the age of the patient, cause of infertility, number of embryos transferred and the average morphology score, as revealed by multiple logistic regression analysis. Hum Reprod. 1995;10:3035–41.
Shulman A, Ben-Nun I, Ghetler Y, Kaneti H, Shilon M, Beyth Y. Relationship between embryo morphology and implantation rate after in vitro fertilization treatment in conception cycles. Fertil Steril. 1993;60:123–6.
Staessen C, Janssenswillen C, Van den Abbeel E, Devroey P, Van Steirteghem AC. Avoidance of triplet pregnancies by elective transfer of two good quality embryos. Hum Reprod. 1993;8:1650–3.
Visser DS, Fourie FR. The applicability of the cumulative embryo score system for embryo selection and quality control in an in-vitro fertilization/embryo transfer programme. Hum Reprod. 1993;8:1719–22.
Volpes A, Sammartano F, Coffaro F, Mistretta V, Scaglione P, Allegra A. Number of good quality embryos on day 3 is predictive for both pregnancy and implantation rates in in vitro fertilization/intracytoplasmic sperm injection cycles. Fertil Steril. 2004;82:1330–6.
Ziebe S, Petersen K, Lindenberg S, Andersen AG, Gabrielsen A, Andersen AN. Embryo morphology or cleavage stage: how to select the best embryos for transfer after in-vitro fertilization. Hum Reprod. 1997;12:1545–9.
Fujimoto VY, Browne RW, Bloom MS, Sakkas D, Alikani M. Pathogenesis, developmental consequences, and clinical correlations of human embryo fragmentation. Fertil Steril. 2011;95:1197–204.
Chi H-J, Koo J-J, Choi S-Y, Jeong H-J, Roh S-I. Fragmentation of embryos is associated with both necrosis and apoptosis. Fertil Steril. 2011;96:187–92.
Racowsky C, Ohno-Machado L, Kim J, Biggers JD. Is there an advantage in scoring early embryos on more than one day? Hum Reprod. 2009;24:2104–13.
Hardy K, Stark J, Winston RML. Maintenance of the inner cell mass in human blastocysts from fragmented embryos. Biol Reprod. 2003;68:1165–9.
Antczak M, Van Blerkom J. Temporal and spatial aspects of fragmentation in early human embryos: possible effects on developmental competence and association with the differential elimination of regulatory proteins from polarized domains. Hum Reprod. 1999;14:429–47.
Mio Y, Maeda K. Time-lapse cinematography of dynamic changes occurring during in vitro development of human embryos. Am J Obstet Gynecol. 2008;199(660):e1-5.
Hardarson T, Löfman C, Coull G, Sjögren A, Hamberger L, Edwards RG. Internalization of cellular fragments in a human embryo: time-lapse recordings. Reprod Biomed Online. 2002;5:36–8.
Van Blerkom J. The Enigma of Fragmentation in Early Human Embryos: Possible Causes and Clinical Relevance. Essential IVF. Boston: Springer US; 2004. 377–421.
Rijnders PM, Jansen CA. The predictive value of day 3 embryo morphology regarding blastocyst formation, pregnancy and implantation rate after day 5 transfer following in-vitro fertilization or intracytoplasmic sperm injection. Hum Reprod. 1998;13:2869–73.
Graham J, Han T, Porter R, Levy M, Stillman R, Tucker MJ. Day 3 morphology is a poor predictor of blastocyst quality in extended culture. Fertil Steril. 2000;74:495–7.
Milki AA, Hinckley MD, Gebhardt J, Dasig D, Westphal LM, Behr B. Accuracy of day 3 criteria for selecting the best embryos. Fertil Steril. 2002;77:1191–5.
Gardner DK, Vella P, Lane M, Wagley L, Schlenker T, Schoolcraft WB. Culture and transfer of human blastocysts increases implantation rates and reduces the need for multiple embryo transfers. Fertil Steril. 1998;69:84–8.
Guerif F, Le Gouge A, Giraudeau B, Poindron J, Bidault R, Gasnier O, et al. Limited value of morphological assessment at days 1 and 2 to predict blastocyst development potential: a prospective study based on 4042 embryos. Hum Reprod. 2007;22:1973–81.
Rienzi L, Ubaldi F, Iacobelli M, Romano S, Minasi MG, Ferrero S, et al. Significance of morphological attributes of the early embryo. Reprod Biomed Online. 2005;10:669–81.
Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ. 2021;372:n71.
Killeen ID, Moore NW. The morphological appearance and development of sheep ova fertilized by surgical insemination. J Reprod Fertil. 1971;24:63–70.
Enders AC, Hendrickx AG, Binkerd PE. Abnormal development of blastocysts and blastomeres in the rhesus monkey. Biol Reprod. 1982;26:353–66.
Meseguer M, Martínez-Conejero JA, O’Connor JE, Pellicer A, Remohí J, Garrido N. The significance of sperm DNA oxidation in embryo development and reproductive outcome in an oocyte donation program: a new model to study a male infertility prognostic factor. Fertil Steril. 2008;89:1191–9.
Stensen MH, Tanbo TG, Storeng R, Åbyholm T, Fedorcsak P. Fragmentation of human cleavage-stage embryos is related to the progression through meiotic and mitotic cell cycles. Fertil Steril. 2015;103:374-81.e4.
Ebner T. First polar body morphology and blastocyst formation rate in ICSI patients. Human Reproduction. 2002;17:2415–8.
Sedó CA, Bilinski M, Lorenzi D, Uriondo H, Noblía F, Longobucco V, et al. Effect of sperm DNA fragmentation on embryo development: clinical and biological aspects. JBRA Assist Reprod. 2017;21:343–50.
Rose BI, Laky D. Polar body fragmentation in IVM oocytes is associated with impaired fertilization and embryo development. J Assist Reprod Genet. 2013;30:679–82.
Zhou W, Fu L, Sha W, Chu D, Li Y. Relationship of polar bodies morphology to embryo quality and pregnancy outcome. Zygote. 2016;24:401–7.
Yang Y, Tan W, Chen C, ** L, Huang B. Correlation of the position and status of the polar body from the fertilized oocyte to the euploid status of blastocysts. Front Genet. 2022;13:1006870. https://doi.org/10.3389/fgene.2022.1006870.
Alikani M. Epithelial cadherin distribution in abnormal human pre-implantation embryos. Hum Reprod. 2005;20:3369–75.
Van Blerkom J, Davis P, Alexander S. Differential mitochondrial distribution in human pronuclear embryos leads to disproportionate inheritance between blastomeres: relationship to microtubular organization ATP content and competence. Hum Reprod. 2000;15:2621–33.
Otasevic V, Surlan L, Vucetic M, Tulic I, Buzadzic B, Stancic A, et al. Expression patterns of mitochondrial OXPHOS components, mitofusin 1 and dynamin-related protein 1 are associated with human embryo fragmentation. Reprod Fertil Dev. 2016;28:319–27.
Wilding M, Dale B, Marino M, di Matteo L, Alviggi C, Pisaturo ML, et al. Mitochondrial aggregation patterns and activity in human oocytes and preimplantation embryos. Hum Reprod. 2001;16:909–17.
Sermondade N, Delarouzière V, Ravel C, Berthaut I, Verstraete L, Mathieu E, et al. Characterization of a recurrent poor-quality embryo morphology phenotype and zygote transfer as a rescue strategy. Reprod Biomed Online. 2012;24:403–9.
Gat I, Levron J, Yerushalmi G, Dor J, Brengauz M, Orvieto R. Should zygote intrafallopian transfer be offered to all patients with unexplained repeated in-vitro fertilization cycle failures? J Ovarian Res. 2014;7:7.
Yang HW, Hwang KJ, Kwon HC, Kim HS, Choi KW, Oh KS. Detection of reactive oxygen species (ROS) and apoptosis in human fragmented embryos. Hum Reprod. 1998;13:998–1002.
Chen EY, Fu**aga M, Giaccia AJ. Hypoxic microenvironment within an embryo induces apoptosis and is essential for proper morphological development. Teratology. 1999;60:215–25.
Lee T-H, Lee M-S, Liu C-H, Tsao H-M, Huang C-C, Yang Y-S. The association between microenvironmental reactive oxygen species and embryo development in assisted reproduction technology cycles. Reprod Sci. 2012;19:725–32.
Lan K-C, Lin Y-C, Chang Y-C, Lin H-J, Tsai Y-R, Kang H-Y. Limited relationships between reactive oxygen species levels in culture media and zygote and embryo development. J Assist Reprod Genet. 2019;36:325–34.
Bedaiwy MA, Falcone T, Mohamed MS, Aleem AAN, Sharma RK, Worley SE, et al. Differential growth of human embryos in vitro: Role of reactive oxygen species. Fertil Steril. 2004;82:593–600.
Pellestor F, Girardet A, Andréo B, Arnal F, Humeau C. Relationship between morphology and chromosomal constitution in human preimplantation embryo. Mol Reprod Dev. 1994;39:141–6.
Chavez SL, Loewke KE, Han J, Moussavi F, Colls P, Munne S, et al. Dynamic blastomere behaviour reflects human embryo ploidy by the four-cell stage. Nat Commun. 2012;3:1251.
Munné S, Alikani M, Tomkin G, Grifo J, Cohen J. Embryo morphology, developmental rates, and maternal age are correlated with chromosome abnormalities. Fertil Steril. 1995;64(2):382–91. Corrected and republished in: Fertil Steril. 2019 Oct;112(4 Suppl1):e71–e80.
Halvaei I, Khalili MA, Nottola SA. A novel method for transmission electron microscopy study of cytoplasmic fragments from preimplantation human embryos. Microsc Res Tech. 2016;79:459–62.
Johansson M, Hardarson T, Lundin K. There is a cutoff limit in diameter between a blastomere and a small anucleate fragment. J Assist Reprod Genet. 2003;20:309–13.
Jurisicova A, Varmuza S, Casper RF. Programmed cell death and human embryo fragmentation. Mol Hum Reprod. 1996;2:93–8.
Liu HC, He ZY, Mele CA, Veeck LL, Davis O, Rosenwaks Z. Expression of apoptosis-related genes in human oocytes and embryos. J Assist Reprod Genet. 2000;17:521–33.
Levy R, Benchaib M, Cordonier H, Souchier C, Guerin JF. Annexin V labelling and terminal transferasemediated DNA end labelling (TUNEL) assay in human arrested embryos. Mol Hum Reprod. 1998;4(8):775–83. https://doi.org/10.1093/molehr/4.8.775.
Van Blerkom J, Davis P, Alexander S. A microscopic and biochemical study of fragmentation phenotypes in stage-appropriate human embryos. Hum Reprod. 2001;16(4):719–29. https://doi.org/10.1093/humrep/16.4.719.
Metcalfe AD, Hunter HR, Bloor DJ, Lieberman BA, Picton HM, Leese HJ, Kimber SJ, Brison DR. Expression of 11 members of the BCL-2 family of apoptosis regulatory molecules during human preimplantation embryo development and fragmentation. Mol Reprod Dev. 2004;68(1):35–50. https://doi.org/10.1002/mrd.20055.
Jurisicova A, Antenos M, Varmuza S, Tilly J, Casper R. Expression of apoptosis-related genes during human preimplantation embryo development: potential roles for the Harakiri gene product and Caspase-3 in blastomere fragmentation. Mol Hum Reprod. 2003;9:133–41.
Bencomo E, Pérez R, Arteaga M-F, Acosta E, Peña O, Lopez L, et al. Apoptosis of cultured granulosa-lutein cells is reduced by insulin-like growth factor I and may correlate with embryo fragmentation and pregnancy rate. Fertil Steril. 2006;85:474–80.
Keltz MD, Skorupski JC, Bradley K, Stein D. Predictors of embryo fragmentation and outcome after fragment removal in in vitro fertilization. Fertil Steril. 2006;86:321–4.
Ziebe S, Loft A, Petersen JH, Andersen AG, Lindenberg S, Petersen K, et al. Embryo quality and developmental potential is compromised by age. Acta Obstet Gynecol Scand. 2001;80:169–74.
Lahav-Baratz S, Blais I, Koifman M, Dirnfeld M, Oron G. Evaluation of fragmented embryos implantation potential using time-lapse technology. J Obstet Gynaecol Res. 2023;49:1560–70.
Stensen MH, Tanbo T, Storeng R, Byholm T, Fèdorcsak P. Routine morphological scoring systems in assisted reproduction treatment fail to reflect age-related impairment of oocyte and embryo quality. Reprod Biomed Online. 2010;21:118–25.
Wu DH, Reynolds K, Maxwell R, Lindheim SR, Aubuchon M, Thomas MA. Age does not influence the effect of embryo fragmentation on successful blastocyst development. Fertil Steril. 2011;95:2778–80.
Frattarelli JL, Leondires MP, Miller BT, Segars JH. Intracytoplasmic sperm injection increases embryo fragmentation without affecting clinical outcome. J Assist Reprod Genet. 2000;17:207–12.
Hsu MI, Mayer J, Aronshon M, Lanzendorf S, Muasher S, Kolm P, et al. Embryo implantation in in vitro fertilization and intracytoplasmic sperm injection: impact of cleavage status, morphology grade, and number of embryos transferred. Fertil Steril. 1999;72:679–85.
Garello C, Baker H, Rai J, Montgomery S, Wilson P, Kennedy CR, et al. Pronuclear orientation, polar body placement, and embryo quality after intracytoplasmic sperm injection and in-vitro fertilization: further evidence for polarity in human oocytes? Hum Reprod. 1999;14:2588–95.
Yoeli R, Orvieto R, Ashkenazi J, Shelef M, Ben-Rafael Z, Bar-Hava I. Comparison of embryo quality between intracytoplasmic sperm injection and in vitro fertilization in sibling oocytes. J Assist Reprod Genet. 2008;25:23–8.
Ruiz A, Remohí J, Minguez Y, Guanes PP, Simón C, Pellicer A. The role of in vitro fertilization and intracytoplasmic sperm injection in couples with unexplained infertility after failed intrauterine insemination. Fertil Steril. 1997;68:171–3.
Zhang XD, Liu JX, Liu WW, Gao Y, Han W, **ong S, et al. Time of insemination culture and outcomes of in vitro fertilization: a systematic review and meta-analysis. Hum Reprod Update. 2013;19:685–95.
Liu J, Zhang X, Yang Y, Zhao J, Hao D, Zhang J, et al. Long-time vs. short-time insemination of sibling eggs. Exp Ther Med. 2016;12:3756–60.
Sathananthan H, Bongso A, Ng SC, Ho J, Mok H, Ratnam S. Ultrastructure of preimplantation human embryos co-cultured with human ampullary cells. Hum Reprod. 1990;5:309–18.
Coticchio G, Barrie A, Lagalla C, Borini A, Fishel S, Griffin D, et al. Plasticity of the human preimplantation embryo: developmental dogmas, variations on themes and self-correction. Hum Reprod Update. 2021;27:848–65.
Watson AJ. The cell biology of blastocyst development. Mol Reprod Dev. 1992;33:492–504.
Hur C, Nanavaty V, Yao M, Desai N. The presence of partial compaction patterns is associated with lower rates of blastocyst formation, sub-optimal morphokinetic parameters and poorer morphologic grade. Reprod Biol Endocrinol. 2023;21:12.
Lagalla C, Tarozzi N, Sciajno R, Wells D, Di Santo M, Nadalini M, et al. Embryos with morphokinetic abnormalities may develop into euploid blastocysts. Reprod Biomed Online. 2017;34:137–46.
Ebner T, Moser M, Shebl O, Sommergruber M, Gaiswinkler U, Tews G. Morphological analysis at compacting stage is a valuable prognostic tool for ICSI patients. Reprod Biomed Online. 2009;18:61–6.
Pellestor F, Dufour MC, Arnal F, Humeau C. Direct assessment of the rate of chromosomal abnormalities in grade IV human embryos produced by in-vitro fertilization procedure. Hum Reprod. 1994;9(2):293–302. https://doi.org/10.1093/oxfordjournals.humrep.a138497.
Morgan K, Wiemer K, Steuerwald N, Hoffman D, Maxson W, Godke R. Use of videocinematography to assess morphological qualities of conventionally cultured and cocultured embryos. Hum Reprod. 1995;10:2371–6.
Alikani M, Calderon G, Tomkin G, Garrisi J, Kokot M, Cohen J. Cleavage anomalies in early human embryos and survival after prolonged culture in-vitro. Hum Reprod. 2000;15:2634–43.
Ivec M, Kovacic B, Vlaisavljevic V. Prediction of human blastocyst development from morulas with delayed and/or incomplete compaction. Fertil Steril. 2011;96:1473-1478.e2.
Hnida C, Engenheiro E, Ziebe S. Computer-controlled, multilevel, morphometric analysis of blastomere size as biomarker of fragmentation and multinuclearity in human embryos. Hum Reprod. 2004;19:288–93.
Sjöblom P, Menezes J, Cummins L, Mathiyalagan B, Costello MF. Prediction of embryo developmental potential and pregnancy based on early stage morphological characteristics. Fertil Steril. 2006;86:848–61.
Kellam L, Pastorelli LM, Bastida AM, Senkbeil A, Montgomery S, Fishel S, et al. Perivitelline threads in cleavage-stage human embryos: observations using time-lapse imaging. Reprod Biomed Online. 2017;35:646–56.
Paternot G, Debrock S, De Neubourg D, D’Hooghe TM, Spiessens C. Semi-automated morphometric analysis of human embryos can reveal correlations between total embryo volume and clinical pregnancy. Hum Reprod. 2013;28:627–33.
Eftekhari-Yazdi P, Valojerdi MR, Ashtiani SK, Eslaminejad MB, Karimian L. Effect of fragment removal on blastocyst formation and quality of human embryos. Reprod Biomed Online. 2006;13:823–32.
Keltz M, Fritz R, Gonzales E, Ozensoy S, Skorupski J, Stein D. Defragmentation of low grade day 3 embryos resulted in sustained reduction in fragmentation, but did not improve compaction or blastulation rates. Fertil Steril. 2010;94:2406–8.
Halvaei I, Khalili MA, Esfandiari N, Safari S, Talebi AR, Miglietta S, et al. Ultrastructure of cytoplasmic fragments in human cleavage stage embryos. J Assist Reprod Genet. 2016;33:1677–84.
Yumoto K, Shimura T, Mio Y. Removing the zona pellucida can decrease cytoplasmic fragmentations in human embryos: a pilot study using 3PN embryos and time-lapse cinematography. J Assist Reprod Genet. 2020;37:1349–54.
Sordia-Hernandez LH, Morales-Martinez FA, Frazer-Moreira LM, Villarreal-Pineda L, Sordia-Piñeyro MO, Valdez-Martinez OH. Clinical Pregnancy After Elimination of Embryo Fragments Before Fresh Cleavage-stage Embryo Transfer. J Family Reprod Health. 2020;14(3):198–204. https://doi.org/10.18502/jfrh.v14i3.4674.
Findikli N, Kahraman S, Kumtepe Y, Donmez E, Benkhalifa M, Biricik A, et al. Assessment of DNA fragmentation and aneuploidy on poor quality human embryos. Reprod Biomed Online. 2004;8:196–206.
Munné S, Alikani M, Tomkin G, Grifo J, Cohen J. Embryo morphology, developmental rates, and maternal age are correlated with chromosome abnormalities. Fertil Steril. 1995;64:382–91.
Almeida PA, Bolton VN. The relationship between chromosomal abnormality in the human preimplantation embryo and development in vitro. Reprod Fertil Dev. 1996;8:235–41.
Magli MC, Gianaroli L, Ferraretti AP. Chromosomal abnormalities in embryos. Mol Cell Endocrinol. 2001;183(Suppl 1):S29-34.
Moayeri SE, Allen RB, Brewster WR, Kim MH, Porto M, Werlin LB. Day-3 embryo morphology predicts euploidy among older subjects. Fertil Steril. 2008;89:118–23.
Baltaci V, Satiroglu H, Kabukçu C, Ünsal E, Aydinuraz B, Üner Ö, et al. Relationship between embryo quality and aneuploidies. Reprod Biomed Online. 2006;12:77–82.
Ziebe S, Lundin K, Loft A, Bergh C, Nyboe Anderson A, Selleskog U. FISH analysis for chromosomes 13, 16, 18, 21, 22, X and Y in all blastomeres of IVF pre-embryos from 144 randomly selected donated human oocytes and impact on pre-embryo morphology. Hum Reprod. 2003;18:2575–81.
Delimitreva SM, Zhivkova RS, Vatev ITS, Toncheva DI. Chromosomal disorders and nuclear and cell destruction in cleaving human embryos. Int J Dev Biol. 2005;49:409–16.
Minasi MG, Colasante A, Riccio T, Ruberti A, Casciani V, Scarselli F, Spinella F, Fiorentino F, Varricchio MT, Greco E. Correlation between aneuploidy, standard morphology evaluation and morphokinetic development in 1730 biopsied blastocysts: a consecutive case series study. Hum Reprod. 2016;31(10):2245–54. https://doi.org/10.1093/humrep/dew183. Epub 2016 Sep 2.
Vera-Rodriguez M, Chavez SL, Rubio C, Reijo Pera RA, Simon C. Prediction model for aneuploidy in early human embryo development revealed by single-cell analysis. Nat Commun. 2015;6:7601. https://doi.org/10.1038/ncomms8601.
Magli MC, Gianaroli L, Ferraretti AP, Lappi M, Ruberti A, Farfalli V. Embryo morphology and development are dependent on the chromosomal complement. Fertil Steril. 2007;87(3):534–41. https://doi.org/10.1016/j.fertnstert.2006.07.1512. Epub 2006 Nov 21.
Bamford T, Barrie A, Montgomery S, Dhillon-Smith R, Campbell A, Easter C, et al. Morphological and morphokinetic associations with aneuploidy: a systematic review and meta-analysis. Hum Reprod Update. 2022;28:656–86.
Baxter Bendus AE, Mayer JF, Shipley SK, Catherino WH. Interobserver and intraobserver variation in day 3 embryo grading. Fertil Steril. 2006;86:1608–15.
Lundin K, Park H. Time-lapse technology for embryo culture and selection. Ups J Med Sci. 2020;125:77–84.
Leahy BD, Jang WD, Yang HY, Struyven R, Wei D, Sun Z, et al. Automated Measurements of Key Morphological Features of Human Embryos for IVF. Lecture Notes in Computer Science (including subseries Lecture Notes in Artificial Intelligence and Lecture Notes in Bioinformatics). 2020.
Funding
We did not receive any funding to prepare this manuscript. We are grateful for receiving an editorial waiver for this manuscript.
Author information
Authors and Affiliations
Contributions
All authors have made substantial contributions to this manuscript. NE designed the work, critically reviewed and edited the manuscript. AY, IH and CB made substantial contribution in writing the manuscript. All authors have approved the paper for submission.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This is a review paper and does not involve human participants, human data or human tissue.
Consent for publication
This manuscript does not contain any individual person’s data in any form (including any individual details, images or videos).
Competing interests
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Yazdani, A., Halvaei, I., Boniface, C. et al. Effect of cytoplasmic fragmentation on embryo development, quality, and pregnancy outcome: a systematic review of the literature. Reprod Biol Endocrinol 22, 55 (2024). https://doi.org/10.1186/s12958-024-01217-7
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12958-024-01217-7