Abstract
Background
Laparoscopic surgery has justified its efficacy in the treatment of early gastric cancer. There are limited data indicating the eligibility of laparoscopic interventions in locally advanced gastric cancer. Publications describing the safety of laparoscopic techniques in the treatment of local and metastatic gastric cancer complicated by bleeding and stenosis are scarce.
Methods
The study included patients with histologically confirmed locally advanced and disseminated gastric cancer and complicated with bleeding and/or stenosis who underwent gastrectomy with vital indications between February 2012 and August 2018. Surgical and oncologic outcomes after laparoscopic surgery (laparoscopic surgery) and open surgery (OS) were compared.
Results
In total, 127 patients (LS, n = 52; OS, n = 75) were analyzed. Baseline characteristics were similar between the groups. Forty-four total gastrectomies with resection of the abdominal part of the esophagus, 63 distal subtotal (43 Billroth-I and 20 Billroth-II), and 19 proximal gastrectomies were performed. The median duration of surgery was significantly longer in the LS group, 253 min (interquartile range [IQR], 200–295) versus 210 min (IQR, 165–220) (p < 0.001), while median intraoperative blood loss in the LS group was significantly less, 180 ml (IQR, 146—214) versus 320 ml (IQR, 290–350), (p < 0.001). Early postoperative complications occurred in 35% in the LS group and in 45 % of patients in the OS group (p = 0.227). There was no difference in postoperative mortality rates between the groups (3 [6 %] versus 5 (7 %), p = 1.00). Median intensive care unit stay and median postoperative hospital stay were significantly shorter after laparoscopy, 2 (IQR, 1–2) versus 4 (IQR, 3–4) days, and 8 (IQR, 7–9) versus 10 (IQR, 8–12) days, both p < 0.001. After laparoscopy, patients started adjuvant chemotherapy significantly earlier than those after open surgery, 20 vs. 28 days (p < 0.001). However, overall survival rates were similar between the group. Three-year overall survival was 24% in the LS group and 27% in the OS groups.
Conclusions
Despite the technical complexity, in patients with complicated locally advanced and metastatic gastric cancer, laparoscopic gastrectomies were associated with longer operation time, reduced intraoperative blood loss, shorter reconvalescence, and similar morbidity, mortality rates and long-term oncologic outcomes compared to conventional open surgery.
Similar content being viewed by others
Introduction
Gastric cancer is the fourth leading cause of cancer death and the fifth most common cancer worldwide. Although there has been a decrease in its incidence and mortality in recent years, over one million new cases were newly diagnosed, and an estimated 769,000 deaths from gastric cancer occurred in 2020 [1]. The prognosis mainly depends on the disease stage at the diagnosis; and since patients are usually diagnosed with locally advanced or metastatic, the prognosis is poor [2,3,4]. Due to the absence of screening programs in most Western сountries, the late detection of gastric cancer is frequent and is often complicated by bleeding and/or stenosis. Current guidelines do not offer an ultimate standardized approach in the case of development of these complications. The vast majority of these patients receive palliative or symptomatic care, and only in about one fourth of cases, is it possible to perform curative surgery [5,6,7,8,9,10].
Bleeding from gastric cancer
The rate of successful endoscopic hemostasis in tumor bleeding, depending on the applied method, can be achieved in 31 to 100% of cases [11, 12], and the incidence of recurrent bleeding reaches 41% [13, 14], which complicates repeated endoscopic interventions and increases mortality [15]. Median overall survival after endoscopic hemostasis is approximately 3–6 months, and mortality (30 days) reaches 22% [13, 16].
The rate of successful hemostasis in transcatheter arterial embolization (TAE) ranges from 40 to 100%, the incidence of recurrent bleeding varies from 41 to 66%, and survival rates and 30-day mortality are 0.9–3.7 months and 25–60%, respectively [17,18,19,20,21].
Palliative radiation therapy at optimal doses is well-tolerated and improves the quality of life of patients with bleeding tumor. The rate of successful hemostasis varies from 50 to 80%, with a median overall survival varying from 2.1 to 5.3 months [22, 23].
Curative and cytoreductive surgeries increase the median survival to 12 months, but the incidents of early postoperative complications can reach 40% [24].
Malignant gastric obstruction
In the late-period after the application of self-expandable metallic stents (SEMS), 30–50% of patients require repeated interventions due to the complications, [25, 26] and survival of patients does not exceed three months [27].
Symptomatic surgeries (gastrostomy, jejunostomy, gastroenterostomy) in patients with tumor stenosis prolong survival only up to 7 months on average [27, 28]. In case of cytoreductive surgeries, survival rates are noticeably higher, median survival in this group is 10 to 13 months, and 46% of patients may complete adjuvant chemotherapy; at the same time, this parameter in patients after stenting and gastroenterostomy is 22% and 29%, respectively [27, 29].
Laparoscopic surgery has justified its efficacy in the treatment of early gastric cancer [30]. Limited data from Japan (JLSSG-0901), China (CLASS-01), and South Korea (KLASS-02) indicate the eligibility of laparoscopic interventions in patients with locally advanced gastric cancer [31,32,33,34]. The subject of the application of laparoscopic technologies on the late stages of gastric cancer remains unresolved, but new publications appear confirming the benefits of minimally invasive surgical interventions for these patients [35]. In this study, we analyze the feasibility and efficacy of laparoscopic gastrectomies in patients with complicated forms of advanced gastric cancer.
Material and methods
Study design and participants
We retrospectively assessed outcomes of patients with histologically confirmed locally advanced (the American Joint Committee on Cancer stage T2 and higher) and disseminated gastric cancer and complicated with bleeding and/or stenosis who underwent laparoscopic or open gastrectomy with vital indications between February 2012 and August 2018 in the N.N.Burdenko Departmental Surgery Clinic, affiliated with the Department of Faculty Surgery №1, I.M.Sechenov First Moscow State Medical University, Moscow, Russia. Surgical and oncologic outcomes after laparoscopic surgery (LS) and open-surgery (OS) were analyzed and compared.
Prior to making a decision on surgical treatment strategies, all patients were discussed at a multidisciplinary board meeting. Neoadjuvant chemotherapy was not conducted due to the severe condition of the patients. The choice of open or laparoscopic approach was made depending on the availability of a senior consultant surgeon experienced in the laparoscopic technique.
To establish a clinical diagnosis, before surgery, all patients underwent the following set of diagnostic investigations: esophagogastroduodenoscopy with biopsy, multi-position X-ray of the esophagus, stomach, and duodenum after oral contrast enhancement, contrast-enhanced multi-slice computer tomography of the chest, abdomen, and pelvis.
In case of severe cachexia and anemia before surgery, infusion therapy and additional enteral or parenteral nutrition were administrated.
All patients underwent assessment of the quality of life using the Karnofsky Performance Status (KPS) [36] and the Eastern Cooperative Oncology Group (ECOG) performance status scales [37] before and after (prior starting adjuvant chemotherapy, 18−28 days after surgery) surgery.
Operative technique
In all laparoscopic interventions, the patients were placed on a supine position on the operating table. Five trocars were used, which were aligned taking into account patients body build and the extent of intervention.
The extent of surgical intervention depended on the localization of the tumor process. In cases with total and subtotal tumorous affection, and tumors of the upper-third of the stomach, gastrectomy with resection of the abdominal esophagus was performed. Tumors located in the lower-third of the body and in the antral segment of the stomach, distal subtotal resection of the stomach was carried out. In case of the tumor location in the middle-third of the body of the stomach, distal subtotal resection of the stomach was performed if adequate resection was possible, in other cases—gastrectomy was carried out. One to 2 short and posterior gastric arteries were spared for blood supply to the stump. For tumors of the cardia, the method of choice was proximal resection of the stomach with resection of the abdominal and lower-thoracic segments of the esophagus, accompanied by an urgent pathological investigation of the resection margins (Fig. 1). In distal resections, B1 reconstruction (Fig. 2) was preferred, as it is functionally beneficial. The indication for the B2 resection of the stomach was tumor invasion into the pylorus and duodenum or spread to the large curvature closer to the left gastric artery.
After dissecting the duodenum with a linear stapler during gastrectomy, the staple line area was routinely sutured. Esophago-jejunal anastomosis in the LS group was performed in different ways: in 4 cases—with application of double-row intracorporal manual anastomosis (Fig. 3), in 3 cases—with the use of circular Orvil cross-linking apparatus (head diameter 21 and 25 mm), in other patients it was applied using supramedian minilaparotomy access.
Five to 7-cm-long pararectal minilaparotomy was used to remove the gross specimen and for B1 gastroduodenostomy.
Early postoperative period
Tube feeding was performed from 1 day via a nasointestinal tube, which was inserted intraoperatively in all patients. On the 3rd–4th day, a control x-ray with a water-soluble contrast was performed, and then the enteral nutrition was started with a gradual increase in volume. As a rule, on the 5th–7th day, the patient independently consumed the desired volume of liquid or strained food [38, 39]. Jejunostomy feeding in this series was not applied.
Statistics
Procedures were analyzed on intent to treat basis, i.e. cases converted to laparotomy were not excluded from the analyses. The data are presented as median (interquartile range [IQR]) or number (percentage). To compare proportions between groups, the chi-square test or the Fisher exact test were used as appropriate. The Mann-Whitney test was used to compare continuous variables for non-normally distributed variables, while the Student t test was used to compare normally distributed variables. The Kaplan-Meier method was applied for survival analyses. Time defined survival values were presented in percentage ± standard error. Log-rank test was applied for comparison of survival between groups. Length of survival was described as median (95% confidence interval [CI]). The reverse Kaplan-Meier method was used to calculate median follow-up of patients for overall survival.
Results
In total, 127 patients were analyzed. Of them, 52 patients underwent LS and 75 patients had traditional OS. In both groups, the number of male patients was higher, 35 (66%) in the LS and 48 (65%) in the OS group. The median age of patients was 63 years in the open group and 65 in the laparoscopy group (p value = 0.074). Physical status of patients before surgery according to ASA classification score was similar between the groups. Other baseline characteristics, such as ECOG score, comorbidities, body mass index, and gastric tumor localization were comparable (Table 1).
Nine patients in the LS group and 14 patients in the OS group, in addition to the tumor, had ulcerative lesions of the stomach and duodenum (p value = 0.845), requiring anti-ulcer therapy.
Forty-four gastrectomies with resection of abdominal esophagus, 44 Billroth-I subtotal resections, 20 Billroth-II subtotal resections, and 19 proximal resections were performed. The extent of gastrectomies were similar between the groups. Combined interventions were significantly higher in the OS group, 32 (62%) versus 59 (79%), p value = 0.035. Simultaneous surgeries were carried out in 27 cases. These were equally distributed between the groups (Table 2). Extended lymph node dissection (D2) was performed in 71% patients in LS group and 75 % patients in OS group (p value = 0.660). Distribution by stages according to the TNM 8 classification was as follows: IIB–8 patients (6.3%), IIIA–25 (19.7%), IIIB–24 (18.9%), IIIC–26 (20.5%), IV–44 (34.6%). This parameter was similar between the groups (Table 3).
In three (6%) patients, laparoscopy was converted to open surgery. In one case, electric injury of the proper hepatic artery occurred when dissecting a lymph node conglomerate from it. In this case, mini-laparotomy was performed and the injured wall of the artery was sutured. The patient developed an esophageal anastamotic leak postoperatively and died on the 13th postoperative day. In other 2 cases, conversion was performed due to the impossibility of mobilization caused by the massive invasion of the tumor into the root of the mesocolon, and the patients had uneventful postoperative recovery..
Median duration of surgery was significantly longer in the LS group—253 min (IQR, 200–295) versus 210 min (IQR, 165–220) in the OS group (p < 0.001), while median intraoperative blood loss in LS group was significantly less and amounted 180 ml (IQR, 146–214) versus 320 ml (IQR, 290–350, p < 0.001) (Table 3).
Median number of removed lymph nodes was comparable between the groups (24 (IQR, 18–25) versus 25 (IQR, 20–26), p = 0.063). 38 (73%) patients in the LS group and 54 (72%) in the OS group underwent radical (R0) gastrectomy (p = 0.688) (Table 3).
Median duration of stay in the intensive care unit after laparoscopic interventions was 2 days (IQR, 1–2), and median duration of the postoperative period was 8 days (IQR, 7–9). In the OS group, these parameters were significantly higher: 4 (IQR, 3–4) and 10 (IQR, 8–12) days, respectively (both p < 0.001).
Early postoperative complications in the LS group occurred in 35% and 45% of patients in LS and OS groups, respectively (p = 0.227) (Table 3). Detailed characteristics of postoperative complications are presented in Table 4.
There was no difference in postoperative mortality rates between groups (3 (6 %) in LS and 5 (7%) in OS groups, p = 1.00). In the LS group, one patient died on the 2nd postoperative day due to pulmonary embolism, another patient underwent repeated interventions after laparoscopic gastrectomy for esophagoenteroanastomosis dehiscence followed by multi-organ failure. Another patient died on the 8th day after laparoscopic proximal resection of the stomach due to respiratory failure against the background of bilateral polysegmental pneumonia. In the OS group, 3 patients died from pulmonary embolism, 2 patients died on the 10–12th day after surgery due to respiratory and cardiopulmonary failure.
High quality of life before surgery (90–100% according to the Karnofsky scale, 0–1 on the ECOG scale) was observed in 43 (83 %) and 61 (81%) patients in the LS and OS groups, respectively. After surgical treatment, this number increased to 49 (94%) in the LS and 63 (84%) in the OS group. The number of patients who assessed their condition after surgery at 100% on the Karnofsky scale and 0 on the ECOG scale increased 3-fold in LS and 2-fold in OS group (Table 5).
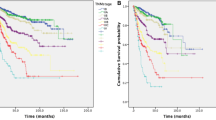
Median follow-up for overall survival was 56 months (95% CI, 36–76). Overall survival rates were similar between the groups. Median overall survival in the LS and OS groups were 18 (95% CI, 9–23) and 16 months (95% CI, 11–25) (Table 6, Fig. 4).
After the exclusion of patients with disseminated forms of gastric cancer, the median survival increased to 27 months (95% confidence interval, 16–38) in the LS group (n = 34) 22 months (95% CI, 16–38) in the OS group (p value = 0.842) (Fig. 5). For those with disseminated disease, the median overall survival was 8 months (95% confidence interval, 4–12) in the LS group (n = 26) and 11 months (95 % CI, 9–13) in the OS group (p value = 0.274) (Fig. 6).
Discussion
In this analysis of surgical and oncologic outcomes after laparoscopic and open gastrectomy for patients with locally advanced and metastatic gastric cancer complicated by bleeding and/or stenosis, we found that laparoscopy was associated with significantly less blood loss, shorter ICU and hospital stay, shorter duration of postoperative opioid analgesia, and longer operation time. Other perioperative results including postoperative morbidity and mortality and long-term oncologic outcomes, were similar to the conventional open approach. However, it needs to be stated that the number of patients who required combined procedures due tumor invasion and/or dissemination was higher in the open group.
Among those admitted to the specialized institutions, 80 to 90% of patients, present with locally advanced cancer, metastatic tumor or complications in the form of bleeding or stenosis [40, 41]. In these cases, taking into account the local spread of the process corresponding to stage III–IV, appropriate surgical intervention is an extremely difficult task.
Currently, there are three main strategies in the treatment of complicated gastric cancer: (1) extended curative surgical interventions; (2) cytoreductive and palliative surgeries; (3) conservative tactics based on the endoscopic procedures/fluoroscopic endovascular interventions. To date, curative interventions in case of complications of stage III and IV gastric cancer are challenging and possible in highly selected cases. Even after potentially curative surgery, most of the patients develop early disease recurrence [41].
There are various palliative and symptomatic treatment methods in case of complications of gastric cancer, but they do not provide satisfactory results. The median overall survival of patients after these interventions does not exceed 7 months [13, 16, 20, 22]. However, extended surgical intervention with a radical intention may prolong survival for these patients. The median overall survival after laparoscopic and open surgery in this cohort compiled 18 and 16 months, respectively. In patients with non-disseminated disease median overall survival reached 27 months in the LS group and 22 months in the OS group.
Current clinical guidelines do not offer a standardized approach in case of such complications of gastric cancer as bleeding from the tumor and progressive tumor stenosis.
The latest guidelines (2017) of the Japan Association for Investigation of Gastric Cancer in patients with locally advanced and metastatic gastric cancer with signs of bleeding or obstruction suggest palliative gastrectomy or bypass gastro-jejunostomy depending on the resectability of the primary tumor and surgical risks [6].
American Guidelines (NCCN, 2016) do not recommend active surgical tactics in case of the development of life-threatening complications [7]. In case of acute gastric cancer bleeding, the first options are endoscopic interventions, such as infiltration of the bleeding area, mechanical hemostasis with an endoscopic clamp, argon plasma coagulation, or a combination of various methods. At the same time, it is noted that the efficacy of endoscopic treatment of bleeding in patients with stomach cancer is not sufficiently studied, and the incidence of recurrent bleeding is very high. In case of stomach obstruction with tumor, endoscopic insertion of self-expanding metal stents or percutaneous puncture gastrostomy are performed.
Guidelines of the European Society of Medical Oncology (ESMO, 2016) do not contain any data on the treatment of patients with complicated gastric cancer. There is only casual indication that hypofractionated radiation therapy may be used for reduction of pain, to control bleeding, and in tumor obstruction [8].
In the Korean Clinical Guidelines (March, 2019) [9] based on the results of the discontinued REGATTA study, it is stated that for the treatment of complications (obstruction, bleeding, perforation, etc.), and in order to improve overall survival, palliative surgery is not recommended. However, they do not offer any other treatment options for these patients.
In RUSSCO Practical Guidelines for the Treatment of Gastric Cancer, it is noted that surgical resection of the primary unresectable locally advanced or disseminated/metastatic gastric cancer can be performed in life-threatening complications, which do not resolve with conservative treatment (perforation of the stomach, recurrent bleeding, tumor stenosis, etc.) [42].
Thus, treatment of patients with advanced forms, which include locally advanced (T2-4N0-3M0) and metastatic (M1) gastric cancer is unclear and widely discussed; at the same time, surgical treatment remains the only method that allows both to improve the quality of life of these patients and to increase survival, especially in cases complicated with bleeding, decompensated stenosis, etc.
Laparoscopic surgery has fully justified its efficacy in the treatment of early gastric cancer [43, 44]; however, limited data indicate the eligibility of laparoscopic interventions in local and disseminated processes. Although minimally invasive interventions in locally advanced gastric cancer are technically complex and time-consuming, the data suggest that they may be applied for long-term benefit [45]. In our series, when comparing minimally invasive and open surgeries, there was no significant difference between these two groups with respect to the number of resected lymph nodes, recurrence rate and survival. In addition, minimally invasive technologies provide the best short-term outcomes: low postoperative pain, early activation, faster recovery, and thus shorter intensive care and hospital stay. Considering the fact that the prognosis and the life expectancy of this group of patients is worse, the above mentioned advantages may be essential. Patients after laparoscopic surgeries had significantly higher quality of life, and shorter rehabilitation period allowing to begin the chemotherapy already in early postoperative period. In our series, patients that underwent laparoscopic surgery started their adjuvant chemotherapy significantly earlier than those after open surgery (20 vs 28 days, p value < 0.001)
The current analysis has obvious limitations and weaknesses. First, this is a retrospective study with its inherent biases including clear selection bias. Second, the analyzed population and the procedures are heterogeneous. Different types of gastrectomies with different combined and simultaneous procedures were performed. Finally, patients with locally advanced and metastatic disease complicated with bleeding or stenosis referred to palliative treatment were not included in this study, while a comparative analysis with those undergoing gastrectomy could be useful in understanding the role of both laparoscopic and open gastrectomy. All in all, well-designed, multicenter studies, and prospective registries are needed to assess the results of laparoscopic and open gastrectomy in this group of patients.
Conclusion
The obtained data indicate that despite the technical complexity, in patients with complicated locally advanced and metastatic gastric cancer, laparoscopic gastrectomies were associated with longer operation time, reduced intraoperative blood loss, shorter reconvalescence, and similar morbidity, mortality rates, and long-term oncologic outcomes compared to conventional open surgery. Based on our series, we recommend to apply laparoscopic approach to perform gastrectomy for this group of patients whenever possible
Availability of data and materials
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
References
Sung H, Ferlay J, Siegel RL, Laversanne M, Soerjomataram I, Jemal A, et al. Global cancer statistics 2020: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin. 2021;71(3):209–49.
Li S, Zang L. The Effectiveness of Gastrectomy With Chemoradiotherapy Among Stage IV Gastric Adenocarcinoma: A Population-Based Analysis. Front Oncol. 2020;10:630.
Sahakyan MA, Gabrielyan A, Aghayan DL, Yesayan S, Petrosyan H, Chobanyan A, et al. Gastrectomy for metastatic gastric cancer: a 15-year experience from a develo** country. Indian J Surg Oncol. 2019;10(3):527–34.
Allemani C, Matsuda T, Di Carlo V, Harewood R, Matz M, Nikšić M, et al. Global surveillance of trends in cancer survival 2000–14 (CONCORD-3): analysis of individual records for 37 513 025 patients diagnosed with one of 18 cancers from 322 population-based registries in 71 countries. Lancet. 2018;391(10125):1023–75.
Bickenbach K, Strong VE. Comparisons of Gastric Cancer Treatments: East vs. West. J Gastric Cancer. 2012;12(2):55–62.
Japanese Gastric Cancer A. Japanese gastric cancer treatment guidelines 2014 (ver. 4). Gastric Cancer. 2017;20(1):1–19.
Jaffer AA, Thomas ADA, Khaldoun A, David JB, Joseph C, Prajnan D, et al. Gastric Cancer, Version 3.2016, NCCN Clinical Practice Guidelines in Oncology. Journal of the National Comprehensive Cancer Network. J Natl Compr Cancer Netw. 2016;14(10):1286–312.
Smyth EC, Verheij M, Allum W, Cunningham D, Cervantes A, Arnold D. Gastric cancer: ESMO Clinical Practice Guidelines for diagnosis, treatment and follow-up†. Ann Oncol. 2016;27:v38–49.
Korean Practice Guideline for Gastric Cancer 2018: an evidence-based, multi-disciplinary approach. J Gastric Cancer. 2019;19(1):1–48.
Valletti M, Eshmuminov D, Gnecco N, Gutschow CA, Schneider PM, Lehmann K. Gastric cancer with positive peritoneal cytology: survival benefit after induction chemotherapy and conversion to negative peritoneal cytology. World J Surg Oncol. 2021;19(1):245.
Koh KH, Kim K, Kwon DH, Chung BS, Sohn JY, Ahn DS, et al. The successful endoscopic hemostasis factors in bleeding from advanced gastric cancer. Gastric Cancer. 2013;16(3):397–403.
Kawabata H, Hitomi M, Motoi S. Management of bleeding from unresectable gastric cancer. Biomedicines. 2019;7(3):54.
Park H, Ahn JY, Jung HY, Chun JH, Nam K, Lee JH, et al. Can endoscopic bleeding control improve the prognosis of advanced gastric cancer patients?: a retrospective case-control study. J Clin Gastroenterol. 2017;51(7):599–606.
Kim YI, Choi IJ, Cho SJ, Lee JY, Kim CG, Kim MJ, et al. Outcome of endoscopic therapy for cancer bleeding in patients with unresectable gastric cancer. J Gastroenterol Hepatol. 2013;28(9):1489–95.
Song IJ, Kim HJ, Lee JA, Park JC, Shin SK, Lee SK, et al. Clinical Outcomes of Endoscopic Hemostasis for Bleeding in Patients with Unresectable Advanced Gastric Cancer. J Gastric Cancer. 2017;17(4):374–83.
Kim YJ, Park JC, Kim EH, Shin SK, Lee SK, Lee YC. Hemostatic powder application for control of acute upper gastrointestinal bleeding in patients with gastric malignancy. Endosc Int Open. 2018;6(6):E700–e5.
Lu Y, Loffroy R, Lau JY, Barkun A. Multidisciplinary management strategies for acute non-variceal upper gastrointestinal bleeding. Br J Surg. 2014;101(1):e34–50.
Mirsadraee S, Tirukonda P, Nicholson A, Everett SM, McPherson SJ. Embolization for non-variceal upper gastrointestinal tract haemorrhage: a systematic review. Clin Radiol. 2011;66(6):500–9.
Yap FY, Omene BO, Patel MN, Yohannan T, Minocha J, Knuttinen MG, et al. Transcatheter embolotherapy for gastrointestinal bleeding: a single center review of safety, efficacy, and clinical outcomes. Dig Dis Sci. 2013;58(7):1976–84.
Meehan T, Stecker MS, Kalva SP, Oklu R, Walker TG, Ganguli S. Outcomes of transcatheter arterial embolization for acute hemorrhage originating from gastric adenocarcinoma. J Vasc Interv Radiol. 2014;25(6):847–51.
Park S, Shin JH, Gwon DI, Kim HJ, Sung KB, Yoon HK, et al. Transcatheter arterial embolization for gastrointestinal bleeding associated with gastric carcinoma: prognostic factors predicting successful hemostasis and survival. J Vasc Interv Radiol. 2017;28(7):1012–21.
Tey J, Zheng H, Soon YY, Leong CN, Koh WY, Lim K, et al. Palliative radiotherapy in symptomatic locally advanced gastric cancer: a phase II trial. Cancer Med. 2019;8(4):1447–58.
Tey J, Choo BA, Leong CN, Loy EY, Wong LC, Lim K, et al. Clinical outcome of palliative radiotherapy for locally advanced symptomatic gastric cancer in the modern era. Medicine (Baltimore). 2014;93(22):e118.
Wang XB, Yu QM, Yu PF, Zhang YL, Yang LT, Zhang ZW, et al. Surgical treatment of huge hepatocarcinoma with invasion or severe adhesion of diaphragm using the technique of orthotopic liver resection. Hepatogastroenterology. 2015;62(137):153–6.
Jeurnink SM, Steyerberg EW, Hof G, van Eijck CH, Kuipers EJ, Siersema PD. Gastrojejunostomy versus stent placement in patients with malignant gastric outlet obstruction: a comparison in 95 patients. J Surg Oncol. 2007;96(5):389–96.
Kim GH, Kang DH, Lee DH, Heo J, Song GA, Cho M, et al. Which types of stent, uncovered or covered, should be used in gastric outlet obstructions? Scand J Gastroenterol. 2004;39(10):1010–4.
Upchurch E, Ragusa M, Cirocchi R. Stent placement versus surgical palliation for adults with malignant gastric outlet obstruction. Cochrane Database Syst Rev. 2018;5(5):Cd012506.
Iwasaki H, Mizushima T, Suzuki Y, Fukusada S, Kachi K, Ozeki T, et al. Factors that affect stent-related complications in patients with malignant obstruction of the esophagus or gastric cardia. Gut Liver. 2017;11(1):47–54.
Zhang JZ, Lu HS, Huang CM, Wu XY, Wang C, Guan GX, et al. Outcome of palliative total gastrectomy for stage IV proximal gastric cancer. Am J Surg. 2011;202(1):91–6.
Ma J, Li X, Zhao S, Zhang R, Yang D. Robotic versus laparoscopic gastrectomy for gastric cancer: a systematic review and meta-analysis. World J Surg Oncol. 2020;18(1):306.
Inaki N, Etoh T, Ohyama T, Uchiyama K, Katada N, Koeda K, et al. A Multi-institutional, prospective, phase II feasibility study of laparoscopy-assisted distal gastrectomy with D2 lymph node dissection for locally advanced gastric cancer (JLSSG0901). World J Surg. 2015;39(11):2734–41.
Lee S-W, Etoh T, Ohyama T, Inaki N, Sakuramoto S, Yoshida K, et al. Short-term outcomes from a multi-institutional, phase III study of laparoscopic versus open distal gastrectomy with D2 lymph node dissection for locally advanced gastric cancer (JLSSG0901). J Clin Oncol. 2017;35(15_suppl):4029.
Yu J, Huang C, Sun Y, Su X, Cao H, Hu J, et al. Effect of laparoscopic vs open distal gastrectomy on 3-year disease-free survival in patients with locally advanced gastric cancer: the CLASS-01 randomized clinical trial. JAMA. 2019;321(20):1983–92.
Lee HJ, Hyung WJ, Yang HK, Han SU, Park YK, An JY, et al. Short-term outcomes of a multicenter randomized controlled trial comparing laparoscopic distal gastrectomy with D2 lymphadenectomy to open distal gastrectomy for locally advanced gastric cancer (KLASS-02-RCT). Ann Surg. 2019;270(6):983–91.
Khaled I, Priego P, Soliman H, Faisal M, Saad AI. Oncological outcomes of laparoscopic versus open gastrectomy after neoadjuvant chemotherapy for locally advanced gastric cancer: a retrospective multicenter study. World J Surg Oncol. 2021;19(1):206.
Karnofsky D, Burchenal J. Evaluation of chemotherpeutic agents, vol. 19. NY: NY Columbia Univ Published online; 1949.
Oken MM, Creech RH, Tormey DC, Horton J, Davis TE, McFadden ET, et al. Toxicity and response criteria of the Eastern Cooperative Oncology Group. Am J Clin Oncol. 1982;5(6):649–55.
Lassen K, Revhaug A. Early oral nutrition after major upper gastrointestinal surgery: why not? Curr Opin Clin Nutr Metab Care. 2006;9(5):613–7.
Mortensen K, Nilsson M, Slim K, Schäfer M, Mariette C, Braga M, et al. Consensus guidelines for enhanced recovery after gastrectomy: Enhanced Recovery After Surgery (ERAS®) Society recommendations. Br J Surg. 2014;101(10):1209–29.
Dicken BJ, Bigam DL, Cass C, Mackey JR, Joy AA, Hamilton SM. Gastric adenocarcinoma: review and considerations for future directions. Ann Surg. 2005;241(1):27–39.
Orditura M, Galizia G, Sforza V, Gambardella V, Fabozzi A, Laterza MM, et al. Treatment of gastric cancer. World J Gastroenterol. 2014;20(7):1635–49.
Besova N, Byakhov M, Konstantinova M, Lyadov V, Ter-Ovanesov M, Tryakin A. Practical recommendations for gastric cancer medication. Malignant Neoplasms. 2017;7(3-S2):248–60 [in Russian].
Zeng F, Chen L, Liao M, Chen B, Long J, Wu W, et al. Laparoscopic versus open gastrectomy for gastric cancer. World J Surg Oncol. 2020;18(1):20.
Wang Y, Wang Y, Wu W, Lu X, An T, Jiang J. Laparoscopic gastrectomy plus D2 lymphadenectomy is as effective as open surgery in terms of long-term survival: a single-institution study on gastric cancer. World J Surg Oncol. 2021;19(1):102.
Wu S-Y, Ho M-H, Chang H-M, Hsu K-F, Yu J-C, Chan D-C. Long-term oncologic result of laparoscopic versus open gastrectomy for gastric cancer: a propensity score matching analysis. World J Surg Oncol. 2021;19(1):101.
Acknowledgements
None
Funding
The authors did not receive any financial support for the research, authorship, and/or publication of this article. The study was performed as a part of clinical and academic positions of the authors.
Author information
Authors and Affiliations
Contributions
TVK—idea, patient treatment, analysis and interpretation, manuscript revision, supervision, administrative support. NMA—manuscript drafting, patient treatment, data collection, analysis, and interpretation. VGA—patient treatment, data collection, analysis and interpretation, manuscript revision. DLA—manuscript drafting, analysis, and interpretation. AMK—manuscript drafting, analysis and interpretation, supervision. The authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The establishment of the prospective database and the initiation of this study were approved by the Institutional Review Board. Written informed consent was obtained from all subjects.
Consent for publication
Not applicable.
Competing interests
TVK, NMA, VGA, DLA, and AMK have no conflict of interests or financial ties to disclose.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Khorobrykh, T.V., Abdulkhakimov, N.M., Agadzhanov, V.G. et al. Laparoscopic versus open surgery for locally advanced and metastatic gastric cancer complicated with bleeding and/or stenosis: short- and long-term outcomes. World J Surg Onc 20, 216 (2022). https://doi.org/10.1186/s12957-022-02674-3
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12957-022-02674-3