Abstract
Objective
To assess how inaccurately the body mass index (BMI) is used to diagnose obesity compared to body fat percentage (BF%) measurement and to compare the cardiometabolic risk in children and adolescents with or without obesity according to BMI but with a similar BF%.
Methods
A retrospective cross-sectional investigation was conducted including 553 (378 females/175 males) white children and adolescents aged 6–17 years, 197 with normal weight (NW), 144 with overweight (OW) and 212 with obesity (OB) according to BMI. In addition to BMI, BF% measured by air displacement plethysmography, as well as markers of cardiometabolic risk had been determined in the existing cohort.
Results
We found that 7% of subjects considered as NW and 62% of children and adolescents classified as OW according to BMI presented a BF% within the obesity range. Children and adolescents without obesity by the BMI criterion but with obesity by BF% exhibited higher blood pressure and C-reactive protein (CRP) in boys, and higher blood pressure, glucose, uric acid, CRP and white blood cells count, as well as reduced HDL-cholesterol, in girls, similar to those with obesity by BMI and BF%. Importantly, both groups of subjects with obesity by BF% showed a similarly altered glucose homeostasis after an OGTT as compared to their NW counterparts.
Conclusions
Results from the present study suggest increased cardiometabolic risk factors in children and adolescents without obesity according to BMI but with obesity based on BF%. Being aware of the difficulty in determining body composition in everyday clinical practice, our data show that its inclusion could yield clinically useful information both for the diagnosis and treatment of overweight and obesity.
Similar content being viewed by others
Background
Obesity prevalence has increased dramatically worldwide in the last decades [1]. Average body mass index (BMI) and prevalence of obesity has risen worldwide also in children and adolescents in the period 1975 to 2016 [2]. The global age-standardized prevalence of obesity observed in children and adolescents between 5 and 19 years old increased from 0.7 to 5.6% for girls and 0.9–7.8% for boys [2]. Likewise, prevalence has increased markedly in school children in developed countries with a 23.8% of boys and 22.6% of girls classified as having overweight or obesity in 2013 [3]. The medical definition of obesity considers it as a state of increased adipose tissue, not body weight, of a magnitude that might have a negative impact on health, being strongly associated with elevated morbidity and also mortality [4, 5]. In this sense, severe pediatric obesity is associated with an increased prevalence of cardiometabolic risk factors [6]. Moreover, it has been evidenced that development of obesity in early ages predicts obesity [7] and cardiovascular events [8] in adulthood.
Despite obesity being defined as an excessive amount of adipose tissue, the most frequently used clinical tool to diagnose obesity in children, adolescents and adults is the BMI, since measurement of body fat is rarely available in routine clinical practice. However, absolute cutoffs cannot be established in children and adolescents given that BMI distribution varies markedly with growth [9]. It is recommended to diagnose a child (> 2 years) or adolescent as with overweight if the BMI is ≥ 85th percentile and < 95th percentile for age and sex, and as with obesity if the BMI is ≥ 95th percentile [10]. Alternatively, the IOTF proposed age- and sex-specific BMI cutoffs for children and adolescents corresponding to the widely used adult obesity cutoffs of 25 and 30 kg/m2, pooling international data [11]. BMI shows a high specificity but low sensitivity to detect excess body fat percentage (BF%) at all ages [12], failing to identify around 25% of children with excess adiposity [13]. Moreover, epidemiological studies analyzing the degree of misclassification using BMI to diagnose obesity in pediatric population as well as the impact of BF% on the levels of cardiometabolic risk factors in children and adolescents are scarce [14, 15]. Since BF% has been shown to determine cardiometabolic risk even in subjects with a BMI within the normal range [12, 16] at the same time as being related to all-cause mortality in adults [17], we hypothesized that already in early ages identifying the clinical use of BF% measurement in determining the cardiometabolic risk linked with obesity in pediatric patients may be crucial.
With this purpose, we used data from an existing cohort of a cross-sectional investigation with two objectives: first, to determine the degree of misclassification in obesity diagnosis with the use of BMI as compared to the direct measurement of BF% in children and adolescents. Second, to evaluate whether the cardiometabolic risk factor profile in subjects without obesity according to BMI but classified as with obesity by BF% cutoff points is different from that of subjects with obesity defined by BMI with a similar BF%.
Methods
Study design and participants
A retrospective cross-sectional analysis was performed with 553 (378 females/175 males) white children and adolescents, aged 6–17 years, recruited for previous studies between January 2001 to February 2019 at the Pediatric Endocrinology Unit and the Dpt. of Endocrinology & Nutrition from the Clínica Universidad de Navarra (Pamplona, Spain), either for an annual routine health check-up (healthy children without long-term diseases) or consulting due to excess weight as previously described [18,19,20]. Children and adolescents were classified on the basis of age- and sex-specific BMI cutoffs as defined by Cole et al. [11]. Pubertal status was evaluated by a pediatrician and determined using the Tanner stage [21]. None of the participants was taking medication potentially affecting body composition.
A subset (subcohort 1) of 360 subjects (232 females/128 males) was considered in the subanalysis used to compare the cardiometabolic risk between individuals classified by BMI as without obesity and with obesity, but with a similar BF%. The analysis included as the group of reference the subjects classified as normal weight (NW) by both the Cole classification and BF% (Normal, 119 girls and 35 boys), and compared it to those classified as without obesity (with NW or overweight) by Cole but with obesity by BF% (NOOB, 52 girls and 39 boys) as well as to a BF%-matched group of subjects classified as having obesity by both Cole and BF% (OBOB, 61 girls and 54 boys). We followed a similar design as the one previously performed in adults [12], but using Cole’s classification instead as the usual BMI cutoff points used for adults.
In order to explore the effect of body composition on glucose metabolism, glucose and insulin curves were determined during an oral glucose tolerance test (OGTT) in a representative subgroup (n = 58, 5 Normal, 17 NOOB and 36 OBOB, subcohort 2) in whom OGTT was available. The study followed the ethical standards of the Declaration of Helsinki and the experimental protocol was approved by the Research Ethical Committee of the Universidad de Navarra (protocol 2020.236). Signed informed consent was obtained from the parents or legal guardians and from the participants over 12 years old. Children under 12 years assented to participate.
Anthropometric measurements
The body composition and the anthropometric determinations as well as the blood sampling were performed on the same day. Height was measured with a Holtain stadiometer (Holtain, Crymych, UK), while body weight was determined with the air displacement plethysmography (ADP) calibrated electronic scale with individuals wearing a swimming suit. BMI was calculated as dividing weight in kg by the square of height in m. Waist circumference was determined at the midpoint placed between the iliac crest and the rib cage on the midaxillary line. Hip circumference was determined at the position yielding the maximum circumference over the buttocks. Blood pressure was measured after a 5-minute rest with a sphygmomanometer. Blood pressure was determined 3 times at the right upper arm and the average was used in the analyses.
Body composition
Body density was calculated by ADP (Bod-Pod®, COSMED, Albano Laziale, Italy). Data for calculation of body fat by this plethysmographic technique has been published to agree closely with the classic gold standard underwater weighing (hydrodensitometry) in children [20, 22] and has been used as the reference method to validate other body composition measurements in children [23]. The Siri equation was used to calculate BF% from body density. Cutoff points for BF% utilized for defining overweight (20.1–24.9% for boys and 30.1–34.9% for girls) and obesity (≥25.0% for boys and ≥35.0% for girls) were similar to those most frequently used in the literature [14, 24,25,26].
Blood biochemistry
Plasma and serum samples were obtained in the morning after an overnight fast to avoid potential confounding bias due to hormonal rhythms. Plasma glucose was measured by an automated analyzer (Modular P800, Roche, Basel, Switzerland) as previously reported [20, 27]. Insulin was quantified using an enzyme-amplified chemiluminescence assay (Immulite®, Diagnostic Products, Los Angeles, CA, USA). The homeostatic model assessment (HOMA) and the quantitative insulin sensitivity check index (QUICKI) were used as proxies of insulin resistance and insulin sensitivity, respectively. Triglyceride and total cholesterol concentrations were measured by enzymatic spectrophotometric methods (Roche). HDL-cholesterol was determined by a colorimetric method in a Beckman Synchron® CX analyzer (Beckman Instruments, Bucks, UK). LDL-cholesterol was estimated by the Friedewald formula. High-sensitivity C-reactive protein (CRP) was determined by the Tina-quant® CRP (Latex) ultrasensitive assay (Roche, Basel, Switzerland). Number of white blood cells (WBC) was studied using an automated cell counter (Beckman Coulter, Fullerton, CA, USA). Uric acid, alanine aminotransferase (ALT), aspartate aminotransferase (AST), γ-glutamyltransferase (γ-GT), and creatinine were determined by enzymatic tests (Roche). Leptin was quantified by a RIA method (Linco Research, St. Charles, MO, USA); intra-and inter-assay coefficients of variation were 5.0% and 4.5%, respectively.
Statistical analysis
Data are presented as mean ± standard deviation (SD). Differences between groups were analyzed by ANOVA followed by Scheffé’s tests or Fisher’s Least Significant Differences, as appropriate. Log transformed CRP concentrations were used given their non-normal distribution. The remaining variables followed an adequate distribution for the application of parametric tests. Correlations between two variables were determined by Pearson (r) correlation coefficient. The calculations were performed by SPSS version 23 (Chicago, IL, USA) and GraphPad Prism 8 (La Jolla, CA, USA). P values lower than 0.05 were considered statistically significant.
Results
Baseline characteristics of the children and adolescents
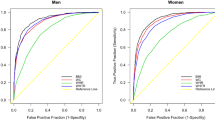
The study population included 197 children and adolescents with NW, 144 with overweight and 212 with obesity according to Cole’s BMI-based classification (Table 1). Boys exhibited higher weight, BMI, waist-to-hip ratio (WHR), waist-to-height ratio (WHtR), visceral adiposity and blood pressure, while girls showed increased BF% as expected, as usually girls have a higher BF% than boys. Average Tanner stage was higher in girls, since they were slightly older (without significant differences in age) and puberty takes place before in girls (Table 1). Analyzing the whole cohort of children and adolescents, BMI and BF% showed a strong correlation (r = 0.79; P < 0.001), which following stratification by gender was stronger for females (r = 0.85; P < 0.001) and weaker for males (r = 0.75; P < 0.001) (Fig. 2A).
Flow chart of children and adolescents included in the global sample and in the different substudies. NW, normal weight by both the Cole classification and BF%; NOOB, individuals classified as without obesity (with NW or overweight) by Cole but with obesity by BF%; OBOB, BF%-matched group of subjects classified as having obesity by both Cole and BF%; OGTT, oral glucose tolerance test
Association of body mass index and body fat percentage stratified by gender in children and adolescents. A) Left: girls (n = 378). Right: boys (n = 175). Horizontal lines delimit cutoffs for defining overweight and obesity according to BF% (30.0 and 35.0% in girls and 20.0 and 25.0% in boys, respectively). B) Classification of subjects as normal, with overweight or with obesity according to body mass index (Cole’s classification) or body fat percentage. Overweight was defined as BF% between 20.1–24.9% in boys or between 30.1–34.9% in girls, while obesity was defined as BF ≥25.0% in boys or ≥35.0% in girls
Use of BMI misclassifies children and adolescents according to BF%
The classification of the subjects of the global cohort as with NW, overweight or obesity according to either Cole’s classification or BF% is depicted in Figs. 2B and Supplementary Fig.1. Depending on the criterion utilized, considerable discrepancies were found for classification. On the basis of the real BF% figures, 22% of the NW participants by the established BMI criteria were misclassified, exhibiting either overweight (15%) or obesity (7%) taking in account their BF%, while only 2% of subjects with obesity using BMI were NW according to BF%. Furthermore, 62% of those subjects classified as having overweight according to Cole had actually obesity considering their BF% (Fig. 2B and Supplementary Fig. 1). This misclassification was higher in boys (15% of those classified as NW by Cole’s had obesity by BF%, while 78% of those with overweight based on BMI had obesity by BF%), than in girls (5% of those classified as NW by Cole’s had obesity according to their BF% and 55% of girls classified as overweight according to BMI had obesity by BF%). The misclassification is also visible in the scatter-plots that compare BF% with BMI with the cutoff points indicated by reference lines for both girls and boys (Fig. 2A). In the global cohort, Cole’s classification had a specificity of 94% and a sensitivity of 66% to detect children and adolescents with obesity according to BF%.
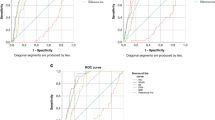
Glucose (A) and insulin (B) curves during an oral glucose tolerance test in 58 children and adolescents (subcohort 2) classified as normal weight by both Cole classification and body fat percentage (BF%) (Normal), as without obesity by Cole but with obesity by BF% (NOOB) or as having obesity by both Cole and BF% (OBOB). Data are mean ± SD. Differences between groups were computed by ANOVA followed by LSD tests. *P < 0.05 vs. Normal group
Increased cardiometabolic risk factors in children and adolescents without obesity according to BMI but with obesity based on BF%
In order to analyze the impact of the detected incorrect classification on the potential underestimation of the cardiometabolic risk associated with obesity, several risk factors were compared in subjects with a similar BF% well within the obesity range but considered either as non-obese (NOOB) or obese (OBOB) by Cole’s classification (subcohort 1). According to these criteria of matching, although boys from the OBOB group exhibited a higher BMI (P < 0.001) than those of the NOOB group, both groups had similar BF% (BF% approx. 35%; P = 0.998), which was well within the obesity range (Table 2). Both groups exhibited higher waist circumference (P < 0.001) and WHtR (P < 0.001) than the NW group being higher in the OBOB group. In the groups with obesity according to BF% WHtR was > 0.50 suggesting increased cardiometabolic risk in those patients. Interestingly, no differences in both WHR (P = 0.527) and visceral fat (P = 0.244) were observed between the groups with obesity by BF%. Systolic blood pressure (SBP) was elevated in the NOOB group and further raised in the OBOB group (P = 0.035 vs. NOOB), while no differences were observed in diastolic blood pressure (DBP) (P = 0.097). Plasma glucose levels were similar between the three groups. However, insulin concentrations, HOMA and QUICKI were altered only in the OBOB group (P < 0.05, as compared to NOOB). Serum triglyceride levels were increased in the OBOB group as compared to the other groups (P < 0.001 and P < 0.05, as compared to the NW and NOOB groups, respectively). Total, LDL- and HDL-cholesterol serum levels were overall similar in the three groups. No differences in uric acid, ALT or the AST/ALT ratio were observed. However, γ-GT levels were increased only in the NOOB (P < 0.01 vs. NW). Interestingly, the marker of inflammation CRP was significantly higher in both groups with obesity (P < 0.05 and P < 0.01, NW vs. NOOB, and NW vs. OBOB, respectively) showing no differences between them (P = 0.670). As expected, leptin levels were significantly elevated in both groups with obesity (P = 0.002 vs. NW), exhibiting no differences between them (P = 0.957).
In girls, BMI, waist circumference, WHR, WHtR and visceral fat were significantly increased in both groups with obesity, being higher in the OBOB in comparison to the NOOB group, while BF%, as the matching criterion, was similar in both groups with obesity according to adiposity (BF approx. 41%; P = 0.219). Comparable to what was shown in boys, CRP and leptin levels were increased in the NOOB and OBOB groups as compared to NW (P < 0.05) exhibiting no differences between them. Moreover, both groups of girls with obesity showed altered blood pressure, fasting glucose levels, HDL-cholesterol, uric acid and WBC as compared to NW (P < 0.01), but exhibiting no differences between them. Given that the pubertal state can decidedly influence body composition, data were analyzed according to Tanner stage. Noteworthy, no differences regarding the Tanner staging were observed, being similar between groups (Table 2 and Supplementary Table 1).
Children and adolescents without obesity according to BMI but with obesity based on BF% exhibit altered glucose tolerance
In order to further explore the potential impact of the increased adiposity on glucose homeostasis we analyzed a subsample of the pediatric patients (n = 58) in whom OGTT was available (subcohort 2). Both groups of children and adolescents with obesity according to adiposity exhibited a higher area under the glucose curve as compared to the NW group (Fig. 3A). Significantly higher values of glucose levels were found in both groups with obesity 90 min after glucose intake (NW 87 ± 10, NOOB 118 ± 32 and OBOB 120 ± 24 mg/dL; P = 0.030), while 120 min after glucose intake, glucose levels were only significantly different in the OBOB group as compared to the NW one, being similar to that of the NOOB group (NW 84 ± 13, NOOB 101 ± 17 and OBOB 111 ± 25 mg/dL; P = 0.026). Insulin curves after glucose intake in the groups with obesity according to BF% were slightly higher than those of the NW group, but the differences were not statistically significant (Fig. 3B).
Discussion
Obesity can be defined as an excessive accumulation of adipose tissue, and the degree of this excess is associated with the development of comorbidities [28,29,30,31,32]. We report herein that 7% of children and adolescents classified as having NW according to BMI, and 62% of those classified as overweight according to BMI had a BF% in the obesity range. On the other hand, only 2% and 4% of the children and adolescents with a BF% in the NW or overweight range, respectively, were misclassified as having obesity according to the BMI value. These results confirm that BMI, despite being a very practical and highly useful tool for epidemiological investigations, underestimates BF particularly in the overweight category, even at early ages. Published results showed an average sensitivity of 73–82% to detect severe adiposity and a mean specificity of 93–96% [13, 33]. This suggests that children and adolescents classified as having obesity by BMI (independently of the BMI-based criteria used) can almost definitely be considered as having obesity, while over a quarter of children not classified as having obesity by BMI might indeed have excess adiposity [13]. In the present study we found a similar 30.2% of children and adolescents classified as not having obesity according to BMI that actually exhibited a BF% within the obesity range, and an additional 14.7% of children pertaining to the NW group that had a BF% within the OW range. These findings indicate a notable degree of misclassification regarding the diagnosis of overweight and obesity in routine clinical practice using only BMI classifications, which translates in the underdiagnosis of children and adolescents at risk. This poses missed opportunities to identify patients with an increased cardiometabolic risk and to treat this life-threatening disease, similarly, although to a lesser degree, as it occurs in adults [12, 13, 34].
It has been shown that BF% and obesity elevates the risk of cardiovascular disease and T2D in adults [32, 35]. However, epidemiological studies which analyze the relation between BF% and blood levels of cardiometabolic risk markers in pediatric populations are scarce. Our study evidences for the first time that cardiometabolic risk factors are similarly altered in children and adolescents classified as with NW or overweight using BMI but with BF% within the obesity range that in those classified by BMI as having obesity with matched BF%. Data from the present study show that subjects without obesity by the BMI criterion but with obesity by BF% exhibit higher blood pressure and CRP in boys, and higher blood pressure, glucose, uric acid, CRP and WBC count, as well as reduced HDL, in girls, similarly to children and adolescents with obesity by both BMI and BF%. Importantly, both groups of school children with obesity by BF% showed altered glucose homeostasis in the OGTT as compared to their NW counterparts. These observations point out that by using the BMI-based classification systems for the diagnosis of obesity without directly assessing the body composition a huge opportunity of detecting children and adolescents with increased cardiometabolic risk factors due to excess adiposity who in the following years may have more serious conditions is being lost. Additionally, our data offer a scientific justification for the observation that body composition underlies the better understanding of the cardiovascular risk in “normal-weight” individuals with elevated adiposity [36,37,38].
Studies analyzing the impact of BF% on cardiometabolic risk factors in children and adolescents are scarce and have been predominantly focused on comparing the influence of adipose tissue distribution rather than to study the effect of increased adiposity itself [39, 40]. In this sense, BF% shows lower [41], similar [38] or higher [42, 43] association with cardiometabolic risk factors than measures of central adiposity. The present study indicates that the real amount of body fat plays a major role in the elevated cardiometabolic risk in children and adolescents. In this regard, the utilization of BF% cutoff points for the diagnostic of obesity allows the detection of more children and adolescents with increased cardiometabolic risk than the mere application of the BMI-based classification criteria [34]. The importance of adiposity distribution should not be underestimated. In the present study, boys did not present differences in WHR and visceral fat between the two groups with high adiposity, a finding that was not observed in girls, who exhibited lower values than males. Larger studies will be needed to analyze the influence of the amount and distribution of adiposity on cardiometabolic risk in children and adolescents.
The present study highlights the importance of determining body composition for the diagnosis of obesity even at early ages. This observation is particularly important taking into account the pathophysiological implications that elevated adiposity exerts in the context of normal- or over-weight. Although BMI is frequently employed as a proxy measure of body fat, it does not provide information on body composition, as demonstrated herein. Therefore, the solution is not reducing or changing the BMI cutoff values, something that would reduce specificity [13], but analyze in more detail body composition and distribution [44]. This is particularly necessary in the era of precision medicine [45]. Our study provides proof that a similar unfavorable cardiometabolic risk factor profile currently exists in children and adolescents with a non-obese BMI but a highly elevated adiposity compared to their counterparts with a BMI-based diagnostic of obesity.
One potential limitation of the present study pertains to the generalizability to other pediatric populations. This investigation was conducted in white children and adolescents and would need to be confirmed in other populations in order to determine ethnic or race-specific differences as regards to BF% ranges for a given BMI and whether the significant associations with the cardiometabolic risk factors are maintained [46]. Another potential limitation may relate to using Cole’s BMI classification system while there are other BMI-based criteria for the diagnosis of obesity in children and adolescents [47, 48]. However, the misclassification is consistently observed using different criteria [13]. Moreover, it could be viewed also as a strength since Cole’s BMI classification is not subject to the existing epidemiological influences and regional differences of z-scores or percentiles.
Conclusion
The utilization of BMI for the diagnosis of obesity in children and adolescents in routine clinical practice underestimates the actual prevalence of this life-threatening disease given its association with the increase of cardiometabolic risk factors. Our study indicates that a marked number of children and adolescents with obesity according to their BF% are at risk of being underdiagnosed, and, therefore, opportunities for the most appropriate treatment instauration and comorbidity evaluation are being missed. In this regard, acknowledging how challenging it is to determine body composition in routine clinical practice, our data evidence that the inclusion of body composition measurements together with the assessment of morbidity for the diagnosis and the instauration of the most adequate treatment of obesity would be advisable.
Data Availability
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
References
Catalán V, Avilés-Olmos I, Rodríguez A, Becerril S, Fernández-Formoso JA, Kiortsis D, Portincasa P, Gómez-Ambrosi J, Frühbeck G. Time to consider the Exposome hypothesis in the development of the obesity pandemic. Nutrients. 2022;14:1597.
Collaboration NRF. Worldwide trends in body-mass index, underweight, overweight, and obesity from 1975 to 2016: a pooled analysis of 2416 population-based measurement studies in 128.9 million children, adolescents, and adults. Lancet. 2017;390:2627–42.
Ng M, Fleming T, Robinson M, Thomson B, Graetz N, Margono C, Mullany EC, Biryukov S, Abbafati C, Abera SF, et al. Global, regional, and national prevalence of overweight and obesity in children and adults during 1980–2013: a systematic analysis for the global burden of Disease Study 2013. Lancet. 2014;384:766–81.
Yárnoz-Esquiroz P, Olazarán L, Aguas-Ayesa M, Perdomo CM, García-Goni M, Silva C, Fernández-Formoso JA, Escalada J, Montecucco F, Portincasa P, et al. Obesities’: position statement on a complex disease entity with multifaceted drivers. Eur J Clin Invest. 2022;52:e13811.
Perdomo CM, Cohen RV, Sumithran P, Clement K, Frühbeck G. Contemporary medical, device, and surgical therapies for obesity in adults. Lancet. 2023;401:1116–30.
Skinner AC, Perrin EM, Moss LA, Skelton JA. Cardiometabolic risks and severity of obesity in children and young adults. N Engl J Med. 2015;373:1307–17.
Ward ZJ, Long MW, Resch SC, Giles CM, Cradock AL, Gortmaker SL. Simulation of growth trajectories of childhood obesity into adulthood. N Engl J Med. 2017;377:2145–53.
Jacobs DR Jr, Woo JG, Sinaiko AR, Daniels SR, Ikonen J, Juonala M, Kartiosuo N, Lehtimaki T, Magnussen CG, Viikari JSA, et al. Childhood cardiovascular risk factors and adult cardiovascular events. N Engl J Med. 2022;386:1877–88.
Wright CM, Cole TJ, Fewtrell M, Williams JE, Eaton S, Wells JC. Body composition data show that high BMI centiles overdiagnose obesity in children aged under 6 years. Am J Clin Nutr. 2022;116:122–31.
Hampl SE, Hassink SG, Skinner AC, Armstrong SC, Barlow SE, Bolling CF, Avila Edwards KC, Eneli I, Hamre R, Joseph MM, et al. Clinical practice guideline for the evaluation and treatment of children and adolescents with obesity. Pediatrics. 2023;151:e2022060640.
Cole TJ, Bellizzi MC, Flegal KM, Dietz WH. Establishing a standard definition for child overweight and obesity worldwide: international survey. BMJ. 2000;320:1240–3.
Gómez-Ambrosi J, Silva C, Galofré JC, Escalada J, Santos S, Millán D, Vila N, Ibañez P, Gil MJ, Valentí V, et al. Body mass index classification misses subjects with increased cardiometabolic risk factors related to elevated adiposity. Int J Obes. 2012;36:286–94.
Javed A, Jumean M, Murad MH, Okorodudu D, Kumar S, Somers VK, Sochor O, Lopez-Jimenez F. Diagnostic performance of body mass index to identify obesity as defined by body adiposity in children and adolescents: a systematic review and meta-analysis. Pediatr Obes. 2015;10:234–44.
Williams DP, Going SB, Lohman TG, Harsha DW, Srinivasan SR, Webber LS, Berenson GS. Body fatness and risk for elevated blood pressure, total cholesterol, and serum lipoprotein ratios in children and adolescents. Am J Public Health. 1992;82:358–63.
Dangardt F, Charakida M, Georgiopoulos G, Chiesa ST, Rapala A, Wade KH, Hughes AD, Timpson NJ, Pateras K, Finer N, et al. Association between fat mass through adolescence and arterial stiffness: a population-based study from the Avon Longitudinal Study of parents and children. Lancet Child Adolesc Health. 2019;3:474–81.
Gómez-Ambrosi J, Silva C, Galofré JC, Escalada J, Santos S, Gil MJ, Valentí V, Rotellar F, Ramírez B, Salvador J, et al. Body adiposity and type 2 diabetes: increased risk with a high body fat percentage even having a normal BMI. Obesity. 2011;19:1439–44.
Flegal KM, Graubard BI. Estimates of excess deaths associated with body mass index and other anthropometric variables. Am J Clin Nutr. 2009;89:1213–9.
Azcona C, Köek N, Frühbeck G. Fat mass by air-displacement plethysmography and impedance in obese/non-obese children and adolescents. Int J Pediatr Obes. 2006;1:176–82.
Gómez-Ambrosi J, Azcona C, Patiño-García A, Frühbeck G. Serum amyloid A concentration is increased in obese children and adolescents. J Pediatr. 2008;153:71–5.
Zapata JK, Catalán V, Rodríguez A, Ramírez B, Silva C, Escalada J, Salvador J, Calamita G, Azcona-Sanjulian MC, Frühbeck G, et al. Resting energy expenditure is not altered in children and adolescents with obesity. Effect of age and gender and association with serum leptin levels. Nutrients. 2021;13:1216.
Berenbaum SA, Beltz AM, Corley R. The importance of puberty for adolescent development: conceptualization and measurement. Adv Child Dev Behav. 2015;48:53–92.
Fields DA, Goran MI, McCrory MA. Body-composition assessment via air-displacement plethysmography in adults and children: a review. Am J Clin Nutr. 2002;75:453–67.
Gutierrez-Marin D, Escribano J, Closa-Monasterolo R, Ferre N, Venables M, Singh P, Wells JC, Munoz-Hernando J, Zaragoza-Jordana M, Gispert-Llaurado M, et al. Validation of bioelectrical impedance analysis for body composition assessment in children with obesity aged 8-14y. Clin Nutr. 2021;40:4132–9.
Taylor RW, Falorni A, Jones IE, Goulding A. Identifying adolescents with high percentage body fat: a comparison of BMI cutoffs using age and stage of pubertal development compared with BMI cutoffs using age alone. Eur J Clin Nutr. 2003;57:764–9.
McCarthy HD, Cole TJ, Fry T, Jebb SA, Prentice AM. Body fat reference curves for children. Int J Obes (Lond). 2006;30:598–602.
Salmón-Gómez L, Catalán V, Frühbeck G, Gómez-Ambrosi J. Relevance of body composition in phenoty** the obesities. Rev Endocr Metab Disord. 2023. https://doi.org/10.1007/s11154-023-09796-3.
Gómez-Ambrosi J, Catalán V, Rodríguez A, Andrada P, Ramírez B, Ibañez P, Vila N, Romero S, Margall MA, Gil MJ, et al. Increased cardiometabolic risk factors and inflammation in adipose tissue in obese subjects classified as metabolically healthy. Diabetes Care. 2014;37:2813–20.
Frühbeck G, Gómez-Ambrosi J. Control of body weight: a physiologic and transgenic perspective. Diabetologia. 2003;46:143–72.
Chung ST, Onuzuruike AU, Magge SN. Cardiometabolic risk in obese children. Ann N Y Acad Sci. 2018;1411:166–83.
Kim JY, Bacha F, Tfayli H, Michaliszyn SF, Yousuf S, Arslanian S. Adipose tissue insulin resistance in youth on the spectrum from normal weight to obese and from normal glucose tolerance to impaired glucose tolerance to type 2 diabetes. Diabetes Care. 2019;42:265–72.
Jebeile H, Kelly AS, O’Malley G, Baur LA. Obesity in children and adolescents: epidemiology, causes, assessment, and management. Lancet Diabetes Endocrinol. 2022;10:351–65.
Cypess AM. Reassessing human adipose tissue. N Engl J Med. 2022;386:768–79.
Simmonds M, Llewellyn A, Owen CG, Woolacott N. Simple tests for the diagnosis of childhood obesity: a systematic review and meta-analysis. Obes Rev. 2016;17:1301–15.
Ryder JR, Kaizer AM, Rudser KD, Daniels SR, Kelly AS. Utility of body mass index in identifying excess adiposity in youth across the obesity spectrum. J Pediatr. 2016;177:255–61.
Heymsfield SB, Wadden TA. Mechanisms, pathophysiology, and management of obesity. N Engl J Med. 2017;376:254–66.
Segal KR, Dunaif A, Gutin B, Albu J, Nyman A, Pi-Sunyer FX. Body composition, not body weight, is related to cardiovascular disease risk factors and sex hormone levels in men. J Clin Invest. 1987;80:1050–5.
Blüher M. Metabolically healthy obesity. Endocr Rev. 2020;41:bnaa004.
Van Hulst A, Ybarra M, Mathieu ME, Benedetti A, Paradis G, Henderson M. Determinants of new onset cardiometabolic risk among normal weight children. Int J Obes (Lond). 2020;44:781–9.
Viitasalo A, Schnurr TM, Pitkanen N, Hollensted M, Nielsen TRH, Pahkala K, Atalay M, Lind MV, Heikkinen S, Frithioff-Bojsoe C, et al. Abdominal adiposity and cardiometabolic risk factors in children and adolescents: a mendelian randomization analysis. Am J Clin Nutr. 2019;110:1079–87.
Raheem J, Sliz E, Shin J, Holmes MV, Pike GB, Richer L, Gaudet D, Paus T, Pausova Z. Visceral adiposity is associated with metabolic profiles predictive of type 2 diabetes and myocardial infarction. Commun Med (Lond). 2022;2:81.
** B, Lin H, Yuan J, Dong G, Huang K, Wu W, Chen X, Zhang L, Wang J, Liang X, et al. Abdominal adiposity and total body fat as predictors of cardiometabolic health in children and adolescents with obesity. Front Endocrinol (Lausanne). 2020;11:579.
Hetherington-Rauth M, Bea JW, Lee VR, Blew RM, Funk JL, Lohman TG, Going SB. Relationship between fat distribution and cardiometabolic risk in hispanic girls. Am J Hum Biol. 2018;30:e23149.
Fu L, Cheng H, Zhao X, Hou D, **e X, Mi J. Distinct causal effects of body fat distribution on cardiometabolic traits among children: findings from the BCAMS study. Nutr Metab Cardiovasc Dis. 2022;32:1753–65.
Yan Y, Liu J, Zhao X, Cheng H, Huang G, Mi J, China CACHSR. Group: Regional adipose compartments confer different cardiometabolic risk in children and adolescents: The China Child and Adolescent Cardiovascular Health Study. Mayo Clin Proc. 2019;94:1974-82.
Frühbeck G, Kiortsis DN, Catalán V. Precision medicine: diagnosis and management of obesity. Lancet Diabetes Endocrinol. 2018;6:164–6.
WHO Expert Consultation. Appropriate body-mass index for asian populations and its implications for policy and intervention strategies. Lancet. 2004;363:157–63.
Barlow SE, Expert C. Expert committee recommendations regarding the prevention, assessment, and treatment of child and adolescent overweight and obesity: summary report. Pediatrics. 2007;120(Suppl 4):164–92.
Kartiosuo N, Ramakrishnan R, Lemeshow S, Juonala M, Burns TL, Woo JG, Jacobs DR Jr, Daniels SR, Venn A, Steinberger J, et al. Predicting overweight and obesity in young adulthood from childhood body-mass index: comparison of cutoffs derived from longitudinal and cross-sectional data. Lancet Child Adolesc Health. 2019;3:795–802.
Acknowledgements
The authors gratefully acknowledge the valuable collaboration of all the members of the Nutrition Unit for their technical support. The authors also wish to thank all subjects who participated in this study.
Funding
This study was funded by Plan Estatal I + D + I from the Spanish Instituto de Salud Carlos III–Subdirección General de Evaluación y Fomento de la Investigación–FEDER (grants number PI20/00080, PI20/00927 and PI22/00745) and CIBEROBN, ISCIII, Spain; Dpt. of Health 58/2021, Gobierno de Navarra-FEDER, Spain; and Dpt. of University, Innovation and Digital Transformation PC098-099 MEPERTROBE, Gobierno de Navarra, Spain. The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
Author information
Authors and Affiliations
Contributions
G.F. and J.G.-A. designed the study and obtained the funds. J.K.Z., G.F. and J.G.-A. analyzed and interpreted the data. G.F. and J.G.-A. drafted the manuscript. J.K.Z. M.C.A.-S., V.C., B.R., C.S., A.R., J.E., G.F. and J.G.-A. provided study materials or performed experiments. J.K.Z., M.C.A.-S., V.C., A.R., B.R., C.S., J.E., G.F. and J.G.-A. critically revised the article for important intellectual content. All authors read and approved the final version of the article. G.F. and J.G.-A. are the guarantors of this work and, as such, had full access to all the data in the study and take responsibility for the integrity of the data and the accuracy of the data analysis.
Corresponding authors
Ethics declarations
Competing interests
The authors declare that they have no competing interests.
Ethics approval and consent to participate
The study was approved by the Universidad de Navarra’s Research Ethics Committee (2020.236).
Consent for publication
Not applicable.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Zapata, J.K., Azcona-Sanjulian, M.C., Catalán, V. et al. BMI-based obesity classification misses children and adolescents with raised cardiometabolic risk due to increased adiposity. Cardiovasc Diabetol 22, 240 (2023). https://doi.org/10.1186/s12933-023-01972-8
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12933-023-01972-8