Abstract
Background
High-sensitivity C-reactive protein (hs-CRP) elevation frequently occurs in acute myocardial infarction (AMI) and is associated with adverse outcomes. Since diabetes mellitus (DM) is characterized by an underlying chronic inflammation, hs-CRP may have a different prognostic power in AMI patients with and without DM.
Methods
We prospectively included 2064 AMI patients; hs-CRP was measured at hospital admission. Patients were grouped according to hs-CRP quartiles and DM status. The primary endpoint was a composite of in-hospital mortality, cardiogenic shock, and acute pulmonary edema. Two-year all-cause mortality was the secondary endpoint.
Results
Twenty-six percent (n = 548) of patients had DM and they had higher hs-CRP levels than non-DM patients (5.32 vs. 3.24 mg/L; P < 0.0001). The primary endpoint incidence in the overall population (7%, 9%, 13%, 22%; P for trend < 0.0001), in DM (14%, 9%, 21%, 27%; P = 0.0001), and non-DM (5%, 8%, 10%, 19%; P < 0.0001) patients increased in parallel with hs-CRP quartiles. The adjusted risk of the primary endpoint increased in parallel with hs-CRP quartiles in DM and non-DM patients but this relationship was less evident in DM patients. In the overall population, the adjusted OR of the primary endpoint associated with an hs-CRP value ≥ 2 mg/L was 2.10 (95% CI 1.46-3.00). For the same risk, hs-CRP was 7 and 2 mg/L in patients with and without DM. A similar behavior was observed for the secondary endpoint when the HR associated with an hs-CRP value ≥ 2 mg/L found in the overall population was 2.25 (95% CI 1.57-3.22). For the same risk, hs-CRP was 8 and 1.5 mg/L in DM and non-DM patients.
Conclusions
This study shows that hs-CRP predicts in-hospital outcome and two-year mortality in AMI patients with and without DM. However, in DM patients, the same risk of develo** events as in non-DM patients is associated to higher hs-CRP levels.
Similar content being viewed by others
Introduction
Type 2 diabetes mellitus (DM) is a common comorbidity in acute myocardial infarction (AMI), and it is associated with two-fold higher in-hospital and long-term mortality rates and with a higher risk of recurrent cardiovascular events [1,2,3]. Both DM and atherosclerosis are multifactorial conditions, which share a common inflammatory basis [4]. Indeed, on the one hand, DM is an independent risk factor for AMI and is considered a state of low-grade inflammation [5, 6]. On the other hand, inflammation plays a critical role in all phases of coronary athero-thrombosis, including plaque progression, rupture, and thrombosis leading to AMI [7].
C-reactive protein (CRP), an acute phase protein secreted by the liver, is the most widely used biomarker for detecting inflammatory conditions [8]. The elevation of CRP levels frequently occurs in AMI, and it has been associated with adverse outcomes, including higher risk of major adverse cardiac events, cardiovascular death, chronic kidney disease progression, acute kidney injury, and all-cause mortality [9,10,11,12,13]. To assess cardiovascular risk, physicians have now adopted high-sensitivity CRP (hs-CRP), instead of standard CRP assays that monitor infections and other inflammatory conditions [9]. In particular, in the AMI setting, hs-CRP demonstrated to be a more reliable indicator of outcome than CRP measured through traditional assays [11,12,13,14,15], showing that even a mild increase (≥ 2 mg/L) is of prognostic relevance [16].
Elevated hs-CRP levels in AMI patients may reflect a variable combination of chronic and acute (due to the ongoing cardiac event) inflammation. Since DM is more frequently associated with some degree of chronic inflammation, it is possible that, in AMI patients with DM, hs-CRP has a different prognostic relevance as compared to their non-DM counterpart.
The purpose of this study was to investigate the association between hs-CRP levels, measured at hospital admission, and in-hospital outcome and two-year mortality in a cohort of AMI patients according to DM status.
Materials and methods
Study population
This was a prospective, observational study. We enrolled all consecutive patients with AMI (n = 2178), both ST-elevation myocardial infarction (STEMI) and non-ST-elevation myocardial infarction (NSTEMI), admitted to the Intensive Cardiac Care Unit of Centro Cardiologico Monzino in Milan between June 1, 2012 and October 1, 2017. Patients experiencing AMI as a complication of elective percutaneous coronary intervention (PCI) (Type 4a AMI) and those with concomitant systemic inflammatory conditions, including active infections (n = 88) or malignancies (n = 26) were excluded. The study complied with the Declaration of Helsinki, and the Ethics Committee of our center approved the research protocol (n. R520-CCM549). Written informed consent was obtained from all participants.
Study protocol
Patients were considered as suffering from DM if one of the following conditions were present: personal history of DM reported in clinical record, treatment with glucose lowering drugs, or a glycated hemoglobin value ≥ 6.5% (48 mmol/mol). Glycated hemoglobin was measured at hospital admission in all patients as a part of our routine laboratory package using a method NGSP certified and standardized to the DCCT assay [17].
High-sensitivity-CRP was measured at hospital admission by Cobas® assay (particle-enhanced immunoturbidimetric assay) on Cobas c501 (Roche) [18]. A hs-CRP value ≥ 2 mg/L was considered a sign of inflammation [16].
Study patients received medical treatment and coronary revascularization based on the current standards of care recommended by published guidelines on AMI [19]. Demographical, clinical, biochemical data, and echocardiographic left ventricular ejection fraction (LVEF) were collected at hospital admission. After hospital discharge, all patients were followed-up for 2 years. Patient follow-up was mainly obtained through regularly scheduled outpatient visits or, in a minority of cases, by telephone calls performed by dedicated medical personnel.
The primary endpoint of the study was a composite of in-hospital mortality, cardiogenic shock, and acute pulmonary edema. Cardiogenic shock was defined as persistent systolic arterial pressure ≤ 80 mmHg and evidence of vital organ hypoperfusion caused by severe left ventricular dysfunction, right ventricular infarction, or mechanical complications of infarction, and not due to hypovolemia, hemorrhage, bradyarrhythmias, or tachyarrhythmias. Acute pulmonary edema was defined as respiratory distress, tachypnea, and orthopnea with rales over the lung fields and arterial oxygen saturation < 90%. To avoid interference, each patient could only account for one event classification. Two-year all-cause mortality was the secondary endpoint of the study.
Statistical analysis
A sample size of 2000 patients was calculated under the following assumptions: 10% overall incidence of the primary endpoint [1,2,3], and an expected odds ratio (OR) increasing by a 1.5 factor from the first to the fourth hs-CRP quartile in the overall population. This sample size allowed an 85% statistical power in assessing a significant difference (α error of 0.05) of the primary endpoint between the two quartiles. Moreover, this sample size allowed a 90% statistical power when an overall incidence of 20% of two-year all-cause mortality was considered [20],with an expected 20% higher mortality risk (hazard ratio [HR] 1.2) between the first and the fourth hs-CRP quartile.
Continuous variables are presented as mean ± SD. Variables with a skewed distribution are presented as median and interquartile ranges. Categorical data are presented as n (%). Trends across hs-CRP quartiles were assessed by ANCOVA and by Mantel–Haenszel Chi square, as appropriate. The association between hs-CRP and study endpoints was assessed by logistic regression analysis. Results are presented as OR with 95% confidence intervals (CI). Cox proportional hazard model was also used to assess HR and 95% CI for two-year mortality associated with hs-CRP quartiles. We calculated the P value for interaction between DM status and hs-CRP quartiles by logistic regression analysis and by Cox proportional hazard model, as appropriate. Pearson coefficient was used to assess the correlation between continuous variables. All analyses were performed in the overall study population as well as in DM and non-DM patients considered separately.
Kaplan–Meier analysis was used to generate time-to-event curves for two-year mortality in patients with hs-CRP < 2 mg/L or ≥ 2 mg/L. Log rank test was used to compare strata.
All analyses were adjusted according to an epidemiological model including the variables most closely associated with prognosis in AMI patients with and without DM [3]: LVEF ≤ 40%, estimated glomerular filtration rate (MDRD equation, based on age, gender, and serum creatinine concentration) ≤ 60 ml/min/1.73 m2, and AMI type (STEMI vs. NSTEMI). Moreover, we included in the model previous statin therapy due to its well-known anti-inflammatory effects [21].
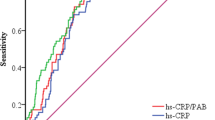
Receiver-operating characteristics (ROC) curves were constructed to assess the sensitivity and specificity throughout the concentrations of hs-CRP to predict both primary and secondary endpoints.
Cochran-Mantel–Haenszel estimator was implemented to calculate the adjusted relative risk (RR) of two-year mortality in patients with and without DM.
A bootstrap approach with 2000 resamples was implemented to assess that, in classifying primary and secondary endpoints, the estimated best cutoff of hs-CRP values was consistently higher in DM patients than in non-DM patients.
All tests were 2-tailed, and a P < 0.05 was required for statistical significance. All analyses were performed using SAS version 9.4 (SAS Institute, Cary, NC).
Results
Two-thousand-sixty-four AMI patients (mean age 67 ± 12 years, 1516 men, 1016 STEMI) were enrolled in the study. Of them, 548 (26%) had DM and 1366 (66%) had hs-CRP levels ≥ 2 mg/L. Inflammation (hs-CRP ≥ 2 mg/L) was more frequent in DM patients than in non-DM patients (74% vs. 64%; P < 0.0001). The baseline clinical characteristics and in-hospital outcomes of patients with and without DM and of those with hs-CRP ≥ and < 2 mg/L are shown in Tables 1 and 2, respectively. Patients with DM were older, more likely to have comorbidities, prior cardiovascular events and higher admission hs-CRP levels than those without DM, despite an almost two-fold higher rate of chronic statin therapy. Moreover, DM patients had a more complicated in-hospital clinical course. Similar differences in clinical characteristics and in-hospital outcomes were observed in patients with hs-CRP ≥ 2 mg/L when compared to those with hs-CRP < 2 mg/L. High-sensitivity-troponin I (hs-TnI) peak value was similar in DM and non-DM patients (43,153 ± 82,894 and 45,392 ± 99,242 ng/L, respectively; P = 0.64) and in patients with and without inflammation (46,427 ± 98,296 and 41,582 ± 89,099 ng/L, respectively; P = 0.28). In the entire population, a significant correlation between admission hs-CRP and hs-TnI peak value was found (r = 0.11; P < 0.0001). This relationship was stronger in non-DM patients (r = 0.12; P < 0.0001) than in DM patients (r = 0.07; P = 0.08).
The incidence of the primary and secondary endpoints in patients with and without DM and in those with hs-CRP ≥ and < 2 mg/L is reported in Fig. 1. Both DM and inflammation had a significantly higher adjusted risk of the two study endpoints.
Panel A: incidence of the in-hospital combined clinical endpoint (death, cardiogenic shock, and acute pulmonary edema) in patients with and without diabetes mellitus (DM) and adjusted odds ratio (OR) and 95% confidence interval (CI) associated with DM. Panel B: Kaplan–Meier survival curves stratified by DM status and adjusted hazard ratio (HR) and 95% CI associated with DM. Panel C: incidence of the in-hospital combined clinical endpoint (death, cardiogenic shock, and acute pulmonary edema) in patients with high-sensitivity C-reactive protein (hs-CRP) ≥ and < 2 mg/L and adjusted OR and 95% CI associated with a hs-CRP value ≥ 2 mg/L. Panel D: Kaplan–Meier survival curves stratified by hs-CRP cut-off value (2 mg/L) and adjusted HR and 95% CI associated with a hs-CRP value ≥ 2 mg/L. All analyses were adjusted for left ventricular ejection fraction (≤ or > 40%), estimated glomerular filtration rate (≤ or > 60 ml/min/1.73 m2), type of acute myocardial infarction (STEMI vs. NSTEMI) and prior statin use
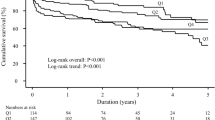
The incidence of the two study endpoints according to hs-CRP quartiles in the overall population, in DM and non-DM patients is shown in Table 3. In the entire study population, the adjusted risk of the primary endpoint increased in parallel with hs-CRP quartiles (Fig. 2; Panel A). However, this trend was more evident in non-DM patients (Fig. 2; Panel B) than in DM patients (Fig. 2; Panel C). A similar behavior was found when two-year mortality was considered (Fig. 3). In line with this result, a significant interaction between DM status and hs-CRP was found for the secondary endpoint (P = 0.02).
Adjusted odds ratios (OR) and 95% confidence intervals for the primary endpoint according to high-sensitivity C-reactive protein (hs-CRP) level quartiles in the overall study population (Panel A), in patients with diabetes mellitus (DM) (Panel B), and in those without DM (Panel C). Odd ratios and P for trend were adjusted for left ventricular ejection fraction (≤ or > 40%), estimated glomerular filtration rate (≤ or > 60 ml/min/1.73 m2), type of acute myocardial infarction (STEMI vs. NSTEMI), and prior statin use. P for interaction between DM status and hs-CRP = 0.36
Adjusted hazard ratios (HR) and 95% confidence intervals for the secondary endpoint according to high-sensitivity C-reactive protein (hs-CRP) level quartiles in the overall study population (Panel A), in patients with diabetes mellitus (DM) (Panel B), and in those without DM (Panel C). Hazard ratios and P for trend were adjusted for left ventricular ejection fraction (≤ or > 40%), estimated glomerular filtration rate (≤ or > 60 ml/min/1.73 m2), type of acute myocardial infarction (STEMI vs. NSTEMI), and prior statin use. P for interaction between DM status and hs-CRP = 0.02
The AUCs for hs-CRP in predicting the primary and secondary endpoints in the entire population were 0.66 (95% CI 0.63–0.70) and 0.66 (95% CI 0.62–0.70), respectively. Again, they were higher in non-DM patients (0.66 [95% CI 0.61–0.70] and 0.67 [95% CI 0.61–0.72]) than in DM patients (0.63 [95% CI 0.58–0.68] and 0.61 [95% CI 0.54–0.67]).
The adjusted OR and HR of the primary and secondary endpoint, respectively, associated with an hs-CRP value ≥ 2 mg/L found in the overall population (Fig. 1) corresponded to higher hs-CRP threshold values in patients with DM than in those without DM (Fig. 4). In parallel, at bootstrap analysis, the hs-CRP cutoff values associated with the primary and secondary endpoint risk in DM patients were higher than those of non-DM patients in 74% and 96% of cases, respectively. When computing adjusted RR of two-year mortality in patients with and without DM, its value increased in both groups in parallel with increasing hs-CRP value. However, RR was consistently higher in non-DM patients for any considered hs-CRP level (Fig. 5).
Threshold values of high-sensitivity C-reactive protein (hs-CRP) in patients with and without diabetes mellitus (DM) considered separately, corresponding to the adjusted risk of the primary and secondary endpoints associated with an hs-CRP value ≥ 2 mg/L found in the overall population. OR Odds ratio, HR Hazard ratio, CI Confidence interval
Relative risks and 95% confidence interval (CI) of two-year mortality associated with different high-sensitivity C-reactive protein (hs-CRP) cut-offs in patients with diabetes mellitus (DM) (blue) and in those without DM (red). Relative risk was adjusted for left ventricular ejection fraction (≤ or > 40%), estimated glomerular filtration rate (≤ or > 60 ml/min/1.73 m2), type of acute myocardial infarction (STEMI vs. NSTEMI) and and prior statin use. The vertical dotted line refers to hs-CRP value of 2 mg/L. The horizontal dotted line refers to the RR associated with hs-CRP value of 2 mg/L in non-DM patients
Discussion
This study supports previous evidence showing that hs-CRP measured at hospital admission in AMI patients is a predictor of in-hospital outcome and long-term mortality. This seems to be true for both DM and non-DM patients. However, we demonstrated that the relationship between the outcomes considered in our study and hs-CRP levels is downshifted in DM patients, who show for each hs-CRP value a lower risk than that of non-DM patients. In other words, in DM patients, the hs-CRP values associated to each event risk were higher than those of non-DM patients.
Inflammation and DM in AMI
The involvement of inflammation in atherosclerosis and, consequently, in AMI is well established [4,5,6,7], as well as the prognostic usefulness of biomarker surrogates, such as hs-CRP, for predicting the risk of mortality and recurrent events [11,12,13,14,15,16, 22]. Moreover, observational and randomized studies indicated that cardiovascular benefits are more apparent when systemic inflammation is reduced [23, 24]. In particular, the Aggrastat-to-Zocor (A to Z) trial demonstrated that the clinical outcome of patients with acute coronary syndromes significantly improves when the hs-CRP levels are lowered below 2 mg/L [16]. Diabetes mellitus is a multifactorial metabolic disease and growing evidence shows that it is characterized by a state of sub-clinical inflammation [5], as reflected by chronic high levels of hs-CRP [6]. In AMI, patients with DM show a more severe inflammatory condition than those without DM [25], and this may, at least in part, explain their higher short-term and long-term mortality risk [26, 27]. However, whether hs-CRP during AMI carries a different prognostic relevance in DM and non-DM patients is still a controversial issue. Indeed, on the one hand, previous studies showed that CRP is an independent predictor of mortality after AMI in both DM and non-DM patients [28, 29]. On the other hand, Meisinger et al. [28] found no association between CRP and long-term mortality (median 4 years) after AMI in DM patients. However, these studies were retrospective analyses of registries including old study populations (enrolled between 1998 and 2004), they considered patients with an outdated DM definition [28, 29], and, in one study [29], traditional CRP was assessed. More recently, ** events as in non-DM patients is associated to higher hs-CRP levels.
Availability of data and materials
The datasets generated and/or analyzed during the current study are not publicly available, as per internal protocol, but are available from the corresponding author on reasonable request.
Abbreviations
- AMI:
-
Acute myocardial infarction
- CAD:
-
Coronary artery disease
- CI:
-
Confidence intervals
- CRP:
-
C-reactive protein
- DM:
-
Diabetes mellitus
- OR:
-
Odds ratio
- hs-CRP:
-
High-sensitivity-C-reactive protein
- HR:
-
Hazard ratio
- LVEF:
-
Left ventricular ejection fraction
- NSTEMI:
-
non-ST-elevation myocardial infarction
- PCI:
-
Percutaneous coronary intervention
- ROC:
-
Receiver-operating characteristics
- RR:
-
Relative risk
- STEMI:
-
ST-elevation myocardial infarction
References
Brener SJ, Mehran R, Dressler O, Cristea E, Stone GW. Diabetes mellitus, myocardial reperfusion, and outcome in patients with acute ST-elevation myocardial infarction treated with primary angioplasty (from HORIZONS AMI). Am J Cardiol. 2012;109:1111–6.
Malmberg K, Yusuf S, Gerstein HC, Brown J, Zhao F, Hunt D, Piegas L, Calvin J, Keltai M, Budaj A. Impact of diabetes on long-term prognosis in patients with unstable angina and non-Q-wave myocardial infarction: results of the OASIS (Organization to Assess Strategies for Ischemic Syndromes) Registry. Circulation. 2000;102:1014–9.
Marenzi G, Cosentino N, Genovese S, Campodonico J, De Metrio M, Rondinelli M, Cornara S, Somaschini A, Camporotondo R, Demarchi A, Milazzo V, Moltrasio M, Rubino M, Marana I, Grazi M, Lauri G, Bonomi A, Veglia F, De Ferrari GM, Bartorelli AL. Reduced cardio-renal function accounts for most of the in-hospital morbidity and mortality risk among patients with type 2 diabetes undergoing primary percutaneous coronary intervention for ST-segment elevation myocardial infarction. Diab Care. 2019;42:1305–11.
Pradhan AD, Ridker PM. Do atherosclerosis and type 2 diabetes share a common inflammatory basis? Eur Heart J. 2002;23:831–4.
Pitsavos C, Tampourlou M, Panagiotakos DB, Skoumas Y, Chrysohoou C, Nomikos T, Stefanadis C. Association between low-grade systemic inflammation and type 2 diabetes mellitus among men and women from the ATTICA Study. Rev Diabet Stud. 2007;4:98–104.
Odegaard AO, Jacobs DR Jr, Sanchez OA, Goff DC Jr, Reiner AP, Gross MD. Oxidative stress, inflammation, endothelial dysfunction and incidence of type 2 diabetes. Cardiovasc Diabetol. 2016;15:51.
Libby P, Ridker PM, Maseri A. Inflammation and atherosclerosis. Circulation. 2002;105:1135–43.
Vigushin DM, Pepys MB, Hawkins PN. Metabolic and scintigraphic studies of radioiodinated human C-reactive protein in health and disease. J Clin Invest. 1993;91:1351–7.
Crea F, Libby P. Acute coronary syndromes: the way forward from mechanisms to precision treatment. Circulation. 2017;136:1155–66.
Yousuf O, Mohanty BD, Martin SS, Joshi PH, Blaha MJ, Nasir K, Blumenthal RS, Budoff MJ. High-sensitivity C-reactive protein and cardiovascular disease: a resolute belief or an elusive link? J Am Coll Cardiol. 2013;62:397–408.
Pai JK, Pischon T, Ma J, Manson JE, Hankinson SE, Joshipura K, Curhan GC, Rifai N, Cannuscio CC, Stampfer MJ, Rimm EB. Inflammatory markers and the risk of coronary heart disease in men and women. N Engl J Med. 2004;351:2599–610.
Fu EL, Franko MA, Obergfell A, Dekker FW, Gabrielsen A, Jernberg T, Carrero JJ. High-sensitivity C-reactive protein and the risk of chronic kidney disease progression or acute kidney injury in post-myocardial infarction patients. Am Heart J. 2019;216:20–9.
Cosentino N, Genovese S, Campodonico J, Bonomi A, Lucci C, Milazzo V, Moltrasio M, Biondi ML, Riggio D, Veglia F, Ceriani R, Celentano K, De Metrio M, Rubino M, Bartorelli AL, Marenzi G. High-sensitivity C-reactive protein and acute kidney injury in patients with acute myocardial infarction: a prospective observational study. J Clin Med. 2019;8:2192.
Zebrack JS, Anderson JL, Maycock CA, Horne BD, Bair TL, Muhlestein JB, Intermountain Heart Collaborative (IHC) Study Group. Usefulness of high-sensitivity C-reactive protein in predicting long-term risk of death or acute myocardial infarction in patients with unstable or stable angina pectoris or acute myocardial infarction. Am J Cardiol. 2002;89:145–9.
Mani P, Puri R, Schwartz GG, Nissen SE, Shao M, Kastelein JJP, Menon V, Lincoff AM, Nicholls SJ. Association of initial and serial C-reactive protein levels with adverse cardiovascular events and death after acute coronary syndrome: a secondary analysis of the VISTA-16 trial. JAMA Cardiol. 2019;4:314–20.
Wiviott SD, de Lemos JA, Cannon CP, Blazing M, Murphy SA, McCabe CH, Califf R, Braunwald E. A tale of two trials: a comparison of the post-acute coronary syndrome lipid-lowering trials A to Z and PROVE IT-TIMI 22. Circulation. 2006;113:1406–14.
American Diabetes Association. 2. Classification and Diagnosis of Diabetes: Standards of Medical Care in Diabetes-2020. Diabetes Care. 2020. 43 (Suppl 1):S14-S31.
Podmore C, Meidtner K, Schulze MB, Scott RA, Ramond A, Butterworth AS, Di Angelantonio E, Danesh J, Arriola L, Barricarte A, Boeing H, Clavel-Chapelon F, Cross AJ, Dahm CC, Fagherazzi G, Franks PW, Gavrila D, Grioni S, Gunter MJ, Gusto G, Jakszyn P, Katzke V, Key TJ, Kühn T, Mattiello A, Nilsson PM, Olsen A, Overvad K, Palli D, Quirós JR, Rolandsson O, Sacerdote C, Sánchez-Cantalejo E, Slimani N, Sluijs I, Spijkerman AM, Tjonneland A, Tumino R, van der A DL, van der Schouw YT, Feskens EJ, Forouhi NG, Sharp SJ, Riboli E, Langenberg C, Wareham NJ. The association of multiple biomarkers of iron metabolism and type 2 diabetes—the EPIC-InterAct Study. Diabetes Care. 2016. 39:572-581.
Neumann FJ, Sousa-Uva M, Ahlsson A, Alfonso F, Banning AP, Benedetto U, Byrne RA, Collet JP, Falk V, Head SJ, Jüni P, Kastrati A, Koller A, Kristensen SD, Niebauer J, Richter DJ, Seferovic PM, Sibbing D, Stefanini GG, Windecker S, Yadav R, Zembala MO, ESC Scientific Document Group. ESC/EACTS Guidelines on myocardial revascularization. Eur Heart J. 2018;2019(40):87–165.
Lehto M, Snapinn S, Dickstein K, Swedberg K, Nieminen MS, OPTIMAAL investigators. Prognostic risk of atrial fibrillation in acute myocardial infarction complicated by left ventricular dysfunction: the OPTIMAAL experience. Eur Heart J. 2005;26:350–6.
Diamantis E, Kyriakos G, Quiles-Sanchez LV, Farmaki P, Troupis T. The anti-inflammatory effects of statins on coronary artery disease: an updated review of the literature. Curr Cardiol Rev. 2017;13:209–16.
Suleiman M, Khatib R, Agmon Y, Mahamid R, Boulos M, Kapeliovich M, Levy Y, Beyar R, Markiewicz W, Hammerman H, Aronson D. Early inflammation and risk of long-term development of heart failure and mortality in survivors of acute myocardial infarction predictive role of C-reactive protein. J Am Coll Cardiol. 2006;47:962–8.
Ridker PM, Everett BM, Thuren T, MacFadyen JG, Chang WH, Ballantyne C, Fonseca F, Nicolau J, Koenig W, Anker SD, Kastelein JJP, Cornel JH, Pais P, Pella D, Genest J, Cifkova R, Lorenzatti A, Forster T, Kobalava Z, Vida-Simiti L, Flather M, Shimokawa H, Ogawa H, Dellborg M, Rossi PRF, Troquay RPT, Libby P, Glynn RJ; CANTOS Trial Group. Antiinflammatory therapy with canakinumab for atherosclerotic disease. N Engl J Med. 2017. 377:1119-1131.
Ridker PM, Everett BM, Thuren T, MacFadyen JG, Chang WH, Ballantyne C, Fonseca F, Nicolau J, Koenig W, Anker SD, Kastelein JJP, Cornel JH, Pais P, Pella D, Genest J, Cifkova R, Lorenzatti A, Forster T, Kobalava Z, Vida-Simiti L, Flather M, Shimokawa H, Ogawa H, Dellborg M, Rossi PRF, Troquay RPT, Libby P, Glynn RJ; CANTOS Trial Group. Relationship of C-reactive protein reduction to cardiovascular event reduction following treatment with canakinumab: a secondary analysis from the CANTOS randomized controlled trial. Lancet. 2018. 391:319-328.
Martín-Timón I, Sevillano-Collantes C, Segura-Galindo A, Del Cañizo-Gómez FJ. Type 2 diabetes and cardiovascular disease: have all risk factors the same strength? World J Diab. 2014;5:444–70.
Marenzi G, Cosentino N, Milazzo V, De Metrio M, Cecere M, Mosca S, Rubino M, Campodonico J, Moltrasio M, Marana I, Grazi M, Lauri G, Bonomi A, Veglia F, Manfrini R, Bartorelli AL. Prognostic value of the acute-to-chronic glycemic ratio at admission in acute myocardial infarction: a prospective study. Diab Care. 2018;41:847–53.
Milazzo V, Cosentino N, Genovese S, Campodonico J, Mazza M, De Metrio M, Marenzi G. Diabetes mellitus and acute myocardial infarction: impact on short and long-term mortality. Adv Exp Med Biol. 2020.
MONICA/KORA Myocardial Infarction Registry, Meisinger C, Heier M, von Scheidt W, Kuch B. Admission C reactive protein and short- as well as long-term mortality in diabetic versus nondiabetic patients with incident myocardial infarction. Clin Res Cardiol. 2010. 99:817-823.
Otter W, Winter M, Doering W, Standl E, Schnell O. C-reactive protein in diabetic and nondiabetic patients with acute myocardial infarction. Diabetes Care. 2007;30:3080–2.
**a M, Zhang C, Gu J, et al. Impact of C-reactive protein on long-term mortality in acute myocardial infarction patients with diabetes and those without. Clin Chim Acta. 2018;480:220–4.
Rudiger A, Singer M. The heart in sepsis: from basic mechanisms to clinical management. Curr Vasc Pharmacol. 2013;11:187–95.
Takasu O, Gaut JP, Watanabe E, To K, Fagley RE, Sato B, Jarman S, Efimov IR, Janks DL, Srivastava A, Bhayani SB, Drewry A, Swanson PE, Hotchkiss RS. Mechanisms of cardiac and renal dysfunction in patients dying of sepsis. Am J Respir Crit Care Med. 2013;187:509–17.
Walley KR. Sepsis-induced myocardial dysfunction. Curr Opin Crit Care. 2018;24:292–9.
Niccoli G, Lanza GA, Spaziani C, Altamura L, Romagnoli E, Leone AM, Fusco B, Trani C, Burzotta F, Mazzari MA, Mongiardo R, Biasucci LM, Rebuzzi AG, Crea F. Baseline systemic inflammatory status and no-reflow phenomenon after percutaneous coronary angioplasty for acute myocardial infarction. Int J Cardiol. 2007;117:306–11.
Ries W, Heigl F, Garlichs C, Sheriff A, Torzewski J. Selective C-Reactive Protein-Apheresis in Patients. Ther Apher Dial. 2019.
Sheriff A, Schindler R, Vogt B, Abdel-Aty H, Unger JK, Bock C, Gebauer F, Slagman A, Jerichow T, Mans D, Yapici G, Janelt G, Schröder M, Kunze R, Möckel M. Selective apheresis of C reactive protein: a new therapeutic option in myocardial infarction? J Clin Apher. 2015;30:15–21.
Kang DO, Park Y, Seo JH, Jeong MH, Chae SC, Ahn TH, Jang WY, Kim W, Park EJ, Choi BG, Na JO, Choi CU, Kim EJ, Rha SW, Park CG, Seo HS, KAMIR-NIH Registry Investigators. Time-dependent prognostic effect of high sensitivity C-reactive protein with statin therapy in acute myocardial infarction. J Cardiol. 2019;74:74–83.
Winzap P, Davies A, Klingenberg R, Obeid S, Roffi M, Mach F, Räber L, Windecker S, Templin C, Nietlispach F, Nanchen D, Gencer B, Muller O, Matter CM, von Eckardstein A, Lüscher TF. Diabetes and baseline glucose are associated with inflammation, left ventricular function and short- and long-term outcome in acute coronary syndromes: role of the novel biomarker Cyr 61. Cardiovasc Diab. 2019;18:142.
Karabağ Y, Çağdaş M, Rencuzogullari I, Karakoyun S, Artaç İ, İliş D, Yesin M, Çiftçi H, Erdoğdu HI, Tanboğa IH. The C-reactive protein to albumin ratio predicts acute kidney injury in patients with ST-segment elevation myocardial infarction undergoing primary percutaneous coronary intervention. Heart Lung Circ. 2019;28:1638–45.
Ammirati E, Cannistraci CV, Cristell NA, Vecchio V, Palini AG, Tornvall P, Paganoni AM, Miendlarzewska EA, Sangalli LM, Monello A, Pernow J, Björnstedt Bennermo M, Marenzi G, Hu D, Uren NG, Cianflone D, Ravasi T, Manfredi AA, Maseri A. Identification and predictive value of interleukin-6 + interleukin-10 + and interleukin-6- interleukin-10 + cytokine patterns in ST-elevation acute myocardial infarction. Circ Res. 2012;111:1336–48.
Cristell N, Cianflone D, Durante A, Ammirati E, Vanuzzo D, Banfi M, Calori G, Latib A, Crea F, Marenzi G, De Metrio M, Moretti L, Li H, Uren NG, Hu D, Maseri A; FAMI Study Investigators. High-sensitivity C-reactive protein is within normal levels at the very onset of first ST-segment elevation acute myocardial infarction in 41% of cases: a multiethnic case-control study. J Am Coll Cardiol. 2011. 58:2654-2661.
Cho DH, Joo HJ, Kim MN, Lim DS, Shim WJ, Park SM. Association between epicardial adipose tissue, high-sensitivity C-reactive protein and myocardial dysfunction in middle-aged men with suspected metabolic syndrome. Cardiovasc Diab. 2018;17:95.
Zhang L, Xu C, Liu J, Bai X, Li R, Wang L, Zhou J, Wu Y, Yuan Z. Baseline plasma fibrinogen is associated with haemoglobin A1c and 2-year major adverse cardiovascular events following percutaneous coronary intervention in patients with acute coronary syndrome: a single-centre, prospective cohort study. Cardiovasc Diabetol. 2019;18:52.
Acknowledgements
Not applicable.
Funding
This work was supported by the Centro Cardiologico Monzino, IRCCS, Milan, Italy. The study’s sponsor had no role in the design and conduct of the study, in the collection, analysis, and interpretation of the data, or in the preparation, review, or approval of the manuscript.
Author information
Authors and Affiliations
Contributions
GM, CL and ALB had full access to all of the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis. Study concept and design: CL, NC, GM, ALB. Acquisition of data: SG, JC, VM, MM, MR, DR, MLB, MR, KC. Analysis and interpretation of data: GM, NC, JC, ALB. Drafting the manuscript: CL, GM, NC. Critical revision of the manuscript for important intellectual content: PA, SG, ALB. Statistical analysis: AB, NC, FV. Administrative, technical, or material support: GM. Study supervision: GM, PA, ALB. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
the Ethics Committee (n. R520-CCM549) approved the study as a prospective cohort study.
Consent for publication
not applicable.
Competing interests
none.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Lucci, C., Cosentino, N., Genovese, S. et al. Prognostic impact of admission high-sensitivity C-reactive protein in acute myocardial infarction patients with and without diabetes mellitus. Cardiovasc Diabetol 19, 183 (2020). https://doi.org/10.1186/s12933-020-01157-7
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12933-020-01157-7