Abstract
Background
Medication errors (MEs) are harmful to patients during hospitalization, especially elderly patients. To reduce MEs, an integrated medication management (IMM) model was developed in a 2500-bed medical center, allowing a clinical pharmacist to participate in the daily ward round and perform medication reconciliation and medication reviews. This study aimed to evaluate the impact of the IMM model on MEs and medication utilization using a quasi-experimental design.
Methods
We conducted an interrupted time-series study using the aggregated data of monthly admissions from two wards of a medical center, where one ward served as the intervention and the other served as the external control. The pre- and post-intervention phases comprised of 40 and 12 monthly observational units, respectively. The primary outcome was the mean number of ME reports, which were further investigated for different ME types. The mean number of daily inpatient prescriptions, mean number of daily self-prepared medications, and median daily medication costs were measured. All outcomes were measured per admission episode. Segmented regression was used to evaluate the level and slope changes in the outcomes after IMM model implementation, and subgroup analyses were performed to examine the effects on different groups.
Results
After IMM model implementation, the mean number of ME reports increased (level change: 1.02, 95% confidence interval [CI]: 0.68 to 1.35, P < 0.001). The number of reports has shown a dramatic increase in omissions or medication discrepancies, inappropriate drug choices, and inappropriate routes or formulations. Furthermore, the mean number of daily inpatient prescriptions was reduced for patients aged ≥75 years (level change: −1.78, 95% CI: −3.06 to −0.50, P = 0.009). No significant level or slope change was observed in the control ward during the post-intervention phase.
Conclusions
The IMM model improved patient safety and optimized medication utilization by increasing the reporting of MEs and decreasing the number of medications used.
Similar content being viewed by others
Background
A medication error (ME) is defined as “a failure in the treatment process that leads to, or has the potential to lead to, harm to the patient” and is usually preventable [1]. During hospitalization, approximately 6% of patients have experienced MEs; some of these MEs have been observed to turn into adverse drug events and result in a prolonged length of stay (LOS) or even death [2]. The elderly are especially at a high risk for ME because they often have multiple morbidities and are already on multiple medications [3, 4]. Moreover, a systematic review published in 2017 revealed that MEs might increase the economic burden, with the cost of an ME during hospitalization ranging from EUR 17.6 to EUR 6432.16 [5]. As MEs are common in practice and potentially harmful to patients, the reduction of MEs has become a challenge for the healthcare system.
MEs can occur during any part of the drug therapy process, including prescription, transcription, dispensation, or administration [1]. Numerous clinical pharmaceutical services (CPS) have been developed to prevent these errors. According to previous studies, CPS not only reduces MEs, but also decreases the medication costs, prevents adverse drug events, and improves other quality indicators [6,7,8]. However, many of these studies have been conducted under highly controlled conditions. Additionally, the efficacy of CPS may be influenced by several factors, such as labor and workflow. Therefore, the results of previous studies cannot sufficiently reflect the effectiveness of CPS in real-world settings.
To reduce MEs and improve the quality of care, we propose an integrated CPS model called the National Taiwan University Hospital Integrated Medication Management (NTUH-IMM) model. This study aimed to evaluate the effectiveness of the NTUH-IMM model on MEs and medication utilization in routine clinical practice using a quasi-experimental design.
Methods
Study design and settings
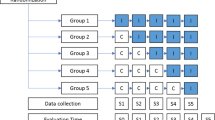
To evaluate the effectiveness of the NTUH-IMM model in a real-world setting, we applied an interrupted time series (ITS) design. The ITS design is a quasi-experimental method used to examine the differences in the outcomes between different periods (time series) using longitudinal data [9].
This study was conducted in the Division of Multidisciplinary Medicine (DMM) of the NTUH, a 2500-bed medical center in Taiwan. There were two wards in the DMM with similar settings, making them suitable for conducting a quasi-experimental study. We implemented the NTUH-IMM model in one of the DMM wards (i.e., the intervention ward) in July 2018 and considered the other as the control ward. As an ITS is usually conducted on a single group, it could avoid issues due to unequal distribution between groups, such as between-group selection bias or unmeasured confounders. However, history, defined as an independent concurrent event with the intervention that potentially influences the outcomes, has been considered as the major threat to any ITS design. Therefore, we introduced an external control group as a counterfactual to address this issue [10].
The two wards, with 36 and 35 beds, respectively, were on the same floor. Five attending physicians, 12 nurse practitioners, 18 nurses, and one central pharmacy pharmacist were allocated to each ward. The staff were rotated between the two study wards during the pre-intervention period, but not the post-intervention period. As usual care was implemented in both study wards before the intervention; therefore, staff rotation should not have affected the pre-intervention estimates.
The patients admitted to the DMM were mainly transferred from the emergency department and presented with acute illnesses. Over 60% of these patients were at least 65 years old, with poor functional status (Barthel’s score, mean and standard deviation: 61 ± 35) and high comorbidity (Charlson score, mean and standard deviation: 3.7 ± 3.4) [11]. The transfer to the DMM was decided by managers who were blind to and independent of this study. No randomization was performed.
Since elderly individuals were more vulnerable to MEs, we chose the DMM wards, with the majority of patients being at least 65 years of age, to implement the intervention and conduct the study. Due to the fact that we also intended to promote the NTUH-IMM model to other wards at the NTUH, the elements of the NTUH-IMM model were not specifically designed for the elderly.
The study period included a 40-month pre-intervention phase (phase 1: January 1, 2015 to April 30, 2018) and a 12-month post-intervention phase (phase 2: July 1, 2018 to June 30, 2019). The crossover period was from May 1, 2018 to June 30, 2018. The patients could have been exposed to the usual care and the new intervention during this period; thus, we did not consider admissions during the crossover period.
Data sources
We used the NTUH Integrated Medical Database (NTUH-iMD) and NTUH Pharmaceutical Service Record Database (NTUH-PSRD) as the data sources. Both databases contained data generated at the NTUH and only de-identified information was available to the researchers. The NTUH-iMD included records from outpatient and inpatient visits at the NTUH, including demographics, diagnosis, laboratory data, and medication records.
The NTUH-PSRD provides records of ME reports from the internal reporting system at the NTUH. All the pharmacists at NTUH voluntarily reported MEs to the reporting system when they detected MEs and made suggestions. The number of ME reports is one of the references used for performance evaluation. Moreover, ME reports should be verified by an independent clinical pharmacist after they have been documented. The content of each ME report included the types of ME, rationale for being regarded as an error, recommendation to correct the error, and whether the recommendation was accepted or not by the prescriber.
Although MEs can occur in any phase of medication use, such as prescription, dispensation, and administration, only the MEs related to prescriptions can be reported to the NTUH reporting system with fixed types. The ME types and their definitions are presented in Table A1. For example, when a pharmacist found that a medication was provided at an incorrect concentration that was different from the prescription, the pharmacist was not able to report this error because it was not a prescription error.
Interventions
The NTUH-IMM model was developed to reduce the MEs occurring in patients and optimize medication utilization. It was based on the integrated medication management services developed by Scullin et al. [12], with some modifications. The ‘integrated’ part of the NTUH-IMM model was extended in two aspects: (1) integration of a clinical pharmacist, who was not included in the DMM wards, to participate in the activities of the medical team and (2) coherent integration of the process of medication reconciliation and medication review.
Implementation preparation
Before the implementation of the NTUH-IMM model in the intervention ward, the clinical pharmacist had to receive a 6-month interdisciplinary-collaboration training, which contained an internship with other experienced clinical pharmacists in different wards. In addition, an explanation session aimed at informing other healthcare professionals about the change and potential benefits held in the intervention ward to facilitate the implementation of the NTUH-IMM model. The standard processes of the NTUH-IMM model were co-developed with the clinical pharmacist and central pharmacy pharmacist, who would execute these interventions.
The details of the NTUH-IMM model are described below, and a comparison between the NTUH-IMM model and usual care is presented in Table 1.
Medication reconciliation during admission
When a patient was admitted to the intervention ward, a central pharmacy pharmacist interviewed the patient or the caregiver within 3 days to collect the medication history and information on allergies, difficulty in taking medication, adherence, and supplement/herb/non-prescription drug use. The medication history was further verified with data from the PharmaCloud system, a cloud-based inquiry system maintained by the National Health Insurance (NHI) Administration in Taiwan since 2013, which provided the prescription drug records of patients over the past 3 months [13]. All the information mentioned above was documented as the best possible medication history (BPMH) in the electronic medical record (EMR) system at the NTUH and could be accessed by all healthcare providers of the patient.
Moreover, the central pharmacy pharmacist compared the admission medication list with the BPMH to identify whether a medication discrepancy existed. If so, the central pharmacy pharmacist would inform and discuss it with the clinical pharmacist, who would further reconcile it according to the patient’s condition.
Medication review during hospitalization
During the hospital stay of the patient, the clinical pharmacist performed a medication review to optimize the medication regimen of the patient periodically. Several aspects were considered, such as the patient demographics, medication history, treatment response, therapeutic goal, laboratory values, and patient preference. Additionally, the clinical pharmacist surveyed drug-drug interactions, drug-food interactions, contraindications, and the potential causes of adverse events in the medication regimen of the patient.
To gather information and provide timely recommendations, the clinical pharmacist participated in daily ward rounds with the medical team, observed the patient directly, and exchanged opinions with other healthcare professionals. When the patient’s regimen required modification, the clinical pharmacist could discuss it with the medical team and make decisions collaboratively. After the ward round, the clinical pharmacist stayed at the nursing station to provide medication consultation services to other healthcare professionals.
Study sample
Admissions to the two DMM wards during the study period were included if they met the following criteria: (1) the age of the patient was a minimum of 20 years at admission, (2) direct transfer from the emergency department, (3) LOS of at least 2 days, and (4) at least 180 days apart for two consecutive admissions to the study wards. There were no specific exclusion criteria. All the patients admitted during the study period participated in this study; thus, no specific sampling technique was implemented.
Measures
We retrieved the demographic variables and primary diagnoses of the patients at admission from the NTUH-iMD; additionally, these data were used to represent the baseline characteristics. For the ITS design, we aggregated the data from patients admitted to the study wards in each calendar month into an observational unit. For instance, if a patient was admitted on May 30, 2018 and discharged on June 10, 2018, the data were placed into an observational unit representing May 2018. The outcome variables were measured for each admission episode.
The primary outcome was the mean number of ME reports as the NTUH-IMM model was developed to reduce the MEs in patients. Since a higher number of MEs reported by pharmacists meant that more MEs were detected and corrected, we assumed that the elevation of the mean number of ME reports indicated a reduction in MEs occurring to the patients. To ensure the validity of the reports, only when the recommendation in the ME reports was accepted by the prescribers would the reports be adopted for this study. We further investigate the effects of the NTUH-IMM model on different types of ME reports. The definitions of each ME type are listed in Table A1. The mean numbers of each type of ME report during phases 1 and 2 were measured, and the post-pre ratio was calculated by dividing the number of reports in phase 2 by those in phase 1.
To further understand the effectiveness of NTUH-IMM on medication use during hospitalization, the following outcome variables were also included: the mean number of daily inpatient prescriptions (IPs), mean number of daily self-prepared medications (SPMs), and median daily medication cost. The medication cost was converted from NTD to USD, according to the exchange rate on June 28, 2019 (NTD: USD = 1:0.033). These outcome variables were selected and evaluated because it was assumed that the NTUH-IMM model would decrease the number of unnecessary medications and could further reduce the medication costs of the patients during hospitalization.
The definitions of the outcome variables are presented in Table A2.
Statistical analysis
Descriptive statistics and chi-square tests were used to describe the baseline characteristics. We used a segmented regression analysis to examine the level or slope changes in the outcome variables between phases 1 and 2. The linear regression model was expressed as follows: Yt = b0 + b1*Tt + b2*Xt + b3*XTt. Here, Yt is the outcome value at time t and Tt is a continuous variable that indicates the time series at time t. Notably, Xt is a dummy variable indicating the implementation of the NTUH-IMM model at time t, and XTt is a continuous variable that denotes the time series after the NTUH-IMM implementation at time t (XTt = 0 before the NTUH-IMM implementation). The estimation of b1 refers to the trend of the outcome value without any intervention effect, the estimation of b2 refers to the intervention effect on the level of outcome value immediately after the intervention implementation, and the estimation of b3 refers to the intervention effect on the trend of outcome value after the intervention implementation.
We used an autoregressive error model to adjust the autocorrelation of the regression model. Segmented regression analyses were applied to both the intervention and control wards. The outcome changes in the intervention ward were interpreted as the effects of the NTUH-IMM model, whereas those in the control ward were interpreted as counterfactuals. All the analyses were conducted using SAS version 9.4, and the significance threshold was set to a P-value< 0.05.
We also conducted a sensitivity analysis by shortening the data collection interval to half a month, as the power of the ITS depends on the number of observational units. Furthermore, we conducted several subgroup analyses to evaluate the potential effect modification by including patients with different characteristics. First, we restricted the admissions to late-elderly patients (aged 75+ years) to determine whether the effects of the NTUH-IMM model were modified by age. Second, we focused on admissions without prolonged LOS (≥ 30 days). Extant studies have revealed that the LOS highly depends on the destination of post-discharge care, and delayed discharge might be due to a lack of patient resources to facilitate discharge [14, 15]. Therefore, medication for admission with prolonged LOS might be stabilized after the acute problem is solved, and the effects of the NTUH-IMM model might be modified by prolonged LOS. Third, we removed the admissions of patients who died or were transferred to the intensive care unit (ICU), as these patients likely had poor prognoses and would not benefit from the intervention.
Results
A total of 5610 admissions were included in the analysis, with 2816 admissions in the intervention ward and 2794 in the control ward. The baseline characteristics are presented in Tables A3 and A4. Only the top five most frequent primary diagnoses, which constituted 30–40% of all primary diagnoses, were analysed, while all other primary diagnoses accounted for less than 3%. First, we compared the baseline characteristics between phases 1 and 2 in the intervention and control wards. The intervention ward showed a lower proportion of patients who were women, had a primary diagnosis of fever, and had a higher proportion of primary diagnosis of pneumonia in phase 2, whereas there were no significant differences in the baseline characteristics in the control ward (Table A3). Subsequently, we compared the intervention and control wards in different phases and found no significant differences in the baseline characteristics except for sex (Table A4).
The time series and estimation of the outcome variables from the intervention and control wards are shown in Fig. 1. The estimated changes in the level and slope for each outcome variable are listed in Table 2. As the results from the control ward served as counterfactuals and the outcome variables did not change significantly with respect to the level or slope, we focused on the results for the intervention ward.
Medication errors
The mean number of ME reports was approximately 0.51 and remained constant in phase 1, but increased immediately after the intervention by 1.02 (95% confidence interval [CI]: 0.70 to 1.34, P < 0.001). However, the slope of the mean number of ME reports showed no significant change during the study period (Table 2).
When we investigated ME reports of different types between phases 1 and 2, the mean number of ME reports of the following types presented significantly elevated levels: omissions or medication discrepancies, inappropriate doses or frequencies, ty** errors, inappropriate concentrations or rates of administration, and not-in-benefit packages. Moreover, the mean number of ME reports of the following types showed a slope escalation: inappropriate drug choices, inappropriate routes or formulations, and others. However, no significant level or slope changes were observed for no indication, duplication, allergy or contraindication, drug interaction, or monitor error (Table 3). Notably, the post-pre ratios were 6.11 for omissions or medication discrepancies, 5.02 for inappropriate drug choices, 4.78 for inappropriate route or formulations, and 3.82 for the not-in-benefit package (Fig. 2).
Number of medications
The mean number of daily IPs and SPMs were 8.56 and 2.13 at baseline, respectively. The slope of the mean number of daily IPs increased slowly every month, with a slope of 0.03 (95% CI: 0.02 to 0.05, P = 0.001), while the mean number of daily SPMs did not change during the study period. However, implementation of the NTUH-IMM model did not significantly affect the level and slope of the mean number of daily IPs and SPMs (Table 2).
Medication cost
The baseline of the median daily medication cost was USD 19.45 and increased continuously at the rate of USD 0.14 per month (95% CI: 0.03 to 0.26, P = 0.016) during the study period. There was no level or slope change in the median daily medication cost after the implementation of the NTUH-IMM model (Table 2).
Sensitivity analyses
When we shortened the observational interval to half a month, the observational units increased from 40 to 80 in Phase 1 and from 12 to 24 in Phase 2. However, the direction and size of the effects of the NTUH-IMM model on each outcome variable remained similar to those of the main analysis (Table A5).
Subgroup analyses
When we restricted admission to late-elderly patients, different results were obtained (Table 4). The level of the mean number of daily IPs dropped significantly by 1.78 (95% CI: − 3.06 to − 0.50, P = 0.009) after the NTUH-IMM model was implemented, while no significant change was found in the main analysis. The level of median daily medication cost also decreased by USD 5.90; however, this change was not statistically significant (95% CI: − 12.31 to 0.51, P = 0.078). When we restricted admissions to those without a prolonged LOS or those who did not expire or were transferred to the ICUs during hospitalization, the results were similar to those of the main analysis (Tables A6 and A7).
Discussion
The results support that NTUH-IMM increases the detection and reporting of MEs significantly in hospitalized patients, consistent with prior studies investigating the effects of pharmacist intervention on MEs [16, 17]. Moreover, the number of medications used by late-elderly patients decreased after the implementation of the NTUH-IMM model.
Reliable information is the cornerstone of high-quality CPS [18,19,20]. Therefore, in the NTUH-IMM model, we included several strategies to enable clinical pharmacists to collect more comprehensive medical information than in the case of usual care. First, the NTUH-IMM model requires the clinical pharmacist to participate in medical teams and ward activities. Therefore, the clinical pharmacist can gather medical information from the EMRs and communicate directly with other healthcare professionals. Considering that medical information is not routinely documented and records may be incomplete or inaccurate in EMRs systems [21, 22], direct interaction with other healthcare professionals is another way to retrieve those pieces of information.
Second, unlike usual care, in the NTUH-IMM model, a central pharmacy pharmacist conducted patient interviews to complete the BPMH, and provided these records to the clinical pharmacist. The NTUH-IMM model allows the clinical pharmacist to retrieve additional details on the types of medications and their administration before admission. Several studies have also supported that pharmacist-led medication reconciliation provides a more accurate patient medication history and identifies more medication discrepancies [23,24,25].
Finally, the NTUH-IMM model integrates two pharmacists to perform different parts of CPS. For example, the central pharmacist interviewed the patients and the clinical pharmacist reconciled the medication discrepancies when performing medication reconciliation. These assignments enabled pharmacists to accomplish care tasks and collect medical information more efficiently.
The number of ME reports were observed to increase after we introduced the NTUH-IMM model, whereas the post-pre ratios differed according to the type of ME reports. According to our results, the reported MEs classified as omissions or medication discrepancies increased by more than six times (from a mean of 0.045 to 0.278 per admission). This is consistent with a previous study showing that the pharmacists’ collaboration with other healthcare professionals increases the reporting of medication omission errors [26]. Our results imply that the clinical pharmacist in the NTUH-IMM model received more information about the current status and previous medication history of the patients on admission than under usual care. Considering that approximately 30% of MEs occur during the transition of care, medication reconciliation on admission is crucial and can affect the subsequent hospital course [27]. In general, medication discrepancies can be defined as intended or unintended, and unintended discrepancies are usually regarded as MEs [28]. It is difficult for a pharmacist to distinguish between intended and unintended medication discrepancies solely by referring to EMRs. However, the clinical pharmacist in the NTUH-IMM model could assess whether a medication discrepancy was intended via direct communication with prescribers.
Notably, two types of reported MEs, inappropriate drug choices and not-in-benefit packages, also increased dramatically from a mean of 0.046 to 0.233 per admission and from a mean of 0.100 to 0.383 per admission, respectively. These ME types indicate that the patients have an indication, but the prescribed medication is inappropriate or not covered by the NHI benefits in Taiwan. A pharmacist cannot decide whether the medication in use is appropriate without sufficient medical information because any medication can be used for several indications and the clinical signs and symptoms of the patients are diverse. Under the NTUH-IMM model, the clinical pharmacist participated in ward rounds to directly observe and interact with patients and to better evaluate the appropriateness of medication use.
From the subgroup analysis, the mean daily IPs decreased in late-elderly patients after implementing the NTUH-IMM model. This is probably because the complex regimen for late-elderly patients with multiple morbidities has more room for improvement. Polypharmacy is a critical problem in elderly patients and is associated with multimorbidity [29, 30], and the incidence of unnecessary medication use is higher in patients with polypharmacy [31]. Based on previous research, up to 44% of hospitalized elderly patients have at least one unnecessary medication at discharge [32]. In our study, the prevalence of excessive polypharmacy (defined as using more than 10 medications) in late-elderly patients was 68.4% in Phase 1 and 74.8% in Phase 2 (data not shown here). Therefore, we expect that the late-elderly have a higher risk of unnecessary medication use, meaning that our intervention can reduce the number of medications.
As the NTUH-IMM model decreased the number of daily IPs for late-elderly patients, we assumed that it could further reduce the daily medication costs. Although the reduction in daily medication costs was not statistically significant, the estimated change for late-elderly patients was larger than that in the main analysis. Furthermore, reducing inappropriate drug choices and doses or frequencies could potentially reduce the medication costs. For example, when a late-elderly patient is treated with antibiotics, the clinical pharmacist might recommend switching to an agent with a narrower spectrum, lowering the dose, or even ceasing it according to the patient’s clinical situation, which could result in a decrease in the cost of medication. Although central pharmacy pharmacists could also recommend prescribers to adjust regimens, they are not able to provide timely responses; additionally, the lack of a collaborative relationship between the central pharmacy pharmacists and other healthcare professionals might impede the application of the recommendation.
To the best of our knowledge, few studies have investigated the impact of a service model on ME reporting and medication utilization in a real-world setting. The ITS design used in this study may further inform researchers who want to examine their services using longitudinal data. As the outcome variables were all potentially confounded by time-varying variables, such as autocorrelation or maturation, we conducted an ITS analysis with segment regression and autoregressive error models to address these problems. Furthermore, we introduced an external control to avoid history threats. The allocation of patients was assumed to be similar to randomization, as the managers were blinded to the study. Sensitivity and subgroup analyses were also conducted to confirm the results and address any effect modifications.
This study has a few limitations. First, only prescription errors were recorded in NTUH-PSRD. However, the NTUH-IMM model can logically reduce administration and transcription errors by integrating a clinical pharmacist into the medical team. Therefore, the actual effect of the NTUH-IMM model on ME reporting should be larger if administration and transcription errors were considered. Second, the study was not blinded to the pharmacists in the intervention ward; therefore, they might have made extra efforts to detect and report MEs. Even though the study did not provide additional rewards to pharmacists, an overestimated effect of the NTUH-IMM model on the number of ME reports is anticipated. Third, our study might be underpowered for some outcomes, given that the effect size of the NTUH-IMM model might be small for the mean number of IPs and SPMs and median medication cost. The power of ITS depends on the number of observational units. We had limited observational units with a relatively short observation period in phase 2, and we might not have been able to observe the long-term effect of the NTUH-IMM. Nevertheless, the number of observational units in our study met the general requirement (at least 12 points before and after the intervention) [33]. Finally, although the medication cost was based on the NHI reimbursement price in November 2020, the reimbursement price may change over time.
To further support the findings of this study, future studies could evaluate the impacts of IMM model implementation in a larger population or a different setting. Future pharmacoeconomics studies may also be conducted to confirm the effects of CPS on medical costs.
Conclusions
These results support our intervention, which helps lower MEs in hospitalized patients and reduces the number of medications used for late-elderly patients. Therefore, we recommend that hospitals include clinical pharmacists in their medical teams to perform CPS, which can improve patient safety and optimize medication utilization.
Availability of data and materials
The datasets generated and analyzed during the current study are not publicly available due to following reasons. First, the data are originated from electronic medical records at NTUH, and they contain sensitive patient information at both the patient and the institution levels. According to the “Personal Information Protection Act”, the availability of medical records is restricted by the government of Taiwan. Thus, the data cannot be distributed publicly. Second, according to the policy and regulations of the data use agreement, the data are only available to the employees of NTUH; using data for other purposes require a direct approval from the Department of Medical Research, NTUH. The authors have no right to share the data without the permission from the Department of Medical Research, NTUH. To request access of the data, please contact Department of Medical Research, NTUH directly at cmrd@ntuh.gov.tw.
Abbreviations
- CPS:
-
Clinical pharmaceutical service
- DMM:
-
Division of Multidisciplinary Medicine
- EMR:
-
Electronic medical record
- ICU:
-
Intensive care unit
- IP:
-
Inpatient prescription
- ITS:
-
Interrupted time series
- LOS:
-
Length of stay
- ME:
-
Medication error
- NHI:
-
National Health Insurance
- NTUH:
-
National Taiwan University Hospital
- NTUH-iMD:
-
NTUH Integrated Medical Database
- NTUH-IMM:
-
NTUH Integrated Medication Management
- NTUH-PSRD:
-
NTUH Pharmaceutical Service Record Database
- NTD:
-
New Taiwan dollar
- SPM:
-
Self-prepared medication
- USD:
-
United States dollar
References
Ferner RE, Aronson JK. Clarification of terminology in medication errors. Drug Saf. 2006;29(11):1011–22.
Krähenbühl-Melcher A, Schlienger R, Lampert M, Haschke M, Drewe J, Krähenbühl S. Drug-related problems in hospitals: a review of the recent literature. Drug Saf. 2007;30(5):379–407.
Lin HY, Liao CC, Cheng SH, Wang PC, Hsueh YS. Association of potentially inappropriate medication use with adverse outcomes in ambulatory elderly patients with chronic diseases: experience in a Taiwanese medical setting. Drugs Aging. 2008;25(1):49–59.
Assiri GA, Shebl NA, Mahmoud MA, Aloudah N, Grant E, Aljadhey H, et al. What is the epidemiology of medication errors, error-related adverse events and risk factors for errors in adults managed in community care contexts? A systematic review of the international literature. BMJ Open. 2018;8(5):e019101.
Walsh EK, Hansen CR, Sahm LJ, Kearney PM, Doherty E, Bradley CP. Economic impact of medication error: a systematic review. Pharmacoepidemiol Drug Saf. 2017;26(5):481–97.
Lehnbom EC, Stewart MJ, Manias E, Westbrook JI. Impact of medication reconciliation and review on clinical outcomes. Ann Pharmacother. 2014;48(10):1298–312.
Beuscart J-B, Pelayo S, Robert L, Thevelin S, Marien S, Dalleur O. Medication review and reconciliation in older adults. Eur Geriatr Med. 2021;12:499–507.
Baudouin A, Herledan C, Poletto N, Guillemin MD, Maison O, Garreau R, et al. Economic impact of clinical pharmaceutical activities in hospital wards: a systematic review. RSAP. 2021;17(3):497–505.
Bernal JL, Cummins S, Gasparrini A. Interrupted time series regression for the evaluation of public health interventions: a tutorial. Int J Epidemiol. 2016;46(1):348–55.
Lopez Bernal J, Cummins S, Gasparrini A. The use of controls in interrupted time series studies of public health interventions. Int J Epidemiol. 2018;47(6):2082–93.
Shu CC, Lin JW, Lin YF, Hsu NC, Ko WJ. Evaluating the performance of a hospitalist system in Taiwan: a pioneer study for nationwide health insurance in Asia. J Hosp Med. 2011;6(7):378–82.
Scullin C, Scott MG, Hogg A, McElnay JC. An innovative approach to integrated medicines management. J Eval Clin Pract. 2007;13(5):781–8.
National Health Insurance, PharmaCloud System, available at: https://www.nhi.gov.tw/english/Content_List.aspx?n=02BA04454AED80E0&topn=BCB2B0D2433F6491, access Dec, 2021.
Majeed MU, Williams DT, Pollock R, Amir F, Liam M, Foong KS, et al. Delay in discharge and its impact on unnecessary hospital bed occupancy. BMC Health Serv Res. 2012;12:410.
Toh HJ, Lim ZY, Yap P, Tang T. Factors associated with prolonged length of stay in older patients. Singap Med J. 2017;58(3):134–8.
Chiewchantanakit D, Meakchai A, Pituchaturont N, Dilokthornsakul P, Dhippayom T. The effectiveness of medication reconciliation to prevent medication error: a systematic review and meta-analysis. RSAP. 2020;16(7):886–94.
Manias E, Kusljic S, Wu A. Interventions to reduce medication errors in adult medical and surgical settings: a systematic review. Ther Adv Drug Saf. 2020;11:2042098620968309.
Boockvar KS, Santos SL, Kushniruk A, Johnson C, Nebeker JR. Medication reconciliation: barriers and facilitators from the perspectives of resident physicians and pharmacists. J Hosp Med. 2011;6(6):329–37.
Brazinha I, Fernandez-Llimos F. Barriers to the implementation of advanced clinical pharmacy services at Portuguese hospitals. Int J Clin Pharm. 2014;36(5):1031–8.
Uema SA, Vega EM, Armando PD, Fontana D. Barriers to pharmaceutical care in Argentina. Pharm World Sci. 2008;30(3):211–5.
Hogan WR, Wagner MM. Accuracy of data in computer-based patient records. J Am Med Inform Assoc. 1997;4(5):342–55.
Monte AA, Anderson P, Hoppe JA, Weinshilboum RM, Vasiliou V, Heard KJ. Accuracy of electronic medical record medication reconciliation in emergency department patients. J Emerg Med. 2015;49(1):78–84.
Becerra-Camargo J, Martinez-Martinez F, Garcia-Jimenez E. A multicentre, double-blind, randomised, controlled, parallel-group study of the effectiveness of a pharmacist-acquired medication history in an emergency department. BMC Health Serv Res. 2013;13(1):1–12.
Kwan Y, Fernandes OA, Nagge JJ, Wong GG, Huh J-H, Hurn DA, et al. Pharmacist medication assessments in a surgical preadmission clinic. Arch Intern Med. 2007;167(10):1034–40.
Marotti S, Kerridge R, Grimer M. A randomised controlled trial of pharmacist medication histories and supplementary prescribing on medication errors in postoperative medications. Anaesth Intensive Care. 2011;39(6):1064–70.
Costello JL, Torowicz DL, Yeh TS. Effects of a pharmacist-led pediatrics medication safety team on medication-error reporting. Am J Health Syst Pharm. 2007;64(13):1422–6.
Tam VC, Knowles SR, Cornish PL, Fine N, Marchesano R, Etchells EE. Frequency, type and clinical importance of medication history errors at admission to hospital: a systematic review. CMAJ. 2005;173(5):510–5.
Action on Patient Safety - High 5s. World Health Organization. Available at: http://www.who.int/patientsafety/topics/high-5s/en/, Accessed May 16, 2021.
Hajjar ER, Cafiero AC, Hanlon JT. Polypharmacy in elderly patients. Am J Geriatr Pharmacother. 2007;5(4):345–51.
Fulton MM, Riley AE. Polypharmacy in the elderly: a literature review. J Am Acad Nurse Pract. 2005;17(4):123–32.
Rahmawati F, Pramantara I, Rohmah W, Sulaiman SAS. Polypharmacy and unnecessary drug therapy on geriatric hospitalized patients in Yogyakarta hospitals. Indonesia Int J Pharm Pharm Sci. 2009;1(1):6–11.
Hajjar ER, Hanlon JT, Sloane RJ, Lindblad CI, Pieper CF, Ruby CM, et al. Unnecessary drug use in frail older people at hospital discharge. J Am Geriatr Soc. 2005;53(9):1518–23.
Zhang F, Wagner AK, Ross-Degnan D. Simulation-based power calculation for designing interrupted time series analyses of health policy interventions. J Clin Epidemiol. 2011;64(11):1252–61.
Acknowledgments
We would like to thank the staff of the Department of Medical Research, NTUH, for retrieving the data from NTUH-iMD and de-identifying the data for NTUH-PSRD. We are also grateful to Ms. Yu-Ting Huang, the clinical pharmacist at the time of the study, and Mr. Chien-Chih Wu and Ms. Ming-Fang Wen for develo** the NTUH-IMM model.
Funding
This program was funded by the NTUH grant for employees (grant number 109-M4455). As a funding party, the NTUH was not directly involved in any aspect of the study design or conduct. The grant only supports reimbursement for consumables, editing services, and publication charges and not for other additional personnel expenses. Therefore, the researchers are independent of the executive management of the NTUH in the design of the study, data analysis, interpretation of the results, and writing of the manuscript.
Author information
Authors and Affiliations
Contributions
K. L. C., C. F. H., C. C. W., and L. J. S. conceived of the study. K. L. C. designed the study. K. L. C. cleaned and analysed the data. K. L. C., C. C. W., and L. J. S. interpreted results. K. L. C. wrote the draft of the manuscript and prepared tables and Figs. C. F. H., W. H. S., Y. K. C., C. C. W., and L. J. S. revised the manuscript. All the authors reviewed the manuscript.
Corresponding authors
Ethics declarations
Ethical approval and consent to participate
The NTUH-IMM model only redesigned the workflow of the pharmacy; thus, the patients did not receive any services or invasive procedures that might increase their risk. In addition, the data used in this study were de-identified and analysed retrospectively. The need for informed consent was waived by the NTUH Research Ethics Committee (NTUH-REC) due to the retrospective nature of the study. The study was approved by the NTUH-REC (201906033RINB). All the methods were carried out in accordance with the in-house guidelines and regulations formulated by the NTUH-REC office.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1: Table A1.
Definitions of the different types of medication errors in the reporting system at the NTUH. Table A2. Outcome variable definitions. Table A3. Baseline characteristics of the patients between phases 1 and 2. Table A4. Baseline characteristics of the patients between the intervention and control wards. Table A5. Sensitivity analysis: effects of the NTUH-IMM model on outcome variables when shortening the observational interval to half-month. Table A6. Subgroup analysis: Effects of the NTUH-IMM model on the outcome variables in patients without prolonged lengths of stay. Table A7. Subgroup analysis: Effects of the NTUH-IMM model on the outcome variables for patients who did not expire or were transferred to the intensive care unit during hospitalization
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Chen, KL., Hunag, CF., Sheng, WH. et al. Impact of integrated medication management program on medication errors in a medical center: an interrupted time series study. BMC Health Serv Res 22, 796 (2022). https://doi.org/10.1186/s12913-022-08178-w
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12913-022-08178-w