Abstract
Background
Surgical treatment for recurrent patellar dislocation (RPD) could yield good outcomes. While, unsatisfactory recovery still exists in some cases. For all prognostic factors, serum biomarkers have rarely been investigated. This study aimed to evaluate the prognostic value of preoperative serum calcium level, a widely used serum biomarker, in surgical treatment for RPD.
Study design
Retrospective study.
Methods
Ninety-nine patients with RPD were enrolled in the study. Preoperative serum calcium was acquired from routinely tested blood 1 day prior to operation. Demographic data, characteristics of RPD, postoperative functional outcomes were obtained. The association between preoperative calcium and postoperative functional outcomes (Kujala, Lysholm, Tegner, IKDC and KOOS score) was determined by correlation analysis and multivariate linear regression analysis. Poor recovery was determined as Kujala score below 80. The receiver operating characteristic (ROC) curve was used to assess the prognostic value of preoperative calcium.
Results
Patients were followed up for a mean period of 2.45 ± 1.33 years. All clinical scores showed significant improvement at the latest follow-up. Correlation and multivariate linear analyses indicated that serum calcium level was an important factor related with the prognosis of surgical treatment for RPD. According to the ROC curve, the cut-off value for preoperative calcium was 2.225 mmol/L. The clinical outcomes of patients with a preoperative blood calcium < 2.225 mmol/L was significantly worse than that with a higher calcium level. The correspondent sensitivity was 0.812 with a specificity of 0.633.
Conclusion
Operative treatment for RPD achieved good results, while in some cases the functional scores remain inferior. As a serum biomarker, preoperative calcium could be prognostic for outcomes after surgical treatment for RPD.
Similar content being viewed by others
Introduction
Recurrent patellar dislocation (RPD), a common issue plaguing adolescent, is associated with various anatomical factors including soft tissue and bony abnormalities [1,2,3]. Medial patellofemoral ligament (MPFL) reconstruction combined with or without tibial tubercle (TT) transfer has been widely employed to treat recurrent patellar dislocation and usually yields favorable outcomes [4]. However, inferior postoperative outcomes are still presented in some cases and reoperation may be required [5].
Identification of prognostic factors may help classify patients for whom postoperative outcome is more likely to be inferior and pay special attention to improve these patients’ recovery [6]. Numerous factors have been investigated for recurrent patellar dislocation, including age, sex, patella alta, trochlear dysplasia, J-sign and various surgical techniques [7, 8]. Multiple researchers have developed predictive models for recurrent instability by combining these individual factors in different ways [9, 10]. To date, these models remain complex and require multiple imaging examinations, imposing a burden on patients’ cost. Postoperative recovery is affected by metabolic processes associated with inflammation [11], collagen or bone turnover [12], which may have a role in predicting the prognosis. Biomarkers, as a manifestation of these metabolic processes, have a potential utility in develo** early diagnoses and evaluating prognosis [13]. Compared with other methods, biomarkers can be collected relatively easily form serum or urine and may be less costly. The identification of such biomarkers could better assist practitioners in assessing the prognosis of patients undergoing operation. As a widespread secondary messenger within multiple intracellular signaling pathways, calcium is involved in the bone turnover and a myriad of vital cellular activities including proliferation, motility and apoptosis, suggesting that calcium plays an important role in tissue regeneration and parenchymal function across the body [14]. In recent years, serum calcium level has been used to help determine the prognosis of cardiovascular event, cognitive decline and cancer [15,16,17].
Therefore, the aim of this study was to evaluate the association between preoperative serum calcium level and the clinical outcome after surgical treatment for recurrent patellar dislocation. Our assumption was that the serum calcium level could be a prognostic factor of recurrent patellar dislocation.
Methods
Study design and participants
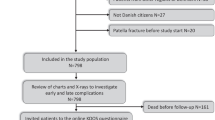
This was a single-center, retrospective study. It was registered in the Chinese Clinical Trial Registry (ChiCTR2100052216) in 22/10/2021. The methods were performed in accordance with the relevant guidelines and regulations. We retrospectively studied the patients that were consecutively enrolled in the institutional database program of RPD from January 2017 to October 2020. The inclusion criteria were closed epiphysis, more than 2 episodes of dislocation or 1 episode of dislocation plus multiple episodes of instability (lateral excursion of the patella), and a tibial tubercle-trochlear groove (TT-TG) distance > 15 mm. The exclusion criteria were concomitant ligament injuries (except MPFL), previous knee surgeries, and femoral trochlear dysplasia requiring trochleoplasty.
Surgical techniques and rehabilitation
A single experienced surgeon (J.Z.) in our institution conducted the surgical procedures. The whole procedure was similar to that described by Zhao et al. [18]. MPFL was reconstructed with autogenous semitendinosus tendons and by tunnel technique. Lateral retinaculum release was performed by pulling the patella medially with the graft. The procedure of TT transfer is a modification of Fulkerson’s osteotomy. The proximal part of the bone fragment was transferred anteromedially, with the distal tapering end left in place or, in some cases, rotated laterally along the osteotomy surface. The purpose was to mitigate the TT-TG distance to 5-10 mm.
Partial to full weightbearing was allowed with a hinged brace locked in extension immediately after the operation. The brace was removed at 6 weeks after surgery. Progressive range of motion exercises were started on the first day after surgery. Squats against the wall, step-up exercises and proprioception training were started at 6 weeks postoperatively. Running and agility training was permitted 3 months after the operation.
Clinical variables and outcome measurements
Demographic data including sex, body mass index, age, and characteristics of patellar dislocation including patellar height, femoral trochlear dysplasia, lateral patellar tilt, sulcus angle, and TT-TG distance were recorded. Serum calcium level 1 day before the operation was also recorded. Functional scores were obtained preoperatively and at the latest follow-up, including the Kujala score, Knee Injury and Osteoarthritis Outcome (KOOS) score, Tegner Score, International Knee Documentation Committee (IKDC) subjective score and Lysholm score. Poor recovery was defined as a Kujala score below 80 [5].
Statistical analysis
Analyses of the data obtained in the study were performed with SPSS (26.0; IBM). The Student t test or Mann-Whitney U test was conducted to compare the postoperative outcomes according to the normality of the data. The chi-square test was used to compare nominal variables. Pearson or Spearman correlation analysis was performed to analyze the relationship between obtained variables and postoperative outcomes. Multivariate linear regression analysis was conducted when more than one factor showed a significant correlation with 1 postoperative outcome. The predictive threshold value was determined by ROC curve and Youden index. Statistical significance was set at 0.05.
Since there are no previous reports testing the diagnosis value of serum calcium for postoperative recovery of patellar dislocation, a sample size calculation was not available prior to the patient enrollment. A post hoc calculation was instead performed with PASS software (15.0) according to the sensitivity and specificity acquired. The type I error was set at 0.05 with a permissible error of 10% for sensitivity and specificity.
Results
Ninety-nine patients were included in this study. The baseline demographic data of the patients are provided in Table 1. No chronic effusion or other adverse events were reported after the surgery. All postoperative functional scores improved significantly compared with preoperative scores (Table 2).
The correlation between the serum calcium and postoperative results was analyzed (Table 3). Preoperative calcium was significantly and positively associated with postoperative Kujala score (P = .001), IKDC score (P < .001), KOOS pain score (P = .001), KOOS daily living activities score (P = .018), KOOS sports and recreation (P = .001), and KOOS knee-related quality of life (P = .035). These correlations suggested that a higher calcium level was associated with a better postoperative recovery.
For other potentially critical factors, a correlation analysis was conducted (Table 4). An older age was significantly related to worse postoperative outcomes: IKDC score (B = − 0.297; P = .003), Lysholm score (B = − 0.316; P = .001), Kujala score (B = − 0.310; P = .002), KOOS pain score (B = − 0.385; P = .001), KOOS daily living activities score (B = − 0.309; P = .002), and KOOS sports score (B = − 0.227; P = .024). Additionally, a greater Insall-Salvati ratio was associated with a worse KOOS symptom score (B = − 0.231; P = .043) and KOOS knee-related quality of life (B = − 0.247; P = .030). A greater sulcus angle was associated with a worse KOOS pain score (B = − 0.225; P = .028).
To further identify whether calcium or age was independently associated with postoperative recovery, multivariate linear regression analysis was performed (Table 5). It was indicated that age and calcium acted together in postoperative Kujala and KOOS pain score, while preoperative calcium was the only factor associated with IKDC (P = .001), KOOS sports (P = .004) and life quality score (P = .035).
In order to identify the cut-off value of serum calcium for postsurgical recovery, the ROC curve was drawn and the area under the curve was 0.744. The Youden index reached a maximum when the cutoff value of calcium was 2.225 (Fig. 1). The correspondent sensitivity was 0.812 with a specificity of 0.633. Post hoc sample size calculation showed that 86 cases were needed to achieve statistical significance with respect to specificity and 58 cases with respect to sensitivity. Given that the present cohort involved 99 patients, the acquired diagnostic information was plausible.
The 99 subjects were then categorized according to this cutoff value, among which 32 were in lower calcium group. The separate pre- and postoperative measurements for each group, and the comparison between the 2 groups are presented in Table 6. For cases with a higher preoperative serum calcium, the postoperative functional scores all improved significantly. In contrast, not all functional scores improved significantly in the lower calcium group and the higher calcium group had a greater score in most postoperative functional tests compared with the lower group. Additionally, by using the cutoff values of Kujala to categorize patients, it is noted that the proportion of cases with Kujala < 80 was significantly greater in cases with calcium < 2.225 mmol/L (59.4%) than those in the higher calcium group (16.4%) and the risk ratio was 3.62 (95% CI, 1.96-6.67) (Fig. 2). These results suggested that the current threshold value of calcium had practicability indeed. For rate of re-dislocation, the higher group was 3.0% (2 of 67) and the lower group was 3.1% (1 of 32). There was no significant difference between the two groups.
Discussion
In the present study, it is noted that for recurrent patellar dislocation, preoperative serum calcium level was an important factor associated with the prognosis of surgical treatment for RPD. Patients with a preoperative calcium < 2.225 mmol/L should be given extra attention postoperatively for a 3.62 times higher risk of poor recovery.
As a common issue in sports medicine, much attention is paid to RPD and numerous researchers have studied the prognostic factors. Ling et al. [6] developed a multivariable model which can identify the first-time dislocation patients who are at high risk for recurrent dislocation and thus could benefit from early surgical treatment. Age, skeletal immaturity and other anatomical factors have been identified as risk factors. Zhang et al. [19] noted that a pre-operative grade 3 J-sign was an adverse factor in operative treatment for RPD. In this study, we attempted to explore relevant factors from easily omitted but abundant blood sample data, and identified calcium as a serum biomarker for the prognosis of RPD for the first time.
As a powerful second messenger, the silent, sub-clinical variation in serum calcium is suggested to be consequential and has implications for disease susceptibility or prognosis [20,21,22]. It has been reported to be associated with the prognosis of various diseases, including neonatal sepsis [23], nasopharyngeal carcinoma [24], acute pulmonary embolism [16] and cognitive impairment [21]. In the present study, serum calcium level was an influential factor associated with postoperative knee function. The patients with poor postoperative recovery (Kujala < 80) had a lower preoperative calcium value than their counterparts in the study. These findings suggest that calcium level has a predictive potential for knee function and recovery after operative treatment of RPD. Patients with a preoperative calcium < 2.225 mmol/L may have a higher risk for poor recovery and low knee function. Extra attention should be paid to these patients during the rehabilitation process and the rehabilitation protocol could be individualized to better fit their recovery situation and improve their knee function.
As the most plentiful mineral in the human body, serum calcium level is usually within the normal range and affected by several vital factors, including vitamin D, parathyroid hormone, phosphorous and magnesium [25, 26]. Parathyroid hormone and vitamin D could raise blood calcium level via increasing the absorption of calcium in the intestine [25]. Increased phosphorus could bind to calcium, thereby lowering the calcium level. Low magnesium level may inhibit the release of parathyroid hormone, leading to calcium deficiency [26].
Although the exact pathophysiological mechanism underlying these clinical observations remains unclear, especially whether serum calcium level exerts a principal effect on recovery, or if it reflects a secondary epiphenomenon of other unidentified factors, there might be several possible explanations for this association. First, calcium is associated with bone formation and metabolism. Extracellular or exogenous calcium could induce mesenchymal stem cell recruitment, osteoblast differentiation and promote bone tissue regeneration [27, 28]. The healing of TT osteotomy site and bone tunnels could potentially benefit from high normocalcemia. Second, as an essential element, calcium is a crucial regulator of epidermal homeostasis and associated with cardiovascular system [29,30,31]. Extracellular calcium could improve skin wound repair, vascular smooth muscle cell proliferation and arterial contractility through Ca2+-sensing receptor, thus benefiting the postoperative recovery. Due to its role in a wide range of physiological processes, including cell signaling, neurotransmission, and muscle contraction, many other factors such as vitamin D or parathyroid hormone may underlie these clinical observations and could be studied further in the future.
Calcium, as a regulated target, is closely related to vitamin D. The intestinal absorption of calcium and phosphorus is optimized by vitamin D to formulate the bone mineral matrix [32, 33]. Calcium and vitamin D both play a crucial role in bone remodeling and mineralization, thus may impacting the orthopaedic outcomes [32]. Recently, vitamin D has been identified as an influential factor in various orthopaedic procedures. Choi et al. demonstrated that patients with vitamin D deficiency had less favorable functional outcomes after high tibial osteotomy surgery [34]. Shin et al. reported that vitamin D deficiency could adversely affect early post-operative functional outcomes following total knee arthroplasty [35]. While, the serum calcium level in their studies showed no significant difference between the vitamin D deficient and sufficient group. Due to the relatively scarce researches, the relationships between calcium, vitamin D and orthopaedic outcomes awaits investigation.
Additionally, in the present study, an older age was associated with a poor outcome in most functional scores and acted together with calcium in influencing postoperative Kujala and KOOS pain score. In line with the current study, Sambeeck et al. [36] indicated that age was correlated with an increased pain score at rest. Ling et al. [6] noted age as a variable of biggest relative importance in a multivariable model predicting for a recurrent dislocation. Since the peak incidence of first patellar dislocation is in adolescence [37], a possible explanation may be that older patients usually have a longer history of patellofemoral instability and patellar maltracking. Therefore, increased cartilage damage and degenerative changes would be seen at time of surgery, thus affecting the postoperative outcomes.
The present study has several limitations. First, patients enrolled all received TT transfer combined with MPFL reconstruction by tunnel technique, therefore the practicability of the current calcium threshold value in other surgical conditions requires more validation. Second, we could only analyze the correlation between serum calcium and the prognosis of RPD instead of disentangling the causality. Thus, we cannot determine the specific role that serum calcium plays in the pathophysiology of RPD. Third, due to the nature of retrospective study, only preoperative serum calcium was evaluated and a potential change in postoperative calcium levels and the impact on outcomes could not be evaluated. Due to the relatively scant information on related topic, it remains unknown whether a patient with preoperative low normocalcemia or hypocalcemia should receive calcium supplementation preoperatively or postoperatively. Fourth, some other contributing factors such as preoperative cartilage status, J-sign, MPFL tear pattern, generalized joint hyperlaxity and limb alignment, were not examined in this study which could add bias.
Conclusion
Overall, operative treatment for RPD achieved good results, while in some cases the functional scores remain inferior. As a serum biomarker, preoperative calcium could be prognostic for outcomes after surgical treatment for RPD.
Availability of data and materials
The datasets used and/or analysed during the current study are available from the corresponding author on reasonable request.
References
Ferlic PW, Runer A, Dammerer D, Wansch J, Hackl W, Liebensteiner MC. Patella height correlates with trochlear dysplasia: a computed tomography image analysis. Arthroscopy. 2018;34(6):1921–8.
Colvin AC, West RV. Patellar instability. J Bone Joint Surg Am. 2008;90(12):2751–62.
Ward SR, Terk MR, Powers CM. Patella alta: association with patellofemoral alignment and changes in contact area during weight-bearing. J Bone Joint Surg Am. 2007;89(8):1749–55.
Fisher B, Nyland J, Brand E, Curtin B. Medial patellofemoral ligament reconstruction for recurrent patellar dislocation: a systematic review including rehabilitation and return-to-sports efficacy. Arthroscopy. 2010;26(10):1384–94.
Schneider DK, Grawe B, Magnussen RA, Ceasar A, Parikh SN, Wall EJ, et al. Outcomes after isolated medial Patellofemoral ligament reconstruction for the treatment of recurrent lateral patellar dislocations: a systematic review and Meta-analysis. Am J Sports Med. 2016;44(11):2993–3005.
Ling DI, Brady JM, Arendt E, Tompkins M, Agel J, Askenberger M, et al. Development of a multivariable model based on individual risk factors for recurrent lateral patellar dislocation. J Bone Joint Surg Am. 2021;103(7):586–92.
Mountney J, Senavongse W, Amis AA, Thomas NP. Tensile strength of the medial patellofemoral ligament before and after repair or reconstruction. J Bone Joint Surg (Br). 2005;87(1):36–40.
Tsuda E, Ishibashi Y, Yamamoto Y, Maeda S. Incidence and radiologic predictor of postoperative patellar instability after Fulkerson procedure of the tibial tuberosity for recurrent patellar dislocation. Knee Surg Sports Traumatol Arthrosc. 2012;20(10):2062–70.
Hevesi M, Heidenreich MJ, Camp CL, Hewett TE, Stuart MJ, Dahm DL, et al. The recurrent instability of the Patella score: a statistically based model for prediction of long-term recurrence risk after first-time dislocation. Arthroscopy. 2019;35(2):537–43.
Arendt EA, Askenberger M, Agel J, Tompkins MA. Risk of Redislocation after primary patellar dislocation: a clinical prediction model based on magnetic resonance imaging variables. Am J Sports Med. 2018;46(14):3385–90.
Szpaderska AM, DiPietro LA. Inflammation in surgical wound healing: friend or foe? Surgery. 2005;137(5):571–3.
Inose H, Yamada T, Mulati M, Hirai T, Ushio S, Yoshii T, et al. Bone turnover markers as a new predicting factor for nonunion after spinal fusion surgery. Spine (Phila Pa 1976). 2018;43(1):E29–e34.
Mayeux R. Biomarkers: potential uses and limitations. NeuroRx. 2004;1(2):182–8.
Hands JM, Moy LS. Calcium: more than bone? Implications for clinical practice and theory. J Clin Med Res. 2021;13(5):253–7.
O'Grady S, Morgan MP. Calcium transport and signalling in breast cancer: functional and prognostic significance. Semin Cancer Biol. 2021;72:19–26.
Wang X, **ang Y, Zhang T, Yang Y, Sun X, Shi J. Association between serum calcium and prognosis in patients with acute pulmonary embolism and the optimization of pulmonary embolism severity index. Respir Res. 2020;21(1):298.
Navakkode S, Liu C, Soong TW. Altered function of neuronal L-type calcium channels in ageing and neuroinflammation: implications in age-related synaptic dysfunction and cognitive decline. Ageing Res Rev. 2018;42:86–99.
Zhao J, Huangfu X, He Y. The role of medial retinaculum plication versus medial patellofemoral ligament reconstruction in combined procedures for recurrent patellar instability in adults. Am J Sports Med. 2012;40(6):1355–64.
Zhang Z, Zhang H, Song G, Zheng T, Feng H. A pre-operative grade 3 J-sign adversely affects short-term clinical outcome and is more likely to yield MPFL residual graft laxity in recurrent patellar dislocation. Knee Surg Sports Traumatol Arthrosc. 2020;28(7):2147–56.
Wu X, Han T, Gao J, Zhang Y, Zhao S, Sun R, et al. Association of serum calcium and insulin resistance with hypertension risk: a prospective population-based study. J Am Heart Assoc. 2019;8(1):e009585.
Sato K, Mano T, Ihara R, Suzuki K, Tomita N, Arai H, et al. Lower serum calcium as a potentially associated factor for conversion of mild cognitive impairment to early Alzheimer's disease in the Japanese Alzheimer's disease neuroimaging initiative. J Alzheimers Dis. 2019;68(2):777–88.
Poudel K, Shah AM, Michos ED, Folsom AR, Konety S, Lutsey PL. Association of serum calcium and phosphorus with measures of left ventricular structure and function: the ARIC study. Nutr Metab Cardiovasc Dis. 2020;30(5):758–67.
Liu Y, Chai Y, Rong Z, Chen Y. Prognostic value of ionized calcium levels in neonatal Sepsis. Ann Nutr Metab. 2020;76(3):193–200.
Huang SY, Chen Y, Tan XR, Gong S, Yang XJ, He QM, et al. Serum calcium levels before antitumour therapy predict clinical outcomes in patients with nasopharyngeal carcinoma. Onco Targets Ther. 2020;13:13111–9.
Goltzman D, Mannstadt M, Marcocci C. Physiology of the calcium-parathyroid hormone-vitamin D Axis. Front Horm Res. 2018;50:1–13.
Goff JP. Calcium and magnesium disorders. Vet Clin North Am Food Anim Pract. 2014;30(2):359–381, vi.
Aquino-Martínez R, Artigas N, Gámez B, Rosa JL, Ventura F. Extracellular calcium promotes bone formation from bone marrow mesenchymal stem cells by amplifying the effects of BMP-2 on SMAD signalling. PLoS One. 2017;12(5):e0178158.
Aquino-Martínez R, Angelo AP, Pujol FV. Calcium-containing scaffolds induce bone regeneration by regulating mesenchymal stem cell differentiation and migration. Stem Cell Res Ther. 2017;8(1):265.
Tu CL, Celli A, Mauro T, Chang W. Calcium-sensing receptor regulates epidermal intracellular Ca (2+) signaling and re-epithelialization after wounding. J Invest Dermatol. 2019;139(4):919–29.
Hannan FM, Kallay E, Chang W, Brandi ML, Thakker RV. The calcium-sensing receptor in physiology and in calcitropic and noncalcitropic diseases. Nat Rev Endocrinol. 2018;15(1):33–51.
Molostvov G, Fletcher S, Bland R, Zehnder D. Extracellular calcium-sensing receptor mediated signalling is involved in human vascular smooth muscle cell proliferation and apoptosis. Cell Physiol Biochem. 2008;22(5-6):413–22.
Fischer V, Haffner-Luntzer M, Amling M, Ignatius A. Calcium and vitamin D in bone fracture healing and post-traumatic bone turnover. Eur Cell Mater. 2018;35:365–85.
Moon AS, Boudreau S, Mussell E, He JK, Brabston EW, Ponce BA, et al. Current concepts in vitamin D and orthopaedic surgery. Orthop Traumatol Surg Res. 2019;105(2):375–82.
Choi W, Kim JH, Byun SE, Ryu HS, Rojas D. Effect of preoperative vitamin D deficiency on functional outcomes after high tibial osteotomy: a retrospective case control study. BMC Musculoskelet Disord. 2020;21(1):251.
Shin K-Y, Park KK, Moon S-H, Yang IH, Choi H-J, Lee W-S. Vitamin D deficiency adversely affects early post-operative functional outcomes after total knee arthroplasty. Knee Surg Sports Traumatol Arthrosc. 2017;25(11):3424–30.
van Sambeeck JDP, Verdonschot N, Van Kampen A, van de Groes SAW. Age at surgery is correlated with pain scores following trochlear osteotomy in lateral patellar instability: a cross-sectional study of 113 cases. J Orthop Surg Res. 2021;16(1):337.
Fithian DC, Paxton EW, Stone ML, Silva P, Davis DK, Elias DA, et al. Epidemiology and natural history of acute patellar dislocation. Am J Sports Med. 2004;32(5):1114–21.
Acknowledgments
Not applicable.
Funding
This work was supported by the Exploratory Research Program of Shanghai Jiao Tong University Affiliated Sixth People’s Hospital (grant YNTS202001) and Shanghai Pujiang Program (grant number 2020PJD041). The funders provided assistance in data collection and manuscript preparation.
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design. The surgeries were performed by JZZ. Material preparation and data collection were performed by YQ, ZPY, JJX, XYZ and JBC. JZZ, SZ and CQX contributed to the design and supervision of the research. The first draft of the manuscript was written by YQ. YQ and ZPY analysed the data. YQ and JJX created the Tables. YQ, XYZ and JBC prepared the drawn images. JZZ, SZ and CQX commented on the previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding authors
Ethics declarations
Ethics approval and consent to participate
The study was approved by the Ethics Committee of Shanghai Sixth People’s Hospital and was registered in the Chinese Clinical Trial Registry (ChiCTR2100052216). Informed consent was obtained from all participants.
Consent for publication
Not Applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Qiao, Y., Ye, Z., Xu, J. et al. Preoperative serum calcium could be a prognostic factor for surgical treatment of recurrent patellar dislocation: a retrospective study. BMC Musculoskelet Disord 23, 578 (2022). https://doi.org/10.1186/s12891-022-05527-y
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12891-022-05527-y