Abstract
Objective
To investigate the clinical effect of internal fixation of a Ni–Ti arched shape-memory connector in the treatment of distal tibiofibular syndesmosis ligament injury.
Methods
From January 2013 to January 2016, 108 cases of ankle fracture with distal tibiofibular syndesmosis ligament injury in our hospital were selected, and all of them were fixed with ASCs or screw fixation. The functional evaluation and efficacy evaluation were performed according to the Olerud Molander Ankle Score (Omas) and SF-36. At the same time, follow-ups recorded the incidence of postoperative complications: osteoarthritis, superficial infection, symptomatic hard and soft tissue irritation, early removal and poor reduction of internal fixation, and later loss of reduction.
Results
In the ASC(Ni–Ti Arched shape-memory Connector) group, the incidence of symptomatic hardware, soft tissue or superficial infection decreased to 2.77%(from 13.8% or 11.1% in SCREW group). The early removal rate(2.77%) of internal fixation was also lower than that of the screw group. While the incidence of osteoarthritis is 13.8% in SCREW group, the incidence of osteoarthritis in the later follow-up was also as low as 1.38% in ASC group. Loss of fracture reduction due to removal of the fixation device for the distal tibiofibular syndesmosis ligament was not observed in the ASC group. With two postoperative scoring systems (OMAS and SF-36), patients in the ASC group significantly get higher score than that in SCREW group.
Conclusion
The design of the Ni–Ti arched shape-memory connector can be adapted to the irregular anatomical structure of the malleolus and the ability to continue to contract by body temperature. The use of ASCs in fixation of articular ligaments can preserve a slight range of motion, and the results suggest that ASCs can effectively reduce the incidence of fixation looseness, fracture, infection and other complications.
Similar content being viewed by others
Introduction
Ankle injuries usually involve ligaments related to the tibia and fibula, of which the joint ligament of the inferior tibia and fibula is the more difficult to detect. These ligaments are named the anterior inferior tibiofibular syndesmosis ligament(AITFL), posterior-distal tibiofibular syndesmosis ligament, inferior transverse tibiofibular syndesmosis ligament and interosseous ligament. These ligaments ensure stability and relative movement between the tibia and fibula. This group of ligaments also helps the tibia and fibula sustain the weight of the body and are key ligaments in the ankle joint [Surgical procedure A total of 108 cases of ankle joint fractures and distal tibifibular syndesmosis ligament injuries underwent open reduction and internal fixation under the guidance of two professors in our department. The difference is that the screw group implemented traditional screw fixation of the distal tibifibular joint, while the ASC group implemented ASC fixation. Here, we describe in detail the reduction and fixation of the distal tibiofibular syndesmosis ligament in patients with ASC. After standard methods of reduction of the fibular and tibial fractures were performed, the distal tibiofibular joint was reduced under direct visualization of the syndesmosis and held at its anatomical position by periarticular reduction forceps. The ankle joint was positioned at an angle of 90° between the tibial shaft and the foot during syndesmosis reduction and fixation. Two holes with diameters of 1.5 to 2.0 mm (According to the size of the ASC spike teeth) were drilled bilaterally on the fibula and tibia. Then, the Ni-Ti arched shape-memory connector (ASC) was placed in cold (0–4 °C) water to allow plastic deformation of the Ni-Ti alloy. The claws were unfolded. Appropriate sized ASCs were implanted in the holes. Warm water (40 °C) was applied for irrigation and compression. The memory alloy creates a continuous fixation force triggered by body temperature. Then, a fluoroscopic stress test was used to confirm the syndesmotic reduction. (Fig. 1) Postoperatively, the affected limb was elevated for 3 days. For most patients, gradual full-range mobilization without weight bearing was recommended as soon as possible under the supervision of a qualified physiotherapist, and patients were encouraged to perform progressive active exercises. Partial or full weight bearing was allowed between three and four weeks after surgery, depending on patient tolerance and fracture stability. Follow-up was obtained at 1, 3, 6, and 12 months after surgery and yearly thereafter. Plain anteroposterior (AP) and lateral radiographs were obtained at each visit. All changes in the position of the implant and reduction, fixation failures and removal or complications were recorded. At the latest follow-up, functional outcomes were assessed by one of the authors using the Olerud Molander Ankle Score (OMAS) [20, 21]. The Medical Outcomes Study 36-item short-form health survey (MOS SF-36) questionnaire was chosen to assess the effect of ankle fractures and lesions on health-related quality of life at the same time [22].
Results
No patients were lost to follow-up. The mean follow-up time from surgery was 42 ± 11 months. SPSS software was used to analyse the basic clinical information of patients in the two groups, and we confirmed that there was no statistically significant difference in the basic clinical information, such as sex, age, BMI and other indicators, between the two groups.
During our follow-up, we had only one case of osteoarthritis in the ASC group, while in the screw group, we found 5 (13.8%) patients with delayed osteoarthritis, and the data were statistically significant.In addition, the screws need to be routinely removed 1-2 months after surgery. The device removal rate was 100%, while in the ASC group, the early removal rate was only 2.77% (2 cases), which greatly reduced the number of operations and costs for patients. The application of ASC was small and located on the surface of the bone, so there was no need to worry about the problem that the fractured ASC cannot be removed. At the same time, in the follow-up of complications in the ASC group, we found that the incidence of symptomatic hardware and soft tissue irritation was only 2.77% and the occurrence of superficial infection was the same, and the incidence of related complications in the SCREW group was 13.8% and 11.1%, respectively. We performed AP assessment for the joint reduction of patients more than one month after the operation and half a year later. We found that the probability of poor reduction and loss of reduction in the screw group was 13.8% and 11.1%, respectively, while in the ASC group, we found only one patient with symptoms of loss of reduction. Statistical analysis of the data are included in Table 1.
To better understand the patient's prognosis and experience, we used the SF-36 and scoring rules for OMAS statistical prognosis. In OMAS score system, patients in ASC group significantly get higher scores than SCREW group. And also, scores collected in ASC group by MOS SF-36 scoring system performs better than that of SCREW group. (Table 2)
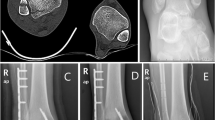
In the group of patients divided by surgical intervention, we selected two patients, and after signing informed consent, pre- and postoperative X-ray fluoroscopy results were used to show the practical effect and prognosis of the two surgical methods (Fig. 2 for ASC and Fig. 3 for SCREW fixation).
Pre- and postoperative radiographs of a patient in the ASC group. A, B Fracture of the lateral malleolus and ligament injury of the distal tibiofibular joint were obvious. C, D After reduction and fixation of the lateral malleolar fracture, ASC was added to reduce and fix the ligament relationship of the distal tibiofibular joint. E, F The figure shows the patient's fracture reduction and stability more than one year after the removal of all fracture internal fixations
Pre- and postoperative radiographs of a patient in the SCREW group. A, B Fragments of the internal and external and posterior ankles and ligaments of the distal tibiofibular joint were evident. C, D After the reduction and fixation of the fracture, a screw was added to reduce and fix the ligament relationship of the distal tibiofibular joint. E, F The figure shows the patient's fracture reduction and stability approximately one month after the removal of all fracture internal fixations
Discussion
After comparing with the follow-up results of the SCREW group, we found that either the screw or the ASC device used to fix the distal tibiofibular joint can obtain satisfactory prognostic results. A slight difference is that in the statistics of complications, we found that the incidence of symbolic hardware and soft tissue irritation and Malreduction has decreased. Simultaneously, because the ASC device does not require early removal of the fixation device, the need for secondary surgery is reduced in the short term and the chance of loss of reduction is also reduced.
With our understanding of ankle joint fractures combined with distal tibifibular syndesmosis ligament injuries, there is no doubt about the necessity of timely and effective stabilization of the distal tibifibular joint [23]. Solid and stable lag screws can effectively recover from the tibiofibular joint and syndesmosis ligament repair. According to the surgeon's habits, after resetting the tibiofibular joint, 3 or 4 layers of cortical bone can be selected to achieve the maximum fixation effect [24, 25]. However, the problems exposed by this fixed method are similar to a chain reaction. Early patients reported cases of lag screw fracture (3 cases) and loose screw fracture (13 cases) [6]. While people are still studying whether penetrating several layers of the cortex, inserting a few screws, or leaving broken screws in the body affects the prognosis of patients [26, 27], more scholars believe that an intact, solid screw limits the slight displacement between the tibiofibular bones, which is the culprit for many complications of the distal tibiofibular syndesmosis ligament group [28]. Statistics show that the incidence of OA (osteoarthritis) in SCREW group patients (13.8%) is significantly higher than that in ASC group. Screw fixation that penetrates three or even four layers of cortical bone is solid and effective, and it also completely limits the microscopic changes in the joint. Activity. Violation of the normal physiological function of joints may be the main reason for the high incidence of OA. Except for the occurrence of definite diagnosis of osteoarthritis as an evaluation of the treatment effect, the postoperative prognostic scores of the two patients we quoted are also used as important parameters for follow-up prognosis. OMAS itself is a professional score related to the ankle joint, and SF-36 is also a commonly used scoring system for evaluating the patient's prognosis comfort [20,21,22]. Solid joint fixation often leads to various degrees of complications in the joint. The removal of inferior tibiofibular screws between 1 and 2 months after surgery is recommended by many professors and literatures. A second operation for implant removal could lead to potential infections, an increased cost to the patient, missed work days, or other complications [29, 30]. Moreover, a small prospective trial suggested that the screw fixation method resulted in malreduction and loss of reduction [31]. Beumer et al. showed that syndesmosis screw fixation did not prevent syndesmosis separation under normal weight bearing [32]. Therefore, the separation of syndesmosis is sometimes inevitable after the screw is removed. Traditional X-ray and intraoperative fluoroscopy are not accurate in assessing the reduction of tibiofibular syndesmosis ligament injury, especially in determining whether the fibula is externally rotated.
ASC is widely used in other medical disciplines and provides inspiration [10,11,12,13,14,15,16,17]. It is a solid and reliable rigid fixation screw that can replace a fixed distal tibiofibular joint in new ways. The results of long-term follow-up and early distal tibiofibular joint fixation show that the removal rate of the device is 1.38% (100% for screws). Of the two patients in the group who had the internal fixation device removed early, one patient strongly requested early removal of the internal fixation device because of his own wishes. Another patient developed local hard object irritation, and the implant had to be removed after the patient's reduction and recovery was assessed. As mentioned above, the existence of the broken screw in the body in the report does not affect the prognosis of the patients [8]. However, broken screws cannot be easily removed, which causes inner anxiety. The investigators found that four patients had ruptured the ASC fixator during follow-up, and superficial fixation enabled the operator to completely remove the ASC device without difficulty. In addition, in the postoperative imaging examination and evaluation of the patient, no malreduction was found until the end of the follow-up. Only one patient had osteoarthritis symptoms in the late follow-up.
Currently, a suture button system as a device-fixed distal tibiofibular joint has been in use for several years by fixing the nonrigid limit under significant activity tibiofibular syndesmosis ligaments and repairing tibiofibular syndesmosis ligaments [33].
The application of this system reduces the risk of poor joint reduction [5]. In terms of its later functional score, compared with patients in the screw group, patients in the suture button system group had a higher OMAS score, a lower VAS pain score, and a stronger VAS function [34,35,36,37]. Allowing the physiological range of movement of the distal tibifibular joint can theoretically avoid the removal of the internal fixation device and reduce the incidence of adverse events such as damage to the fixation device and loss of reduction after early removal. Even though the TightRope system was initially presented as a device that did not need removal, the rate of implant removal might be as high as 25% [38]. In the current review it was 10% on average. Several authors have already made suggestions to lower the rate of implant irritation and subsequent removal [39,40,41]. In addition, the main material of the suture button device is an ultrahigh molecular weight polyethylene loop, which can become loose under load, even if the tension has been adjusted during surgery. Forsyth et al. found that in their model of distal tibiofibular syndesmosis ligament injury, no amount of force applied was able to maintain distal tibiofibular syndesmosis ligament reduction by a suture button device. The study found that the suture button device loosened after the patient had been fully weight-bearing for some time [42, 43].
Researchers have not stopped at the problem of avoiding early removal of internal fixation, so absorbable screws have emerged. Polyosteolytic acid degrades more slowly than other polymers and retains strength for longer periods, so it may be more suitable for the fixation of tibiofibular syndesmosis ligament. However, studies have shown that absorbable screws have failed to effectively reduce the incidence of complications compared with traditional screws. Removal rates of internal fixation are higher [44,45,46,47,48]. Moreover, Bostman et al. found that the reaction rate of polyglycolic acid-related foreign bodies reached 5.3% and that of polylactic acid foreign bodies reached 0.2% [49].
ASC fixtures perform well in other medical disciplines, giving us encouragement. We tried to use nitinol alloy memory ASC internal fixation to treat distal tibiofibular syndesmosis ligament injury. Medical nitinol alloy is an alloy material with a special shape memory function at a specific temperature, and its deformation temperature is 0 °C- 5 °C and recovery temperature is 30 °C-40°C. It has the characteristics of high strength, strong bending and torsion resistance, fatigue resistance, corrosion resistance, nontoxicity and good histocompatibility. The restorative force generated by the memory alloy at a body temperature of 37 °C is used to generate dynamic and continuous compressive stress to achieve the fixation effect. Nitinol alloy ASC, as one of its important applications in recent years, has been widely used in the treatment of multiple fractures. Navicular bone, shoulder blades, and collarbone non-load-bearing bone can be used independently to obtain reliable fixation. In the tibia platform, the femoral condyle position can also adapt to changeful fracture lines, such as auxiliary steel, and obtain satisfactory curative effects [10,11,12,13,14,15,16,17]. Nitinol memory ASCs were used for the first time in the treatment of tibiofibular syndesmosis ligament injury in this group. Compared with other internal fixation materials, it has the following characteristics: (1) According to the different types of ankle fractures, the anterior or posterior part of the tibiofibular joint was exposed through the lateral malleolar fracture incision. Imminent reduction under direct vision without additional incisions helps to avoid poor or excessive reduction of the tibiofibular joint (Fig. 1). (2) The ASC design medium, a variety of models, generally medium (20 mm wide) can meet most of the cases, the two claws of the ASC range 12 to 15 mm, can pass through a layer of cortical bone hook into the medullary cavity. The ASC device can limit the gap between the joints by immobilizing the joints with a single layer of cortex, while maintaining slight movement. The incidence of broken is also reduced; (3) The continuous compressive stress of ASC at normal body temperature may be one of the important factors of high healing rate and short healing time in this group of cases. (4) ASC fixation of the tibiofibular joint does not require a second operation to remove the joint in advance. In some cases, fractures occurred after ligament healing, and there was no loss of reduction. The two broken segments were located on both sides of the tibiofibular joint and did not enter the bone marrow cavity. (5) ASC is located on the surface of the anterior distal tibiofibular syndesmosis ligament or the posterior syndesmosis ligament, which is deep on the surface, without complications such as soft tissue irritation or internal fixation discomfort.
In conclusion, in this study, we adopted two surgical methods to draw conclusions after comparing prognosis and complications. We failed to set all the operation methods, and the second follow-up time was not long enough. Although there are many limitations in our research, we can still obtain guidance from them. The results of our series suggest favourable treatment outcomes of syndesmosis injuries with ASC fixation. The ASC group was used to fix the inferior tibiofibular syndesmosis ligament injury. We fixed the joint by only penetrating the single layer of cortical bone, and only one claw was screwed into the tibia and fibula. This fixation method can effectively limit the gap between the tibia and fibula (Although it shrinks after warming, the device is a monocortical fixation, and the spacing between the compressed tibia and fibula depends on the location of the drill hole in the monocortical fixation). The relative mobility of the joints, but the unicortical fixation allows slight movement between the joints, which is also consistent with the physiology of the inferior tibiofibular joint. According to the results of the initial control study, the ASC may not only serve as an effective device providing continuous concentrative compression for syndesmosis lesion healing but also retain the micromovable feature, thereby aiding the restoration of joint function permitting early rehabilitation with a low incidence of postoperative hardware complications such as breakage, irritation and looseness. Furthermore, a large, prospective, randomized controlled trial and bio-mechanical testing are underway for a future study.
Availability of data and materials
The table in the article has provided the data of this study in more detail, If you need more information, please contact the newsletter and the first author of this article.
References
**e Y, Cai L, Deng Z, Ran B, Hu C. Absorbable screws versus metallic screws for distal tibiofibular syndesmosis injuries: a meta-analysis. J Foot Ankle Surg. 2015;54(4):663–70. https://doi.org/10.1053/j.jfas.2015.03.010.
Zhang Y, Wang P, **a Y, et al. Application of a shape-memory alloy concentrator in displaced patella fractures: technique and long-term results. J Knee Surg. 2017;30(2):166–73. https://doi.org/10.1055/s-0036-1584187.
Latham AJ, Goodwin PC, Stirling B, Budgen A. Ankle syndesmosis repair and rehabilitation in professional rugby league players: a case series report. BMJ Open Sport Exerc Med. 2017;3(1):e000175. https://doi.org/10.1136/bmjsem-2016-000175.
Amis JA. Avoiding suture knot prominence with suture button along distal fibula: technical tip. Foot Ankle Int. 2011;32(11):1102.
Andersen MR, Frihagen F, Madsen JE, Figved W. High complication rate after syndesmotic screw removal. Injury. 2015;46(11):2283–7. https://doi.org/10.1016/j.injury.2015.08.021.
Beumer A, van Hemert WL, Niesing R, et al. Radiographic measurement of the distal tibiofibular syndesmosis has limited use. Clin Orthop Relat Res. 2004;423:227–34. https://doi.org/10.1097/01.blo.0000129152.81015.ad.
Brosky T, Nyland J, Nitz A, Caborn DN. The ankle ligaments: consideration of syndesmotic injury and implications for rehabilitation. J Orthop Sports Phys Ther. 1995;21(4):197–205. https://doi.org/10.2519/jospt.1995.21.4.197.
Choudhary RK, Theruvil B, Taylor GR. First metatarsophalangeal joint arthrodesis: a new technique of internal fixation by using memory compression staples. J Foot Ankle Surg. 2004;43(5):312–7. https://doi.org/10.1053/j.jfas.2004.07.003.
Chen B, Chen C, Yang Z, Huang P, Dong H, Zeng Z. To compare the efficacy between fixation with tightrope and screw in the treatment of syndesmotic injuries: A meta-analysis. Foot Ankle Surg. 2019;25(1):63–70. https://doi.org/10.1016/j.fas.2017.08.001.
Cong DY, Saha G, Barnett MR. Thermomechanical properties of Ni-Ti shape memory wires containing nanoscale precipitates induced by stress-assisted ageing. Acta Biomater. 2014;10(12):5178–92. https://doi.org/10.1016/j.actbio.2014.08.017.
Sun H, Luo CF, Zhong B, Shi HP, Zhang CQ, Zeng BF. A prospective, randomised trial comparing the use of absorbable and metallic screws in the fixation of distal tibiofibular syndesmosis injuries: mid-term follow-up. Bone Joint J. 2014;96-B(4):548–54. https://doi.org/10.1302/0301-620X.96B4.32171.
Dattani R, Patnaik S, Kantak A, Srikanth B, Selvan TP. Injuries to the tibiofibular syndesmosis. J Bone Joint Surg Br. 2008;90(4):405–10. https://doi.org/10.1302/0301-620X.90B4.19750.
Gräff P, Alanazi S, Alazzawi S, et al. Screw fixation for syndesmotic injury is stronger and provides more contact area of the joint surface than TightRope®: a biomechanical study. Technol Health Care. 2020;28(5):533–9. https://doi.org/10.3233/THC-191638.
Hao ZC, **a Y, Wu JH, Zhang YT, Xu SG. Application of a Ni-Ti arched shape-memory connector in unstable lateral malleolus fractures: a retrospective study. Injury. 2019;50(2):551–7. https://doi.org/10.1016/j.injury.2018.10.037.
Høiness P, Strømsøe K. Tricortical versus quadricortical syndesmosis fixation in ankle fractures: a prospective, randomized study comparing two methods of syndesmosis fixation. J Orthop Trauma. 2004;18(6):331–7. https://doi.org/10.1097/00005131-200407000-00001.
Huber T, Schmoelz W, Bölderl A. Motion of the fibula relative to the tibia and its alterations with syndesmosis screws: a cadaver study. Foot Ankle Surg. 2012;18(3):203–9. https://doi.org/10.1016/j.fas.2011.11.003.
Hunt KJ. In fibular fractures with associated syndesmotic injury, open reduction and internal fixation with the tightrope device reduced malreduction at 3 months compared with screw fixation. J Bone Joint Surg Am. 2020;102(16):1465. https://doi.org/10.2106/JBJS.20.00992.
Jan Bartoníček. Anatomy of the tibiofibular syndesmosis and its clinical relevance. Surg Radiol Anat. 2003;25(5–6):379–86.
Kortekangas T, Savola O, Flinkkilä T, et al. A prospective randomised study comparing TightRope and syndesmotic screw fixation for accuracy and maintenance of syndesmotic reduction assessed with bilateral computed tomography. Injury. 2015;46(6):1119–26. https://doi.org/10.1016/j.injury.2015.02.004.
Forsythe K, Freedman KB, Stover MD, Patwardhan AG. Comparison of a novel FiberWire-button construct versus metallic screw fixation in a syndesmotic injury model. Foot Ankle Int. 2008;29(1):49–54. https://doi.org/10.3113/FAI.2008.0049.
Le B, McVary K, McKenna K, Colombo A. A Novel Thermal-activated shape memory penile prosthesis: comparative mechanical testing. Urology. 2017;99:136–41. https://doi.org/10.1016/j.urology.2016.09.007.
Res LCS, Lubberts B, Shah SH, DiGiovanni CW. Health-related quality of life after adverse bleeding events associated with antithrombotic drug therapy - A systematic review. Hellenic J Cardiol. 2019;60(1):3–10. https://doi.org/10.1016/j.hjc.2018.06.012.
Levi DS, Kusnezov N, Carman GP. Smart materials applications for pediatric cardiovascular devices. Pediatr Res. 2008;63(5):552–8. https://doi.org/10.1203/PDR.0b013e31816a9d18.
**e L, **e H, Wang J, et al. Comparison of suture button fixation and syndesmotic screw fixation in the treatment of distal tibiofibular syndesmosis injury: a systematic review and meta-analysis. Int J Surg. 2018;60:120–31. https://doi.org/10.1016/j.ijsu.2018.11.007.
Lin CF, Gross ML, Weinhold P. Ankle syndesmosis injuries: anatomy, biomechanics, mechanism of injury, and clinical guidelines for diagnosis and intervention. J Orthop Sports Phys Ther. 2006;36(6):372–84. https://doi.org/10.2519/jospt.2006.2195.
**long L, Tongxiang L, Chen W, Limin D. Surface corrosion enhancement of passive films on NiTi shape memory alloy in different solutions. Mater Sci Eng C Mater Biol Appl. 2016;63:192–7. https://doi.org/10.1016/j.msec.2016.02.066.
Manjoo A, Sanders DW, Tieszer C, MacLeod MD. Functional and radiographic results of patients with syndesmotic screw fixation: implications for screw removal. J Orthop Trauma. 2010;24(1):2–6. https://doi.org/10.1097/BOT.0b013e3181a9f7a5.
Naqvi GA, Shafqat A, Awan N. Tightrope fixation of ankle syndesmosis injuries: clinical outcome, complications and technique modification. Injury. 2012;43(6):838–42. https://doi.org/10.1016/j.injury.2011.10.002.
Norkus SA, Floyd RT. The anatomy and mechanisms of syndesmotic ankle sprains. J Athl Train. 2001;36(1):68–73.
Obaisi NA, Galang-Boquiren MT, Evans CA, et al. Comparison of the transformation temperatures of heat-activated Nickel-Titanium orthodontic archwires by two different techniques. Dent Mater. 2016;32(7):879–88. https://doi.org/10.1016/j.dental.2016.03.017.
Böstman O, Päivärinta U, Manninen M, Rokkanen P. Polymeric debris from absorbable polyglycolide screws and pins. Intraosseous migration studied in rabbits. Acta Orthop Scand. 1992;63(5):555–9. https://doi.org/10.3109/17453679209154737.
Olerud C, Molander H. A scoring scale for symptom evaluation after ankle fracture. Arch Orthop Trauma Surg. 1984;103(3):190–4. https://doi.org/10.1007/BF00435553.
Sanders D, Schneider P, Taylor M, et al. Improved reduction of the tibio-fibular syndesmosis with tightrope compared to screw fixation: results of a randomized controlled study. J Orthop Trauma. 2019;33(11):531–7.
Schepers T. Acute distal tibiofibular syndesmosis injury: a systematic review of suture-button versus syndesmotic screw repair. Int Orthop. 2012;36(6):1199–206. https://doi.org/10.1007/s00264-012-1500-2.
Schepers T, Van Esther MM, et al. Complications of syndesmotic screw removal. Foot Ankle Int. 2011;32(11):1040–4.
Schepers T. To retain or remove the syndesmotic screw: a review of literature. Arch Orthop Trauma Surg. 2011;131(7):879–83. https://doi.org/10.1007/s00402-010-1225-x.
Shur VB, Georgiev KG, Richards JJ. Internal compression screw exchange for reduction of distal tibiofibular syndesmotic injuries. Orthopedics. 2016;39(2):e377–9. https://doi.org/10.3928/01477447-20160201-06.
Förschner PF, Beitzel K, Imhoff AB, et al. Five-year outcomes after treatment for acute instability of the tibiofibular syndesmosis using a suture-button fixation system. Orthop J Sports Med. 2017;5(4):2325967117702854. https://doi.org/10.1177/2325967117702854.
Song DJ, Lanzi JT, Groth AT, et al. the effect of syndesmosis screw removal on the reduction of the distal tibiofibular joint: a prospective radiographic study. Foot Ankle Int. 2014;35(6):543–8. https://doi.org/10.1177/1071100714524552.
Song Y. Comparative Study of the Clinical Results of Absorbable Screws and Cortical Bone Screws on Distal Tibiofibular Syndesmosis Injury[J]. Medical Recapitulate. ISSN:1006-2084,2013,19(12).
Tao Y, Zou Y, Yang J. Clinical Application Observation of Absorbable Screw in The Treatment of Distal Tibiofibular Syndesmosis Injury[J]. Sichuan Medical Journal. ISSN:1004-0501,2016,37(06).
Lalli TA, Matthews LJ, Hanselman AE, Hubbard DF, Bramer MA, Santrock RD. Economic impact of syndesmosis hardware removal. Foot (Edinb). 2015;25(3):131–3. https://doi.org/10.1016/j.foot.2015.03.001.
Toker SM, Canadinc D. Evaluation of the biocompatibility of NiTi dental wires: a comparison of laboratory experiments and clinical conditions. Mater Sci Eng C Mater Biol Appl. 2014;40:142–7. https://doi.org/10.1016/j.msec.2014.03.060.
Tucker A, Street J, Kealey D, McDonald S, Stevenson M. Functional outcomes following syndesmotic fixation: a comparison of screws retained in situ versus routine removal - Is it really necessary? Injury. 2013;44(12):1880–4. https://doi.org/10.1016/j.injury.2013.08.011.
Yablon IG, Heller FG, Shouse L. The key role of the lateral malleolus in displaced fractures of the ankle. J Bone Joint Surg Am. 1977;59(2):169–73.
Willmott HJS. Re: Outcome and complications of treatment of ankle diastasis with tightrope fixation[J]. Injury. 2010;41(10):1097.
Wuest TK. Injuries to the Distal Lower Extremity Syndesmosis. J Am Acad Orthop Surg. 1997;5(3):172–81. https://doi.org/10.5435/00124635-199705000-00006.
Zhang P, Liang Y, He J, Fang Y, Chen P, Wang J. A systematic review of suture-button versus syndesmotic screw in the treatment of distal tibiofibular syndesmosis injury. BMC Musculoskelet Disord. 2017;18(1):286. https://doi.org/10.1186/s12891-017-1645-7.
Zhang Y, Zhao X, Tang Y, Zhang C, Xu S, **e Y. Application of Ni-Ti alloy connector for the treatment of comminuted coronal plane supracondylar-condylar femoral fractures: a retrospective review of 21 patients. BMC Musculoskelet Disord. 2013;14:355. https://doi.org/10.1186/1471-2474-14-355.
Acknowledgements
The completion of this study is thanks to the various facilities provided by the hospital, the help of the authors and the staff of the department, and finally, the most important thanks to the patients for selflessly providing relevant research data.
Funding
This study did not receive any funding.
Author information
Authors and Affiliations
Contributions
**bo Zhao and Yuntong Zhang designed and completed the project, and Yan **a undertook the statistical analysis and conclusion summary of the project data. Xuhui Wang was responsible for the follow-up of the two groups of patients, Shuogui Xu hosted and communicated the whole topic and article writing, and Yang **e participated in the topic discussion and conclusion summary. **bo Zhao and Yuntong Zhang contributed the same as co-first authors. Shuogui Xu is the corresponding author of this paper. The author(s) read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participants
The Ethics Committee of The First Affiliated Hospital of Naval Military Medical University approved the research project and analysis of the patient. Written informed consent to participants was obtained from all subjects and/or their legal guardian(s) in ethical approval and consent to participants section.
Consent for publication
All subjects or legal guardians signed an informed consent form, supporting and agreeing to the publication of relevant images and table data in the research.
Competing interests
The authors have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Zhao, J., Zhang, Y., **a, Y. et al. Application of an arched, Ni–Ti shape-memory connector in repairing distal tibiofibular syndesmosis ligament injury. BMC Musculoskelet Disord 23, 476 (2022). https://doi.org/10.1186/s12891-022-05449-9
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12891-022-05449-9